INTRODUCTION
Internal resorption (IR) is a relatively rare occurrence, and most cases follow injury to pulp tissue, such as physical trauma or caries-related pulpitis. The condition is more frequently observed in male than in female subjects.1 Although IR is a relatively rare entity,2, 3 a higher prevalence of the condition has been associated with teeth that had undergone specific treatment procedures such as auto-transplantation.4
Tooth resorption may go unnoticed for many years; often the patient is unaware of it because of the lack of symptoms. Pain may be reported if the process is associated with significant pulpal inflammation. The resorption remains as long as vital tissue remains and may result in the communication of pulp tissue with the periodontal ligaments. Usually, the clinician will discover the resorption as an unusual radiographic finding on a routine examination when periapical radiographs are taken. The patient's history will give the practitioner clues to when the tooth was last worked on and whether trauma was involved.
CASE REPORT
A 23-year-old male, reported to Military Dental Centre, with chief complaint of discolouration of upper front tooth. History revealed trauma to upper anterior teeth a year back.
On examination, upper left central incisor was discoloured (pinkish blue) (Figure 1), with perforation on its lingual surface. Tooth was non-tender to percussion. Vitality was checked using hot gutta purcha stick and cold ice stick, which concluded the tooth to be vital. An intra-oral periapical radiograph of the tooth was taken which revealed large radiolucent lesion completely involving the pulp chamber, along with the perforation of the lingual wall (Figure 2).
Figure 1.

Pretreatment intra-oral photograph.
Figure 2.
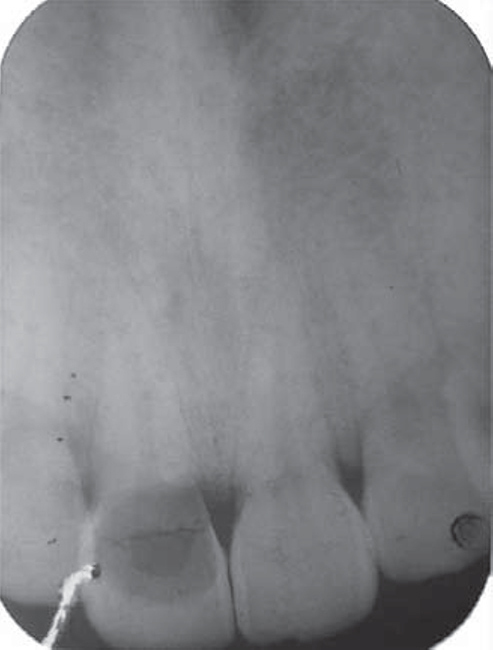
Pretreatment intra-oral periapical radiograph.
On the basis of clinical and radiological examination, a diagnosis of inflammatory hyperplasia of pulp (IR) was made. The patient was advised root canal treatment followed by jacket crown for tooth number 21.
Root canal treatment was completed with conventional root canal therapy (Figure 3). Post and core was built and porcelain fused to metal jacket crown was made to give the best aesthetic to the patient (Figure 4). A four-month follow-up demonstrated clinically asymptomatic and adequately functional tooth.
Figure 3.

Post-obturation intra-oral periapical radiograph.
Figure 4.

Post-treatment intra-oral photograph.
DISCUSSION
Resorption of calcified dental tissue, involves demineralisation due to reversal of the cation exchange and lacunar resorption by osteoclasts.5 The resorptive process can progress at different speeds and with different periods of activity. Two main patterns are seen: (i) inflammatory resorption, and (ii) replacement or metaplastic absorption. In inflammatory resorption, the resorbed dentin is replaced by inflamed granulation tissue. Although this pattern may involve any portion of the canal, the cervical zone is affected most frequently (pulp inflammation is usually caused by bacterial invasion).6 The resorption continues as long as vital pulp remains; typically, the coronal pulp is necrotic with the apical portion remaining vital. The results of pulp testing are variable. In this pattern the area of destruction usually appear as a uniform well-circumscribed symmetric radiolucent enlargement of the pulp chamber or canal. When it affect the coronal pulp, the crown can display a pink discolouration (pink tooth of Mummery, named after the anatomist “James Howard Mummery”) as vascular resorptive process approaches the surface. When it occurs in the root, the original outline of the canal is lost and a balloon like radiographic dilation of the canal is seen. Although most cases are progressive, some cases are transient and arise in traumatised teeth or those that have recently undergone orthodontic or periodontal therapy.7
For IR to occur, the outermost protective odontoblast layer and the predentin of the canal wall must be damaged, resulting in exposure of the underlying mineralised dentin to odentoclasts. The precise injurious events necessary to bring about such damages have not been completely elucidated. Various aetiological factors have been proposed for the loss of predentin, including trauma, caries and periodontal infections, excessive heat generated during restorative procedures on vital teeth, calcium hydroxide idiopathic dystrophic changes within normal pulp.3, 7, 8, 9, 10, 11, 12, 13 In a study of 25 teeth with IR, trauma was found to be the most common predisposing factor that was responsible for 45% of cases examined.14 The suggested aetiologies in the other cases were inflammation as a result of carious lesions (25%) and carious/periodontal lesions (14%). The cause of IR in the remaining teeth was unknown. Other reports in the literature also support the view that trauma and pulpal inflammation/infection are the major contributory factors in the initiation of IR.15
Genetic factors have been implicated in the development of IR lesions in a study of monozygotic twins. The link between interleukin (IL)-1 gene polymorphism and root resorption has been reported. The presence of IL-1 + C3953 allele is the sign of predisposed susceptibility to an exaggerated inflammatory response.16 In patients with IR, the pulp tissue in the area of destruction is vascular and exhibits increased cellularity and collagenisation, immediately adjacent to the dentinal wall are numerous multinucleated dentinoclasts, which are histologically and functionally identical to osteoclasts, an inflammatory infiltrates characterised by leucocytes, histiocytes and polymorphonuclear leucocyte is not uncommon.17 In replacement resorption, the normal pulp tissue is replaced by woven bone that fuses with the adjacent dentin.
TREATMENT PERSPECTIVES
Successful treatment requires proper diagnosis and a good history. Once IR has been diagnosed, the clinician must make a decision on the prognosis of the tooth. It is important to know if the resorption is purely internal, initiating within the pulp chamber and not communicating with the periodontal ligament. If the resorptive area is communicating, then it is an internal-external resorptive case, and the prognosis is questionable. If the tooth is deemed restorable and has a reasonable prognosis, root canal treatment is the treatment of choice. The aim of root canal treatment is to remove any vital and necrotic pulp that might be sustaining and stimulating the resorbing cells via their blood supply and to disinfect and obturate the root canal system. Access cavity preparation should be conservative, preserving as much tooth structure as possible and should avoid further weakening of the already compromised tooth.
Prognosis is good; however, the patient must be recalled, since the resorptive defect can recur. Once perforation occurs, therapy becomes more difficult and the prognosis is poor; in such cases repair must be carried out to create a barrier. Initial placement of calcium hydroxide paste occasionally may result in re-mineralisation of the site of perforation and stop the resorptive process.6 Extraction often is necessary for radicular perforation that does not respond to therapy.
CONCLUSION
To date, root canal treatment remains the only treatment of choice with teeth diagnosed with IR. Early detection and a correct differential diagnosis are essential for successful management of the outcome of IR to prevent over weakening of remaining tooth structure and root perforations. Because the resorptive defect is the result of an inflamed pulp and the clastic precursor cells are predominantly recruited through the blood vessels, controlling the process of internal root resorption is conceptually easy, via the blood supply to the resorbing tissues with conventional root canal therapy.
CONFLICTS OF INTEREST
None identified.
REFERENCES
- 1.Goultschn J, Nitzan D, Azaz B. Root resorption: review and discussion. Oral Surg Oral Med Oral Pathol. 1982;54:586–591. doi: 10.1016/0030-4220(82)90199-2. [DOI] [PubMed] [Google Scholar]
- 2.Andreasen JO, Andreasen FM. Root resorption following traumatic dental injuries. Proc Finn Dent Soc. 1992;88:95–114. [PubMed] [Google Scholar]
- 3.Andreasen JO. Luxation of permanent teeth due to trauma: a clinical and radiographic follow up study of 189 injured teeth. Scand J Dent Res. 1970;19:273–286. doi: 10.1111/j.1600-0722.1970.tb02074.x. [DOI] [PubMed] [Google Scholar]
- 4.Ahlberg K, Bystedt H, Eliasson S, Odenrick L. Long term evaluation of auto-transplanted maxillary canines with completed root formation. Acta Odontol Scand. 1983;41:23–31. doi: 10.3109/00016358309162300. [DOI] [PubMed] [Google Scholar]
- 5.Jablonski S. Jablonski's Dictionary of Dentistry. Krieger; Malabar, FL: 1992. p. 676. [Google Scholar]
- 6.Neville BW, Damn DD, Allen CM, Bouquot JE. Oral and Maxillofacial Pathology. 2nd ed. WB Saunders; Philadelphia: 1995. [Google Scholar]
- 7.Silveria FF, Nunes E, Soares JA, Ferreria CL, Rotstein I. Double ‘pink tooth’ associated with extensive internal root resorption after orthodontic treatment: a case report. Dent Traumatol. 2009;25:43–47. doi: 10.1111/j.1600-9657.2008.00755.x. [DOI] [PubMed] [Google Scholar]
- 8.Cabrini R, Maisto O, Manfredi E. Internal resorption of dentin: his-topathologic control of eight cases after pulp amputation and capping with calcium hydroxide. Oral Surg Oral Med Oral Pathol. 1957;10:90–96. doi: 10.1016/s0030-4220(57)80120-0. [DOI] [PubMed] [Google Scholar]
- 9.Rabinowitch BZ. Internal resorption. Oral Surg Oral Med Oral Pathol. 1972;33:263–282. doi: 10.1016/0030-4220(72)90396-9. [DOI] [PubMed] [Google Scholar]
- 10.Ashrafi MH, Sadeghi EM. Idiopathic multiple internal resorptions: report of case. ASDC J Dent Child. 1980;47:196–199. [PubMed] [Google Scholar]
- 11.Brady J, Lewis DH. Internal resorption complicating orthodontic tooth movement. Br J Orthod. 1984;11:155–157. doi: 10.1179/bjo.11.3.155. [DOI] [PubMed] [Google Scholar]
- 12.Walton RE, Leonard LA. Cracked tooth: an etiology for ‘idiopathic’ internal resorption? J Endod. 1986;12:167–169. doi: 10.1016/S0099-2399(86)80056-5. [DOI] [PubMed] [Google Scholar]
- 13.Brooks JK. An unusual case of idiopathic internal root resorption beginning in an unerupted permanent tooth. J Endod. 1986;12:309–310. doi: 10.1016/S0099-2399(86)80114-5. [DOI] [PubMed] [Google Scholar]
- 14.Caliskan MK, Türkün M. Prognosis of permanent teeth with internal resorption: a clinical review. Endod Dent Traumatol. 1997;13:75–81. doi: 10.1111/j.1600-9657.1997.tb00014.x. [DOI] [PubMed] [Google Scholar]
- 15.Patel S, Ricucci D, Durak C, Tay F. Internal root resorption: a review. J Endod. 2010;36:1107–1121. doi: 10.1016/j.joen.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 16.Urban D, Mincik J. Monozygotic twins with idiopathic internal root resorption: a case report. Aust Endod J. 2010;36:79–82. doi: 10.1111/j.1747-4477.2010.00223.x. [DOI] [PubMed] [Google Scholar]
- 17.Shafer WG, Hine MK, Levy BM, Tomich CE. A Text Book of Oral Pathology. 4th ed. Saunders; Philadelphia: 1993. [Google Scholar]


