INTRODUCTION
Right iliac fossa (RIF) pain is a common clinical problem. Acute appendicitis is the commonest cause for RIF pain and emergency abdominal surgery. Clinical symptoms and signs of appendicitis are often non-specific and can mimic a variety of commonly encountered disease processes leading to false negative diagnosis. Prompt and accurate diagnosis with early surgical intervention is essential to minimise morbidity. Despite advances in various investigative modalities, diagnosis of appendicitis may still remain difficult in sizeable number of patients. Misdiagnosis of appendicitis is maximal in women of child bearing age because of frequent clinical overlap of appendicitis with various gynaecological conditions. We report a rare case of pelvic endometriosis with involvement of the right fallopian tube simulating acute appendicitis in a young female.
CASE REPORT
A 37-year-old lady presented at our emergency department with chief complaints of pain RIF for one day duration associated with three episodes of vomiting in last 12 hours. She denied any history of urinary or bowel complaints. Her menstrual cycle had been regular; however, she often used to have dysmenorrhoea. She had her last menstrual period seven days back. On clinical examination, she was febrile (temp: 100°F) and had tachycardia (pulse rate: 92 per minute). Local examination revealed tenderness in the RIF and hypogastric region with rebound tenderness especially around the McBurney's point. An urgent total leucocyte count showed leukocytosis (TLC 12300 per cu mm). Based on the history, clinical and laboratory findings a provisional diagnosis of acute appendicitis was made. She was referred for an urgent ultrasonography (USG) for confirmation of the diagnosis. Transabdominal USG (5 MHz, 6 MHz convex and linear probes; Wipro GE LOGIQ P3) with a partially distended urinary bladder revealed bilateral complex adnexal masses with internal echoes (Figure 1A, B) abutting the uterus. The uterus, however, was found to be normal. The ovaries could not be demonstrated separately. Free fluid was present in RIF as well as pouch of Douglas. Using graded compression, a blind ending, tubular, non-compressible and non-peristaltic structure (diameter: 7 mm) was found extending from the RIF towards the midline (Figure 2). There was probe tenderness over this tubular structure. Although, the images of the tubular structure as mentioned above were not typical for classical appendicitis, based on the clinical profile and ultrasonographic findings, possibility of atypical appendicitis in association with pelvic endometriosis was raised. The attending surgical specialist was informed about pros and cons of the ultrasonographic findings who decided in favour of surgery. At surgery, the appendix was found to be normal. Appendectomy was carried out. The incision line was extended to look for pelvic pathologies. There were bilateral endometriotic ovarian cysts (chocolate cysts) with the right ovarian cyst having been ruptured with spillage of chocolate coloured fluid contents in the pelvis and RIF. Both ovarian cysts were plastered with the uterus with extensive adhesions in the pelvis and nearby areas (grade IV endometriosis). What was thought to be an atypical appendicitis on USG was actually an inflamed and kinked right fallopian tube extending from the right iliac fossa reaching almost up to the midline with the ampullary end directed medially. There were multiple areas of endometrial implants on the fallopian tube. Opinion of gynaecologist was sought during the surgery who advised medical treatment for endometriosis. The patient has been put on tab danazol 100 mg BD and has shown good response on follow up after two months.
Figure 1(A, B).
Ultrasonogram of pelvis (transverse & longitudinal sections) demonstrating bilateral complex adnexal masses with internal echoes. UT: uterus, UB: urinary bladder, TR: transverse, SAG: sagittal
Figure 2.
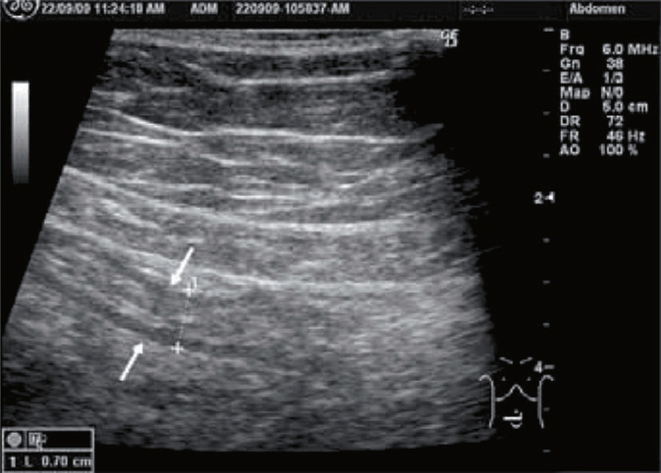
High resolution ultrasonogram of right iliac fossa and hypogastric region demonstrating a blind ending tubular structure with diameter of 7 mm.
DISCUSSION
Acute appendicitis remains the most common surgical emergency with a life-time occurrence of 7%.1
Despite being a common problem and technological advancement in the recent past, acute appendicitis may still pose a diagnostic dilemma even to the best of clinicians. Laboratory investigations, though useful, are often non-specific. There are a sizeable number of conditions which can mimic appendicitis, some of them are urolithiasis, pelvic inflammatory disease, pyelonephritis, haemorrhagic ovarian cyst, ovarian torsion, ruptured ectopic pregnancy, mesenteric adenitis, infectious ileocolitis, typhlitis, Crohn's disease, right sided diverticulitis, epiploic appendagitis, bowel ischaemia, mucocoele of appendix, ovarian vein thrombosis, endometriosis, intussusceptions, perforated peptic ulcer and cholecystitis.2, 3, 4 Rarely, endometriosis involving the terminal ileum can mimic clinical features of appendicitis. The RIF and hypogastric pain which our patient had can be retrospectively explained by rupture of endometriotic cyst in the right adnexa and/or inflamed right fallopian tube. Jeffrey et al5 mentions about dilated right fallopian tube mimicking the appearance of an appendix and suggests presence of undulating mucosal folds in the fallopian tube as a differentiating factor from appendix. Our patient had salpingitis resulting in overall thickening and enlargement of tubal diameter. The right fallopian tube, which was persistently tender, non-compressible, non-peristaltic and was blind ending (usual sonographic criteria for diagnosing appendicitis) in its terminal aspect was mistaken as inflamed appendix in the clinical setting of localised peritonitis at RIF. The atypical sonographic features in this case were: the proximal end of the tubular structure could not be traced to the caecum, diameter of the tubular structure was 7 mm which could be considered borderline for a diagnosis of appendicitis and the structure was rather too long to be a normal sized appendix.
Imaging has a well established and definite role in the assessment of RIF pain including acute appendicitis. Imaging of appendicitis has seen paradigm shift from graded compression ultrasonography to multidetector CT each with its pros and cons.5, 6, 7 A dedicated appendiceal ultrasonography by an experienced sonologist preferably a radiologist should be the frontline imaging modality for a suspected case of appendicitis even today. CT scan is best reserved as a second line imaging modality when ultrasonography findings are negative or equivocal in a case with strong clinical suspicion.8, 9, 10 Advantages of ultrasonography are that it can be carried out with minimum delay and can yield surgically relevant information like confirmation of diagnosis of appendicitis, status of inflamed appendix, location and orientation of appendix, presence or absence of any associated complications, etc. besides suggesting alternative diagnoses, which helps in appropriate surgical planning. However, the potential pitfalls of USG as well as CT scan in the diagnosis of appendicitis need to be understood.
Our case is unique in the sense that there is no mention in the literature about endometriosis with inflamed fallopian tube simulating appendicitis clinically and sonologically. It also highlights two important issues. Firstly, all non-compressible, non-peristaltic and blind ending tubular structures in RIF in an appropriate clinical setting need not necessarily represent an inflamed appendix. Secondly, rarely an inflamed fallopian tube can simulate appendicitis on ultrasonography and should be kept a differential diagnosis when imaging features are atypical.
CONFLICTS OF INTEREST
None.
REFERENCES
- 1.Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910–925. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- 2.Ripolles T, Martinez-Perez MJ, Morote V, Solaz J. Diseases that simulate acute appendicitis on ultrasound. Br J Radiol. 1998;71:94–98. doi: 10.1259/bjr.71.841.9534708. [DOI] [PubMed] [Google Scholar]
- 3.Yu J, Fulcher AS, Turner MA, Halvorsen RA. Helical CT evaluation of acute right lower quadrant pain: part I, common mimics of appendicitis. Am J Roentgenol. 2005;184:1136–1142. doi: 10.2214/ajr.184.4.01841136. [DOI] [PubMed] [Google Scholar]
- 4.Yu J, Fulcher AS, Turner MA, Halvorsen RA. Helical CT evaluation of acute right lower quadrant pain: part II, uncommon mimics of appendicitis. Am J Roentgenol. 2005;184:1143–1149. doi: 10.2214/ajr.184.4.01841143. [DOI] [PubMed] [Google Scholar]
- 5.Jeffrey RB, Jain KA, Nghiem HV. Sonographic diagnosis of acute appendicitis: interpretive pitfalls. Am J Roentgenol. 1994;162:55–59. doi: 10.2214/ajr.162.1.8273690. [DOI] [PubMed] [Google Scholar]
- 6.Levine CD, Aizenstein O, Wachsberg RH. Pitfalls in the CT diagnosis of appendicitis. Br J Radiol. 2004;77:792–799. doi: 10.1259/bjr/95663370. [DOI] [PubMed] [Google Scholar]
- 7.Levine CD, Aizenstein O, Lehavi O, Blachar A. Why we miss the diagnosis of appendicitis on abdominal CT: evaluation of imaging features of appendicitis incorrectly diagnosed on CT. Am J Roentgenol. 2005;184:855–859. doi: 10.2214/ajr.184.3.01840855. [DOI] [PubMed] [Google Scholar]
- 8.Gaitini D, Beck-Razi N, Mor-Yosef D. Diagnosing acute appendicitis in adults: accuracy of colour Doppler sonography and MDCT compared with surgery and clinical follow-up. Am J Roentgenol. 2008;190:1300–1306. doi: 10.2214/AJR.07.2955. [DOI] [PubMed] [Google Scholar]
- 9.Poortman P, Oostvogel HJ, Bosma E. Improving diagnosis of acute appendicitis: results of a diagnostic pathway with standard use of ultrasonography followed by selective use of CT. J Am Coll Surg. 2009;208:434–441. doi: 10.1016/j.jamcollsurg.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 10.Holscher HC, Heij HA. Imaging of acute appendicitis in children: EU versus US or US versus CT? A European perspective. Pediatr Radiol. 2009;39:497–499. doi: 10.1007/s00247-008-1130-4. [DOI] [PubMed] [Google Scholar]



