INTRODUCTION
A female child presented with clitoromegaly due to virilisation caused by congenital adrenal hyperplasia (CAH). After correction of the endocrine imbalance, clitoral reduction was done by the ventral approach. The advantages of the ventral approach over the traditional dorsolateral approach are discussed.
CASE REPORT
A girl presently eight years of age was first brought at the age of three years to the paediatric OPD of our hospital by the parents with complaints of an enlarged clitoris since birth. Examination of the genitalia showed ambiguity with an enlarged clitoris resembling a penis. The labia major were normal with no rugosity or fusion. The labia minora were absent. Clitoromegaly was present; the clitoris measured about 3 cm in length in the non-tumescent state, with a penile appearance. The urethral meatus was caudally located (hypospadiac). The introitus was normal. The patient was not hirsute. Growth and development were consistent with age. Radiograph of the wrist revealed bony age corresponding to chronological age. Karyotyping done revealed the patient to be a female (44+XX). Serum 17 α hydroxyprogesterone (17 α OHP) was high (132.8 ng/mL, normal 0–0.6 ng/mL). Blood pressure was normal. Ultrasound examination of the abdomen and pelvis did not clearly image the internal genitalia. MRI revealed a normal vagina, right ovary, and a hypoplastic uterus. Serum electrolytes were within normal limits.
A diagnosis of a female child with congenital adrenal hyperplasia (CAH), a low salt-losing type with clitoral hypertrophy was made. The patient was placed on cortisol therapy. The patient progressed well; 17 α OHP after six months of therapy was within normal limits. The patient remained well thereafter on cortisol replacement therapy. The clitoral hypertrophy persisted and the patient was taken up for correction in June 2009 at the age of eight years.
Surgery was performed under general anaesthesia under cortisol cover. The patient was positioned supine with legs abducted, catheterised, prepped, and draped. Stay sutures were placed on the labia majora to keep them abducted and on the glans clitoris to keep it in traction. The incision was marked, being circumcoronal and extending posteriorly on either side of the urethral plate region up to the introitus. About 1:200,000 adrenaline was infiltrated under the clitoral skin and urethral plate area. The clitoris was degloved till its root (Figure 1). Two vertical incisions were made over the degloved clitoral shaft ventrally, incising the Bucks fascia and tunica albuginea in this region. The corpora cavernosa were dissected and ligated at the clitoral base and excised preserving the neurovascular structures to the glans clitoris running dorsally on the clitoral shaft. The clitoris was shortened by folding the redundant clitoral tissue and anchoring the glans clitoris to soft tissues below the symphysis pubis. The redundant clitoral skin was split dorsally in the midline and transposed down both sides to form the clitoral hood and labia minora (Figure 2). The postoperative recovery was uneventful. The patient now has normal appearing genitalia and sensate clitoris. Figure 3 is a sketch showing the operative plan.
Figure 1.
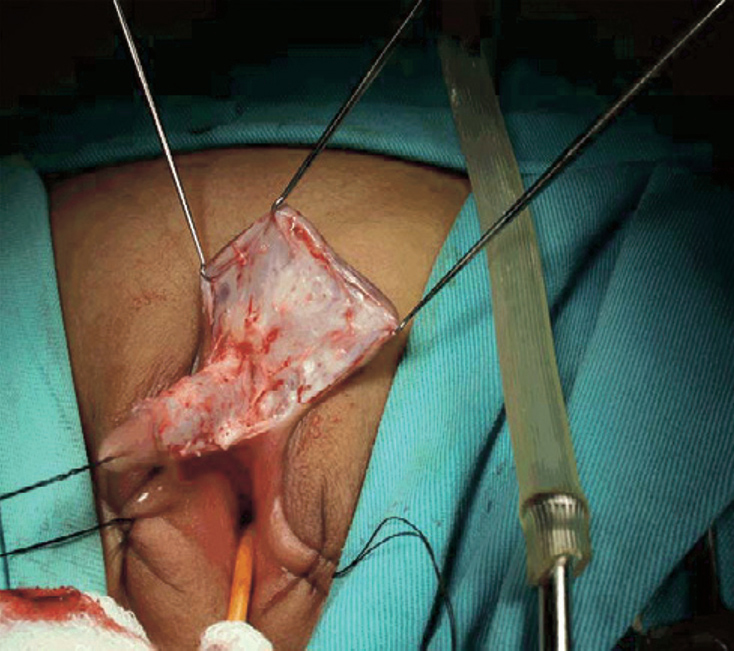
The enlarged clitoris has been degloved at surgery.
Figure 2.

Immediate postoperative appearance. The clitoris has been reduced and the missing clitoral hood and labia minora have been reconstructed.
Figure 3.
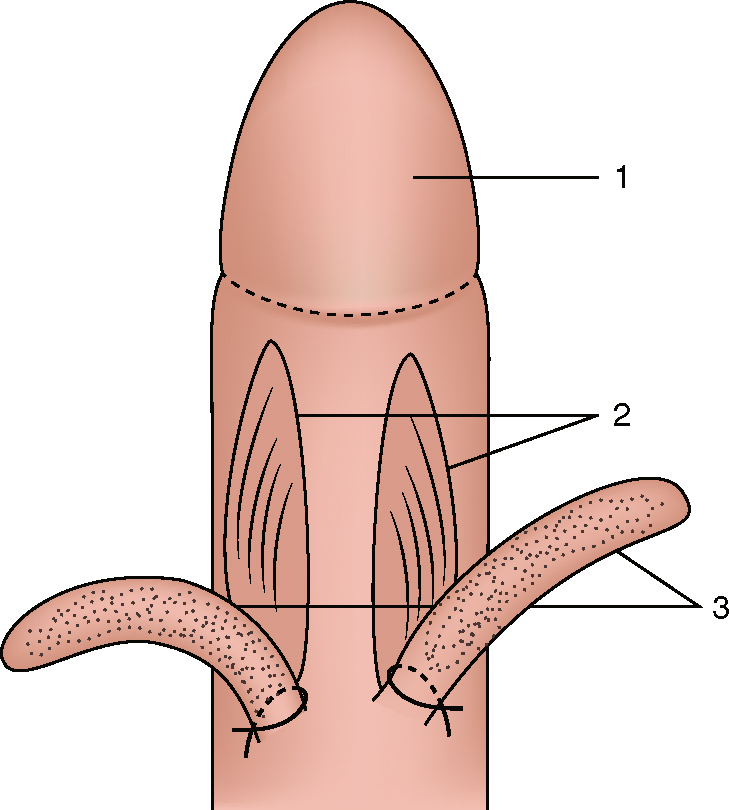
Sketch of the operative plan showing the ventral aspect of the degloved clitoris; (1) glans clitoris, (2) ventral incisions on shaft, (3) corpora dissected and ligated.
DISCUSSION
Enlargement of the clitoris can be found in CAH and other virilising states. Clitoral enlargement is frequent in CAH and the decision to undergo reduction is an individualised one.1 While minor degrees of clitoral enlargement can be left alone, marked enlargement can cause confusion as to gender, embarrassment and a morbid body image and anxiety to the parent. The preferred age for surgery is debatable. Opinion is divided between early surgery which offers better healing and early restitution of a normal body image and surgery at a later age where the patient can participate in the decision making.1 The surgical goals are achievement of a normal appearance of the genitalia with preservation of sensation in the clitoris, as loss of sensation in the clitoris is disabling with inability to achieve orgasm.
Surgery for clitoral enlargement has seen some evolution. The earliest surgery done was clitorectomy; this is no longer acceptable. Clitoral recession involves repositioning the clitoris under the symphysis pubis. This procedure has the disadvantages that tumescence of the clitoris (as occurs during sexual stimulation) can be painful and micturition can be interfered with.
Clitoral reduction involves the removal of all erectile tissue from the corpora cavernosa of the clitoris with preservation of the neurovascular supply to the glans clitoris. The neurovascular structures to the glans clitoris course on the dorsal aspect of the shaft of the clitoris deep to Buck's fascia.2 The customary approach to the reduction has been by the dorsolateral approach where these structures are identified, isolated, and protected while the erectile tissues are removed.3, 4 A newer approach (as adopted in this case) is the ventral approach where the erectile tissues are excised without identifying or disturbing the neurovascular structures.5 This technique should result in better preservation of sensation in the clitoris and better sexual function.
Alizai et al studied the post-pubertal outcome of patients who underwent clitoral surgery.5 They found the outcomes unsatisfactory with clitoral atrophy or a prominent glans in several cases. Crouch et al studied the sensory thresholds in patients who had undergone clitoral surgery and found significant impairment to sensitivity in the clitoris compared to controls. It is very important to perform clitoral reduction through a ‘safe channel’.6
Pippi et al advocate a corporeal sparing dismembered clito-roplasty; the corpora are repositioned into the labia majora instead of being excised.7 This technique is yet to be evaluated fully. Our patient had an uneventful postoperative recovery with good preservation of sensation (light touch) in the clitoris.
In conclusion, CAH is a not an infrequently encountered entity requiring clitoral reduction in these patients. It is important that sensation in the glans clitoris is preserved during this surgery.
ACKNOWLEDGEMENT
The authors gratefully acknowledge the expert advice and assistance provided at surgery by Dr. Ranjit Raje, MCh.
REFERENCES
- 1.Baskin LS, Erol A, Li YW, Liu WH, Kurzrock E, Cunha GR. Anatomical studies of the human clitoris. Urol. 1999;162:1015–1020. doi: 10.1016/S0022-5347(01)68052-2. [DOI] [PubMed] [Google Scholar]
- 2.O'Connell HE, Sanjeevan KV, Hutson JM. Anatomy of the clitoris. J Urol. 2005;174:1189–1195. doi: 10.1097/01.ju.0000173639.38898.cd. [DOI] [PubMed] [Google Scholar]
- 3.Baskin LS, Erol A, Li YW, Liu WH. Anatomy of the neurovascular bundle: is safe mobilization possible? J Urol. 2001;166:225–230. doi: 10.1097/00005392-200009020-00014. [DOI] [PubMed] [Google Scholar]
- 4.Yang J, Felsen D, Poppas DP. Nerve sparing ventral clitoroplasty: analysis of clitoral sensitivity and viability. J Urol. 2007;178:1598–1601. doi: 10.1016/j.juro.2007.05.097. [DOI] [PubMed] [Google Scholar]
- 5.Alizai NK, Thomas DF, Lilford RJ, Batchelor AG, Johnson N. Feminizing genitoplasty for congenital adrenal hyperplasia: what happens at puberty? J Urol. 1999;161:1592–1593. [PubMed] [Google Scholar]
- 6.Crouch NS, Liao LM, Woodhouse CR, Conway GS, Creighton SM. Sexual function and genital sensitivity following feminizing genitoplasty for congenital adrenal hyperplasia. J Urol. 2008;179:634–638. doi: 10.1016/j.juro.2007.09.079. [DOI] [PubMed] [Google Scholar]
- 7.Pippi Salle JL, Braga LP, Macedo N, Rosito N, Bagli D. Corporeal sparing dismembered clitoroplasty: an alternative technique for feminizing genitoplasty. J Urol. 2007;178:1796–1801. doi: 10.1016/j.juro.2007.03.167. [DOI] [PubMed] [Google Scholar]


