Abstract
Background
Folstein's Mini Mental Status Examination (MMSE) often fails to identify executive dysfunction even if quite severe. Detailed neuropsychological tests and extensive bedside tests are available to evaluate executive function, but most of them are time consuming. This study was done to determine the value of a Clock Drawing Test (CDT) as a simple tool to identify cognitive dysfunction in various neurological disorders and to assess its utility as an adjunct to MMSE in identifying executive dysfunction in a a busy out patient department (OPD).
Methods
A total of 81 patients suffering from neurological disorders and 81 controls were studied. All subjects received the MMSE and the CDT. The CDT is divided into an unprompted task that is sensitive to executive control (CDT 1) and a copying task which is not (CDT 2).
Result
All the three tests (CDT 1, CDT 2 and MMSE) could recognize cognitive and executive function deficits, when compared with age and sex matched controls (p < 0. 001). CDT scores correlated strongly with the level of executive function deficits. CDT+MMSE detected 95% cases as abnormal as compared to 47% detected by MMSE alone.
Conclusion
CDT along with MMSE can detect executive control deficits and cognitive deficits. The CDT 1 tests executive control performance, while CDT 2 tests posterior cortical deficits.
Key Words: Clock drawing, Cognition, Executive control function, Mini mental status examination, Dementia
Introduction
The potential of clock drawing test (CDT) as a screening tool for cognitive impairment has long been a matter of great interest. A completely normal clock suggests that a number of functions are intact [1]. Clock drawing involves comprehension, perception, memory, gross motor function, visual spatial organization, concentration, numerical knowledge, concept of time and inhibition of distracting stimuli. Though it appears simple, drawing of a clock correlates to a complex goal directed behaviour in an abstract environment [1, 2].
Routine tests of cognition such as the Folstein's test or Mini Mental Status Examination (MMSE) often fail to identify executive dysfunction even if severe. There are neuropsychological and extensive bedside tests available to evaluate executive function, but most of them are time consuming. We undertook this study to determine the value of CDT as a simple bed side tool to identify cognitive dysfunction and to assess its utility as an adjunct to MMSE in identifying potential executive dysfunction in a clinical setting [3, 4].
Alzheimer's disease is a typical primary degenerative dementia characterised by defective declarative memory and impaired anterograde learning. However, disturbance of executive function often occurs before the memory decline and can cause problems in day-to-day activities. For example, patients retain their ability to dress but are unable to initiate the task or choose appropriate clothes. The challenge is to identify executive cognitive dysfunction in such patients. Early diagnosis of cognitive deficits in primary degenerative dementia facilitates planning (e.g. execution of will, precautions and advanced directives) while the patient is still capable of taking important decisions [5]. Besides Alzheimer's, various neurological diseases are also known to affect cognition e.g. cerebrovascular accidents (CVA), space occupying lesions (SOL) and infections.
Inability to complete a CDT in a busy outpatient department (OPD) does not establish a diagnosis of dementia but indicates further testing is needed [1, 2, 3, 4, 5, 6, 7, 8]. A normal or equivocal MMSE result doesn't exclude the diagnosis of dementia. However, addition of CDT with careful selection of instructions and time to be depicted can be a useful adjunct [11, 12]. In screening for dementia, CDT proves superior to MMSE [13]. CDT is not designed to be the only form of cognitive evaluation and should be an adjunct to the MMSE [6, 10, 14].
Material and Methods
A total of 81 patients and 81 control subjects were recruited for the study. The study was carried out in the internal medicine outpatient department (OPD) of AFMC, neurology OPD of Command Hospital (Southern Command) and old age homes located in Pune. Informed consent was taken and confidentiality assured. Age, sex and education matched controls were also studied to minimize the confounding effect. Both cases and controls were exposed to CDT (1 and 2) and MMSE tests.
The survivors of stroke, head trauma, meningitis, encephalitis and hypoxic insult to brain, after recovery and becoming independent in daily activities, elderly individuals (>65 years) with reported cognitive impairment and patients with suspected neurological deficits after hypoxic insult to the brain were included in the study. Illiterates, patients with altered sensorium (Glasgow coma scale < 15) and those with sepsis and obvious discomfort were excluded.
The MMSE is a widely used cognitive screening tool due to its brevity, ease of administration and relative breadth. The MMSE consists of 30 items comprising subscales assessing orientation, word registration, attention (via a serial sevens or spelling task), word recall and language. Additionally, a figure copy exercise is included to examine visuospatial abilities [2]. Analysis of MMSE is done based on the age and educational status of the subjects. No direct cut offs are taken as suggested by Crum et al [16].
CDT has been employed by Royall et al [3]. CDT1 reflects performance in a novel situation. The patient selects the overall form of the clock, its size, position on the paper, hands of clock and Roman vs Arabic numerals etc. He must be able to initiate and then maintain his concentration to complete the clock [1, 3, 4]. CDT 2 is a simple copying task also affected by gross motor function. Thus, while CDT 1 reflects overall executive function in clock drawing performance, CDT 2 helps to differentiate it from contribution due to visuospatial praxis [3, 4, 5, 6, 7, 8]. Analysis of CDT was done on a scale of 0-6 as described by Shua et al [15].
Results
In this study, age group of patients varied from 20-79 years and male to female ratio was 58:23. The subjects were divided into groups according to the aetiology (Table 1).
Table 1.
Categorization of patients into various groups for clock drawing test
| Group | Age group | Number of patients |
Mean CDT 1 score | Mean CDT 2 score | Mean MMSE score | |
|---|---|---|---|---|---|---|
| Male | Female | |||||
| Space Occupying Lesions (SOL) | 22-72 | 18 | 4 | 2.44 | 3.33 | 25.44 |
| Vascular | 23-77 | 19 | 6 | 2.1 | 3.7 | 23.6 |
| CNS Infections | 22-79 | 5 | 6 | 4 | 4.66 | 27.66 |
| Metabolic | 46-78 | 4 | − | 1.25 | 2.25 | 21.75 |
| Head Injury | 24 | 1 | − | 6 | 6 | 28 |
| Neuro-AIDS | 32-65 | 4 | 2 | 2.28 | 3.85 | 22.28 |
| Alzheimer's | 46-80 | 7 | 5 | 2.28 | 2.32 | 25.68 |
Examples of clocks drawn are shown in Table 2. Since the data is in terms of scores given to individuals (cases and controls), non parametric Mann-Whitney U test was applied. The hypothesis was to test whether there is any significant difference between the cases and controls with respect to their mean scores (Table 3).
Table 2.
Clock drawing and MMSE pentagons in various neurological disorders
| Age & Sex | CDT1 clock with score | CDT2 clock with score | MMSE pentagon with score | Diagnosis | Education (normal MMSE score) | |
|---|---|---|---|---|---|---|
| SOL | 66, Male | 1
|
1
|
24
|
Multiple ICSOL | 6th (22) |
| Vascular | 54, Male | 1
|
1
|
20
|
Old infarct in Rt. Temporo-parietal region | 7th (23) |
| CNS Infection | 70, Male | 2
|
2
|
24
|
Multiple infective granulomas | Graduate (28) |
| Metabolic | 46, Male | 1
|
1
|
20
|
Hepatic encephalopathy | 12th (28) |
| Head Injury | 24, Male | 6
|
6
|
28
|
Severe head injury | 10th (27) |
| Neuro AIDS | 32, Male | 2
|
1
|
18
|
HIV neurological symptoms | Graduate (29) |
| Alzheimers | 63, Male | 2
|
2
|
27
|
Azheimers | Graduate (28) |
Table 3.
Statistical analysis clock drawing test study
| Variable | Group | n | Mean rank | p value | Significance |
|---|---|---|---|---|---|
| MMSE | Cases | 81 | 49.15 | 0.000 | Highly significant |
| Controls | 81 | 113.85 | |||
| Total | 162 | ||||
| CDT1 | Cases | 81 | 48.99 | 0.000 | Highly significant |
| Controls | 81 | 114.01 | |||
| Total | 162 | ||||
| CDT2 | Cases | 81 | 55.19 | 0.000 | Highly significant |
| Controls | 81 | 107.81 | |||
| Total | 162 |
All the three tests (CDT 1, CDT 2 and MMSE) were able to recognize cognitive and executive function deficits, when compared with age and sex matched controls (p < 0. 001). The segregation of CDT1 scores with respect to number of cases in which MMSE was found to be normal or abnormal is shown in (Fig. 1).
Fig. 1.

MMSE scores for patients with various CDT1 scores
The Shua et al [15] scoring system (0-6) did not have any clear cut off value to identify abnormality. Therefore, 95% confidence interval (CI) for CDT score of controls was calculated (5.24-5.63) and cut off value was taken to be the whole number below the lower 95% confidence limit i.e. 5. MMSE alone could detect 38 (47%) cases as abnormal whereas CDT1 with MMSE detected 77 (95%). When the two tests were compared it was found that they were statistically significant (p value =0.000). Thus CDT1 along with MMSE detects higher percentage of abnormality as compared to MMSE alone (Fig. 2).
Fig. 2.
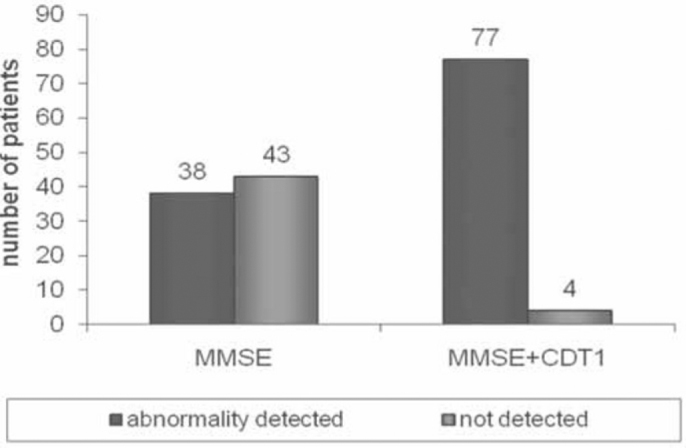
Comparison of MMSE alone with CDT 1+ MMSE.
Two distinct patterns of clock drawing were observed apart from the well established unilateral spatial neglect pattern. Pattern A was observed in cortical diseases particularly with the involvement of right parietal cortex in which both CDT1 and CDT2 scores were affected and pattern B in subcortical lesions or lesions sparing the right parietal cortex where CDT2 was usually found to be normal.
In Table 4, pattern A shows clock drawing of a 70 year old male with Alzheimer's disease where both CDT1 and CDT2 scores are affected indicating involvement of right parietal cortical function. Pattern B on the other hand is clock drawn by a 44 year old male with stroke (right hemiparesis with frontal and temporal lobe affection due to left middle cerebral artery involvement) with normal CDT2 score.
Table 4.
Pattern of clock drawing in cortical lesions with right parietal involvement (A) and right parietal sparing (B)
| Age and Sex | CDT 1 score | CDT 2 score | MMSE pentagon score | |
|---|---|---|---|---|
| A | 70 yr old male | 1 | 1 | 25 |
| B | 44 yr old male | 2 | 6 | 28 |
Discussion
In this study we have found that a CDT can be administered which is strongly associated with an executive function measure. We found that CDT when combined with MMSE is a sensitive tool for detection of cognitive and executive function deficits in various neurological conditions (p value= 0.00), which is in agreement with other studies by Royall et al [3].
When the MMSE score is abnormal and suspicion of cognitive impairment high, abnormal CDT reinforces the diagnosis of cognitive impairment. Difficulty arises in patients with a history of unusual or abnormal function or when the physician doubts their cognitive function (e.g. medication compliance or competency assessment) and when MMSE is normal. In such cases, the CDT can be particularly useful. We found that though CDT2 subset is indicative of posterior cortical deficits and is a copying task much like the MMSE pentagon, CDT1 reflects performance in a novel and ambiguous situation.
In our study we included a heterogeneous group of neurological conditions usually not considered as dementing. Acute infections of the central nervous system (CNS) usually cause delirium and other neurological symptoms. However, chronic CNS infections such as tuberculosis or cryptococcosis may produce a dementing illness. Between 20-30% of patients in advanced stages of HIV infection become demented. CDT may help in early detection of progressive dementia and thus can be used both as a diagnostic as well as a prognostic tool in such patients [17].
Conflicts of Interest
None identified
Intellectual Contribution of Authors
Study Concept : Col SP Gorthi
Drafting & Manuscript Revision : C Mittal
Statistical Analysis : C Mittal, Col S P Gorthi
Study Supervision : Maj Gen S Rohatgi, vsm
References
- 1.Manos PJ, Wu R. The ten point clock test: a quick screen and grading method for cognitive impairment in medical and surgical patients. Int J Psychiatry Med. 1994;24:229–244. doi: 10.2190/5A0F-936P-VG8N-0F5R. [DOI] [PubMed] [Google Scholar]
- 2.Royall DR. Comments on the executive control of clock drawing. J Am Geriatr Soc. 1996;44:218–219. doi: 10.1111/j.1532-5415.1996.tb02452.x. [DOI] [PubMed] [Google Scholar]
- 3.Royall DR, Cordes JA, Polk M. CLOX: an executive clock drawing test. J Neurol Neurosurg Psychiatry. 1998;64:588–594. doi: 10.1136/jnnp.64.5.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berit A. The clock drawing Test. Age and Ageing. 1998;27:399–403. [Google Scholar]
- 5.Solomon PR, Hirschoff A, Kelly B, Relin M, Brush M, Deveaux RD. A 7 minute neuron cognitive screening battery highly sensitive to Alzheimer's disease. Arch neural. 1998;55:349–355. doi: 10.1001/archneur.55.3.349. [DOI] [PubMed] [Google Scholar]
- 6.Folstein M, Folstein S, Mc Hugh PR. Mini Mental State: A practical method for grading the cognitive state of patients for the clinician. Psychiatry Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 7.Royall DR, Polk M. Dementias that present with and without posterior cortical features: an important clinical distinction. J Am Geriatr Soc. 1998;46:98–105. doi: 10.1111/j.1532-5415.1998.tb01022.x. [DOI] [PubMed] [Google Scholar]
- 8.Shulman K, Shedletsky R, Silver IL. The challenge of Time: clock drawing and cognitive functioning in the elderly. Int J Geriatr Psychiatry. 1986;1:135–140. [Google Scholar]
- 10.Freund B, Gravenstein S, Ferris R, Shaheen E. Evaluating driving performance of cognitively impaired and healthy older adults: A pilot study comparing on-road testing and driving simulation. J Am Geriatr Soc. 2002;50:1309–1310. doi: 10.1046/j.1532-5415.2002.50325.x. [DOI] [PubMed] [Google Scholar]
- 11.American Academy of Neurology Subcortical vascular dementia: integrating neuropsychological and neuroradiological data. Neurology. 2005;65(Suppl 3):21–25. doi: 10.1212/01.wnl.0000168877.06011.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Psychometric properties of clock drawing test and MMSE or short performance test (SKT) in dementia screening in a memory clinic population (editorial) J Am Geriatr Soc. 1993;41:249–252. doi: 10.1002/gps.585. [DOI] [PubMed] [Google Scholar]
- 13.Brodaty H, Moore CM. The clock drawing test for dementia of the Alzheimer's type: a comparison of three scoring methods in a memory disorder clinic. Alzheimer Dis Assoc Disord. 1998;12:1–13. [PubMed] [Google Scholar]
- 14.The value of clock drawing in identifying executive dysfunction in people with a normal Mini Mental State Examination Score. CMAJ. 2002;167:859–864. The University of Alberta Division of Geriatrics, Department of Medicine. The Geriatric Assessment Team and the Department of Psychiatry. [PMC free article] [PubMed] [Google Scholar]
- 15.Shua HJ, Koppuzha G, Gross J. A simple scoring system for clock drawing in patients with Alzheimer's disease. J Am Geriatr Soc. 1996;44:335. doi: 10.1111/j.1532-5415.1996.tb00931.x. [DOI] [PubMed] [Google Scholar]
- 16.Crum M, Anthony C, Bassett S, Folstein M. Population based norms for the mini-mental state examination by age and educational level. JAMA 18: 2386-2391. [PubMed]
- 17.Yamamoto S, Mogi N, Umegaki H, Suzuki Y, Ando F, Shimokata H. The clock drawing test as a valid screening method for mild cognitive impairment. Dement Geriatr Cogn Disord. 2004;18:172–179. doi: 10.1159/000079198. [DOI] [PubMed] [Google Scholar]
Uncited Reference
- 9.Shulman K, Gold DP, Cohen CA. Clock drawing and dementia in the community : a longitudinal study. Int J Geriatr Psychiatry. 1993;8:487–496. [Google Scholar]


