Abstract
Drug testing, when carefully collected and thoughtfully interpreted, offers a critical adjunct to clinical care and substance use treatment. However, because test results can be misleading if not interpreted in the correct clinical context, clinicians should always conduct a careful interview with adolescent patients to understand what testing is likely to show and then use testing to validate or refute their expectations. Due to the ease with which samples can be tampered, providers should also carefully reflect on their own collection protocols and sample validation procedures to ensure optimal accuracy.
Keywords: Substance abuse detection, adolescents, substance-related disorders, ethanol, street drugs, urine
It is incumbent on clinicians to detect substance use early and intervene to reduce acute risks and to improve the life course trajectory of addiction and its harms. For clinicians working with adolescents, screening for alcohol and drug use is a critical skill that allows for brief intervention and referral to treatment, an approach endorsed by major professional bodies [1–3] including the American Academy of Pediatrics (AAP) [4]. Screening is best conducted using a validated instrument (such as the S2BI instrument [5]) that can then prompt a discussion between the clinician and adolescent.
At first blush, routine screening of adolescents by testing urine or other bodily fluids might seem like a reasonable strategy for detecting substance use, but this approach is fraught with inaccurate findings and misinterpretation, and worse, leads to mistrust on the part of the adolescent and missed opportunities for nuanced discussions about substance use with a clinician. Abstinence from all substances is recommended throughout adolescence because of the impact of alcohol, marijuana and other drugs on brain development [6]. Routine drug testing of all adolescents, however, is insensitive for detecting sporadic use, and risks obscuring opportunities for counseling and brief interventions that may be better identified by self-report [7].
While routine laboratory testing is not recommended for adolescents there are several indications for which this procedure may provide useful information to supplement a clinical history or to regularly monitor patients in treatment for substance use disorders. Here, we review drugs commonly included in testing panels, bodily fluids and tissues tested, indications for testing, practical concerns, and issues unique to drug testing adolescents as contrasted with its use in adults.
Drugs tested
Although it is possible to test for use of an individual drug, multiple drugs or classes are usually tested at the same time using a single biological sample [8]. The most commonly used immunoassay (IA) drug test panel includes the “SAMHSA-5”, a standard panel established in the 1980s under the Drug-Free Workplace Act. The SAMHSA-5 includes amphetamines, marijuana (tetrahydrocannabinol [THC]), cocaine metabolites, opiates (including heroin, morphine, and codeine, but not synthetic opioids such as oxycodone, hydrocodone, buprenorphine, or methadone), and phencyclidine (PCP) [8,9]. Most drug screens available commercially have panels that expand beyond the SAMHSA-5 to also include benzodiazepines, barbiturates, and additional opiates [8].
Alcohol and drugs vary substantially in their windows of detection, largely owing to their degree of fat solubility. For example, THC and other highly fat-soluble compounds have a very long half-life of elimination and can be detected in urine up to weeks after last use among heavy users). The various windows of detection for a number of commonly used substances are shown in Table 1 [10].
TABLE 1.
Windows of detection in urine for various substances.
| Detection Windows by Drug Test Type
| ||||
|---|---|---|---|---|
| Substance | Urine | Hair | Oral Fluid | Sweat |
| Alcohol | 10-12 hours | N/A | Up to 24 hours | N/A |
| EtG -- Up to 48 hours | ||||
|
| ||||
| Amphetamines | 2 to 4 days | Up to 90 days | 1-48 hours | 7-14 days |
|
| ||||
| Methamphetamine | 2 to 5 days | Up to 90 days | 1-48 hours | 7-14 days |
|
| ||||
| Barbiturates | Up to 7 days | Up to 90 days | N/A | N/A |
|
| ||||
| Benzodiazepines | Up to 7 days | Up to 90 days | N/A | N/A |
|
| ||||
| Cannabis (Marijuana) | 1-30 days | Up to 90 days | Up to 24 hours | 7-14 days |
|
| ||||
| Cocaine | 1 to B days | Up to 90 days | 1-36 hours | 7-14 days |
|
| ||||
| Codeine (Opiate) | 2 to 4 days | Up to 90 days | 1-36 hours | 7-14 days |
|
| ||||
| Morphine (Opiate) | 2 to 5 days | Up to 90 days | 1-36 hours | 7-14 days |
|
| ||||
| Heroin (Opiate) | 2 to 3 days | Up to 90 days | 1-36 hours | 7-14 days |
|
| ||||
| PCP (Phencyclidine) | 5 to 6 days | Up to 90 days | N/A | 7-14 days |
LSD, Mushrooms, Synthetic Cannabinoids, Ecstasy (MDMA) will not be detected by typical drug testing
Sources for testing
There are multiple sources for biologic specimens (often referred to as “biological matrices” in the scientific literature): urine, blood, saliva, hair, breath, sweat, and meconium. These various tissues and bodily fluids exhibit different rates and durations of excretion that result in different detection windows for substances, as demonstrated in Figure 1.
FIGURE 1.
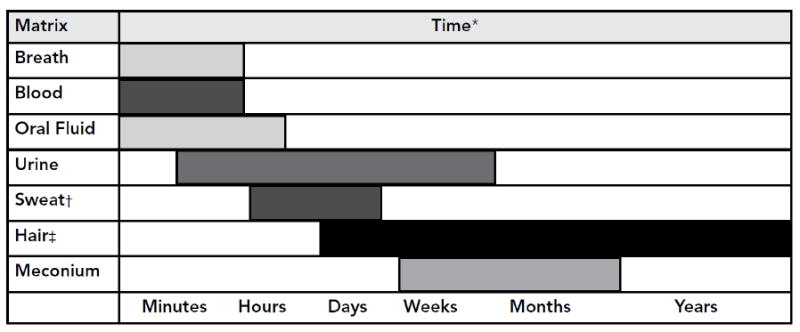
Drug detection times for different biologic specimens used in drug testing.
*Very broad estimates that also depend on the substance, the amount and frequency of the substance taken, and other factors previously listed.
†As long as the patch is worn, usually 7 days.
‡7–10 days after use to the time passed to grow the length of hair, but may be limited to 6 months hair growth. However, most laboratories analyze the amount of hair equivalent to 3 months of growth.
When substances are ingested, they are absorbed in the gastrointestinal tract and distributed to tissues of the body [9]. Substances that are injected, inhaled or snorted bypass gastrointestinal absorption and are delivered immediately to tissues. Since many drugs are lipid soluble, they must undergo metabolism in the liver to render them water soluble which then allows them to be eliminated in urine. Blood and breath reflect moment-to-moment serum levels of an ingested substance, and offer the earliest and shortest windows of detection for substances [8]. Sweat and saliva reflect the presence of a drug within the body several hours later. Urine offers a somewhat longer window of detection for substances, usually varying from one day after consumption to several weeks. Hair and meconium offer the longest windows of detection (weeks to months). Advantages and disadvantages of different matrices for drug testing are shown in Table 2.
TABLE 2.
Advantages and disadvantages of various matrices (i.e., bodily fluids and tissues) used for drug testing.
| a | ||
|---|---|---|
| Matrix | Advantages | Disadvantages |
| Urine |
|
|
| Oral Fluid |
|
|
| Sweat |
|
|
| Blood |
|
|
| b | ||
| Hair |
|
|
| Breath |
|
|
| Meconium |
|
|
Here we review the various biologic matrices for drug testing:
(1) Urine
Of all the matrices, urine is the most commonly used for adolescent drug testing and is the most thoroughly studied [9,11]. However, for an adolescent patient, its collection is somewhat invasive since it requires either a sophisticated collection protocol which is not readily available in medical offices or direct observation (e.g., by a clinician or a parent) to prevent tampering [7,12]. Compounding this, many pediatricians are unfamiliar with proper collection procedures and with the limitations of urine drug screening [11].
Currently, the most commonly used urine drug testing approach involves automated immunoassay either alone as a point-of-care test or as an initial screen for a 2-step testing procedure [7,8]. Results from IA are qualitative (i.e., a drug or its metabolite is denoted either present or absent, without the quantity reported). In the 2-step approach, a screening IA is followed by confirmatory gas chromatography-mass spectrometry (GC-MS). If any substances are positive on the initial IA, a separate quantity of the same sample is then subjected to GC-MS as a confirmatory test for those same substances, with negative results on the IA disregarded. GC-MS provides a quantitative result to help guide the clinician, which can be used to follow serial samples and determine whether the metabolite concentration is rising or falling, which may suggest ongoing use or abstinence, respectively. Even still, caution is warranted as levels may vary with urine concentration, the amount of drug used, and time since last use, thus making an absolute determination regarding whether use is ongoing difficult.
IA is often used as a point-of-care test given its convenience, low cost, and relatively rapid results (although results are often not available quickly enough to guide clinical management in emergent situations) [7]. Most home urine drug test kits use IA. Although IA has high sensitivity, it has poorer specificity than GC-MS owing to cross-reactivity, whereby compounds in the biologic specimen other than the actual substance or its metabolite bind to the assay and trigger a false-positive result. (For example, PCP assays can turn positive if an individual consumes dextromethorphan, a common component of cough syrup.) Additionally, IA drug tests performed in isolation do not distinguish among drugs within a class (i.e., IA cannot distinguish between various amphetamines, barbiturates, benzodiazepines, or opiates) [8]. GC-MS is not performed as a point-of-care test and usually must be sent to a laboratory, resulting in a delay [7]. Newer but less widely used technologies include liquid chromatography-mass spectrometry and tandem mass-spectrometry, which can be used to bypass the initial screening IA and identify a larger number of substances and metabolites [8].
Often, laboratories report the urine creatinine, which helps the clinician correct for the relative concentration or dilution of the urine. Concentration of the urine by the kidneys results in elevated levels of drug metabolites; therefore, urine concentrations of certain drugs and their metabolites are usually divided by the urine creatinine. An example of this is THC, whose excretion in the urine can continue for up to one month after most recent use in heavy users [13], and urine samples positive for THC must be carefully interpreted to distinguish ongoing excretion from new use. Urine THC concentration should be divided by the urine creatinine concentration in order to determine whether the creatinine-normalized THC concentration is increasing or decreasing with consecutive urine samples [14] and these ratios can then be compared to nomograms of THC excretion in order to make a clinical interpretation [15]. Practical issues, such as timing of the urine sample collection, specimen collection techniques, validation of the sample, and result interpretation are covered later in this chapter.
(2) Blood
Drug testing of blood samples is usually only performed in emergency situations, and due to the invasiveness of obtaining a blood sample, the need for specially trained phlebotomists, and the expense of blood drug testing, it is rarely performed in primary care settings [7,9]. An additional limitation is that obtaining blood samples requires venipuncture and locating venous access among injection drug users can be very difficult [9]. Unlike urine samples, blood samples generally detect alcohol and drug compounds themselves rather than their metabolites. Blood testing typically detects substance use that occurred within 2 to 12 hours of the test [7].
(3) Oral (saliva)
Oral fluid testing is less commonly used but oral samples represent a convenient, promising matrix for many settings. Unlike urine samples, oral samples are not easily tampered with, and can be collected with minimal invasion of privacy [15,16]. Oral secretions contain either the original drug compound or its metabolite for approximately 24-48 hours after last use [9,15,16]. Importantly, use of breath sprays, mouthwash or other oral rinses containing alcohol does not affect drug testing result as long as they are not used within 30 minutes of sample collection [17]. To collect an oral sample, a swab is placed adjacent to the lower gums against the inner cheek and left in place for several minutes before being inserted into a vial for transportation to the laboratory [9]. Point-of-care oral testing is also available in some settings [18].
(4) Hair
Hair drug tests have the advantage of detecting substance use days to months, or in some cases, years, later [9,19]. Drug metabolites are present in hair as early as one week after most recent use, and because metabolites remain trapped in the core of the hair as it grows, hair provides a rough timeline of use over an extended period [9,20]. Hair grows at a rate of approximately one-half inch per month, and so the standard 1.5-inch hair sample obtained close to the root in most drug testing protocols gives information over past 3-month drug use [8].
Because of the long period of detection for hair samples, they are useful for detecting chronic substance use, understanding the duration of a patient’s drug use over the long term, and indicating periods of abstinence [20–22]. Conversely, hair testing is not helpful in detecting sporadic use when weekly or even monthly drug testing is required as part of a drug treatment plan [9]. Additionally, drug use often must relatively heavy in order for testing to detect levels in hair. Other limitations of hair testing include that individuals can surreptitiously remove the sample through shaving, that sweat production can cause drug metabolites to travel proximally up the hair shaft thus affecting drug test interpretation, and that drugs can be incorporated into hair through simple exposure from second-hand smoke [23,24]. An additional potential consideration is that drug concentrations can be affected by the melanin content of hair, resulting in potentially higher concentrations of certain drugs in dark hair as compared to blond or red hair [15,25]. Bleaching or coloring the hair may also alter concentrations of metabolites [26].
The hair sample is typically cut from the back of the head using scissors, cutting as close to the scalp as possible to estimate most recent drug use [9]. For patients who are bald or who have shaved their head, hair can be taken from the armpit, face, or other unshaven part of the body, so long as a sufficiently long enough sample can be taken. No point-of-care hair drug testing currently exists.
(5) Breath
Breath testing, often referred to colloquially as the “Breathalyzer” test after the original brand name testing device, is used exclusively for instantaneous estimation of blood alcohol content [8]. Breath testing provides an accurate measure of the actual blood alcohol content at that moment in time, and is more frequently used in law enforcement or in emergency departments than in primary care. The US Department of Transportation maintains an active list of approved breath testing devices for the interested reader (https://www.transportation.gov/odapc/approved-evidential-breath-testing-devices) [27].
(6) Sweat
The US Food and Drug Administration (FDA) has approved a patch for collection of sweat for drug testing that is placed on the skin for 3-7 days prior to being sent to a laboratory for interpretation [8,9]. In Europe. a wipe is also available that is not currently FDA-approved due to concerns regarding its accuracy [9,12]. Sweat testing checks for substances and their metabolites in the bloodstream in the hours before and during the time that the patch is applied [8,9]. Currently, sweat testing is only available for the SAMHSA-5. Patches that pucker or show other evidence of interference when removed have been designed in attempt to reduce tampering [8].
(7) Meconium
Meconium is obtained from newborns and used as a measure of maternal substance use in the third trimester [8,12,28,29]. Meconium is present in a newborn’s first several stools. Meconium testing is used as a screen in the newborn nursery or neonatal intensive care unit when maternal substance use during pregnancy is suspected, and can have critical legal consequences for guardianship of the child [30]. Meconium testing can also inform clinical management of neonatal abstinence syndrome and other newborn withdrawal syndromes.
Indications for drug testing
According to the American Society for Addiction Medicine (ASAM), drug testing should be used “to discourage nonmedical drug use and diversion of controlled substances, to encourage appropriate entry into addiction treatment, to identify early relapse and to improve outcomes of addiction treatment through the use of long-term post-treatment monitoring.” Since substance use is often secret, adolescents may not forthcoming and drug testing may be useful when history is negative in the context of clinical signs and symptoms suggesting substance use. [7]. Indications for adolescent drug testing are explored here.
(1) Emergent care
Drug tests are commonly used in emergent situations, such as when an adolescent presents with altered mental status [7,8]. Some common clinical scenarios include attempted suicide, motor vehicle injury or other injury in which substance use may have been a contributor, unexplained seizures, syncope, arrhythmia, or toxidromal signs that suggest a particular intoxication or withdrawal pattern [7]. In such cases, consent for the drug screen is inferred, and its results may be used to guide clinical management. However, drug testing results are generally not available immediately and cannot reliably be used early in emergent management; therefore, initial decisions, such as whether to provide naloxone for suspected opioid overdose should be made by the clinician based on presenting signs and symptoms [7,8]. Additionally, because highly sensitive drug testing may detect substances at limits far lower than therapeutic doses, drug screens may identify additional substances that are present but not contributing to the acute intoxication or withdrawal picture and may therefore be misleading [7]. Once the patient is stabilized, however, drug testing results may be helpful in determining subsequent management, particularly once confirmatory testing results are available.
(2) Assessment of behavioral or other mental health concerns
In primary care or mental health care settings, substance use by an adolescent may be suspected as underlying or complicating symptoms of depression, anxiety, inattention, hyperactivity, or other broader concerns such as a school failure or interpersonal difficulties [7,9]. In these situations, voluntary drug testing (i.e., drug testing with the assent of the adolescent and the consent of a guardian) may serve as a helpful complement to a careful history. A positive drug screen might indicate substance use that an adolescent previously denied, leading to an opportunity for an honest conversation [7]. However, as highlighted below in the discussion of interpretation of results, there are a number of limitations in drug testing that might result in a negative result despite clinically significant substance use by an adolescent.
(3) Substance use treatment
Drug testing is performed as a routine component of outpatient adolescent substance use treatment [7,9]. It serves multiple roles, including preventing adverse effects of pharmacotherapy (e.g., precipitating opioid withdrawal if a clinician provides naltrexone for alcohol use disorder if that patient were also surreptitiously using opioids), and monitoring for use of illicit substances during treatment and/or adherence with prescribed medications. such as stimulants for comorbid attention deficit hyperactivity disorder (ADHD) or buprenorphine for opioid use disorder [9]. In residential substance use treatment, drug testing helps support the drug-free therapeutic environment [8].
In monitoring for illicit drug use during treatment, testing should be performed at random times, as discussed below, since adolescents are often knowledge of the short window of detection in urine for many substances and might otherwise simply abstain from use for the several days leading up to a scheduled test [7,9]. Testing should also be performed frequently enough (e.g., at least weekly) to detect any use occurring during treatment [8]. A positive drug screen should never serve as grounds for termination from the substance use treatment program, but rather should prompt a careful conversation between the adolescent and clinician to reconsider the current treatment plan [7,8]; multiple positive drug tests may indicate the need for a higher level of care, for example [8].
Contingency management, which relies on incentives to encourage ongoing abstinence for adolescents with a substance use disorder, often uses drug testing for monitoring [31]. Adolescents who attend their scheduled visits and/or have negative urine drug tests are provided monetary prizes or other rewards to reinforce their treatment plan adherence [9,31,32]. In many settings, the value of prizes increases incrementally with each successive attended visit or negative drug screen, which further improves the efficacy of treatment [31,33,34].
(4) Other settings
A number of other potential settings for adolescent drug testing exist. Workplace drug testing is federally mandated by the Department of Transportation (DOT) for private-sector transportation workers, and many of the current standards for workplace testing have emerged from these regulations [9]. For example, the SAMHSA-5 urine drug screen was codified in the late 1980s for DOT workplace testing. Some adolescents and young adults may find themselves seeking or maintaining employment in settings where drug screening is routine [7]. Drug screens from non-federal employers can and often do expand their drug testing panels to include substances in addition to those on the SAMHSA-5 [9]. Many policies regarding when, where and how employers can test their employees are set by states; a full review is beyond the scope of this article but a complete, up-to-date listing of relevant policies is available at a cost from the Drug and Alcohol Testing Industry Association (DATIA), an independent industry organization [35].
Some jurisdictions have proposed drug screening in school. However, this approach is opposed by the AAP due to insufficient evidence that it discourages adolescent drug use, difficulty in correctly interpreting results, and potential adverse consequences such as disciplinary action, decreased participation in sports and other school activities, breaches of confidentiality, and increased use of substances not included in the drug testing panel used [36]. Similarly, although home urine drug tests are commercially available for purchase from, for example, drugstores and online marketplaces, use of these ‘over-the-counter’ home tests by parents without the guidance of a clinician is not recommended due to the complexities in interpreting results [7]. (Use of over-the-counter drug screens is distinguished from formal drug screens collected at home under the guidance of a clinician to be sent to an approved laboratory, which is frequently recommended as part of drug treatment.) Youth involved in the criminal justice system are typically routinely drug tested and the specifics of this practice vary from state to state [8].
Practical concerns in adolescent drug testing
(1) Adolescent assent / parental consent, and confidentiality
Once a practitioner feels that drug testing (usually urine) would be helpful clinically, he or should have a careful discussion with both the adolescent and parent regarding the potential benefits (i.e., supporting reducing substance use) and the limitations of testing [7]. Any questions should be addressed, and then the clinician should communicate to the adolescent the recommendation for drug testing, emphasizing the potential benefits (confirming a history of no recent substance use, improving trust with parents, etc.). Assent should always be obtained from the adolescent, and permission to share results of any drug tests with his or her parent should be sought.
In addition to the usual privacy provisions dictated by the Health Insurance Portability and Accountability Act of 1996 (HIPAA), programs providing substance use diagnosis, treatment, or referral for treatment are subject to stricter confidentiality requirements under federal regulations [9]. These regulations are contained in Volume 42 of the Code of Federal Regulations, Part 2 (42 CFR Part 2) – often referred to by practitioners as “Part 2” provisions. Whereas under HIPAA, personal health information can be disclosed among an adolescent’s providers without written consent if done as part of routine clinical care, Part 2 requires written permission from the adolescent patient for any disclosure. As always, if emergent clinical care for the adolescent is required, consent is implied and written permission need not be obtained. Many readers of this chapter are unlikely to be affected by Part 2 regulations.
The age at which an adolescent can independently seek, consent for, and receive substance use treatment services varies from state to state [37]. In some cases, a minor’s emotional, social and cognitive maturity is considered in addition to chronologic age. Moreover, whether an adolescent’s parent must by law be notified once the adolescent has consented for treatment varies across states. Readers are encouraged to seek out regulations in their own states; the National District Attorneys Association (NDAA) compiles a list of relevant state laws and regulations that providers can review [38].
(2) Test selection and timing
The clinician should also carefully consider what tests should be included in a drug screen. The SAMHSA-5, though widely available, notably misses a number of commonly used substances, including alcohol, opioids and synthetic cannabinoids, among other drugs and their metabolites [39]; clinicians should ensure that the laboratory they work with is able to broadly test for these commonly used substances. The SAMHSA-5 also tests for certain substances that are not commonly used in many places in the US. An example is phencyclidine (PCP), which is included in the SAMHSA-5 despite very low prevalence of use in most settings. In fact, where prevalence is low, a positive PCP screen is likely to be false, having been triggered by cross-reactivity by with another compound (e.g., dextromethorphan, a component of many cough syrups, is often implicated; even though technically a false positive, such a result may indicate misuse of cold medications) [40].
For adolescents who use marijuana, metabolites are detected in the urine for longer than for other substances owing to the fat solubility of cannabinoids. For intermittent users, metabolites can be detected in the urine for up to one week after last use; for daily users, they can be detected for up to one month [13]. For adolescents who drink alcohol, urine ethyl glucoronide (ETG) and ethyl sulfate (ETS) are helpful tests with a window of detection of several days. Liver tests, such as asparate aminotransferase (AST), alanine aminotransferase (ALT), and gamma-glutamyl transferase (GGT) also are also somewhat sensitive to alcohol use, but have poor specificity thus limiting their use [41]. Carbohydrate-deficient transferrin (CDT) is a more specific marker for ongoing heavy alcohol use, but requires drinking in excess of 40 g/day of ethanol for several weeks (approximately 3 standard drinks/day), and may not accurately detect intermittent heavy drinking.
Random drug testing is preferred to scheduled drug testing [8]. Since the window of detection for most substances varies between 1 to 3 days, adolescents who hope to evade detection on a drug test simply need to abstain from substance use for several days beforehand (though a longer period of abstinence is required for marijuana, as highlighted above). Random testing entails notifying the adolescent (or preferably, the adolescent’s parent or guardian) of an immediate testing time. Carefully counseling the adolescent and his or her family beforehand about the expectation to immediately complete random drug tests as part of the treatment plan is essential. Random tests should occasionally be done on consecutive days to avoid drug use immediately after testing.
(3) Specimen collection
Proper specimen collection procedures are critical for ensuring an adequate urine sample for drug testing. The internet provides advice on a host of mechanisms for defeating urine drug tests that range from simple to sophisticated. A survey of practicing pediatricians found that while the large majority have ordered urine drug tests for an adolescent patient, most often these tests are collected without supervision, making it relatively easy for an adolescent to defeat a test [11].
The most easily accomplished methods for tampering with a urine sample are adding water or other fluids or substituting a previously collected sample. Simple specimen validity checks (described below) can identify most samples that have been adulterated. Nonetheless, supervised sample collection is recommended to discourage tampering and increase the utility of testing.
The DOT describes two adequate methods for collecting a urine sample for drug testing [12]. For most routine workplace testing with adults, a collection protocol is used that does not involve direct observation. In this protocol, urine samples are collected in a private bathroom without running water, soap, or other liquids, and with toilet water stained blue. No outer clothing, bags or brief cases are permitted in the bathroom. The sample is checked for temperature immediately after it is produced. While effective, this protocol is expensive to implement and monitor. Some commercial laboratories may offer this service, though it must be ordered separately and adds significant expense to the cost of a test, which may not be covered by insurance.
An alternative acceptable collection method requires direct observation of the specimen as it is being produced. This method is more invasive, though is simpler and does not require a specialized bathroom. This alternate collection protocol is often not practical in a clinical office.
For adolescents receiving treatment for substance use problems or disorders, urine specimens can be collected at home under the supervision of a parent or guardian. First morning specimens are recommended because the bladder is reliably full and urine is most concentrated. Random, unannounced tests are difficult to prepare for and repeated testing over several weeks is likely to detect ongoing use. A series of negative drug tests over several weeks provide strong support for a report of abstinence. Thus home urine collection may be a reasonable mechanism for monitoring an adolescent that is receiving treatment for a substance use disorder.
While urine specimens may be collected at home, it is recommended that all urine drug tests be coordinated with a medical professional and only ordered in the context of an appropriate clinical indication. As noted earlier, the AAP recommends against suspicionless drug testing – whether at home, school, medical offices or in other settings – because these tests provide little useful clinical information and may cause tension between an adolescent and parents, school administrators, physicians, or other adults. Furthermore, the AAP discourages physicians from recommending drug tests for home use interpreted by families because they rely on relatively non-specific and insensitive enzyme linked panels and may generate false-positive and false-negative results. (Again, this is distinguished from home collection of drug tests to be sent to a laboratory for formal interpretation under the guidance of a clinician in a substance use treatment program, which is commonly indicated.)
(4) Specimen validation
Regardless of collection procedures, validity checks are recommended for all urine specimens. The DOT recommends checking temperature, creatinine and specific gravity on every urine sample [12]. Temperature is checked immediately after voiding. Urine specimen cups with temperature strips that fluoresce between 90 and 100 degrees Fahrenheit facilitate temperature validation. Urine creatinine and specific gravity can be ordered together with a drug test panel. Many commercial labs also offer adulterant panels that can detect many substances added to a test in vitro.
Creatinine is a product of muscle metabolism that can be used as a marker of urine concentration. According to DOT guidelines, urine samples with a random creatinine between 2 and 20 mg/mL should be considered dilute; a specimen with a creatinine less than 2 mg/mL should be considered substituted (i.e., not urine) or artificially diluted (i.e., water has been added) [12]. Since adolescence is the period in life during which muscle mass is greatest, this creatinine range may need to be adjusted for larger teens. For example, a specimen with a creatinine between 20 and 50 mg/mL may be considered dilute if the specific gravity is also low.
A dilute specimen suggests that a teen has recently consumed a large volume of fluid. This may occur incidentally or intentionally in attempt to drive the concentration of a drug or metabolite below the detection level of the test. It is not possible to distinguish between these possibilities based on the results of a urine test alone, and clinical correlation is advised whenever interpreting negative drug test. Repeat drug testing may be warranted using first morning specimens if possible. A dilute urine sample can still be positive, although in such cases it is possible to miss other substances present in lower concentrations. For example, a urine specimen may be positive for marijuana but too dilute to identify low levels of cocaine.
(5) Interpretation of results
As with all laboratory tests, urine drug tests can yield false positive and false negative results. Unlike most other laboratory results, however, results of urine drug tests can be accurate and still yield misleading information – in other words a test can yield a true negative result in the context of ongoing psychoactive substance use (e.g., if the test was performed outside the window of detection of the drug that the adolescent was using), or a true positive result in the context of no use of psychoactive substances (e.g., if the test detects substances found in food such as poppy seeds, which can trigger an opioid screen, or in a patient’s prescribed medications such as stimulants for ADHD, which can trigger an amphetamine screen). Urine drug tests may also yield ambiguous results if a test is too dilute for interpretation, or does not match a patient’s stated history. Because of their differing properties, different interpretation strategies are required for IA screening tests as compared to confirmatory GC-MS tests.
a. Interpretation of IA tests
Enzyme-linked IA tests are relatively quick, inexpensive, and easy to perform and as such are often used by laboratories as a first line screen. This testing format identifies drugs or metabolites above a certain threshold concentration in the urine. Typically the threshold concentration is set high enough to limit detection of low levels of drugs or metabolites that may be found in foods. For example, poppy seeds contain very low levels of morphine that can be detected by sensitive tests, but under usual circumstances concentrations of morphine in the blood and urine from consuming typical amounts of poppy seeds will be well under the detection threshold.
IA is non-specific and cross-reactions can occur. As an example, quinolone antibiotics can cross react with an opioid panel yielding a false positive test result. To eliminate this type of error, IA tests should be confirmed with a more definitive chromatographic test (e.g., GC-MS), particularly if a test result is unexpected and does not correlate with a patient’s history.
b. Interpretation of confirmatory chromatography tests
Chromatographic tests generally take longer to perform, are more labor intensive and more expensive than IA, though newer technologies may address these issues. Chromatographic tests are specific and are not susceptible to cross-reactions, thus false positive results are rare. However, chromatographic tests can detect prescribed medications (such as stimulants used for ADHD treatment) and it is impossible to distinguish whether a patient used the medication as prescribed or misused it by using more than prescribed or using an alternate route of administration (e.g., crushing and snorting pills).
c. Interpretation of negative tests
Whether IA or chromatographic testing is preformed, special consideration should be given to the interpretation of negative tests. A drug test will be negative despite ongoing drug use in four different circumstances:
The window of detection has passed. The window of detection for most substances is 2-3 days and drug use will not be detected after this period. One notable exception is heavy, chronic use of cannabis, which can result in prolonged excretion for up to 4 weeks [14], complicating interpretation during this period.
The patient has used a substance not detected by the testing panel. While nearly any substance can be tested for in urine, standard test panels are limited to commonly used substances. For example, synthetic cannabinoids are not detected by standard tests for cannabis and should be ordered separately if use is suspected. Inhalants are excreted by the lungs and cannot be detected in a urine specimen.
The concentration of the substance is below the detection limit of the test. This is uncommon with chromatographic tests which are typically very sensitive, but may occur with IA tests which have a set cut-off threshold typically designed to eliminate false positives from cross-reaction or trace amounts of a drug or metabolite that may be found in food products. Intentional urine dilution may result in a falsely negative test.
The specimen has been substituted or adulterated. Distinct from most instances of laboratory medicine, patients may be motivated to falsify test results by substituting or adulterating specimens. Proper specimen collection techniques (see above), use of temperature testing, and adulterant panels can minimize opportunities for interfering with testing in this way.
d. Presenting drug test results to adolescents
Reviewing positive urine drug test results presents the simultaneous challenges of sharing relevant information while maintaining a therapeutic alliance with an adolescent patient and his or her family. Prior to ordering a drug test, a discussion of how results will be reported and to whom can help maximize the utility of drug testing.
In most instances it is useful to have a private conversation with the adolescent to clarify interpretation of the drug test result. Simply sharing that the drug test yielded an “unexpected result” without revealing specific details may set the stage for an honest conversation about substance use, and at times, patients will reveal use of substances that were not detected by the test. If the patient gives a history that is consistent with the drug test results the conversation can move on to a discussion of next steps – which could include changes to the treatment plan. Sharing drug test results together with a plan may facilitate a positive conversation. For example, a clinician may report to a parent that their son has recently used marijuana and has now agreed to speak with a counselor about anxiety and marijuana use.
When a drug test result is dilute or otherwise ambiguous a clinical interview may be helpful. Starting with a simple statement about an “unexpected test result” without revealing all of the details can serve as an open-ended way of beginning the conversation. If a patient does not report substance use the clinician can review methods for reducing the chance of a dilute specimen – by providing a first morning urine if possible, or if not, limiting water intake in the hour prior to giving a sample. Repeat testing may be useful.
During a clinical interview an adolescent may offer an explanation that is consistent with the observed drug test results, such as a new prescription medication or supervised use of cold medication. This history can be confirmed with a parent and the drug test can be interpreted as negative (i.e., consistent with a history of no illicit substance use).
In some instances an adolescent’s history may be inconsistent with observed drug test results. As with all laboratory testing, drug test results provide limited information and clinical correlation is always advised. A single positive drug test may be spurious and can be treated that way if the patient otherwise seems to be doing well and adhering to the treatment plan. In these cases repeat urine testing is recommended; a second occurrence of a positive drug test is unlikely to be another false-positive result. In this case, the clinician may recommend modifications to the treatment plan.
Conclusion
Drug testing, when carefully collected and thoughtfully interpreted, offers a critical adjunct to clinical care and substance use treatment (Box 1). However, because test results can be misleading if not interpreted in the correct clinical context, clinicians should always conduct a careful interview with adolescent patients to understand what testing is likely to show and then use testing to validate or refute their expectations. Due to the ease with which samples can be tampered, providers should also carefully reflect on their own collection protocols and sample validation procedures to ensure optimal accuracy.
Box 1. Suggested Further Reading.
American Society for Addiction Medicine. Drug Testing: A White Paper of the American Society of Addiction Medicine (ASAM). Chevy Chase, MD: 2013.
Levy S, Siqueira LM, Ammerman SD, et al. Testing for drugs of abuse in children and adolescents. Pediatrics 2014;133:e1798–807.
Substance Abuse and Mental Health Services Administration. Clinical Drug Testing in Primary Care. Technical Assistance Publication (TAP) 32. HHS Publication No. (SMA) 12-4668. Rockville, MD: 2012.
Warner E, Lorch E. Laboratory Diagnosis. In: Ries RK, Fiellin DA, Miller SC, et al., editors. ASAM Princ. Addict. Med. 5th ed., Philadelphia, PA: 2014
Key Points.
Routine laboratory testing of adolescents, whether in primary care, school or at home is not recommended though testing may be useful in a number of clinical situations.
Laboratory testing is complex and requires careful attention to specimen collection and interpretation of results.
As with all laboratory testing, drug testing offers limited information and should always be interpreted in a clinical context.
Acknowledgments
Dr. Hadland is supported by the Division of Adolescent and Young Adult Medicine at Boston Children’s Hospital and the Leadership Education in Adolescent Health Training Program T71 MC00009 (MCH/HRSA) and by a National Research Service Award 1T32 HD075727 (NIH/NICHD). Dr. Levy is supported by 1R01AA021913–01 (NIH/NIAAA).
Footnotes
Conflict of Interest Statement
The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Moyer VA. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: U.S. preventive services task force recommendation statement. Ann Intern Med. 2013;159:210–8. doi: 10.7326/0003-4819-159-3-201308060-00652. [DOI] [PubMed] [Google Scholar]
- 2.National Institute on Alcohol Abuse and Alcoholism. Alcohol Screening and Brief Intervention for Youth: A Practitioner’s Guide. Bethesda, MD: 2011. [Google Scholar]
- 3.Higgins-Biddle J, Hungerford D, Cates-Wessel K. Screening and Brief Interventions (SBI) for Unhealthy Alcohol Use: A Step-by-Step Implementation Guide for Trauma Centers. Atlanta, GA: 2009. [Google Scholar]
- 4.Levy SJ, Kokotailo PK. Substance use screening, brief intervention, and referral to treatment for pediatricians. Pediatrics. 2011;128:e1330–40. doi: 10.1542/peds.2011-1754. [DOI] [PubMed] [Google Scholar]
- 5.Levy S. Effects of marijuana policy on children and adolescents. JAMA Pediatr. 2013;167:600–2. doi: 10.1001/jamapediatrics.2013.2270. [DOI] [PubMed] [Google Scholar]
- 6.Hagan JF, Shaw JS, Duncan PM. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. (3) Available at: http://brightfutures.aap.org/3rd_Edition_Guidelines_and_Pocket_Guide.html.
- 7.Levy S, Siqueira LM, Ammerman SD, et al. Testing for drugs of abuse in children and adolescents. Pediatrics. 2014;133:e1798–807. doi: 10.1542/peds.2014-0865. [DOI] [PubMed] [Google Scholar]
- 8.American Society for Addiction Medicine. Drug Testing: A White Paper of the American Society of Addiction Medicine (ASAM) Chevy Chase, MD: 2013. [Google Scholar]
- 9.Substance Abuse and Mental Health Services Administration. Clinical Drug Testing in Primary Care Technical Assistance Publication (TAP) 32 HHS Publication No (SMA) 12-4668. Rockville, MD: 2012. [Google Scholar]
- 10.National Center on Substance Abuse and Child Welfare / Substance Abuse and Mental Health Services Administration. [October 10, 2015];Drug Testing Practice Guidelines. Available at: https://ncsacw.samhsa.gov/files/IA_Drug_Testing_Bench_Card_508.pdf.
- 11.Levy S, Harris SK, Sherritt L, et al. Drug testing of adolescents in ambulatory medicine: physician practices and knowledge. Arch Pediatr Adolesc Med. 2006;160:146–50. doi: 10.1001/archpedi.160.2.146. [DOI] [PubMed] [Google Scholar]
- 12.Jones RK, Shinar D, Walsh JM. Detection and Measurement of Drugs State Knowl Drug-Impaired Driving, NHTSA Rep DOT HS 809 642. Washington, DC: US National Highway Traffic Safety Administration; 2003. [Google Scholar]
- 13.Grotenhermen F. Pharmacokinetics and pharmacodynamics of cannabinoids. Clin Pharmacokinet. 2003;42:327–60. doi: 10.2165/00003088-200342040-00003. [DOI] [PubMed] [Google Scholar]
- 14.Schwilke EW, Gullberg RG, Darwin WD, et al. Differentiating new cannabis use from residual urinary cannabinoid excretion in chronic, daily cannabis users. Addiction. 2011;106:499–506. doi: 10.1111/j.1360-0443.2010.03228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cone EJ. New Developments in Biological Measures of Drug Prevalence. In: Harrison L, Hughes A, editors. Validity Self-Reported Drug Use Improv Accuracy Surv Estim. Bethesda, MD: National Institute on Drug Abuse; 1997. [Google Scholar]
- 16.Dams R, Choo RE, Lambert WE, et al. Oral fluid as an alternative matrix to monitor opiate and cocaine use in substance-abuse treatment patients. Drug Alcohol Depend. 2007;87:258–67. doi: 10.1016/j.drugalcdep.2006.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bosker WM, Huestis MA. Oral Fluid Testing for Drugs of Abuse. Clin Chem. 2009;55:1910–31. doi: 10.1373/clinchem.2008.108670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drummer OH. Drug testing in oral fluid. Clin Biochem Rev. 2006;27:147–59. [PMC free article] [PubMed] [Google Scholar]
- 19.Boumba V, Ziavrou K, Vougiouklakis T. Hair as a Biological Indicator of Drug Use, Drug Abuse or Chronic Exposure to Environmental Toxicants. Int J Toxicol. 2006;25:143–63. doi: 10.1080/10915810600683028. [DOI] [PubMed] [Google Scholar]
- 20.Dolan K, Rouen D, Kimber J. An overview of the use of urine, hair, sweat and saliva to detect drug use. Drug Alcohol Rev. 2004;23:213–7. doi: 10.1080/09595230410001704208. [DOI] [PubMed] [Google Scholar]
- 21.Warner E, Lorch E. Laboratory Diagnosis. In: Ries RK, Fiellin DA, Miller SC, et al., editors. ASAM Princ Addict Med. 5. Philadelphia, PA: 2014. [Google Scholar]
- 22.Pragst F, Balikova MA. State of the art in hair analysis for detection of drug and alcohol abuse. Clin Chim Acta. 2006;370:17–49. doi: 10.1016/j.cca.2006.02.019. [DOI] [PubMed] [Google Scholar]
- 23.Henderson GL, Harkey MR, Zhou C, et al. Incorporation of isotopically labeled cocaine and metabolites into human hair: 1. dose-response relationships. J Anal Toxicol. 20:1–12. doi: 10.1093/jat/20.1.1. [DOI] [PubMed] [Google Scholar]
- 24.Ropero-Miller JD, Huestis MA, Stout PR. Cocaine analytes in human hair: evaluation of concentration ratios in different cocaine sources, drug-user populations and surface-contaminated specimens. J Anal Toxicol. 2012;36:390–8. doi: 10.1093/jat/bks050. [DOI] [PubMed] [Google Scholar]
- 25.Dasgupta A. Handbook of Drug Monitoring Methods: Therapeutics and Drugs of Abuse. Totowa, NJ: 2008. [Google Scholar]
- 26.Pötsch L, Skopp G, Moeller MR. Influence of pigmentation on the codeine content of hair fibers in guinea pigs. J Forensic Sci. 1997;42:1095–8. [PubMed] [Google Scholar]
- 27.US Department of Transporation. [October 4, 2015];Approved Evidential Breath Testing Devices. Available at: https://www.transportation.gov/odapc/approved-evidential-breath-testing-devices.
- 28.Concheiro M, Jones HE, Johnson RE, et al. Maternal buprenorphine dose, placenta buprenorphine, and metabolite concentrations and neonatal outcomes. Ther Drug Monit. 2010;32:206–15. doi: 10.1097/FTD.0b013e3181d0bd68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gray T, Huestis M. Bioanalytical procedures for monitoring in utero drug exposure. Anal Bioanal Chem. 2007;388:1455–65. doi: 10.1007/s00216-007-1228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hudak ML, Tan RC. Neonatal Drug Withdrawal. Pediatrics. 2012;129:e540–60. doi: 10.1542/peds.2011-3212. [DOI] [PubMed] [Google Scholar]
- 31.Stanger C, Budney AJ. Contingency management approaches for adolescent substance use disorders. Child Adolesc Psychiatr Clin N Am. 2010;19:547–62. doi: 10.1016/j.chc.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hartzler B, Lash SJ, Roll JM. Contingency management in substance abuse treatment: a structured review of the evidence for its transportability. Drug Alcohol Depend. 2012;122:1–10. doi: 10.1016/j.drugalcdep.2011.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shearer J, Tie H, Byford S. Economic evaluations of contingency management in illicit drug misuse programmes: A systematic review. Drug Alcohol Rev. 2015;34:289–98. doi: 10.1111/dar.12240. [DOI] [PubMed] [Google Scholar]
- 34.Dennis M, Godley SH, Diamond G, et al. The Cannabis Youth Treatment (CYT) Study: main findings from two randomized trials. J Subst Abuse Treat. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 35.Drug & Alcohol Testing Industry Association. [October 12, 2015];Ultimate Guide to State Drug Testing Laws. Available at: http://www.datia.org/publications/ultimate-guide-to-state-drug-testing-laws.html.
- 36.Levy S, Schizer M. Adolescent Drug Testing Policies in Schools. Pediatrics. 2015;135:782–3. doi: 10.1542/peds.2015-0055. [DOI] [PubMed] [Google Scholar]
- 37.Center for Substance Abuse Treatment. Substance Abuse and Mental Health Administration. Rockville, MD: 1999. Chapter 8—Legal and Ethical Issues. [Google Scholar]
- 38.National District Attorneys Association. [September 25, 2015];Minor Consent to Medical Treatment Laws. Available at: http://www.ndaa.org/pdf/Minor Consent to Medical Treatment (2).pdf.
- 39.Johnston LD, O’Malley PM, Miech RA, et al. Monitoring the Future National Results on Drug Use: 2014 Overview. Key Findings on Adolescent Drug Use [Google Scholar]
- 40.Rengarajan A, Mullins ME. How often do false-positive phencyclidine urine screens occur with use of common medications? Clin Toxicol. 2013;51:493–6. doi: 10.3109/15563650.2013.801982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nanau RM, Neuman MG. Biomolecules and Biomarkers Used in Diagnosis of Alcohol Drinking and in Monitoring Therapeutic Interventions. Biomolecules. 2015;5:1339–85. doi: 10.3390/biom5031339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Warner E. Princ Addict Med. 3. Chevy Chase, MD: American Society of Addiction Medicine; 2003. Laboratory Diagnosis; pp. 337–48. [Google Scholar]
- 43.Center for Substance Abuse Treatment. The Role of Biomarkers in the Treatment of Alcohol Use Disorders. Rockville, MD: 2006. [Google Scholar]
- 44.Kwong TC, Ryan RM. Detection of intrauterine illicit drug exposure by newborn drug testing. National Academy of Clinical Biochemistry. Clin Chem. 1997;43:235–42. [PubMed] [Google Scholar]


