Abstract
Objectives
Our objective was to predict the knee extension strength and post-operative function in quadriceps resection for soft-tissue sarcoma of the thigh.
Methods
A total of 18 patients (14 men, four women) underwent total or partial quadriceps resection for soft-tissue sarcoma of the thigh between 2002 and 2014. The number of resected quadriceps was surveyed, knee extension strength was measured with the Biodex isokinetic dynamometer system (affected side/unaffected side) and relationships between these were examined. The Musculoskeletal Tumor Society (MSTS) score, Toronto Extremity Salvage Score (TESS), European Quality of Life-5 Dimensions (EQ-5D) score and the Short Form 8 were used to evaluate post-operative function and examine correlations with extension strength. The cutoff value for extension strength to expect good post-operative function was also calculated using a receiver operating characteristic (ROC) curve and Fisher’s exact test.
Results
Extension strength decreased when the number of resected quadriceps increased (p < 0.001), and was associated with lower MSTS score, TESS and EQ-5D (p = 0.004, p = 0.005, p = 0.006, respectively). Based on the functional evaluation scales, the cutoff value of extension strength was 56.2%, the equivalent to muscle strength with resection of up to two muscles.
Conclusion
Good post-operative results can be expected if at least two quadriceps muscles are preserved.
Cite this article: A. Tanaka, Y. Yoshimura, K. Aoki, M. Kito, M. Okamoto, S. Suzuki, T. Momose, H. Kato. Knee extension strength and post-operative functional prediction in quadriceps resection for soft-tissue sarcoma of the thigh. Bone Joint Res 2016;5:232–238. DOI: 10.1302/2046-3758.56.2000631.
Keywords: Soft-tissue sarcoma, Quadriceps muscle, Muscle strength, Post-operative function, Prediction
Article focus
The purpose of this study was to clarify pre-operative predictors for post-operative function and the extent of resection necessary for good post-operative results in quadriceps resection for soft-tissue sarcoma of the thigh.
Key messages
When estimating post-operative muscle strength and function, the number of muscles resected could be a useful pre-operative predictor.
If continuity of at least two muscles are preserved, a functional level not causing significant difficulty with activities can be expected.
Strengths and limitations
Strength: The results of the present study could help to predict post-operative function after quadriceps resection in more detail and enable surgeons to provide patients with concrete post-operative expectations.
Limitation: A larger sample size may be needed to compare the results of multiple-muscle resection adequately.
Introduction
Soft-tissue sarcomas often occur on the thigh and are frequently observed in the anterior compartment.1 They are usually treated with surgery and require wide resection. Therefore, partial or total quadriceps resection for soft-tissue sarcoma in the anterior compartment of the thigh can reduce knee extension strength and decrease post-operative function. Various factors can affect declining strength, such as which and how many muscles are resected. The extent of resection for good post-operative results in quadriceps resection for soft-tissue sarcoma of the thigh is unclear.
In the present study, we used an isokinetic dynamometer to objectively evaluate knee extension strength after surgery for soft-tissue sarcoma in the anterior compartment of the thigh, and investigated factors affecting post-operative extension strength. We also examined correlations between extension strength and the results of four functional evaluations of activities of daily living (ADL) and quality of life (QOL). Furthermore, we introduce a pre-operative predictor for post-operative function based on the extent of resection.
Patients and Methods
A total of 29 patients with soft-tissue sarcoma in the anterior compartment of the thigh underwent partial or total quadriceps resection at our hospital between 2002 and 2014. After excluding the following patients: those with subcutaneous tumours; those who underwent extensor reconstructive surgery; and those who had died, were terminal, or were undergoing chemotherapy at the time of the survey: 18 patients remained. We reviewed these patients’ medical records to determine age at final follow-up, follow-up period, tumour site, maximum tumour diameter, number of resected quadriceps, type of resected quadriceps, pathology type, adjuvant therapy and time from final adjuvant therapy to measurement. Knee extension strength was measured and post-operative function was evaluated at the final observation point. Factors affecting post-operative extension strength were investigated and correlations between knee extension strength and post-operative functional evaluations were examined. Based on these results, we calculated a cutoff value for extension strength to expect good post-operative results. This study was approved by our hospital’s ethics committee, and all patients provided informed consent.
Complete excision of a muscle’s continuity was counted as one muscle and resection of a muscle with continuity maintained was counted as 0.5 muscles. Femoral nerve trunk resection was considered to be a four-muscle resection. The tumour site was considered proximal or distal based on which half of the thigh the tumour was on, or middle when the tumour extended over both halves. The Biodex System 4 isokinetic dynamometer (Biodex Medical Systems, Inc., Shirley, New York) was used to measure muscle strength. Isokinetic movements were performed by moving the knee from 90º flexion to 0º extension five times in succession at 60º per second. The affected and unaffected sides were both measured twice, and the maximum values on each side were used to calculate the ratio of the affected side to the unaffected side (%). All measurements were performed under the same conditions by the same physical therapist, who was blinded to the number of muscles resected.
The Musculoskeletal Tumor Society (MSTS) score2 was used to evaluate post-operative function; Toronto Extremity Salvage Score (TESS) to evaluate ADL;3,4 and European Quality of Life-5 Dimensions (EQ-5D)5,6 and Short Form 8 (SF-8),7 to evaluate QOL. Acceptable results were defined as ⩾ 80% for MSTS score8 and TESS, and ⩾ 0.800 for EQ-5D. The cutoff value for extension strength was the point where acceptable results could be expected. The parameters of SF-8 were compared with the national standard value of 50 points in Japan.7
Differences between median values were examined with the Mann-Whitney U test, correlations between two variables with Spearman’s rank correlation coefficients and cutoff values with a receiver operating characteristic (ROC) curve and Fisher’s exact test. Statistically significant differences were defined as p < 0.05. Data were analysed with IBM SPSS Statistics version 21 (IBM Corp., Armonk, New York).
Results
Median age at final follow-up of the 18 patients (14 men, four women) was 62.0 years (interquartile range (IQR), 57.5 to 73.8). Median follow-up period was 46.0 months (IQR 19.0 to 78.5). Chemotherapy and radiation therapy were performed in six and five patients, respectively and median time from final adjuvant therapy to measurement was 60.0 months (IQR 19.0 to 88.3). The demographic and clinical characteristics of the 18 eligible patients are presented in Tables I and II.
Table I.
Details of 18 patients with quadriceps resection for soft-tissue sarcoma of the thigh
| Patient number | Gender | Age (yrs) | Follow-up period (mths) | Tumour site | Maximum tumour diameter (mm) | Resected muscles | Quadriceps resections (n) | Extension strength (%) | MSTS score (%) | TESS(%) | EQ-5D(pts) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 66 | 123 | distal | 120 | VL,TFL,BL,BS | 1 | 91.3 | 100 | 100 | 1.000 |
| 2 | M | 85 | 19 | proximal | 114 | RF,IP,S,TFL | 1 | 89.7 | 86.7 | 93.7 | 1.000 |
| 3 | M | 60 | 136 | distal | 60 | VM | 1 | 82.9 | 100 | 100 | 1.000 |
| 4 | M | 74 | 85 | distal | 200 | VI | 1 | 69.9 | 93.3 | 75.9 | 0.691 |
| 5 | F | 57 | 18 | proximal | 113 | RF | 1 | 79.4 | 100 | 100 | 1.000 |
| 6 | F | 66 | 60 | distal | 60 | VM | 1 | 91.2 | 86.7 | 99.1 | 0.769 |
| 7 | M | 75 | 45 | distal | 56 | VL,VI1/2 | 1.5 | 52.6 | 70.0 | 60.6 | 0.516 |
| 8 | M | 63 | 34 | distal | 81 | VM,VI1/2,S | 1.5 | 65.2 | 100 | 100 | 1.000 |
| 9 | M | 60 | 80 | proximal | 78 | VL,VI1/2,TFL | 1.5 | 52.2 | 86.7 | 72.0 | 0.656 |
| 10 | M | 34 | 124 | distal | 50 | RF,VL1/2 | 1.5 | 56.2 | 90.0 | 90.1 | 0.850 |
| 11 | F | 59 | 21 | proximal | 94 | RF1/2,VL,TFL | 1.5 | 32.6 | 50.0 | 89.8 | 0.796 |
| 12 | M | 34 | 19 | distal | 61 | VM,VI1/2 | 1.5 | 71.7 | 96.7 | 100 | 0.796 |
| 13 | M | 76 | 12 | proximal | 132 | RF,VL1/2,GMe1/2,S,TFL | 1.5 | 60.0 | 73.3 | 80.0 | 0.691 |
| 14 | M | 61 | 74 | proximal | 107 | RF,VL | 2 | 58.4 | 96.7 | 98.2 | 1.000 |
| 15 | M | 74 | 47 | proximal | 110 | RF,VM,VI1/2, S,G,AM,AL,AB | 2.5 | 53.3 | 70.0 | 62.5 | 0.533 |
| 16 | F | 73 | 73 | middle | 140 | VM,VL,VI,TFL | 3 | 24.8 | 53.3 | 86.1 | 0.631 |
| 17 | M | 57 | 15 | proximal | 150 | RF,VM,VL,VI,S,TFL | 4 | 0 | 73.3 | 75.0 | 0.693 |
| 18 | M | 50 | 12 | proximal | 100 | RF,VL1/2,VI2/3,FN,IP,S | 4 (FN) | 0 | 73.3 | 78.3 | 0.587 |
VL, vastus lateralis; TFL, tensor fasciae latae; BL, biceps femoris long head; BS, biceps femoris short head; RF, rectus femoris; IP, iliopsoas; S, sartorius; VM, vastus medialis; VI, vastus intermedius; GMe, gluteus medius; G, gracilis; AM, adductor magnus; AL, adductor longus; AB, adductor brevis; FN, femoral nerve; MSTS, Musculoskeletal Tumor Society; TESS, Toronto Extremity Salvage Score; EQ-5D, European Quality of Life-5 Dimensions
Table II.
Pathology type and adjuvant therapy
| Patient number | Pathology type | Chemotherapy | Radiation therapy | Time from final adjuvant therapy to measurement (mths) |
|---|---|---|---|---|
| 1 | Malignant fibrous histiocytoma | + | + | 121 |
| 2 | Pleomorphic liposarcoma | - | - | |
| 3 | Malignant fibrous histiocytoma | + | - | 85 |
| 4 | Dedifferentiated liposarcoma | - | + | 83 |
| 5 | Liposarcoma | - | - | |
| 6 | Low-grade fibromyxoid sarcoma | - | - | |
| 7 | Synovial sarcoma | - | - | |
| 8 | Inflammatory myofibroblastic sarcoma | - | - | |
| 9 | Myxofibrosarcoma | + | - | 37 |
| 10 | Malignant peripheral nerve sheath tumour | + | + | 98 |
| 11 | Undifferentiated pleomorphic sarcoma | + | + | 20 |
| 12 | Undifferentiated pleomorphic sarcoma | + | - | 16 |
| 13 | Myxofibrosarcoma | - | - | |
| 14 | Myxofibrosarcoma | - | - | |
| 15 | Myxofibrosarcoma | - | - | |
| 16 | Malignant fibrous histiocytoma | - | - | |
| 17 | Dedifferentiated liposarcoma | - | + | 15 |
| 18 | Myxoid liposarcoma | - | - |
A total of six patients had one muscle resected, seven patients had 1.5 muscles resected, one patient each had two, 2.5, three and four muscles resected, and one patient had the femoral nerve trunk resected. Median extension strength was 86.3% (IQR 80.3% to 90.8%) for one muscle, 54.4% (IQR 52.4% to 62.6%) for 1.5 muscles, 58.4% for two muscles, 53.3% for 2.5 muscles, 24.8% for three muscles and 0% for four muscles. A significant difference was observed between resection of one and 1.5 muscles (Mann-Whitney test, p = 0.004; Fig. 1). Furthermore, reduced extension strength correlated with increased number of muscles resected (Spearman’s test, r = -0.87, p < 0.001; Table III).
Fig. 1.
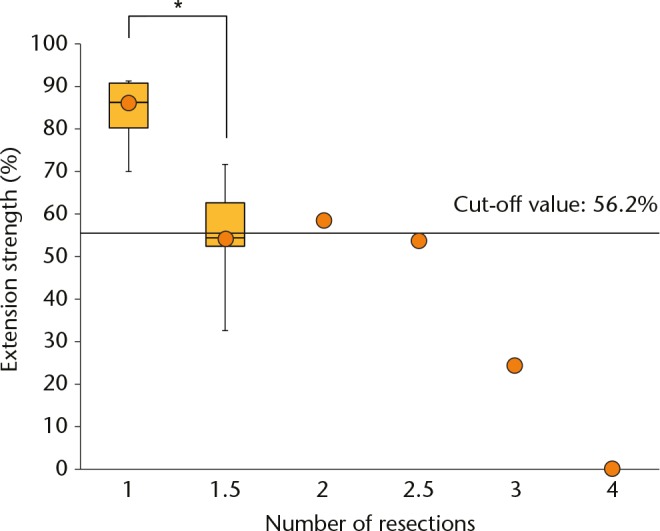
Extension strength by number of resected muscles. Dots denote median extension strength values. The solid line shows the significant difference between the resection of one and 1.5 muscles (Mann-Whitney test, *p = 0.004). The horizontal line shows the cutoff value for extension strength (56.2%) at which acceptable results can be obtained. Strength at least equivalent to the cutoff value was observed with resection of up to 2.5 muscles.
Table III.
Correlation between extension strength and various parameters by Spearman’s test
| Correlation coefficient | p-value | |
|---|---|---|
| Resection (n) | -0.87 | < 0.001* |
| Maximum tumour diameter | -0.08 | 0.730 |
| Functional assessment scores | ||
| MSTS score | 0.70 | 0.004* |
| TESS | 0.68 | 0.005* |
| EQ-5D | 0.66 | 0.006* |
Statistically significant difference
MSTS, Musculoskeletal Tumor Society; TESS, Toronto Extremity Salvage Score; EQ-5D, European Quality of Life-5 Dimensions
Extension strength for the six patients with one muscle resected was 91.3% when the vastus lateralis was resected (case 1), 82.9% and 91.2% for the vastus medialis (cases 3 and 6), 69.9% for the vastus intermedius (case 4) and 89.7% and 79.4% for the rectus femoris (cases 2 and 5). Vastus intermedius resection caused the greatest reduction in extension strength.
The median maximum tumour diameter was 103.5 mm (IQR 65.3 to 118.5). No correlation was observed between maximum tumour diameter and extension strength (Spearman’s test, r = -0.08, p = 0.730; Table III). Maximum tumour diameter when ⩾ two muscles were resected was greater than the median value. In four of the six patients who had one muscle resected, maximum diameter was greater than the median value, but muscle strength remained from 69.9% to 91.3%.
A total of nine tumours were proximal, eight were distal and one was middle. No significant difference in extension strength was observed between proximal and distal cases (Mann-Whitney test, p = 0.053). When patients with the same quadriceps resected at different sites were compared, no difference in post-operative muscle strength based on tumour site was observed when the vastus lateralis and half of the vastus intermedius were resected (cases 7 and 9) or when the rectus femoris and half of the vastus lateralis were resected (cases 10 and 13).
Functional scale median values were 86.7% (IQR 73.3% to 96.7%) for MSTS score, 90.0% (IQR 76.5% to 99.8%) for TESS, and 0.782 (IQR 0.665 to 1.000) for EQ-5D. All functional scales exhibited significant differences when compared with extension strength, with decreased extension strength associated with lower scores (Spearman’s test, MSTS score, r = 0.70, p = 0.004; TESS, r = 0.68, p = 0.005; EQ-5D, r = 0.66, p = 0.006; Table III).
Correlations between reduced extension strength and reduced function occurred in 21 of 30 TESS items. No correlations were observed for the other nine items, with functional decline not linked to reduced extension strength (Spearman’s test; Table IV).
Table IV.
Correlation between extension strength and Toronto Extremity Salvage Score (TESS) items by Spearman’s test
| TESS items | |
|---|---|
| 1) Putting on a pair of pants* | 16) Walking downstairs* |
| 2) Putting on shoes* | 17) Driving* |
| 3) Putting on socks or stockings* | 18) Walking within the house |
| 4) Showering | 19) Walking outdoors* |
| 5) Light household chores | 20) Sitting |
| 6) Gardening and yard work* | 21) Walking up or down hills or a ramp* |
| 7) Preparing and serving meals* | 22) Standing upright |
| 8) Going shopping* | 23) Getting up from kneeling* |
| 9) Heavy household chores* | 24) Getting in and out of a car* |
| 10) Getting in and out of the bath tub* | 25) Participating in sexual activities |
| 11) Getting out of bed* | 26) Completing my usual duties at work* |
| 12) Rising from a chair* | 27) Working my usual number of hours |
| 13) Kneeling* | 28) Participating in my usual leisure activities* |
| 14) Bending to pick something up off the floor* | 29) Socialising with friends and family |
| 15) Walking upstairs* | 30) Participating in my usual sporting activities |
Statistically significant difference
For SF-8, median values for the physical scales of physical functioning (PF), role physical (RP), bodily pain (BP) and physical component summary (PCS) in the eight subscales and two summary scores were below the national standard values. Only PF score significantly declined as extension strength decreased (Spearman’s test, r = 0.50, p = 0.038). In contrast, median values for the mental scales of social functioning (SF), role emotional (RE), mental health (MH) and mental component summary (MCS) were at or above the national standard values, showing no correlations with extension strength (Table V).
Table V.
Correlation between extension strength and Short Form 8 parameters by Spearman’s test
| Median point (IQR) | Correlation coefficient | p-value | |
|---|---|---|---|
| PF | 41.5 (41.5 to 53.5) | 0.50 | 0.038* |
| RP | 47.4 (40.7 to 54.1) | 0.47 | 0.055 |
| BP | 46.1 (46.1 to 58.4) | 0.44 | 0.071 |
| GH | 50.3 (50.3 to 50.3) | 0.19 | 0.419 |
| VT | 53.7 (44.5 to 53.7) | 0.02 | 0.946 |
| SF | 55.1 (45.6 to 55.1) | 0.16 | 0.514 |
| RE | 54.2 (43.7 to 54.2) | 0.26 | 0.281 |
| MH | 50.7 (44.9 to 56.9) | 0.32 | 0.184 |
| PCS | 42.9 (42.3 to 52.1) | 0.45 | 0.062 |
| MCS | 52.7 (45.8 to 55.9) | 0.02 | 0.172 |
Statistically significant difference
PF, physical functioning; RP, role physical; BP, bodily pain; GH, general health perceptions; VT, vitality; SF, social functioning; RE, role emotional; MH, mental health; PCS, physical component summary; MCS, mental component summary
We calculated the extension strength cutoff value of MSTS score, TESS and EQ-5D to show when acceptable results could be obtained (ROC curve, Fisher’s exact test; Table VI). A cutoff value of 56.2% was obtained for all scales (sensitivity, specificity, area under the curve, and p-values, respectively, were 90.9%, 100%, 0.96 and < 0.001 for MSTS score; 81.8%, 85.7%, 0.83 and 0.009 for TESS; and 100%, 63.6%, 0.81 and 0.004 for EQ-5D). Patients with one or two muscles resected had median extension strength scores above the cutoff value; 1.5 or 2.5 muscles resected, scores equal to the cutoff value; and ⩾ three muscles resected, scores significantly below the cutoff value (Fig. 1).
Table VI.
The cutoff value of extension strength to expect good post-operative results by receiver operating characteristic curve, Fisher’s exact test
| MSTS score | TESS | EQ-5D | |
|---|---|---|---|
| Cutoff value of extension strength (%) | 56.2 | 56.2 | 56.2 |
| Sensitivity (%) | 90.9 | 81.8 | 100 |
| Specificity (%) | 100 | 85.7 | 63.6 |
| Area under the curve | 0.96 | 0.83 | 0.81 |
| p-value | < 0.001* | 0.009* | 0.004* |
Statistically significant difference
MSTS, Musculoskeletal Tumor Society; TESS, Toronto Extremity Salvage Score; EQ-5D, European Quality of Life-5 Dimensions
Discussion
When planning the resection of a soft-tissue sarcoma, predicting post-operative functional decline and providing patients with concrete explanations is important in order to increase patients’ treatment satisfaction and enthusiasm for rehabilitation. For physicians, making detailed predictions about post-operative function (ADL, QOL) could enhance goal setting and post-operative rehabilitation planning. However, most surgeons predict post-operative functions based on individual experience, partly because few studies have been published focusing on pre-operative predictors of post-operative function. Here, we reviewed cases involving the anterior compartment of the thigh, where soft-tissue sarcomas frequently occur,1 as this especially affects post-operative function. The quadriceps functions as a hip flexor and knee extensor. Although the hip flexor can be substituted by other muscles, the quadriceps is the only knee extensor and cannot be substituted. As such, we believe that knee extension strength may be more reflective of the loss of muscle strength and function due to quadriceps resection. Therefore, our retrospective study focused on knee extension strength after soft-tissue sarcoma surgery.
Various factors including number, type and amount of muscles resected, tumour site and size, age, adjuvant therapy, nerve or vessel injury, muscle atrophy, follow-up period and pre-operative muscle strength are all likely to affect post-operative muscle strength. In the present study, a significant difference was found between resection of one and 1.5 muscles; extension strength was found to decrease as more muscles were resected. Only a few reports exist on post-operative muscle strength after quadriceps resection.9,10 According to Markhede and Stener,9 residual isometric strength was 78% with one muscle resected, 67% with two muscles resected and 45% with three muscles resected. Although the authors used a different measurement method, their results resemble those of the present study, suggesting that the number of muscles resected could be a useful pre-operative indicator for post-operative muscle strength. Differences between quadriceps, including their cross section, functional anatomy (mono-, bi-articular muscles) and area of origin, likely mean that each muscle contributes differently to overall extension strength. While there are reports that post-operative muscle strength is independent of resected muscle type,9,10 electrophysiological research by Zhang et al11 and Lieb and Perry12 showed that during maximum isometric contraction, extension strength is the smallest in the vastus medialis and the greatest in the vastus intermedius. These studies obtained electrophysiological results from isometric movements, therefore they may differ somewhat from our isokinetic dynamometer results. However, the present study did obtain similar results for cases with one muscle resected.
Due to the small sample size, we could not perform statistical investigations of cases with only one muscle resected, however, single resection of the vastus intermedius is likely to affect post-operative muscle strength greatly, which we believe may lead to loss of function. Although the amount of muscle resected may influence post-operative muscle strength, precise measurement and objective comparison between cases remain difficult. Whether the amount of muscle resected is large or small, we believe that the number of muscles resected may have a greater influence on post-operative muscle strength because loss of muscle continuity results in decreased muscle strength. Although distal tumours requiring resection around the quadriceps insertions would be expected to reduce extension strength, significant differences between proximal and distal tumours were not observed in the present study. Only a few cases involved resection of the same muscles, so statistical analyses were not possible, but as no differences were observed when the same muscles were resected at different sites, extension strength might not depend on tumour site. In addition, no correlation was observed between maximum tumour diameter and extension strength. Cases in which three or four muscles were resected had large tumours, but good extension strength was maintained even with large tumours if only one muscle was resected.
Ageing reduces muscle mass and subsequently decreases muscle strength and physical performance.13 Thus, instead of comparing maximum muscle strength, which tends to create age disparity, we minimised the influence of age by drawing a comparison using the ratio of affected to unaffected sides. Adjuvant therapy, including chemotherapy and radiation therapy, may also cause muscle weakness and disuse syndrome.13 Therefore, patients who were undergoing chemotherapy at the time of measurement were excluded. Even when adjuvant therapy was performed, time from final adjuvant therapy to measurement of muscle strength was at least one year, which we believe minimised the effect.
Nerve or vessel injury and muscle atrophy also should be considered with regard to post-operative muscle strength. In the present study, except for one case of femoral nerve trunk resection, there was no denervation or muscle atrophy of residual muscle on the post-operative magnetic resonance imaging. Reports on recovery of muscle strength after femoral limb lengthening14 or shortening15,16 state that post-operative muscle strength demonstrates the greatest improvement at three months to one year,16 continues to improve at two years, but is unlikely to improve beyond two years.14-16 In addition, post-operative function has been reported to reach pre-operative levels for TESS and number of sit-to-stand repetitions at one year and for number of stairs climbed at two years.15 Although a simple comparison cannot be drawn from these reports due to performing muscle resections in the present study, we measured post-operative muscle strength and function at more than one year, at which time recovery of muscle strength is likely to have roughly plateaued. However, because the present study also includes measurements within two years of surgery, muscle strength and function may show further improvement. Thus, further prospective studies may be necessary to consider the pre-operative-to-post-operative transition.
We also investigated the effect of reduced extension strength on post-operative function using four functional evaluation scales. Ploutz-Snyder et al17 reported that the quadriceps is closely related to many ADLs, therefore reduced quadriceps strength could be a useful indicator of difficulty with daily activities. In the present study, post-operative function of the affected limb based on MSTS score and ADL evaluations based on TESS both decreased as extension strength declined. When individual TESS items were examined, functional decline was not observed in simpler movements (for example, walking within the house versus walking up and down stairs) or vague movements (for example, socialising with friends and family). However, functional decline accompanied reduced extension strength with many movements (21 items). Moreover, a study on QOL in osteosarcoma patients18 found that function of the affected limb correlated with physical but not mental QOL, and positive function of the affected limb was not always necessary for good QOL. In the present study, decreased extension strength was associated with reduced EQ-5D, which expresses QOL in one dimension. However, physical scales of SF-8 (a multidimensional evaluation) declined with reduced extension strength, although mental scales did not.
Knee extension strength correlated with physical function and QOL (particularly physical scales) after quadriceps resection. The number of muscles resected had the greatest impact on knee extension strength, indicating that it could be a useful pre-operative predictor for post-operative muscle strength and function. We also calculated a cutoff value for extension strength to show when good post-operative results could be obtained, and we estimated that the extent of resection predicted good post-operative function. Satisfactory function was obtained at an extension strength cutoff value of 56.2%. Strength remained at or above the cutoff value when up to 2.5 muscles were resected. In contrast, when ⩾ three muscles were resected, extension strength was significantly below the cutoff value. Therefore, if 56.2% of extension strength remains, a functional level not causing significant difficulties with activities can be expected. Thus, as an estimate, good results can be expected if continuity of at least two muscles is maintained.
Methods for quadriceps reconstruction include pedicled muscle transfer using the sartorius or biceps femoris and free muscle transfer using the latissimus dorsi,8,19-21 however, their indications are unclear.22 Resection of four muscles or the femoral nerve increases risk of bone fracture from falling and decreases functional evaluation scores.23 The present study obtained good results without reconstruction if ⩽ two muscles were resected. On the other hand, knee extension strength declined markedly when ⩾ three muscles were resected. In such cases, reconstruction of the extension mechanism should be considered to obtain good post-operative results. However, because satisfactory post-operative function is not necessarily guaranteed with existing reconstruction techniques,8,20,22 methods for reconstructive surgery require further investigation. We can suture the residual quadriceps to a nearby muscle and in resections of ⩾ three muscles the resection site can be reinforced using either a pedicled muscle transfer or synthetic mesh. While these procedures improve knee extension strength, cases that underwent these procedures were excluded from the present study. Further research comparing muscle strength in cases with or without reconstruction is required.
Only early post-operative rehabilitation of approximately three weeks is performed at our hospital, and patients do not participate in rehabilitation after discharge. Thus, the results of the present study reflect patients without active muscle training, which we believe may be used as a guide for setting goals for rehabilitation. Furthermore, a shorter functional recovery period may be achieved with more extensive post-operative rehabilitation.
One limitation of this study is that muscles besides the quadriceps were resected in some cases. Additionally, the number of patients varied considerably in terms of the number of muscles resected. We believe that the non-quadriceps resected muscles were not directly related to knee extension strength, but they may have affected the functional evaluations. Furthermore, as few patients had ⩾ two muscles resected, a larger sample size would be needed to compare the results of multiple-muscle resection adequately. However, muscle strength was maintained when one or 1.5 muscles were resected, and there were several such cases included. Accordingly, good results will likely be obtained if continuity of two muscles is maintained.
Bone and soft-tissue tumours occur infrequently, and the extent of resection varies between patients, which is possibly why so few research studies have been performed on pre-operative predictions of post-operative function. Nevertheless, accumulating more studies such as the present study could help predict post-operative function after quadriceps resection in more detail and enable physicians to provide patients with concrete post-operative expectations. It could also aid in devising more effective rehabilitation methods and in determining when reconstructive surgery is needed.
Acknowledgments
We would like to thank T. Ishida (physical therapist), K. Isobe and A. Takazawa for their assistance with data collection.
Footnotes
Author Contribution: A. Tanaka: Study design, Data collection, Data analysis, Writing and revising the paper.
Y. Yoshimura: Study design, Data collection, Data analysis, Revising the paper.
K. Aoki: Data collection, Data analysis.
M. Kito: Data collection, Data analysis
M. Okamoto: Data collection, Data analysis.
S. Suzuki: Data collection, Data analysis.
T. Momose: Study design, Data collection, Data analysis.
H. Kato: Data analysis, Revising the paper.
ICMJE conflict of interest: None declared.
Funding
None declared.
References
- 1. Rimner A, Brennan MF, Zhang Z, Singer S, Alektiar KM. Influence of compartmental involvement on the patterns of morbidity in soft tissue sarcoma of the thigh. Cancer 2009;115:149-157. [DOI] [PubMed] [Google Scholar]
- 2. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res 1993;286:241-246. [PubMed] [Google Scholar]
- 3. Davis AM, Wright JG, Williams JI, et al. Development of a measure of physical function for patients with bone and soft tissue sarcoma. Qual Life Res 1996;5:508-516. [DOI] [PubMed] [Google Scholar]
- 4. Ogura K, Uehara K, Akiyama T, et al. Cross-cultural adaptation and validation of the Japanese version of the Toronto Extremity Salvage Score (TESS) for patients with malignant musculoskeletal tumors in the lower extremities. J Orthop Sci 2015;20:1098-1105. [DOI] [PubMed] [Google Scholar]
- 5. EuroQol Group. EuroQol–a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. [DOI] [PubMed] [Google Scholar]
- 6. Tsuchiya A, Ikeda S, Ikegami N, et al. Estimating an EQ-5D population value set: the case of Japan. Health Econ 2002;11:341-353. [DOI] [PubMed] [Google Scholar]
- 7. Fukuhara S, Suzukamo Y. Manual of the SF-8 Japanese version. Kyoto: Institute for Health Outcomes & Process Evaluation Research; 2004.(In Japanese.) [Google Scholar]
- 8. Pritsch T, Malawer MM, Wu CC, Squires MH, Bickels J. Functional reconstruction of the extensor mechanism following massive tumor resections from the anterior compartment of the thigh. Plast Reconstr Surg 2007;120:960-969. [DOI] [PubMed] [Google Scholar]
- 9. Markhede G, Stener B. Function after removal of various hip and thigh muscles for extirpation of tumors. Acta Orthop Scand 1981;52:373-395. [DOI] [PubMed] [Google Scholar]
- 10. Murray MP, Jacobs PA, Mollinger LA, Gore DR. Functional performance after excision of the vastus lateralis and vastus intermedius. A case report. J Bone Joint Surg [Am] 1983;65-A:856-859. [PubMed] [Google Scholar]
- 11. Zhang LQ, Wang G, Nuber GW, Press JM, Koh JL. In vivo load sharing among the quadriceps components. J Orthop Res 2003;21:565-571. [DOI] [PubMed] [Google Scholar]
- 12. Lieb FJ, Perry J. Quadriceps function. An anatomical and mechanical study using amputated limbs. J Bone Joint Surg [Am] 1968;50-A:1535-1548. [PubMed] [Google Scholar]
- 13. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010;39:412-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Barker KL, Lamb SE, Simpson HR. Recovery of muscle strength and power after limb-lengthening surgery. Arch Phys Med Rehabil 2010;91:384-388. [DOI] [PubMed] [Google Scholar]
- 15. Barker KL, Simpson AH. Recovery of function after closed femoral shortening. J Bone Joint Surg [Br] 2004;86-B:1182-1186. [DOI] [PubMed] [Google Scholar]
- 16. Holm I, Nordsletten L, Steen H, Follerås G, Bjerkreim I. Muscle function after mid-shaft femoral shortening. A prospective study with a two-year follow-up. J Bone Joint Surg [Br] 1994;76-B:143-146. [PubMed] [Google Scholar]
- 17. Ploutz-Snyder LL, Manini T, Ploutz-Snyder RJ, Wolf DA. Functionally relevant thresholds of quadriceps femoris strength. J Gerontol A Biol Sci Med Sci 2002;57:B144-B152. [DOI] [PubMed] [Google Scholar]
- 18. Yonemoto T, Ishii T, Takeuchi Y, et al. Evaluation of quality of life (QOL) in long-term survivors of high-grade osteosarcoma: a Japanese single center experience. Anticancer Res 2007;27:3621-3624. [PubMed] [Google Scholar]
- 19. Ihara K, Shigetomi M, Kawai S, Doi K, Yamamoto M. Functioning muscle transplantation after wide excision of sarcomas in the extremity. Clin Orthop Relat Res 1999;358:140-148. [PubMed] [Google Scholar]
- 20. Muramatsu K, Ihara K, Miyoshi T, et al. Transfer of latissimus dorsi muscle for the functional reconstruction of quadriceps femoris muscle following oncological resection of sarcoma in the thigh. J Plast Reconstr Aesthet Surg 2011;64:1068-1074. [DOI] [PubMed] [Google Scholar]
- 21. Innocenti M, Abed YY, Beltrami G, et al. Quadriceps muscle reconstruction with free functioning latissimus dorsi muscle flap after oncological resection. Microsurgery 2009;29:189-198. [DOI] [PubMed] [Google Scholar]
- 22. Lo SJ, Yeo M, Puhaindran M, Hsu CC, Wei FC. A reappraisal of functional reconstruction of extension of the knee following quadriceps resection or loss. J Bone Joint Surg [Br] 2012;94-B:1016-1023. [DOI] [PubMed] [Google Scholar]
- 23. Jones KB, Ferguson PC, Deheshi B, et al. Complete femoral nerve resection with soft tissue sarcoma: functional outcomes. Ann Surg Oncol 2010;17:401-406. [DOI] [PubMed] [Google Scholar]


