Abstract
Objectives
Normal sagittal spine-pelvis-lower extremity alignment is crucial in humans for maintaining an ergonomic upright standing posture, and pathogenesis in any segment leads to poor balance. The present study aimed to investigate how this sagittal alignment can be affected by severe knee osteoarthritis (KOA), and whether associated changes corresponded with symptoms of lower back pain (LBP) in this patient population.
Methods
Lateral radiograph films in an upright standing position were obtained from 59 patients with severe KOA and 58 asymptomatic controls free from KOA. Sagittal alignment of the spine, pelvis, hip and proximal femur was quantified by measuring several radiographic parameters. Global balance was accessed according to the relative position of the C7 plumb line to the sacrum and femoral heads. The presence of chronic LBP was documented. Comparisons between the two groups were carried by independent samples t-tests or chi-squared test.
Results
Patients with severe KOA showed significant backward femoral inclination (FI), hip flexion, forward spinal inclination, and higher prevalence of global imbalance (27.1% versus 3.4%, p < 0.001) compared with controls. In addition, patients with FI of 10° (n = 23) showed reduced lumbar lordosis and significant forward spinal inclination compared with controls, whereas those with FI > 10° (n = 36) presented with significant pelvic anteversion and hip flexion. A total of 39 patients with KOA (66.1%) suffered from LBP. There was no significant difference in sagittal alignment between KOA patients with and without LBP.
Conclusions
The sagittal alignment of spine-pelvis-lower extremity axis was significantly influenced by severe KOA. The lumbar spine served as the primary source of compensation, while hip flexion and pelvic anteversion increased for further compensation. Changes in sagittal alignment may not be involved in the pathogenesis of LBP in this patient population.
Cite this article: W. J. Wang, F. Liu, Y.W. Zhu, M.H. Sun, Y. Qiu, W. J. Weng. Sagittal alignment of the spine-pelvis-lower extremity axis in patients with severe knee osteoarthritis: A radiographic study. Bone Joint Res 2016;5:198–205. DOI:10.1302/2046-3758.55.2000538.
Keywords: Knee osteoarthritis, Sagittal alignment, Low back pain, Lumbar lordosis, Hip flexion
Article focus
Chronic lower back pain (LBP) is common in patients suffering from severe knee osteoarthritis (KOA), but the pathogenesis is unclear.
This study aimed to determine the compensation patterns in spine-pelvis-lower extremity alignment associated with knee flexion caused by severe KOA.
We also assessed whether the sagittal alignment of the spine-pelvis lower extremity axis is involved in the pathogenesis of LBP in patients with severe KOA.
Key messages
Spine-pelvis-lower extremity sagittal alignment was significantly influenced by severe KOA.
Changes in the lumbar spine primarily compensated for KOA, while hip flexion and pelvic anteversion provided further compensation.
Changes in sagittal spinopelvic alignment may not be involved in the pathogenesis of LBP in this patient population.
Strengths and limitations
The spine-pelvis-lower extremity sagittal alignment in patients suffered severe KOA was analysed on lateral full length radiographs and abnormalities were identified.
The incidence of LBP in patients suffered severe KOA was documented.
The interaction between LBP and the abnormalities in sagittal alignment was interpreted in these patients.
Knee flexion was not directly measured using radiographs.
Introduction
Ambulatory humans maintain a stable and ergonomic upright standing position by co-ordinating the alignment of the spine, pelvis and lower extremity, particularly in the sagittal plane.1,2 Pathology in any segment of the trunk or lower leg can disturb the global postural equilibrium, resulting in compensatory changes in other segments. The development of new radiographic parameters3 has led to significant progress in understanding the sagittal spinopelvic alignment in both the general population4-9 and in patients suffering from spinal disorders10-12 and hip pathogenesis.13 These patients adjust the sagittal alignment not only by spinal inclination, but also by pelvic rotation, or even hip and knee flexion, to maintain a static horizontal gaze with the least expenditure of energy.14-16 In patients suffering from chronic lower back pain (LBP), a significant association between lumbar lordosis (LL) and knee extension has been documented.17 Moreover, Obeid et al18 found that knee flexion was the main compensatory mechanism for a lack of LL in patients with major spinal deformities and severe sagittal imbalance.
Chronic LBP is very common in patients with knee osteoarthritis (KOA), and this phenomenon has been termed ‘knee–spine syndrome’.17,19 The pathogenesis of associated LBP, however, has not been well investigated. Given that abnormal sagittal spinopelvic alignment has been found in patients with chronic LBP and is thought to contribute to its pathogenesis,10,20,21 we hypothesised that knee pain might lead to changes in spine-lower extremity sagittal alignment, and subsequently contribute to the development of LBP. Therefore, the present study investigated the static sagittal alignment of patients suffering from KOA and compared it with that of healthy controls. The objectives were: to understand the sagittal spine-pelvis-lower extremity alignment pattern and explore compensatory mechanisms in patients with KOA, and to determine if the sagittal alignment was associated with LBP secondary in KOA patients.
Materials and Methods
Study subjects
This cross-sectional study was approved by the Nanjing Drum Tower Hospital Clinical Research Ethics Committee (Nanjing, China). During 2014, patients admitted to our department for total knee arthroplasty (TKA) were screened by medical history and physical examination, and patients who met the following criteria were recruited into the present study: diagnosis of primary KOA; ambulatory without assistance; normal muscle strength in the lower extremity; and no leg-length discrepancy. Patients were not included if they had arthritis secondary to another aetiology, such as rheumatoid arthritis, ankylosing spondylitis (AS), trauma, meniscectomy or previous surgical interventions to the knee; osteoarthritic symptoms in the hip or ankle joints spinal disease or a history of procedures that would affect the sagittal alignment of the spine and pelvis. In addition, subjects who were identified on radiographs as having skeletal abnormalities other than knee OA were excluded, such as those with severe osteophytes, vertebral collapse, spondylolisthesis, scoliosis (> 10°), or degeneration in other joints with Kellgren-Lawrence (K-L) grade ⩾ 2.22
The healthy controls were selected randomly from our ongoing project in screening for OA in local residents. In total, 100 subjects were selected with the following criteria set for recruitment: 50 to 70 years of age; no spinal pathology or deformity; and no history of hip, pelvis, or lower-limb disorders. Subjects were excluded if they had a history of pain in the lower back, hip or knee for ⩾ three months consecutively. In all, 42 subjects were excluded based on these criteria, leaving 58 subjects recruited as healthy controls.
Informed consent was obtained from each subject and demographic characteristics (e.g., age, gender) were collected. Furthermore, patients with severe KOA were asked about the presence and duration of pain in the lumbar spine. Chronic LBP was defined as pain for ⩾ three consecutive months.
Radiographs and measurements
Posteroanterior and lateral digital radiographs of the spine, pelvis and proximal femur were taken using a standard protocol with the subject standing upright.23,24 For lateral radiographs, subjects were asked to stand upright in a relaxed and natural manner, avoiding a forced position, looking forward with feet together on flat ground. The fingers were held on the clavicle with upper arms positioned approximately 45° to the vertical. Three films were taken focusing on T8, L2 and the hip axis and then combined into one radiograph (including the whole spine, pelvis and femur).
Radiographs were first reviewed by a senior spinal surgeon (YQ) to exclude the presence of spinal disorders. Then the following parameters describing the sagittal profile of the spine, pelvis and lower leg were quantified on lateral radiographs using Surgimap Spine version 2.0.7 (Nemaris Inc., New York, New York): sagittal alignment of the pelvis and hip (Fig. 1a): pelvic incidence (PI),2,25 pelvic tilt (PT),2 sacral slope (SS),2 pelvic femoral angle (PFA),3,26 sacrofemoral angle (SFA),27 and femoral inclination (FI);28 and sagittal alignment and balance of the spine (Fig. 1b): LL, spinosacral angle, and C7 tilt (C7T). Table I describes these parameters.
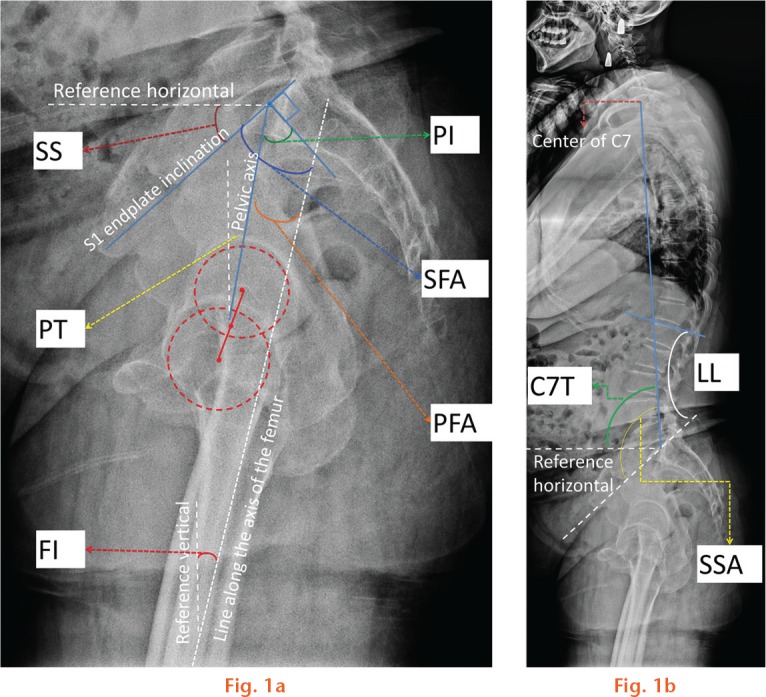
Illustration of the radiographic parameters of the sagittal alignment of the spine, pelvis and hip: a) parameters of the pelvis and hip joint. PI, pelvic incidence; PT, pelvic tilt; SS, sacral slope; PFA, pelvic femoral angle; SFA, sacrofemoral angle; FI, femoral inclination; b) parameters of the spine. LL, lumbar lordosis; C7T, C7 tilt; SSA, spinosacral angle.
Table I.
Radiographic parameters of sagittal spine-pelvis-leg alignment2
| Parameters | Abbreviation | Description |
|---|---|---|
| Pelvic incidence (°)2 | PI | The angle between the line joining the hip axis and the centre of the S1 end plate and the line orthogonal to the S1 end plate |
| Pelvic tilt (°)2 | PT | The angle between the line joining the hip axis and the centre of the S1 end plate and the reference vertical line |
| Sacral slope (°)2) | SS | The angle between the line along the S1 end plate and the reference horizontal line |
| Lumbar lordosis (°) | LL | Segmental angle of spinal segment in lordosis (L1 to L5) |
| Spinosacral angle (°) | SSA | The angle between the line along the S1 end plate and the reference vertical line |
| C7 tilt (°) | C7T | The angle between the line joining the centre of S1 end plate and the centre of C7 and the reference vertical line |
| Sacrofemoral angle (°)2 | SFA | The angle between the line along the S1 end plate and the line along the axis of the femur |
| Pelvic femoral angle (°)3 | PFA | The angle between the line joining the hip axis and the centre of the S1 end plate and the line along the axis of the femur |
| Femoral inclination (°)28 | FI | The angle between the line along the axis of the femur and the reference vertical line |
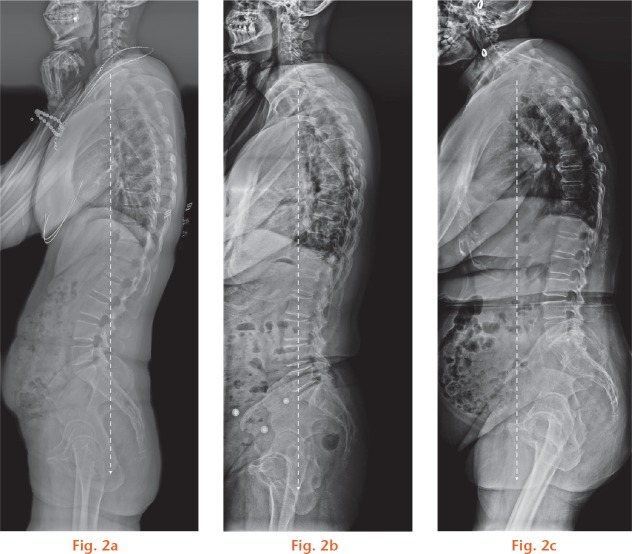
In addition, the global balance pattern of spinopelvic alignment20,29 was classified into three types according to the relative position of the C7 plumb line to the pelvis (Fig. 2): normal balance: the C7 plumb line is located over the sacral end plate; slight imbalance: the C7 plumb line is located between the sacrum and femoral heads; and severe imbalance: the C7 plumb line is located to the anterior of the femoral heads.
The sagittal balance pattern of spinopelvic alignment: a) normal balance, with slight pelvic retroversion and the C7 plumb line over the sacral end plate; b) slight unbalance, the C7 plumb line was located between the sacrum and femoral heads; c) severe unbalance, the C7 plumb line was located in the anterior of the femoral heads.
The measurements were made by two independent observers (WJW, FL) to compare interobserver reliability. After four weeks, the measurements were repeated by one observer (WJW) to compare intra-observer reliability.
Statistical analysis
Data analysis was performed using SPSS version 13.0 (SPSS, Inc., Chicago, Illinois). Intra- and interobserver reliability were analysed using intraclass correlations. Comparisons of participant ages and radiographic parameters between controls and patients, and between patient subgroups, were performed using independent samples t-tests. The global balance patterns between groups were compared using the chi-squared test. The level of significance was defined as p ⩽ 0.05.
Results
During the period of study, TKA was carried out in 103 knees in our department, 87 of which were diagnosed as primary KOA. In total, 13 patients were excluded due to arthroplasty in the hip (n = 7) or the other knee (n = 3), or operations on the spine (n = 3). Three patients refused to participate in the study. In addition, further radiographic examination revealed lumbar spondylolisthesis in three patients, degenerative lumbar scoliosis in one patient (Cobb 27°), osteoporotic vertebral fracture in two patients, and osteoarthritis of the hip with K-L grade ⩾ 2 in three patients. Consequently, images were analysed from the remaining 59 patients (16 men and 43 women; mean age 65.9 years, 50 to 80). An additional 14 men and 44 women free from KOA were recruited as controls (mean age 62.9 years, 50 to 69). The gender distribution was comparable between the two groups, but patients with severe KOA were significantly older than control subjects (p < 0.01).
Reliability analysis showed high intra- and inter-observer agreements in the spine-pelvis-leg parameters, with intraclass correlations > 0.8.
The mean values and standard deviations of the studied parameters in the control subjects and severe KOA patients are summarised in Table II. Comparable PI, SS, and PT values were revealed between the two groups, suggesting similar sagittal morphology and pelvic alignment. However, patients with severe KOA showed significantly larger FI (11.3° versus 4.2°, p < 0.001) and smaller SFA (43.1° versus 51.8°, p < 0.001) and PFA (2.2° versus 9.1°, p < 0.001) values compared with controls. These results indicate flexed knee and hip joints among patients with severe KOA. In addition, C7T was significantly smaller among severe KOA patients compared with controls (88.4° versus 92.9°, p < 0.001), indicating forward inclination of the spine. Analysis of global sagittal balance patterns found that patients with severe KOA had a significantly higher prevalence of severe imbalance than controls (27.1% versus 3.4%, χ2 = 33.4, p = 5.5*10−8; Table II).
Table II.
Comparison of the sagittal spine-pelvis-leg alignment parameters between patients with knee osteoarthritis and asymptomatic controls
| Control (n = 58) | KOA |
|||||||
|---|---|---|---|---|---|---|---|---|
| Total (n = 59) | p-value* | FI ⩽ 10° (n = 23) | p-value* | FI > 10° (n = 36) | p-value* | p-value† | ||
| SS | 32.7(7.6) | 35.0(9.0) | 0.074 | 32.9(7.0) | 0.510 | 36.4(10.3) | 0.012 | 0.138 |
| PT | 13.4(6.0) | 12.4(6.5) | 0.245 | 13.5(5.1) | 0.681 | 11.9(7.5) | 0.184 | 0.465 |
| PI | 46.8(9.0) | 47.3(10.3) | 0.476 | 46.2(8.0) | 0.954 | 48.3(11.9) | 0.279 | 0.359 |
| LL | 49.1(9.4) | 48.0(11.4) | 0.883 | 44.1(11.0) | 0.116 | 50.2(11.5) | 0.429 | 0.062 |
| SSA | 126.0(7.4) | 123.9(8.5) | 0.501 | 122.9(7.6) | 0.412 | 124.6(9.4) | 0.822 | 0.636 |
| C7T | 92.9(3.5) | 88.4(4.1) | < 0.001 | 89.9(3.6) | 0.008 | 87.5(4.4) | < 0.001 | 0.008 |
| SFA | 51.8(8.5) | 43.1(11.9) | < 0.001 | 49.9(8.9) | 0.188 | 38.8(11.6) | < 0.001 | < 0.001 |
| PFA | 9.1(8.1) | 2.2(8.9) | < 0.001 | 7.0(7.2) | 0.196 | –0.7(8.7) | < 0.001 | < 0.001 |
| FI | 4.2(3.5) | 11.3(5.1) | < 0.001 | 6.7(2.8) | 0.005 | 14.1(4.1) | < 0.001 | < 0.001 |
| Global balance pattern of spine (% within group) | ||||||||
| Normal balance | 49 (84.5) | 19 (32.2) | 10 (43.5) | 9 (25.0) | ||||
| Slight unbalance | 7 (12.1) | 24 (40.7) | 10 (43.5) | 14 (38.9) | ||||
| Severe unbalance | 2 (3.4) | 16 (27.1) | 3 (13.0) | 13 (36.1) | ||||
| Lower back pain (% within group) | ||||||||
| No | 20 (33.9) | 5 (21.7) | 15 (41.7) | |||||
| Yes | 39 (66.1) | 18 (78.3) | 21 (58.3) | |||||
the p-value by comparing with control
the p-value by comparing with KOA with FI ⩽ 10°
KOA, knee osteoarthritis; SS, sacral slope; PT, pelvic tilt; PI, pelvic incidence; LL, lumbar lordosis; SSA, spinosacral angle; C7T, C7 tilt; SFA, sacrofemoral angle; PFA, pelvic femoral angle; FI, femoral inclination
Data presented as mean (sd)
The distribution of global balance pattern between groups was compared with the chi-squared test. A significant difference was revealed between the controls and patients in total (x2 = 33.4, p = 5.5*10−8), patients with FI ⩽ 10° (chi squared = 14.0, p = 0.0009) or FI > 10° (chi squared = 34.7, p = 2.9*10−8)
Patients placed into a subgroup by FI showed no difference in prevalence of LBP
Comparisons between control and KOA patients, and between patient subgroups, were performed using independent sample t-tests. The global balance patterns between groups were compared using the Chi-squared test.
To understand the compensatory pattern of the pelvis and spine to knee flexion, patients with severe KOA were divided into two subgroups according to FI: ⩽ 10° (n = 23) and > 10° (n = 36) (Table II). Compared with controls, patients with FI ⩽ 10° showed reduced LL and smaller C7T value, but no differences in pelvic (PT, PI, SS) or hip flexion (SFA, PFA) parameters. Conversely, patients with FI > 10° showed significantly larger FI and SS values, but smaller C7T, SFA, and PFA values, compared with controls. Comparing these parameters between the two subgroups of patients with severe KOA, we found that those with FI > 10° had significantly smaller C7T, SFA, and PFA values than those with FI ⩽ 10°. In addition, LL in patients with FI > 10° was larger than that in patients with FI ⩽ 10° but the difference did not reach statistical significance (p = 0.063). The prevalence of severe imbalance in spinopelvic alignment was higher in both subgroups than in the control group and the prevalence in patients with FI > 10° (36.1%) was even higher than that in patients with FI ⩽ 10° (13.0%) (Table II).
A total of 39 patients with severe KOA reported chronic LBP, giving a prevalence of 66.1%. Patients with a severely imbalanced global spine showed a higher prevalence of LBP. The sagittal alignment parameters of these patients were compared with those of severe KOA patients without LBP, but no significant differences were identified with the numbers available (Table III). In addition, patients with FI ⩽ 10° showed no significant difference in the prevalence of LBP compared with those with FI > 10° (18/23 versus 21/36 patients, chi-squared = 2.5, p = 0.11).
Table III.
Comparisons of the sagittal spine-pelvis-lower extremity alignment parameters in KOA patients with or without LBP
| Without LBP | With LBP | p value | |
|---|---|---|---|
| SS | 32.9(8.4) | 36.2(9.2) | 0.921 |
| PT | 12.2(7.1) | 12.5(6.3) | 0.315 |
| PI | 45.0(10.0) | 48.5(10.4) | 0.683 |
| LL | 46(10.4) | 49.0(11.9) | 0.234 |
| SSA | 121.6(8.1) | 125.1(8.5) | 0.654 |
| C7T | 88.7(3.9) | 88.3(4.3) | 0.418 |
| SFA | 44.6(13.0) | 42.2(11.3) | 0.377 |
| PFA | 0.6(11.1) | 3.1(7.4) | 0.615 |
| FI | 12.3(6.3) | 10.7(4.3) | 0.256 |
LBP, lower back pain; SS, sacral slope; PT, pelvic tilt; PI, pelvic incidence; LL, lumbar lordosis; SSA, spinosacral angle; C7T, C7 tilt; SFA, sacrofemoral angle; PFA, pelvic femoral angle; FI, femoral inclination
Data presented as mean (sd)
The comparison was carried out by independent samples t-test. No significant difference was revealed between the two subgroups of patients with knee osteoarthritis
Discussion
Sagittal spine-pelvis-lower extremity alignment can be significantly affected by spinal disorders and hip osteoarthritis, and abnormal sagittal alignment has been identified as a contributor to the pathogenesis of LBP. In major spinal deformities, flexion of the knee has been found to be the main compensatory mechanism for a lack of LL.18 In the present study, significant abnormal sagittal spine-pelvis-lower extremity alignment was identified in patients with severe KOA compared with asymptomatic controls. Patients with severe KOA showed a more forwardly inclined femur and spine, flexed hip, and higher risk of global imbalance than control subjects. In addition, patients with different FI severities showed different compensatory patterns.
The effect of knee flexion on sagittal spinal alignment has been investigated by Lee et al28 who asked 30 young men to wear a motion-controlled knee brace to produce knee flexion. They found that by flexing the knee to 15° and 30°, the participants showed a significantly reduced femoropelvic angle (PFA in the present study) but an increased femoral tilt angle (FI in the present study). They also found reduced LL, but a more anteriorly shifted centre of C7 relative to the superoposterior corner of S1 and the bicoxofemoral axis. These findings indicated more hip flexion and less LL on knee flexion, and more forward inclination of the spine. Conversely, the alignment of the pelvis was not affected, with no significant changes in SS and PT. In the present study, patients with severe KOA showed more hip flexion and forward spinal inclination than controls, leading to a significantly higher prevalence of severe imbalance in sagittal alignment than controls (27.1%, versus 3.4%). However, it is interesting to note that the LL was comparable between the two groups, which differs from the compensation mechanism reported by Lee et al.28 We believe that this inconsistency might be a result of the flexibility of the subjects studied. The subjects recruited by Lee et al were young adults in their 20s and 30s with no history of spinal pathologies,28 while the severe KOA patients in our study were all candidates for knee replacement and had a mean age of 65.9 years (50 to 80). Older populations might suffer from poor flexibility of the lumbar spine and have limited compensatory abilities for knee flexion.
To determine the contribution of the hip and lumbar spine to the compensatory knee flexion caused by severe KOA, the patients were further divided into two groups according to FI (⩽ 10° and > 10°); 10° was selected as the cut-off because significant changes in sagittal alignment have been found with 15° changes in knee flexion, either via stimulation28 or knee replacement.30 Interestingly, the severe KOA patients in the two subgroups showed significantly different patterns in sagittal spinopelvic alignment. Compared with controls, patients with FI ⩽ 10° showed less LL and more forward inclination of spine but comparable pelvic alignment, suggesting that the compensation was mainly contributed by the lumbar spine. In contrast, patients with FI >10° showed significant forward spinal inclination, hip flexion (small SFA and PFA), and pelvic anteversion (larger SS) but comparable LL versus controls. Therefore, changes in sagittal spinopelvic alignment in severe KOA patients with FI > 10° were mainly a result of hip flexion and pelvic anteversion. Lee et al28 proposed two mechanisms of compensation on knee flexion. The authors suggested that the lumbar spine will respond first to maintain global balance when it is flexible and the pelvis does not need to rotate, while the pelvis will respond first by rotation and hip flexion if the lumbar spine is rigid.28 This might help to explain the findings in the present study. When the knee is in mild flexion (i.e. FI ⩽ 10°), patients might compensate for their disturbed global balance through the lumbar spine, presenting as reduced LL and forward spinal inclination (Fig. 3). However, with increased knee flexion and posterior inclination of the femur, the limited flexibility of the lumbar spine in aged patients might fail to compensate, and instead, the hip joint would be responsible for this response by flexion and forward inclination of the pelvis. This would present as increased SS and decreased PFA and SFA (Fig. 3). Furthermore, Lee et al28 found that PFA might be a better measure to represent true pelvic compensation, whereas PT can represent apparent pelvic compensation. Our results also show that although PT was similar between the control group and both subgroups of severe KOA patients, those with FI > 10° showed a significantly decreased PFA compared with both controls and patients with FI ⩽ 10°, indicating a role for the pelvis in compensating for knee flexion in these patients.
Fig. 3.
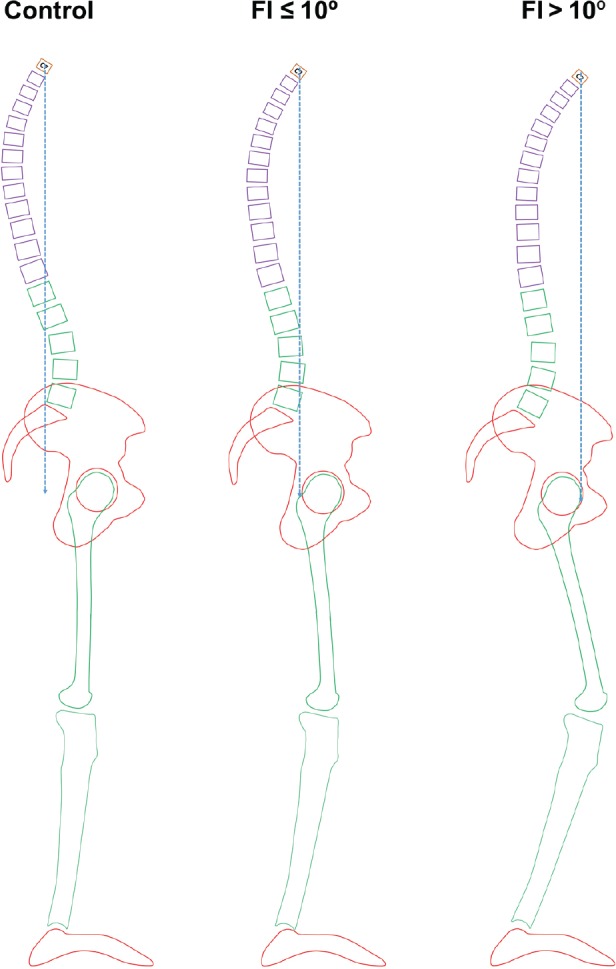
Pattern of compensation in patients with knee osteoarthritis (KOA) with different severities of knee flexion. In normal subjects, the C7 plumb line would pass through or behind the S1 vertebral body, and the anterior pelvic plane would be vertical to the horizontal plane. In patients with KOA and mild knee flexion (FI ⩽ 10°), the femur is posteriorly inclined. To compensate for the disturbed sagittal balance, patients would extend the lumbar spine, showing decreased LL and forward inclined spine. When the knee flexion becomes severe (FI > 10°) and the sagittal balance cannot be compensated by lumbar spine only, the compensation in the sagittal plane is achieved by hip flexion, pelvic anteversion and forward inclination of the spine.
Chronic LBP has been found to be a risk factor for poor outcomes following total knee replacement.31,32 In the present study, chronic LBP was reported by 66.1% of severe KOA patients, which is an even higher prevalence than that reported in patients with symptomatic tibiofemoral KOA (57.4%) by Suri et al33 and in KOA patients recruited from an outpatient rheumatology clinic by Wolfe et al.34 In all three studies, however, the prevalence of LBP was extraordinarily higher than that reported in the general population.35 Abnormal sagittal spinopelvic alignment has been found in patients suffering from chronic LBP, presenting as low SS, low LL, and small PI values, and this specific pattern of sagittal alignment has been suggested as being associated with the presence of chronic LBP.10 In our study, the PI of severe KOA patients, either with or without LBP, was comparable with that of controls, suggesting normal sagittal morphology of the pelvis in these patients. Although abnormalities in sagittal alignment were revealed in the spine and hip, these abnormalities showed no distinction between patients with and without LBP. Hence, the results of the current study cannot support the hypothesis that the abnormal sagittal spinopelvic alignment is involved in the pathogenesis of LBP in patients with severe KOA. However, the numbers of this study were small and, therefore, definitive conclusions cannot be made.
We would like to acknowledge several limitations of the present study. Firstly, concerns over high-dosage radiographic exposure meant that we did not take radiographs of the distal parts of the lower extremities. Therefore, direct measurement of knee flexion was not available for these patients and FI was instead used to represent knee flexion, a method previously used in by others.28 Although FI could be affected by both the knee and ankle joints, anteroposterior radiographs of the ankle were carefully inspected and patients with disorders in this joint were excluded; therefore the FI was most likely mainly affected by knee flexion. In addition, patient body mass index (BMI) was not documented in the current study. In an ageing population, overweight adults (BMI ⩾ 25.0 Kg/m2) had higher odds of Roussouly classification types 2 and 4 non-neutral postures, while adults with an even higher BMI (⩾ 30.0 Kg/m2) and central obesity had higher odds of type 1 non-neutral posture.36 Moreover, our radiological analysis showed only static interactions between knee flexion, pelvic inclination, and LL. It should be remembered that these interactions would be more complex during daily activities such as work and sport. Gait analysis would be helpful in understanding the dynamic interactions between knee flexion and LL. Moreover, we recruited asymptomatic controls instead of recruiting a consecutive control without KOA. Hence, data regarding LBP in the general population are unavailable in the current study, and a direct comparison of the sagittal alignment between patients with KOA and controls with LBP could not be carried out in the present study. Furthermore, it is difficult to identify LBP secondary to KOA, and even LBP occurring after knee symptoms could be coexistent with KOA.
Despite these limitations, a distinct sagittal alignment of the spine-pelvis-lower extremity was identified in patients suffering from severe KOA when compared with asymptomatic controls. Overall, patients with severe KOA showed a more forward inclination of the global spine and greater flexion of the hip and knee joints. The lumbar spine appeared to serve as the primary source of compensation for disturbances of the sagittal alignment in patients with mild knee flexion (FI ⩽ 10°). In patients with severe knee flexion (FI > 10°), however, the spine, pelvis and hip joint were all involved in compensation, presenting as a forward inclined spine and pelvis and a flexed hip joint. The present study cannot support the involvement of abnormal sagittal spinopelvic alignment in the development or deterioration of LBP in patients with KOA. Further study of changes in sagittal alignment and LBP in these patients after knee replacement would be of interest.
Footnotes
Author Contribution: W. J. Wang: Study design, Data collection and analysis, Writing the paper.
F. Liu: Data collection and analysis.
Y.W. Zhu: Study design, Data analysis.
M.H. Sun: Data collection and analysis.
Y. Qiu: Study design, Data analysis, Writing the paper.
W. J. Weng: Study design, Data collection and analysis, Writing the paper.
ICMJE conflict of interest: None declared.
Supplementary material
A table showing intraclass correlation coefficient reliability is available alongside the online version of this article at www.bjr.boneandjoint.org.uk.
Funding Statement
This work was supported by the Project for Distinguished Young Scholars (JQX13008) and Key Project (YKK12081) of the Medical Science and Technology Development Foundation, Nanjing Department of Health, and The Six Categories of Top Talents, Jiangsu Provincial Department of Human Resources and Social Security (WSW-002).
References
- 1. Le Huec JC, Saddiki R, Franke J, Rigal J, Aunoble S. Equilibrium of the human body and the gravity line: the basics. Eur Spine J 2011;20(Suppl 5):558-563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 1998;7:99-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vrtovec T, Janssen MM, Likar B, et al. A review of methods for evaluating the quantitative parameters of sagittal pelvic alignment. Spine J 2012;12:433-446. [DOI] [PubMed] [Google Scholar]
- 4. Zhu Z, Xu L, Zhu F, et al. Sagittal alignment of spine and pelvis in asymptomatic adults: norms in Chinese populations. Spine (Phila Pa 1976) 2014;39:E1-E6. [DOI] [PubMed] [Google Scholar]
- 5. Mac-Thiong JM, Labelle H, Roussouly P. Pediatric sagittal alignment. Eur Spine J 2011; 20:586-590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P. Age- and sex-related variations in sagittal sacropelvic morphology and balance in asymptomatic adults. Eur Spine J 2011;20(Suppl 5):572-577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zárate-Kalfópulos B, Romero-Vargas S, Otero-Cámara E, Correa VC, Reyes-Sánchez A. Differences in pelvic parameters among Mexican, Caucasian, and Asian populations. J Neurosurg Spine 2012;16:516-519. [DOI] [PubMed] [Google Scholar]
- 8. Wang W, Wang Z, Liu Z, et al. Are there gender differences in sagittal spinal pelvic inclination before and after the adolescent pubertal growth spurt? Eur Spine J 2015;24:1168-1174. [DOI] [PubMed] [Google Scholar]
- 9. Faldini C, Pagkrati S, Leonetti D, Miscione MT, Giannini S. Sagittal segmental alignment as predictor of adjacent-level degeneration after a cloward procedure. Clin Orthop Relat Res 2011;469:674-681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chaléat-Valayer E, Mac-Thiong JM, Paquet J, et al. Sagittal spino-pelvic alignment in chronic low back pain. Eur Spine J 2011;20(Suppl 5):634-640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Roussouly P, Gollogly S, Berthonnaud E, Labelle H, Weidenbaum M. Sagittal alignment of the spine and pelvis in the presence of L5-s1 isthmic lysis and low-grade spondylolisthesis. Spine (Phila Pa 1976) 2006;31:2484-2490. [DOI] [PubMed] [Google Scholar]
- 12. Yong Q, Zhen L, Zezhang Z, et al. Comparison of sagittal spinopelvic alignment in Chinese adolescents with and without idiopathic thoracic scoliosis. Spine (Phila Pa 1976) 2012;37:E714-E720. [DOI] [PubMed] [Google Scholar]
- 13. Weng W-J, Wang W-J, Wu M-D, et al. Characteristics of sagittal spine-pelvis-leg alignment in patients with severe hip osteoarthritis. Eur Spine J 2015;24:1228-1236. [DOI] [PubMed] [Google Scholar]
- 14. Klineberg E, Schwab F, Smith JS, et al. Sagittal spinal pelvic alignment. Neurosurg Clin N Am 2013;24:157-162. [DOI] [PubMed] [Google Scholar]
- 15. Barrey C, Roussouly P, Perrin G, Le Huec JC. Sagittal balance disorders in severe degenerative spine. Can we identify the compensatory mechanisms? Eur Spine J 2011;20(Suppl 5):626-633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Watelain E, Dujardin F, Babier F, Dubois D, Allard P. Pelvic and lower limb compensatory actions of subjects in an early stage of hip osteoarthritis. Arch Phys Med Rehabil 2001;82:1705-1711. [DOI] [PubMed] [Google Scholar]
- 17. Murata Y, Takahashi K, Yamagata M, Hanaoka E, Moriya H. The knee-spine syndrome. Association between lumbar lordosis and extension of the knee. J Bone Joint Surg [Br] 2003;85-B:95-99. [DOI] [PubMed] [Google Scholar]
- 18. Obeid I, Hauger O, Aunoble S, et al. Global analysis of sagittal spinal alignment in major deformities: correlation between lack of lumbar lordosis and flexion of the knee. Eur Spine J 2011;20(Suppl 5):681-685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tsuji T, Matsuyama Y, Goto M, et al. Knee-spine syndrome: correlation between sacral inclination and patellofemoral joint pain. J Orthop Sci 2002;7:519-523. [DOI] [PubMed] [Google Scholar]
- 20. Roussouly P, Pinheiro-Franco JL. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 2011;20(Suppl 5):609-618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine (Phila Pa 1976) 1994;19:1611-1618. [DOI] [PubMed] [Google Scholar]
- 22. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Janssen MM, Drevelle X, Humbert L, Skalli W, Castelein RM. Differences in male and female spino-pelvic alignment in asymptomatic young adults: a three-dimensional analysis using upright low-dose digital biplanar X-rays. Spine (Phila Pa 1976) 2009;34:E826-E832. [DOI] [PubMed] [Google Scholar]
- 24. Morvan G, Mathieu P, Vuillemin V, et al. Standardized way for imaging of the sagittal spinal balance. Eur Spine J 2011;20(Suppl 5):602-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Duval-Beaupère G, Schmidt C, Cosson P. A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 1992;20:451-462. [DOI] [PubMed] [Google Scholar]
- 26. Mangione P, Senegas J. Sagittal balance of the spine. Rev Chir Orthop Repar Appar Mot 1997;83:22-32. (in French) [PubMed] [Google Scholar]
- 27. Takemitsu Y, Harada Y, Iwahara T, Miyamoto M, Miyatake Y. Lumbar degenerative kyphosis. Clinical, radiological and epidemiological studies. Spine (Phila Pa 1976) 1988;13:1317-1326. [PubMed] [Google Scholar]
- 28. Lee CS, Park SJ, Chung SS, Lee KH. The effect of simulated knee flexion on sagittal spinal alignment: novel interpretation of spinopelvic alignment. Eur Spine J 2013;22:1059-1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Roussouly P, Nnadi C. Sagittal plane deformity: an overview of interpretation and management. Eur Spine J 2010;19:1824-1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lee SM, Yoon MG, Moon MS, et al. Effect of correction of the contractured flexed osteoarthritic knee on the sagittal alignment by total replacement. Asian Spine J 2013;7:204-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Escobar A, Quintana JM, Bilbao A, et al. Effect of patient characteristics on reported outcomes after total knee replacement. Rheumatology (Oxford) 2007;46:112-119. [DOI] [PubMed] [Google Scholar]
- 32. Novicoff WM, Rion D, Mihalko WM, Saleh KJ. Does concomitant low back pain affect revision total knee arthroplasty outcomes? Clin Orthop Relat Res 2009;467:2623-2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Suri P, Morgenroth DC, Kwoh CK, et al. Low back pain and other musculoskeletal pain comorbidities in individuals with symptomatic osteoarthritis of the knee: data from the osteoarthritis initiative. Arthritis Care Res (Hoboken) 2010;62:1715-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wolfe F, Hawley DJ, Peloso PM, Wilson K, Anderson J. Back pain in osteoarthritis of the knee. Arthritis Care Res 1996;9:376-383. [DOI] [PubMed] [Google Scholar]
- 35. Raspe H. Back pain. In: Silman AJ, Hochberg M, eds. Epidemiology of the rheumatic diseases. Oxford: Oxford University Press, 1993. [Google Scholar]
- 36. Araújo F, Lucas R, Alegrete N, Azevedo A, Barros H. Individual and contextual characteristics as determinants of sagittal standing posture: a population-based study of adults. Spine J 2014;14:2373-2383. [DOI] [PubMed] [Google Scholar]