Abstract
The cochlear implant (CI) is the first effective treatment for deafness and severe losses in hearing. As such, the CI is now widely regarded as one of the great advances in modern medicine. This paper reviews the key events and discoveries that led up to the current CI systems, and we review and present some among the many possibilities for further improvements in device design and performance. The past achievements include: (1) development of reliable devices that can be used over the lifetime of a patient; (2) development of arrays of implanted electrodes that can stimulate more than one site in the cochlea; and (3) progressive and large improvements in sound processing strategies for CIs. In addition, cooperation between research organizations and companies greatly accelerated the widespread availability and use of safe and effective devices. Possibilities for the future include: (1) use of otoprotective drugs; (2) further improvements in electrode designs and placements; (3) further improvements in sound processing strategies; (4) use of stem cells to replace lost sensory hair cells and neural structures in the cochlea; (5) gene therapy; (6) further reductions in the trauma caused by insertions of electrodes and other manipulations during implant surgeries; and (7) optical rather electrical stimulation of the auditory nerve. Each of these possibilities is the subject of active research. Although great progress has been made to date in the development of the CI, including the first substantial restoration of a human sense, much more progress seems likely and certainly would not be a surprise.
Keywords: Cochlear implant, Hair cells, Deafness, Hearing preservation, Optical stimulation, Infrared nerve stimulation, Spiral ganglion neurons
I. Introduction
The cochlear implant (CI) has transformed the field of otology. Just 50 years ago, there were no effective treatments for deafness and severe losses in hearing. The development of the CI changed that completely and today most recipients of CIs can converse with ease using their cell phones. The development has been both rapid and remarkable.
In most cases, deafness and severe losses in hearing are caused by damage to or destruction of the sensory hair cells in the cochlea. The function of the CI is to bypass those damaged or missing structures by exciting neurons in the auditory nerve directly with electrical stimuli. Modern CIs selectively excite subpopulations of neurons using different electrodes in an array of electrodes inserted at surgery into the scala tympani of the cochlea. The bioengineering and surgical principles underlying successful CIs are explained in detail in a companion paper in this special issue (Eshraghi et al., 2012).
The purposes of the present paper are to (1) provide an overview of the efforts leading up to the current devices, and (2) describe some among the many possibilities for further improvements in design and performance. Remaining problems that might be addressed or at least ameliorated include a persistent variability in outcomes even with the newest CI systems; difficulties experienced by most patients in listening to speech in noisy environments or in competition with other talkers ; and reception of sounds more complex than western speech such as music and tone languages. Any further improvements would of course build upon the already impressive performances achieved to date.
II. Historical aspects
II.a Electrically evoked hearing
Alessandro Volta, who developed the electric battery, provided the first account of electrical stimulation of the auditory system. In the early 1800s, he connected each pole of a battery to a metal probe and inserted one probe into one of his ear canals and the other probe into the other canal. One of the probes had a switch to interrupt or allow the flow of current. He described his experience after closing the switch as a “jolt in the head,” followed by a sound that resembled “a kind of crackling, jerking, or bubbling as if some dough or thick material was boiling” (Volta, 1982).
In 1855, Duchenne de Boulogne stimulated the cochlea with an alternating rather than direct current, and he experienced similar sensations of buzzing, hissing, and ringing. The stimulation also elicited multiple other non-auditory sensations such as the sensation of a metallic taste (probably due to stimulation of the chorda tympani nerve, authors’ note). A fascinating series of experiments involving electrically evoked hearing is described in Chapter 22 of the book “Selections from the Clinical Works of Dr. Duchenne (de Boulogne)” (translated, edited, and condensed by G. V. Poole, 1883).
In 1930, Wever and Bray recorded electrical potentials in the cochlea that closely followed the waveform of the sound stimulus (Wever and Bray, 1930). This “Wever and Bray effect” suggested the possibility to some that, if the potentials could somehow be replicated, then lost or absent hearing could be restored.
Finally, in 1957, André Djourno and Charles Eyriès performed the first direct electrical stimulation of the human auditory system (Djourno and Eyries, 1957). The patient had only the stump of the auditory nerve remaining on both sides following previous ear surgeries. The patient was operated on again by the otolaryngologist Eyriès to address a recurring problem and during the operation he placed an electrode designed by the electrophysiologist Djourno into the stump of the auditory nerve on one side. In addition, an induction coil with a return electrode was placed into the temporalis muscle. Postoperative testing revealed successful detections of electrical stimuli generated from a microphone. The patient could discriminate different intensities, but discrimination of different frequencies was very poor and was nonexistent for frequencies above about 1000 Hz. Although some words in small closed sets (e.g., with three words) could be identified, probably on the basis of rhythmic cues, the patient could not understand any speech spoken naturally and could not differentiate among talkers. The device failed only a few weeks after the implantation. One other patient also was implanted, but that device failed as well; thus leading Eyriès to refuse to proceed further with the project (see review in Seitz, 2002).
II.b Initial efforts to develop a safe and effective CI
Although the studies in Paris by Djourno and Eyriès were abandoned almost as soon as they began, publication of the results in the French medical journal La Presse Médicale had far-reaching effects. In particular, the publication prompted brief news accounts that were published outside of France, including the Los Angeles Times in the USA. A patient visiting the Los Angeles clinic of Dr. William F. House, M.D., gave Dr. House a copy of the news article and Dr. House later obtained a translated version of the publication in La Presse Médicale. The news article and the publication demonstrated to Dr. House that hearing percepts could be elicited with direct electrical stimulation of the auditory nerve, and this fact inspired him to develop an auditory prosthesis for deaf persons that could be used reliably for many years and hopefully a lifetime.
In 1961, Dr. House, who was an otologist, teamed with Dr. John Doyle, who was a neurosurgeon, to implant the first patients in Los Angeles (House and Urban, 1973; House, 1976). These first implants consisted of either a single wire with a flamed ball contact at the end or an array of five electrodes made in the same way. A surgical approach was developed to allow insertion of the electrode(s) into the scala tympani through an incision in the round window membrane. The results obtained with these implants were promising: the patients had some basic frequency discrimination and could identify words in small closed sets. However, the insufficient biocompatibility of the electrodes resulted in complications that required removal of the electrodes and limited long-term testing. The fear of infection and electrode rejection led House to postpone any further work on the implant for several years. Doyle, however, continued to implant numerous patients. Glowing reports of the results were presented in newspaper articles, but little systematic analysis of these patients was published (Doyle et al., 1963). In 1968, a lack of funding finally brought Doyle's work to a halt. House's interest in implants was rekindled when he witnessed the development and success of other devices, such as pacemakers and ventriculoperitoneal shunts. The long term safety and efficacy of these devices suggested to House that a reliable and fully biocompatible CI could be made using the new techniques.
House resumed his work on implants in 1967. Soon thereafter he enlisted the help and partnership of Mr. Jack Urban, who was an electrical engineer. That partnership produced the first CI system that could be used outside of the laboratory and for many years by patients. This result was a landmark in the history of CIs, and House is widely regarded as the “father” or first and foremost pioneer of the CI.
In 1966, Simmons implanted single-wire electrodes into the auditory nerve in the modiolus of a deaf-blind volunteer. This approach of course differed from that of the scala tympani implants.
Many basic studies were conducted with this patient by Simmons and his teams (Simmons, 1966; Simmons et al., 1967). The results showed that perceived pitch varied with either a change in the stimulating electrode or a relatively large change in the rate of stimulation at a particular electrode (a change of about 30 Hz), up to a rate of about 300 pulses/s. When a wide-band speech signal was presented to one of the electrodes, or when speech signals filtered into different bands were each directed to different electrodes, the patient reported speech-like percepts, perhaps from a language other than the patient's native language (he said Spanish, and his native language was English), but he could not understand what was being said. Simmons was somewhat disappointed by these results and decided to cease further studies with human subjects until animal studies could be conducted to evaluate physiological responses to a wide range of electrical stimuli, and also to evaluate in greater detail than before the safety aspects of electrical stimulation. The results from the initial experiments with the chronically-implanted human subject indicated for the first time that both the “volley” and “place” theories of pitch perception are correct, and that changes in pitch due to different rates of stimulation (the volley theory) operate over a narrow range up to about 300 pulses/s only.
Beginning in the early 1970s, a team at the University of California at San Francisco (UCSF) also investigated the feasibility and possible efficacy of single-electrode implants. The first members of the team included Robin Michelson, who was an otologist, and Michael Merzenich, who was a neurophysiologist. A few patients were implanted and the results were similar to those previously reported by House, e.g., recognition of speech was not possible for the applied devices and the studied patients.
Merzenich also conducted a series of animal experiments whose results demonstrated that different frequencies of stimulation at a single electrode in the cochlea could evoke time-locked neural responses in the auditory pathways up to about 600 Hz only (Merzenich et al., 1973). This limit in time locking was judged to be too low for representing speech, which contains important information at frequencies above 600 Hz and indeed extending up to about 6 kHz. Subsequent studies by the UCSF teams therefore were directed at the development of CI systems that could provide multiple sites of stimulation along the length of the cochlea and thereby represent frequencies above 600 Hz with the place code mentioned previously.
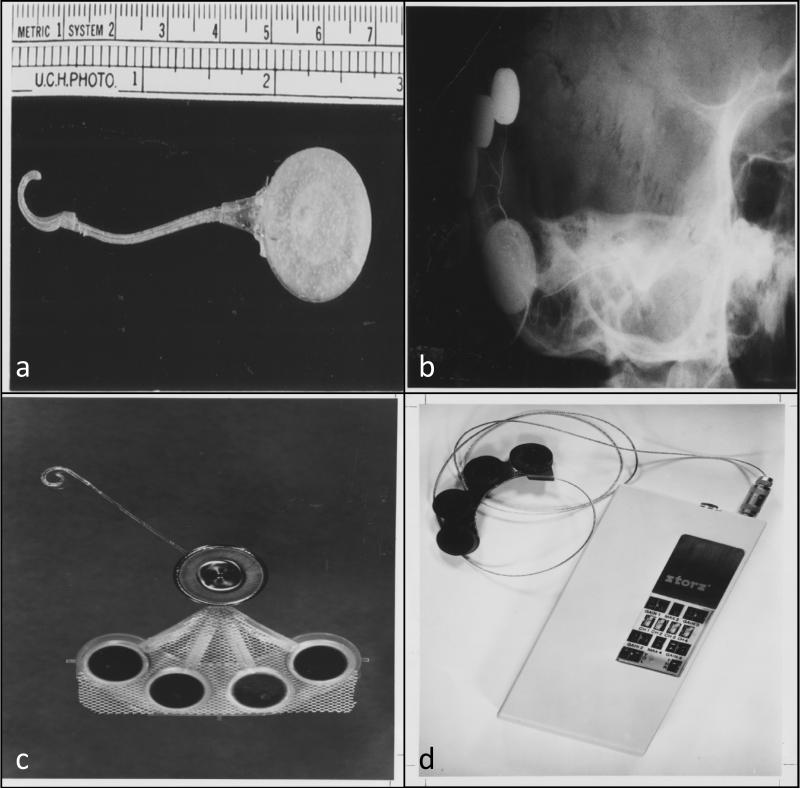
The first single-electrode and multi-electrode systems developed by the UCSF teams are shown in Figure 1. They are large and cumbersome by today's standards, but also were among the first devices that could be used by patients outside of the laboratory.
Fig 1.
The cochlear implant designed by Michelson in 1978. a) The internal portion of the device measuring 70 mm in length; b) Radiographic image of a skull with an implant in place, c) The internal portion of the implant, d) The external portion of the implant. (Courtesy of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
II.c Evaluations of and reactions to the first implants
The initial reaction to CIs by auditory scientists and by otologists other than the developers was highly critical. Many of these experts offered categorical statements that CIs could not possibly restore any useful hearing, primarily because the patterns of stimulation and neural responses provided with the CIs of the time were incredibly crude and distorted compared with the patterns and responses observed in animals with normal hearing. For example, Dr. Merle Lawrence, Ph.D., who was an eminent auditory scientist, said that “direct stimulation of the auditory nerve fibers with resultant perception of speech is not feasible” (cited in Wilson and Dorman, 2008). Many other experts expressed similar views. However, pioneers persisted in the face of this intense criticism and provided the foundations for today's devices.
A review of the changing perspectives on CIs over the years is presented in Wilson and Dorman (2008). At first, the view was highly negative, as just mentioned. By 2008, however, Gifford et al. reported that more than a quarter of their CI patients were achieving scores of 100 percent correct in tests of sentence recognition. CIs had improved so much that the standard audiological tests were no longer sensitive enough to demonstrate deficits in speech understanding. Gifford et al. called for tests with much greater difficulty to regain the sensitivity, and in essence complained that performance was too good with the contemporary CIs for meaningful measures with the standard tests.
In 1976, when CIs still were highly controversial, the United States National Institutes of Health (the NIH) commissioned a study at the University of Pittsburg to evaluate the performance (and the claims by the developers) of the first CI devices. The study was led by Dr. Robert C. Bilger, Ph.D., and included all 13 of the patients who had been in implanted in the USA as of that date. The CI devices all used a single site of stimulation in cochlea.
The results demonstrated that the CI enabled a better quality of life for each of the studied subjects and that, on average, lip-reading and speech productions scores were significantly better with the implant activated than without it. The report produced by the University of Pittsburg team is another landmark in the development of the CI, and is often called the “Bilger Report.” That report produced a fundamental change in the perception of the CI at the NIH and by many other experts elsewhere. The CI gained some respectability in the medical and scientific communities with the report, and the NIH increased its support of CI research and development substantially beginning in 1978, soon after the report was published. These events and others are described in detail in the paper by Wilson and Dorman (2008).
Although approval from the scientific community was growing, suspicion and resistance to the implant from members of the deaf community continued. Several groups, such as the World Federation of the Deaf, fought against medical treatments of deafness and argued in favor of preserving the deaf culture. In the United States, opposition to CIs became commonplace in the 1990s, and opposition to implants in children who could not provide informed consent was especially vigorous (Lane and Bahan, 1998). The main argument related to the teaching and adoption of American Sign Language (ASL) for deaf persons, which presumably enabled the persons to become members of a highly supportive ethnic group, rather than being regarded by themselves and others as impaired or disabled (Baynton, 1996). To some members of the deaf community, implantation was perceived as a form of “ethnocide,” and a threat to the efforts made by the deaf social movement. The CI was believed to be a very poor substitute indeed for the support that the community could already provide. Furthermore, Deaf studies scholars have asserted that the CI was not only unnecessary but also unethical (Lane and Bahan, 1998). Balkany et al. pointed out however that the arguments made by some advocates of the deaf culture were in fact internally contradictory: “they hold that deafness is not a disability but support disability benefits for the deaf; they maintain both that cochlear implants do not work and that they work so well that they are genocidal” (Balkany et al., 1996). In addition, ethical standards hold that the best interests of the child should certainly supersede those of a special interest group and that parents have the right and the responsibility to determine their children's best interests (Balkany et al., 1996). The test of time has alleviated most of these initial concerns as one can no longer argue that CIs are not safe and effective. Today, there is no doubt regarding the benefits of the CI and most parents of deaf children now opt to have their children implanted.
II.d Further developments leading up to today's commercially available devices
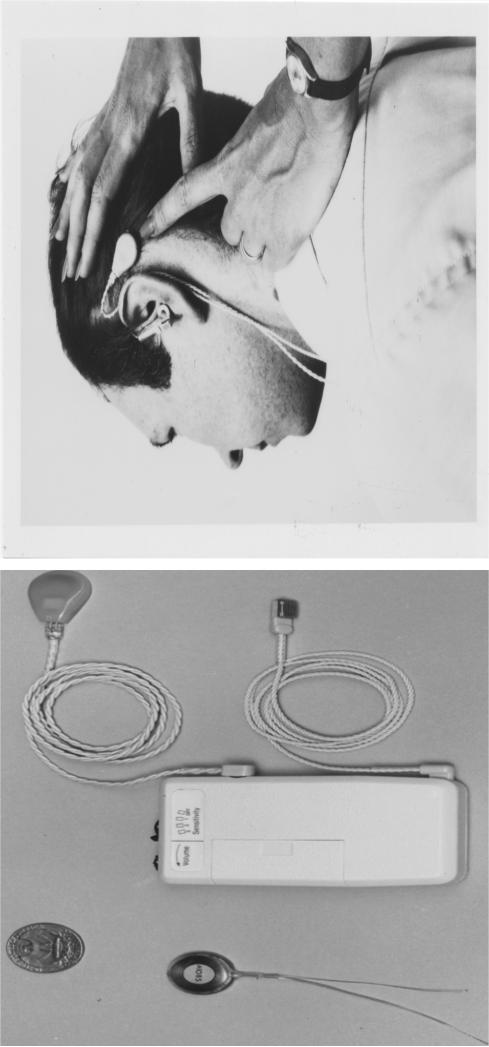
Relations between research institutions and industry strengthened during the early 1980s. In particular, House and Urban collaborated with the 3M Company to create the House/3M single channel device (Fig 2). Several groups around the world began to develop multi-site implants. In Australia, Graham Clark began studies on a multi-electrode device. Clark's work provided the foundation for early Nucleus devices, which were manufactured at the time by Nucleus Ltd. Several other international initiatives allowed for the early advances of the device with assistance of private industries: In San Francisco, the UCSF group, led by Robin Michelson and Michael Merzenich; the Utah group led by Don Eddington; and the Vienna group led by Erwin Hochmair, Ingeborg Desoyer and Kurt Burian. This history is well documented in a review by Wilson and Dorman (2008).
Fig 2.
The 3M Cochlear implant system developed by House in 1973. Left image) The internal and external portions of the device, Right image) External portion of the device placed on the patient head.(Courtesy of the American Academy of Otolaryngology-Head and Neck Surgery Foundation)
The 1990s stretched the limits of what a CI could do for its patients. From speech perception, to music appreciation, and discerning speech in loud environments, CI research continued to surprise researchers, clinicians, and patients. By 1990, children as young as 2 years of age were being selected for implantation.
An important advance with the device included spatial separation of the electrodes along the length of the cochlea and non-simultaneous stimulations, which resulted in improved understanding of speech. This concept became known as “continuous interleaved sampling” (CIS), and was incorporated in major implant systems to become the basis of many processing strategies that were subsequently developed. This produced a significant jump up in implant performance. This History is well described in Fayad et al., 2008 and in Wilson and Dorman, 2008.
In the industrial arena, companies such as Advanced Bionics, Cochlear Limited, MED-EL, and MXM emerged and grew as major cochlear implant industries in the 1990s. This relationship of industry and research led to more focused and applied studies directed at improving the benefit of implantation in patients. The continued collaborative efforts serve as steps in improvements and advances for the future. Prior to discussing the future goals, we discuss the historical events that marked the development of some of the current major industry participants in the development of cochlear implant technology.
1 - MXM & Neurelec (France)
French otologists showed interest in the development of cochlear implants dating back to the early work of Djourno and Eyries. Henri Chouard, a student of Eyries, resumed Eyries work on cochlear implants. The development of the French Cochlear Implant began in Paris in 1973 in collaboration with INSERM (Institut National de la Santé et de la Recherche Scientifique). It was here that Chouard and Mac Leod collaborated with the Bertin Company (Chouard and Mac Leod, 1973). The result was the first extra-cochlear mono-channel device, which was appropriately named “Monomac”. A processor was developed in which the speech signal was divided into frequency bands according to an empirically derived map gained from experience with unilaterally deaf implantees through comparison with the opposite hearing ear. Energy in each frequency band was encoded as a repetition rate of fixed amplitude pulses. Further work in the 1980s led to the development of the Chorimac device. This implant originally had eight channels, which later evolved into a 12-channel device.
In Paris, the speech-processing strategy originating at the University of Paris led to the development of a device with eight fixed filters. It was commercially manufactured by the Bertin Company and introduced initially in 1976 as Chorimac-8. Their first implantation was performed on September 22nd 1976 in Paris. Further improvement to the device in 1982 resulted in a 12-channel implant named the Chorimac-12. This was a turning point for the team as the technology was one of the first speech-processing strategies to use a constant rate of stimulation on each electrode (Chouard et al., 1985 a,b).
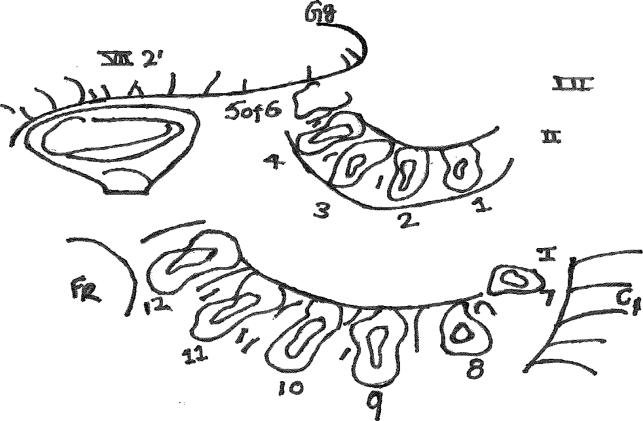
Chouard and his associates arduously implanted 12 electrodes through 12 separate openings into the cochlea (Fig 3). A considerable variability in outcomes was reported for this prosthesis in comparison to other devices in development at that time. For example, it was noted that place pitch information was poorly transmitted. Since standardized open set words were not used, it is not clear to what extent open-set speech could be recognized by the users of this early device. Two major problems with this device were difficulty of implantation and the large size of the external unit. However, the main achievements were summarized at the time by Chouard: Vowels were well recognized, consonant voicing was well differentiated, and different fricatives could be distinguished as well. (Chouard, 2010).
Fig 3.
Figure drawn by Chouard in 1973 representing the multiple cochleostomies performed on the promontory of the cochlea from the aspect of the middle ear. Structures are labeled: facial nerve (middle ear segment- (VII 2); Internal carotid artery- (C); Geniculate ganglion- (Gg); Basal turn of Cochlea- (I); Second turn of Cochlea- (II). Courtesy of PR Chouard
In Lyon, the Chorimac implant with its speech processing strategy were studied by Morgon and colleagues (Morgon et al., 1984). His team worked with two implanted post-lingual deaf adults. Although the two patients demonstrated a trend for improved word recognition with the implant, the results were not statistically significant. Research in Lyon by Berger-Vachon et al., in 1992 also focused on developing a computer model for speech processing, where the spectral composition could be varied and tested on subjects to suit their pitch perception variation.
In 1986, Bertin's corporate patent was acquired by MXM. The young company was founded and owned by engineer Guy Charvin. The company developed slowly and launched its first cochlear implant (DX-10) in 1992. Today, MXM is a holding company owning the CI manufacturer, Neurelec, which has been developing new implants under the model name of Digisonic. An Auditory Brainstem Implant (ABI) and a binaural CI have also been developed by Neurelec.
2 - MED-EL GmbH (Austria)
The development of CIs at the Technical University of Vienna began with the request of Kurt Burian, the head of the ENT-clinic, to Ervin Hochmair (Hochmair, 2012). With the help of Ingeborg Desoyer, they gathered the information needed for a first concept of a CI with the goal to design a device which would provide some auditory input without undue burden to the CI patient. Their system included two parts: An external unit and an implanted receiver and stimulator: the external unit contained the sound processing and stimulation parameter generation;the implanted unit was powered via a transcutaneous link that received encoded acoustical information and generated the corresponding stimulation current at the different contacts of the electrode array. The transcutaneous link was comprised of two inductively coupled coils: One implanted and connected to the implant circuitry, and other an external sender coil. This approach left the skin intact, as opposed to a percutaneous plug, which would have facilitated research but would have constituted a hazard to the patient (Zierhofer and Hochmair, 1992).
At the time of development, the scala tympani had been established as a stimulation site by House and Simmons and the Hochmair team pursued this strategy for their own device. Together with Burian, the team applied for a research grant in the amount close to 10,000 Euros at the Austrian research council in 1975, and the development of a first CI model soon followed. Eight Teflon insulated platinum-iridium wires were molded into a silicone carrier for ease of insertion. To overcome biocompatibility issues, the feed through consisted of gold/nickel-chrome paths on the glass substrate (Burian, 1979). The manufacturing of the implants took place in the Semiconductor Lab of the “Institut für Allgemeine Elektrotechnik” of the Technical University at Innsbruck. For sound processing, it seemed reasonable for the team to use of the well-known vocoder principle (Weisenberger et al., 1989). This required several stimulation sites, multichannel processing, and a multichannel implant. Eight channels appeared to be a reasonable compromise between complexity of the device and research possibilities (Hochmair, 2012).
After little more than 18 months of development time, several implants were completed and tested. The first implantation took place on Dec. 16, 1977. Out of the two devices that had been implanted at the time by the team, one was functional (Hochmair, 2012). Several sound processing schemes were tested for this patient: from single channel quasi-analog-stimulation to more complex patterns, but no open speech understanding could be attained. In the course of the trial sessions, it appeared that with one particular single broadband channel, some rudimentary speech understanding was possible and at least some support of lip reading could be obtained. With this finding, the team concluded that it might be well worth trying some device featuring just one, or two stimulation channels, while being much more transparent to analog stimulation signals than was possible with pulsatile stimulation at a sampling rate of 10 kHz. This new approach changed the direction of their research completely.
In 1978, the Vienna team had designed and manufactured a passive single channel broadband analog implant. This simple device was biocompatible after molding it in epoxy used in the construction of pacemakers. It was easy to produce, since no complex hybrid circuit and no complicated hermetic housing was necessary, and two or four electrodes could be combined to a two- or four-channel implant, which was compliant with any type of analog signal, and even simultaneous analog signals. Several years later the epoxy case was replaced by a ceramic housing. These multichannel implants became the workhorse for future years, and provided the group with ample possibilities to experiment with different processing strategies. The first implantation with such a device took place in May 1978. Some open speech understanding could already be demonstrated in this same year. One interesting advantage of the Vienna device was the low power consumption of the broadband analog system (Hochmair, 2012).
In 1981, the 3M Corporation negotiated a license and support agreement involving the commercialization of their cochlear implant system. The 3M Company had some experience with the medical application of their contact lens business, but they intended to enter the market for hearing devices with the cochlear implant as their flagship product. 3M was already marketing the single-channel House device, and had high expectations for the new Vienna implant. However, a complete re-design with replacement of the intra-cochlear electrode with an extra-cochlear electrode resulted in speech performance below their earlier result. After only a few years with the 3M Corporation, the Hochmair group established its own company known as MED-EL in 1990. The company comprised three employees, two engineers for the manufacturing and one salesperson. Ingeborg Desoyer, one of the original team members, resigned from her academic career to head the new MED-EL company. Hochmair maintained his position at the university as head of the Institute of Applied Physics, where basic cochlear implant research was expanded by an agreement between the University and MED-EL and by financial support from the Austrian Research Fund. In order to improve processing strategies, the team incorporated Wilson's CIS-strategy (Hochmair 2012) to the MED-EL device. Within a year, the newly designed eight-channel implant for pulsatile stimulation, the COMBI 40, and a wearable processor were made available for implantation (Von Wallenberg et al., 1990, Zierhofer et al., 1993, Teissl et al., 1998). This first multichannel system distributed by MED-EL proved successful and laid the basis for further developments. Today, MED-EL is still a private enterprise based in Innsbruck and directed by Desoyer Hochmair Ingeborg. Their cochlear implant devices are FDA approved. The company has developed several other devices including brain stem implants and electroacoustic stimulation (EAS) devices for patients with residual hearing (Gstoettner et al., 2009).
3 - Cochlear Ltd. (Australia)
In the mid-1970s, the single-electrode device was developed in Los Angeles, and some scientists and surgeons were asserting at meetings that a more complex multi-electrode system may not be needed. Such doubts did not prevent Graeme Clark and his team in Melbourne, from creating a multi-channel electrode. In 1971, several studies at the University of Melbourne began to investigate the limitations of using the rate of electrical stimulation to code speech and other sounds (Clark et al., 1973 and Clark, 2003). The results from this research suggested that location along the cochlea dominates over the rate of pulse delivery. This research helped highlight the emerging principle shared by other groups that a multiple-channel rather than a single-channel implant should be developed.
In 1973, Clark partnered up with the physicist David Dewhurst, to help him with the electrical aspects required in creating a prototype for what they later called the Bionic Ear (Clark, 2003). With this partnership, Clark was able to focus on technical issues, such as the type of electrode array that would be inserted into the cochlea. While on the beach, Clark had collected some turban-shells, which have shape similar to that of the cochlea. He observed that grass and fine twigs with increased flexibility at their distal end had an easier time making it to the top turn of the turbon shells. It was here that he was inspired to design an electrode with graded stiffness in order to allow full insertion into spiral anatomy of the cochlea and still allowing adequate force to be exerted on the electrode at its base (Clark, 2000). The University of Melbourne's multi-channel prototype involved an array of 20 electrodes: 10 to act as active electrodes and 10 to act as interleaved common grounds.
By 1976, the search for deaf recipients as candidates to receive the first Australian implant was underway. Theoretical surgical techniques were also being perfected. The implantation surgery was performed on about 50 cadaveric temporal bones before it was conducted on a living individual, who had become completely deaf after a traumatic head injury as an adult. It was on August 1st, 1978 when the University of Melbourne's first multiple channel CI was implanted into this post-linguistically deaf volunteer patient (Clark, 2003).
The Melbourne multi-channel implant was a success, but several obstacles still remained before this implant evolved into today's Bionic Ear. First, much effort was placed into making the speech processor smaller and more portable. Research funding was running low, so the team sought help from the Australian government as well as industry, to bring this new implant to the public in great quantities (Clark 2000). The Australian team partnered with Nucleus to market their multi-channel implant. A competition soon began between the 3M single-channel device and the newer multichannel devices to determine which product would provide the most benefit for speech understanding.
By 1985, results from clinical trial centers showed that the Nucleus multiple-channel device provided most people with considerable help with lip-reading, but it also gave them some understanding of speech using electrical stimulation alone, a result which had not been achieved with the 3M single-channel device (Dowell 1986). This information was presented to the FDA, and in October 1985, the Nucleus device became approved for use in treating post-lingually deaf adults (Clark, 2003). The US subsidiary, Cochlear Corporation, took the initiative in encouraging certain centers in the US to set up special training courses so that surgeons who were not familiar with the surgical approach were trained to perform the procedure with a minimal of risk to the patient..
In 1995, Cochlear Limited was listed on the Australian Stock Exchange as a separate company. Since then, Cochlear Limited has continued in the ventures began by its predecessor Nucleus (Cochlear Pty Limited). Today, Cochlear Limited manufactures not only cochlear implants, but also brain stem implants and hybrid EAS devices for patients with residual hearing.
4 - Advanced Bionics Corp. (USA)
Original developments at the University of California, San Francisco began with the efforts of Francis Sooy to bring together the collaboration between Robin Michelson and Michael Merzenich. Michelson, a clinical pioneer, and Merzenich, a talented basic scientist with a solid foundation in neurophysiology, was an integral element in the development of the UCSF cochlear implant team. Michelson was recognized for implanting a single-channel device into a congenitally deaf woman. She demonstrated auditory sensations from stimulation, as well as pitch perception for stimulus frequencies less that 600 Hz. Unfortunately, This patient had no word recognition. His pioneering work was presented, but not well-received at the 1971 annual meeting of the American Otological Society (Michelson, 1971 and Merzenich et al., 1973).
Merzenich performed his studies of recording the response properties of single units in the cat inferior colliculus in response to sound stimulation from one ear and electrical stimulation from the other ear of unilateral implanted cats. This was an effective model as the spatial attenuation of current along the cochlea would be determined through knowing the site of the response from the unit's acoustic input from the contralateral ear (Merzenich et al., 1973). His results showed that with bipolar stimulation from electrodes on a mold of the scala tympani could be localized to separate groups of nerve fibers (Merzenich et al., 1974).
The team soon began to focus on developing the bipolar multi-channel array that would be inserted into the scala tympani. With the help of several NIH grants, the UCSF multi-channel device was created and first implanted in the early 1980s. Further studies were undertaken to measure the biocompatibility of an improved electrode array for human insertion through long- term implantation in the cat (Leake-Jones and Rebscher, 1983).
Following the initial research at UCSF, Storz Medical Instruments collaborated with UCSF research group to develop a prototype device. The partnership also included the collaboration with the Research Triangle Institute (RTI) in North Carolina. Investigators at RTI were developing processing strategies for both single and multi-site implants, which were sponsored by the NIH and with UCSF Department of Otolaryngology as one of the collaborating clinical partners. The results from these studies showed promising outcomes in implanted patients (Merzenich et al., 1987). However, the team required more support to fully develop and market the UCSF multi-channel implant. This was the beginning of a partnership created Alfred E. Mann, which involved the Advanced Bionics Company.
The Advanced Bionics Company originally evolved from two medical device companies, which specialized in pacemakers and micro-infusion systems. Alfred E. Mann was the owner of several companies, including MiniMed Inc. in Sylmar, CA. MiniMed Inc. took part in developing a new multichannel device, which included the electrode array originally developed by UCSF research and clinical teams and an “interleaved pulses” processing strategy originally developed at RTI. The starting design for the electrode array was provided by UCSF. The starting design for the sound processor, transcutaneous transmission system, and implanted electronics was provided by the RTI. At the start, Mann appointed Jeffrey H. Greiner to lead an organization of seven engineers and scientists into making the first development team in Advanced Bionics (AB). The multi-channel processor was released with the Clarion cochlear implant, which had a pre-formed electrode array for use in adults. Clinical trials began at UCSF in 1991, and in 1996 the FDA approved the AB device. The Clarion sound processor had a multiprogram processor with a unique single headpiece design, independent volume and sensitivity controls, and in 1997 was approved for use in children.
By 2001, the launch of the CII Bionic Ear implant and HiFocus electrode allowed for the advantage of being upgraded through software programming for advancing hearing performance without additional surgery. In 2002, the launch of the T-Mic™ microphone gave recipients wireless connectivity to cell phones, headsets, and MP3 players. Some controversy arose during this same time period regarding the usage of a silastic positioner, which was suggested as a possible cause to several cases of meningitis, that were most likely due to inner ear trauma or abnormal sealing of the cochleostomy.
In 2003, the HiRes 90K implant was introduced with the Harmony CI device being released shortly thereafter in 2006. In 2004, Boston Scientific acquired the Advanced Bionics Company. This acquisition was short-lived as Advanced Bionics again became a separate entity as it was sold back to Al Mann following a disagreement with Boston Scientific that ended up in court for a legal decision that favored Al Mann In 2009, Advanced Bionics was acquired by Sonova Holding AG.
III. Ongoing research and the future
Over the past several decades, developments in the field of microelectronics and advances in signal processing techniques not only helped make CIs a reality, but led to increased efficiency and effectiveness of these CI devices in patients. The early efforts in the development of CIs led to the multi-channel electrode. More recent advances in user performance were gained thorough improvements in surgical approaches and by the development of elaborate speech coding strategies. The development of the n-of-m (Wilson et al., 1988), the continuous interleaved sampling (CIS) (Wilson et al., 1991), and spectral peak (SPEAK) (Skinner et al., 1994) strategies allowed improvements in CI performance.
While a substantial progress has already been made, the CIs are not perfect and further challenges remain. Recent and future research efforts will include several major approaches: preservation of hearing post-implantation, the improvement of the electrode design, novel strategies to increase the number of functional channels on the CIs, the design of novel coding strategies, the development of a less traumatic insertion of the electrode, as well as the use of stem cells and various drugs to retain and regenerate neurons in the cochleae.
III.a Hearing preservation
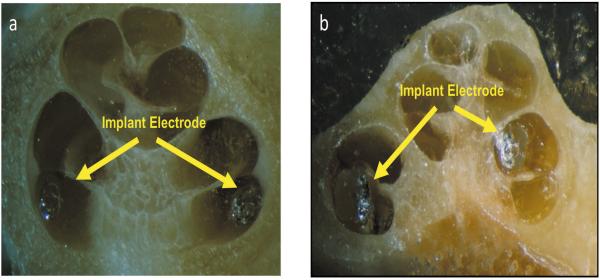
Preserving residual hearing in the CI patients has been an important goal as more institutions across the world are implanting children as young as 1 year of age (Yoon, 2011). Many patients with residual hearing (generally in low frequency range) are also becoming candidates for implantation (Balkany et al., 2006). Temporal bone studies began to evaluate various electrode designs and resulting trauma to cochlear structures (Fayad et al., 2000, Nadol et al., 2001). A grading system was established (Eshraghi et al., 2003) and used by various cochlear implant research teams (Adunka et al., 2004, Berrettini et al., 2008, Cervera-Paz and Linthicum, 2005). The grading system ranged from 0 to 4 (Eshraghi et al., 2003): With grade 0 having no macroscopic damage to grade 4 having evidence of fractures to the osseous spiral lamina or modiolus (Fig 5).
Fig 5.
Photograph of cryo-histological sectioned surfaces from two fresh temporal bones that underwent cochlear implantation. a) Grade 0- with no macroscopic damage; b) Grade 4- where a fracture of osseous spiral lamina can be seen. (see Eshraghi et al. Table-1, this issue)
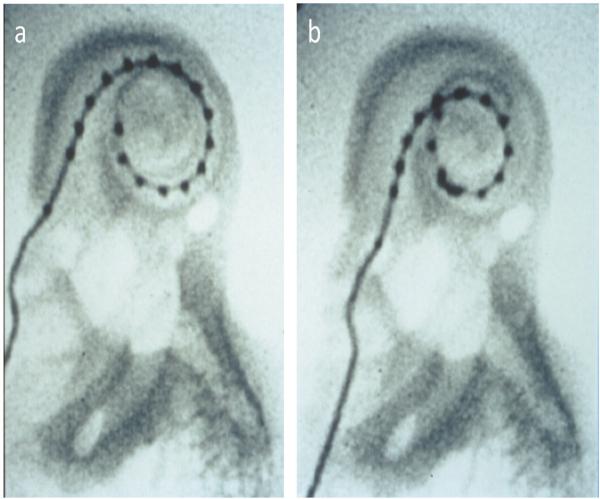
These studies, combined with video fluoroscopic evaluation (Fig 6) of the dynamics of insertion, helped to improve the surgical techniques used by the surgeons to improve the design of the CI electrodes (Balkany et al., 2003; Roland et al., 2000; Fayad and Linthicum, 2006; Eshraghi et al., 2004). One of the applications of these hearing preservation techniques was to improve the short and long-term expectation of newer hybrid or electro-acoustic devices that are at present under clinical evaluation. These newer EAS devices are a combination of hearing aids and cochlear implants, and are designed for patients who still have residual hearing in the lower frequencies. MED-EL GmbH (Gstoettner et al., 2008) and Cochlear Corporation are independently performing clinical trials on such hybrid devices (Gantz et al. 2005).
Fig 6.
Videofluoroscopic evaluation of two stages of an electrode insertion. These images represent two pictures taken during the videofuoroscopy evaluation of the insertion characteristics of a Nucleus contour electrode array. Before (a) and after (b) removal of the insertion stylet, the electrode is positioned at a more perimodialar position (compare a with b).
Various studies have focused on measuring mechanical insertion forces and insertion trauma caused to the cochlea from different multichannel cochlear implant electrodes (Rebscher et al., 2008, Roland, 2005, Gstoettner, 1997, O'Leary et al., 1991, Welling et al., 1993, Adunka et al., 2004; Nadol et al., 2001, Gstoettner et al., 2004; Fraysse et al., 2006; Helbig et al., 2011). Efforts to reduce trauma and improve hearing preservation included improvements in the surgical approach (see e.g. Gantz and Turner, 2003) and the development of improved more atraumatic CI electrode arrays. Today, small and more compliant electrodes have been designed and produced, so that insertion into the cochlea provides a reduced risk for insertion-associated trauma to cochlear structures.
Several cochlear implant models have been designed over the last 10 years. In perimodiolar design, the placement of the stimulating electrodes is closer to the long modiolus and auditory nerve, which reduces the stimulation thresholds. In another electrode design, the tip of the electrode is softer and the contact with the outer cochlear wall (i.e area of the spiral ligament) is intended to be less traumatic. Several studies have been performed, which include the use of commercial and experimental perimodiolar electrode models (Eshraghi et al., 2003, Wardrop et al., 2005, Adunka et al., 2006). A study conducted by Balkany et al. (2002) demonstrated that various devices evaluated were effective at placing the electrodes close to the modiolus, but that each had sections of the electrode array where electrodes were pushed slightly away from the bony wall of the modiolus. The CI manufacturers have addressed these issues by designing smaller, softer, and more flexible electrodes. Furthermore, changes in insertion techniques may lead to less insertion caused trauma and hence, improvement in residual hearing preservation.
The possible traumatic effect of the cochlear implant electrode insertion has been evaluated in humans (e.g. Nadol et al., 2001). The effects measured were small and predictions on outcome measures were difficult. Recently, animal studies have been used to better study the effect of insertion trauma on spiral ganglion neuron survival. The pattern of hearing loss caused by electrode insertion trauma has been studied in rats (Eshraghi et al., 2005) and guinea pigs (Eshraghi et al., 2006). In these studies, electrode insertion damaged cochlear function. Functional changes had an immediate and a delayed component. The insertion of a CI electrode array causes direct tissue trauma and cell loss via both necrosis and apoptosis (the acute component). In addition, the results show generation of major molecular events that may contribute further to a loss of residual hearing on days following trauma (the delayed component of hearing loss). These events include oxidative stresses and release of pro-inflammatory cytokines, activation of the caspase pathway resulting in apoptosis, and/or generation of proapoptotic signal cascades via the mitogen-activated protein kinases/c-Jun-N-terminal kinases (MAPK/JNK) (Eshraghi et al., 2011). Damage to the cochlea can occur on both cellular and molecular levels and do not cause detectable macroscopic damage to cochlear structures when “soft techniques” and proper surgical measures were used. Programmed cell death caused by this cellular and molecular damage may explain the loss of residual hearing observed in some patients after cochlear implantation (Adunka et al., 2010, Eshraghi et al., 2006).
Currently, several otoprotective drugs such as dexamethasone (Vivero et al., 2008, Eshraghi et al., 2007, James et al., 2008) and AM-111 (Eshraghi et al., 2007, Eshraghi et al., 2011) are under evaluation to test their efficacy against inner ear electrode insertion trauma. Novel techniques of stimulation using infrared nerve stimulator are also under investigation (Izzo et al., 2006, Richter et al., 2011a). Since the optical fibers coupled to the laser do not require direct contact with the neural tissue, such implants open the door to even less traumatic ganglion cell stimulation (Rajguru et al., 2010b).
III.b Optical stimulation of auditory neurons
In recent years, optical methods to manipulate excitable cells have been explored and have become an important tool for the studies of the nervous system. The techniques require that the target tissue is sensitized by light. This can be achieved in several ways: By introducing and expressing the genes for light-sensitive ion channels into the cells (also known as optogenetics), by directly introducing chemicals such as caged neurotransmitters to the cells, or by utilizing the endogenous sensitivity of cells to light (Callaway and Yuste, 2002; Hirase et al., 2002; Boyden et al., 2005; Wells et al., 2005; Izzo et al., 2006; Rajguru et al., 2010a). Pulsed infrared radiation (IR) can excite tissues without any pre-treatment. Application of short pulses of long-wavelength IR result in transient temperature changes that stimulate the cells (Wells et al., 2007; Dittami et al., 2011; Shapiro et al., 2012). Infrared neural stimulation (1450-1550, and 1844-2120 nm) has great potential for basic science investigations and as a new approach for therapeutic interventions such as cochlear implants (Richter et al., 2011a). The potential mechanism and further application of pulsed IR in the cochlea is reviewed by Goyal et al. (Goyal et al., 2012) in the same issue.
Pulses of IR radiation are delivered via an optical fiber coupled to a diode laser. No direct contact between the optical fiber and the target tissue is required for stimulation, and the excitable cells in the beam path are stimulated. The most attractive feature of infrared neural stimulation is the improvement in spatial selectivity of stimulation (Richter et al., 2011b). The optical radiation does not spread significantly in the tissue, when compared with conventional electric current (Izzo et al., 2007c), and it can be further focused using optical lenses. This ability to confine the infrared stimulation to a smaller portion of neurons may allow for more discrete neural stimulation with improved spatial resolution.
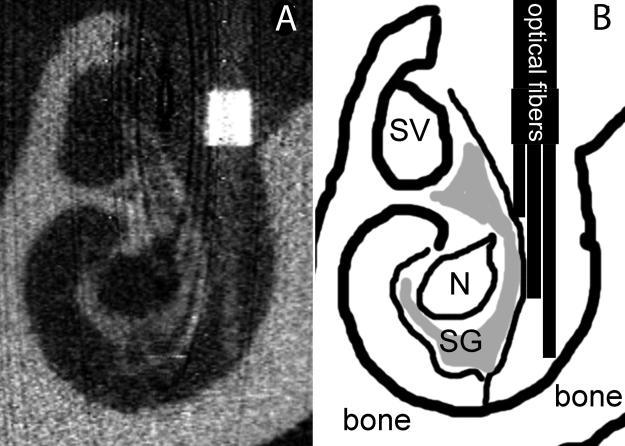
While cochlear implants remain the success story among neuroprostheses, they still have room for improvement. In particular, the performance of cochlear implant users in noisy listening environments, the performance with tonal languages, and the appreciation of music need significant improvement. Infrared neural stimulation of a selective population of the spiral ganglion can be extremely beneficial and may improve user performance in noisy listening environments and provide better music appreciation by providing more independent channels to encode the acoustic information. The efficacy of infrared to stimulate cochlear neurons in gerbils, guinea pigs and cats has been demonstrated (Izzo et al., 2007a; Izzo et al., 2007b; Izzo et al., 2008; Rajguru et al., 2010b; Rajguru et al., 2011). Experiments are currently underway to investigate the safety and efficacy of a chronic optical cochlear implant in a cat model. As shown in figure 7, a method to chronically implant a multi-channel light delivery system to stimulate an animal over extended periods of time has been developed in Dr. Richter's laboratory in collaboration with Lockheed Martin Aculight Corporation. The data obtained from these studies will verify that the smaller spread of excitation can result in a separation of the independent channels to stimulate the cochlea. The experiments will also provide the safe repetition rate and energy levels for chronic stimulation. It remains to be seen if the neural responses evoked by the optical stimulus correlate with a meaningful perception of sound. Preliminary results obtained with a single channel implant do not suggest any damage caused by the long-term stimulation (Robinson et al., 2011). The implant has been in place for only a short time and has been used to stimulate the cochlea repeatedly for this time. It should be emphasized that that the design of the light delivery system as currently presented is not a prototype for a human cochlear implant based on infrared neural stimulation. The current design instead serves to determine basic parameters for laser stimulation that can be the basis for the future parameter space for an implantable human prototype. Infrared radiation of the cochlear neural structures will likely take advantage of the tonotopic organization of the cochlea and will stimulate selected neuron populations along the cochlea to convey frequency information.
Fig 7.
A three-channel light delivery system with side-firing optical fibers was inserted into the cochlea via a cochleostomy created near the round window niche. The light delivery system was stabilized with dental acrylic. A) Shows a micro-Computed Tomography reconstructed section of a cat cochlea with the placed three-channel light delivery system (optical fibers). B) This is a sketch of panel A. (Courtesy: Drs. Claus-Peter Richter and Suhrud M. Rajguru).Structures that can be identified are labeled: SV=scala vestibuli, N=auditory nerve, SG=spiral ganglion, bone=otic capsule bone.
III.c Protection, generation, and replacement of neural structures in the cochlea
CIs continue to provide a great benefit to the congenitally deaf and those individuals with profound sensorineural hearing loss. However, it is possible that the progressive degeneration of auditory neurons over time may compromise the function of CIs (Hardie and Shepherd, 1999). In addition, the future advances in CI technology such as spatially restricted stimulation with infrared stimulation of spiral ganglion neurons (Rajguru et al., 2010a), placement of intra-neural electrode arrays (Middlebrooks and Synder, 2008), and the development of advanced stimulation strategies, can further benefit from efforts at replacing degenerated spiral ganglion neurons. Several researchers have investigated the ability of stem cells to replace damaged hair cells after injection of these stem cells into the damaged cochlea of animals (Parker, 2011). The results suggest that stem cells transplanted in the cochlea can survive. Cells such as neural stem cells may be efficacious in replacing lost hair cells and/or neurons. The current results suggest that only a fraction of the injected stem cells develop hair cell characteristics.
On the other hand, various investigations have identified the cellular and molecular mechanisms underlying the degenerative changes of the cochlear spiral ganglion neurons. Efforts to manipulate these mechanisms may allow researchers to prevent the degeneration of these neurons following hair cell loss (Roehm and Hansen, 2005). Other strategies include directing the differentiation of embryonic and adult neural stem cells into neural cell types that extend axons toward the hair cells (reviewed by Coleman et al., 2007). This has led to exciting new research aimed at promoting the differentiation of stem cells into spiral ganglion neurons. However, more work is required to identify the best means of directing stem cell development and differentiation into the specialized neurons that exist in the cochlea, as well as to determine whether their axons can form synapses with hair cells, leading to signaling in the central auditory pathway.
While most of this work has been limited to animal models, the continued efforts of many research groups with stem cell therapy targeting development and regeneration of cells may promise a novel solution for hearing loss. Excellent reviews have summarized these topics for readers interested in more detail should consult these (Staecker, 2005, Roehm and Hansen, 2005, Fritzsch et al., 2007, Coleman et al., 2007, Parker 2011, Collado et al., 2008, Brigande and Heller, 2009).
A related and promising area of research is gene therapy, which recruits undamaged endogenous cells at the location of damage within the cochlea to develop into hair cell like cells. The principle relies on the discovery that expression of the basic helix-loop- helix transcription factor Atoh1 is sufficient to promote supporting cell trans-differentiation and restoration of hair cells (Akazawa et al., 1995; Bermingham et al., 1999; Shimizu et al., 1995, Zheng et al., 2000, Kelley 2006). Several investigators have used adenoviral vectors to deliver the Atoh 1 gene in animal models and demonstrated improvement in cochlear function and hair cell recovery at least in the low frequency region (Staecker et al., 2011, Izumikawa et al., 2005).
The challenge also remains to deliver the stem cells and/or various neuroprotective drugs directly into the inner ear. Current research in progress includes delivery of drugs via hydrogels or nanoparticles. Other approaches include direct drug-delivery using osmotic pumps or a reciprocating perfusion system (Borenstein, 2011) as well as modifications to current implant electrode arrays. While these drug-delivery techniques are currently at an early stage of development, their success in delivering various otoprotective agents will potentially aid the efforts to alleviate various hearing and balance disorders.
IV. Concluding remarks
As microchip technology advances at an exponential rate, the size of both internal and external devices is expected to be miniaturized. In addition, advances in directional microphone technology will improve the design of future devices. Combined, the improvements in technology (including laser technology) and utilization of robotic electrode insertion to reduce the electrode insertion trauma and improve surgical accuracy, will achieve the goal of having a completely implantable device with a significant improvement in battery life (Bell et al., 2012). Better speech processing strategies will continue to improve the quality of sound perceived and improve the perception of music by cochlear implant recipients. Furthermore, bilateral implantation using a single internal device and a single processor (Eshraghi et al., 2012) will allow a true binaural stereophonic hearing with excellent sound perception in noise.
Finally, continued collaborations between institutions, industry and governments worldwide will make cochlear implantation affordable for all. Cost-saving initiatives such as more efficient and affordable microprocessors, as well as streamlining the post-operative care and rehabilitation process may play a part in making the cochlear implantation an affordable possibility for all CI candidates around the globe.
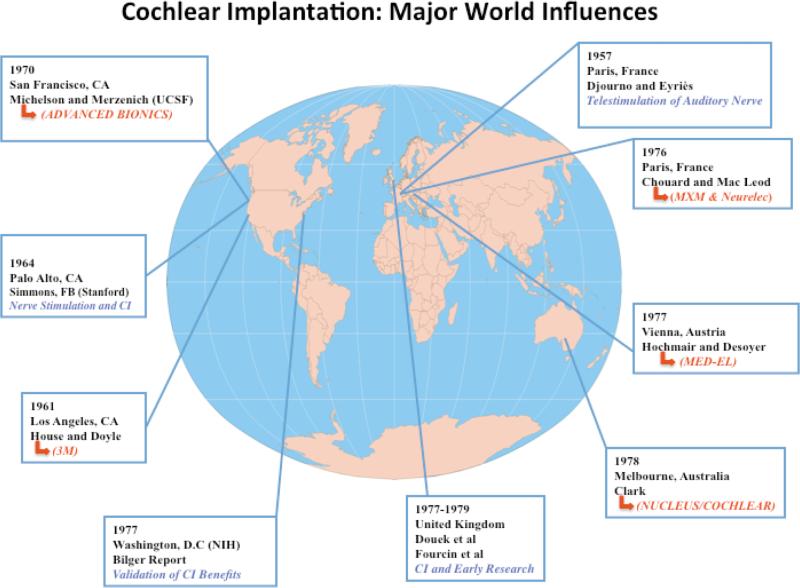
Fig 4.
The success of the cochlear implant was a worldwide mission. Some important influences are depicted above, with years representing the time of first cochlear implantation and/or the time period of significant research contributions. Some of the major companies which later originated from the early works of each team are also depicted in red.
Literature Cited
- Adunka OF, Pillsbury HC, Buchman CA. Minimizing intracochlear trauma during cochlear implantation. Adv Otorhinolaryngol. 2010;67:96–107. doi: 10.1159/000262601. [DOI] [PubMed] [Google Scholar]
- Adunka OF, Pillsbury HC, Kiefer J. Combining perimodiolar electrode placement and atraumatic insertion properties in cochlear implantation -- fact or fantasy? Acta Otolaryngol. 2006;126(5):475–482. doi: 10.1080/00016480500437393. [DOI] [PubMed] [Google Scholar]
- Adunka O, Kiefer J, Unkelbach MH, Lehnert T, Gstoettner W. Development and evaluation of an improved cochlear implant electrode design for electric acoustic stimulation. Laryngoscope. 2004;114:1237–1241. doi: 10.1097/00005537-200407000-00018. [DOI] [PubMed] [Google Scholar]
- Akazawa C, Ishibashi M, Shimizu C, Nakanishi S, Kageyama R. A mammalian helixloop-helix factor structurally related to the product of Drosophila proneural gene atonal is a positive transcriptional regulator expressed in the developing nervous system. J Biol Chem. 4. 1995;270(15):8730–8738. doi: 10.1074/jbc.270.15.8730. [DOI] [PubMed] [Google Scholar]
- Balkany TJ, Connell S, Hodges AV, Payne SL, Telischi FF, Eshraghi AA, Angeli SI, Germani R, Messiah S, Arheart KL. Conservation of residual acoustic hearing after cochlear implantation. Otol Neurotol. 2006;27(8):1083–1088. doi: 10.1097/01.mao.0000244355.34577.85. [DOI] [PubMed] [Google Scholar]
- Balkany TJ, Eshraghi AA, Yang N. Modiolar proximity of three perimodiolar cochlear implant electrodes. Acta Otolaryngol. 2002;122(4):363–369. doi: 10.1080/00016480260000021. [DOI] [PubMed] [Google Scholar]
- Balkany TJ, Hodges AV, Goodman KW. Ethics of cochlear implantation in young children. Otolaryngology Head Neck Surgery. 1996 Jun;114(6):748–55. doi: 10.1016/S0194-59989670097-9. [DOI] [PubMed] [Google Scholar]
- Balkany TJ, Telischi FF, Angeli SI, Eshraghi AA. Tympanomental flaps. Laryngoscope. 2003;113(7):1266–1268. doi: 10.1097/00005537-200307000-00028. [DOI] [PubMed] [Google Scholar]
- Baynton DC. Forbidden signs: American culture and the campaign against sign language. University of Chicago Press; Chicago: 1996. 1996. [Google Scholar]
- Bell B, Stieger C, Gerber N, Arnold A, Nauer C, Hamacher V, Kompis M, Nolte L, Caversaccio M, Weber S. A self-developed and constructed robot for minimally invasive cochlear implantation. Acta Otolaryngol. 2012;132(4):355–360. doi: 10.3109/00016489.2011.642813. [DOI] [PubMed] [Google Scholar]
- Berger-Vachon C, Collet L, Djedou B, Morgon A. Model for understanding the influence of some parameters in cochlear implantation. Ann OtolRhinolLaryngol. 1992;101(1):42–45. doi: 10.1177/000348949210100112. [DOI] [PubMed] [Google Scholar]
- BerminghamNA Hassan BA, Price SD Vollrath MA, Ben-Arie N Eatock RA, et al. Math1: an essential gene for the generation of inner ear hair cells. Science. 1999;284(5421):1837–1841. doi: 10.1126/science.284.5421.1837. [DOI] [PubMed] [Google Scholar]
- Berrettini S, Forli F, Passetti S. Preservation of residual hearing following cochlear implantation: comparison between three surgical techniques. J Laryngol Otol. 2008;122:246–252. doi: 10.1017/S0022215107000254. [DOI] [PubMed] [Google Scholar]
- Bilger RC, Black FO. Auditory prostheses in perspective. Ann Otol Rhinol Laryngol Suppl. 1977;86(3 Pt 2 Suppl 38):3–10. doi: 10.1177/00034894770860s301. [DOI] [PubMed] [Google Scholar]
- Borenstein JT. Intracochlear drug delivery systems. Expert Opin Drug Deliv. 2011;8(9):1161–1174. doi: 10.1517/17425247.2011.588207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyden ES, Zhang F, Bamberg E, Nagel G, Deisseroth K. Millisecond-timescale, genetically targeted optical control of neural activity. Nat Neurosci. 2005;8:1263–1268. doi: 10.1038/nn1525. [DOI] [PubMed] [Google Scholar]
- Brigande JV, Heller S. Quo vadis, hair cell regeneration? Nat Neurosci. 2009;12(6):679–685. doi: 10.1038/nn.2311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burian K. Clinical observations in electric stimulation of the ear. Arch Acta Otorhinolaryngol. 1979;223(1):139–166. doi: 10.1007/BF00455078. [DOI] [PubMed] [Google Scholar]
- Callaway EM, Yuste R. Stimulating neurons with light. Current opinion in neurobiology. 2002;12:587–592. doi: 10.1016/s0959-4388(02)00364-1. [DOI] [PubMed] [Google Scholar]
- Cervera-Paz FJ, Linthicum FH. Annals of Otology, Rhinol laryngol. 2005;114:543–546. doi: 10.1177/000348940511400709. [DOI] [PubMed] [Google Scholar]
- Chouard CH, Fugain C, Meyer B. Technique and indications for the French multichannel cochlear implant “Chorimac-12” for total deafness rehabilitation. Am J Otol. 1985;6(4):291–294. [PubMed] [Google Scholar]
- Chouard CH, Fugain C, Meyer B. The Chorimac-12 A multichannel cochlear implant for total deafness. Description and clinical results. Acta Otorhinolaryngol Belg. 1985;39(4):735–748. [PubMed] [Google Scholar]
- Chouard CH, Mac Leod P. Letter: rehabilitation of total deafness. Trial of cochlear implantation with multiple electrodes. NouvPresse Med. 1973;2(44):2958. [PubMed] [Google Scholar]
- Chouard CH. Histoire de l'implantcochleaire. Annalesfrancaised'Oto-Rhinolaryngologieet de Pathologiecervico-Faciale. 2010;127:288–296. [Google Scholar]
- Clark G. Cochlear Implants: Fundamentals and Applications. Springer-Verlag; New York: 2003. [Google Scholar]
- Clark GM, Kranz HG, Minas H. Behavioral threshold in the cat to frequency modulated sound and electrical stimulation of the auditory nerve. Experimental Neurology. 1973;41:190–200. doi: 10.1016/0014-4886(73)90189-1. [DOI] [PubMed] [Google Scholar]
- Clark GM. Sounds from Silence: Graeme Clark and the Bionic Ear Story. Unwin Publishing; Australia. Allen &: 2000. [Google Scholar]
- Collado MS, Burns JC, Hu Z, Corwin JT. Recent advances in hair cell regeneration research. Curr Opin Otolaryngol Head Neck Surg. 2008;16(5):465–471. doi: 10.1097/MOO.0b013e32830f4ab5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman B, de Silva MG, Shepherd RK. Concise review: the potential of stem cells for auditory neuron generation and replacement. Stem Cells. 2007;25(11):2685–2694. doi: 10.1634/stemcells.2007-0393. [DOI] [PubMed] [Google Scholar]
- Desloges P. M. l'Abbé Deschamps (Chapelain de l'Église d'Orléans) Amsterdam and B. Morin, Paris: 1779. Observations d'un sourd et muèt, sur un cours elémentaire d'education des sourds et muèts. [Google Scholar]
- Dittami GM, Rajguru SM, Lasher RA, Hitchcock RW, Rabbitt RD. Intracellular calcium transients evoked by pulsed infrared radiation in neonatal cardiomyocytes. J Physiol. 2011;589:1295–1306. doi: 10.1113/jphysiol.2010.198804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djourno A, Eyries C. Auditory prosthesis by means of a distant electrical stimulation of the sensory nerve with the use of an indwelt coiling. Presse Med. 31. 1957;65(63):1417. [PubMed] [Google Scholar]
- Dowell RC, Mecklenburg DJ, Clark GM. Speech Recognition for 40 patients receiving multichannel cochlear implants. Archives of Otolaryngology. 1986;112:1054–1059. doi: 10.1001/archotol.1986.03780100042005. [DOI] [PubMed] [Google Scholar]
- Doyle J, Doyle D, House W. Electical stimulation of eight nerve deafness. Bulletin of the Los Angeles Neurological Society. 1963;28:148–150. [PubMed] [Google Scholar]
- Eshraghi AA, Adil E, He J, Graves R, Balkany TJ, Van De Water TR. Local dexamethasone therapy conserves hearing in an animal model of electrode insertion trauma-induced hearing loss. Otol Neurotol. 2007;28(6):842–849. doi: 10.1097/mao.0b013e31805778fc. [DOI] [PubMed] [Google Scholar]
- Eshraghi AA, Gupta C, Ozdamar O, Balkany TJ, Truy R, Nazarian R. Drs Van De Water, Laitman, editors. Biomedical engineering principles of modern cochlear implants and recent surgical innovations. Special Issue Anatomical Record: The Anatomy and Biology of Hearing & Balance. 2012 doi: 10.1002/ar.22584. [DOI] [PubMed] [Google Scholar]
- Eshraghi AA, Jolly C, Balkany TJ. Small-fenestra cochleostomy for MED-EL electrode. Cochlear Implants Int. 2004;5(2):71–75. doi: 10.1179/cim.2004.5.2.71. [DOI] [PubMed] [Google Scholar]
- Eshraghi AA, Wang J, Adil E, He J, Zine A, Bublik M, Bonny C, Puel JL, Balkany TJ, Van De Water TR. Blocking c-Jun-N-terminal kinase signaling can prevent hearing loss induced by both electrode insertion trauma and neomycin ototoxicity. Hear Res. 2007;226(1-2):168–177. doi: 10.1016/j.heares.2006.09.008. [DOI] [PubMed] [Google Scholar]
- Eshraghi AA, Polak M, He J, Telischi FF, Balkany TJ, Van De Water TR. Pattern of hearing loss in a rat model of cochlear implantation trauma. Otol Neurotol. 2005;26(3):442–447. doi: 10.1097/01.mao.0000169791.53201.e1. [DOI] [PubMed] [Google Scholar]
- Eshraghi AA. Local pre-treatment of the cochlea with AM-111 prevents electrode traumainduced hearing loss in an animal model of cochlear implantation. Triological Society. 2012 [Google Scholar]
- Eshraghi AA, He J, Mou CH, Polak M, Zine A, Bonny C. D-JNKI-1 treatment prevents the progression of hearing loss in a model of cochlear implantation trauma. Otol Neurotol. 2006;27(4):504–511. doi: 10.1097/01.mao.0000217354.88710.13. [DOI] [PubMed] [Google Scholar]
- Eshraghi AA, Nehme O, Polak M, He J, Alonso OF, Dietrich WD, Balkany TJ, Van De Water TR. Cochlear temperature correlates with both temporalis muscle and rectal temperatures. Application for testing the otoprotective effect of hypothermia. Acta Otolaryngol. 2005;125(9):922–928. doi: 10.1080/00016480510043918. [DOI] [PubMed] [Google Scholar]
- Eshraghi AA, Yang NW, Balkany TJ. Comparative study of cochlear damage with three perimodiolar electrode designs. Laryngoscope. 2003;113(3):415–419. doi: 10.1097/00005537-200303000-00005. [DOI] [PubMed] [Google Scholar]
- Fayad JN, Linthicum FH., Jr Multichannel cochlear implants: relation of histopathology to performance. Laryngoscope. 2006;116(8):1310–1320. doi: 10.1097/01.mlg.0000227176.09500.28. [DOI] [PubMed] [Google Scholar]
- Fayad JN, Luxford W, Linthicum FH. The Clarion electrode positioner: temporal bone studies. Am J Otol. 2000;21(2):226–229. doi: 10.1016/s0196-0709(00)80013-7. [DOI] [PubMed] [Google Scholar]
- Fayad JN, Otto SR, Shannon RV, Brackmann DE. Cochlear and Brainstem Auditory Prostheses “Neural Interface for Hearing Restoration: Cochlear and Brain Stem Implants”. Proceedings of the IEEE. 2008;96(7):1085–1095. [Google Scholar]
- Fraysse B, Macías AR, Sterkers O, Burdo S, Ramsden R, Deguine O, et al. Residual hearing conservation and electroacoustic stimulation with the nucleus 24 contour advance cochlear implant. Otol Neurotol. 2006;27(5):624–633. doi: 10.1097/01.mao.0000226289.04048.0f. [DOI] [PubMed] [Google Scholar]
- Fritzsch B, Beisel KW, Pauley S, Soukup G. Molecular evolution of the vertebrate mechanosensory cell and ear. Int J Dev Biol. 2007;51(6-7):663–678. doi: 10.1387/ijdb.072367bf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gantz BJ, Turner CW. Combining acoustic and electrical hearing. Laryngoscope. 2003 Oct. 2003;113(10):1726–30. doi: 10.1097/00005537-200310000-00012. [DOI] [PubMed] [Google Scholar]
- Gantz BJ, Turner C, Gfeller KE, Lowder MW. Preservation of hearing in cochlear implant surgery: advantages of combined electrical and acoustical speech processing. Laryngoscope. 2005;115(5):796–802. doi: 10.1097/01.MLG.0000157695.07536.D2. [DOI] [PubMed] [Google Scholar]
- Goyal V, Rajguru SM, Matic AI, Stock SR, Richter C-P. Drs Van De Water, Laitman, editors. Acute damage threshold for infrared neural stimulation of the cochlea: functional and histological evaluation. Special Issue Anatomical Record: The Anatomy and Biology of Hearing & Balance. 2012 doi: 10.1002/ar.22583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gstoettner W, Plenk H, Jr, Franz P, Hamzavi J, Baumgartner W, Czerny C, Ehrenberger K. Cochlear implant deep electrode insertion: extent of insertional trauma. Acta Otolaryngol. 1997;117(2):274–277. doi: 10.3109/00016489709117786. [DOI] [PubMed] [Google Scholar]
- Gstoettner W, Helbig S, Settevendemie C, Baumann U, Wagenblast J, Arnoldner C. A new electrode for residual hearing preservation in cochlear implantation: first clinical results. Acta Otolaryngol. 2009;129(4):372–379. doi: 10.1080/00016480802552568. [DOI] [PubMed] [Google Scholar]
- Gstoettner W, Kiefer J, Baumgartner WD, Pok S, Peters S, Adunka O. Hearing preservation in cochlear implantation for electric acoustic stimulation. Acta Otolaryngol. 2004;24(4):348–352. doi: 10.1080/00016480410016432. [DOI] [PubMed] [Google Scholar]
- Gstoettner WK, van de Heyning P, O'Connor AF, Morera C, Sainz M, Vermeire K, Mcdonald S, Cavallé L, Helbig S, Valdecasas JG, Anderson I, Adunka OF. Electric acoustic stimulation of the auditory system: results of a multi-centre investigation. Acta Otolaryngol. 2008;128(9):968–975. doi: 10.1080/00016480701805471. [DOI] [PubMed] [Google Scholar]
- Hardie NA, Shepherd RK. Sensorineural hearing loss during development: morphological and physiological response of the cochlea and auditory brainstem. Hear Res. 1999;128(1-2):147–165. doi: 10.1016/s0378-5955(98)00209-3. [DOI] [PubMed] [Google Scholar]
- Helbig S, Van de Heyning P, Kiefer J, Baumann U, Kleine-Punte A, Brockmeier H, et al. Combined electric acoustic stimulation with the PULSARCI(100) implant system using the FLEX(EAS) electrode array. Acta Otolaryngol. 2011;131(6):585–595. doi: 10.3109/00016489.2010.544327. [DOI] [PubMed] [Google Scholar]
- Hirase H, Nikolenko V, Goldberg JH, Yuste R. Multiphoton stimulation of neurons. J Neurobiol. 2002;51:237–247. doi: 10.1002/neu.10056. [DOI] [PubMed] [Google Scholar]
- Hochmair E. Personal communication with Authors. 2012 [Google Scholar]
- House WF, Urban J. Long term results of electrode implantation and electronic stimulation of the cochlea of man. Ann Otol Rhinol Laryngol. 1973;85:504. doi: 10.1177/000348947308200408. [DOI] [PubMed] [Google Scholar]
- House WF. Cochlear Implants. Ann Otol Rhino Laryngol. 1976;85(Suppl 27):1–93. [PubMed] [Google Scholar]
- Izumikawa M, Minoda R, Kawamoto K, Abrashkin KA, Swiderski DL, Dolan DF, et al. Auditory hair cell replacement and hearing improvement by Atoh1 gene therapy in deaf mammals. Nat Med. 2005;11(3):271–276. doi: 10.1038/nm1193. [DOI] [PubMed] [Google Scholar]
- Izzo AD, Joseph T, Walsh J, Jansen ED, Bendett M, Webb J, Ralph H, Richter C-P. Optical parameter variability in laser nerve stimulation: a study of pulse duration, repetition rate, and wavelength. IEEE Trans Biomed Eng. 2007a;54:1108–1114. doi: 10.1109/TBME.2007.892925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izzo AD, Littlefield P, Walsh J, J.T., Webb J, Ralph H, Bendett M, Jansen DE, Richter C-P. Laser stimulation of auditory neurons at high repetition rate. SPIE. 2007b;6435:64359R–64351-64357. [Google Scholar]
- Izzo AD, Richter C-P, Jansen ED, Joseph T, Walsh J. Laser stimulation of the auditory nerve. Laser Surg Med. 2006;38:745–753. doi: 10.1002/lsm.20358. [DOI] [PubMed] [Google Scholar]
- Izzo AD, Su HS, Pathria J, Walsh JT, Jr., Whitlon DS, Richter C-P. Selectivity of neural stimulation in the auditory system: a comparison of optic and electric stimuli. Journal of biomedical optics. 2007c;12:1–7. doi: 10.1117/1.2714296. [DOI] [PubMed] [Google Scholar]
- Izzo AD, Walsh JT, Ralph H, Webb J, Bendett M, Wells J, Richter C-P. Laser stimulation of auditory neurons at shorter pulse durations and penetration depths. Biophys J. 2008;94(8):3159–3166. doi: 10.1529/biophysj.107.117150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James DP, Eastwood H, Richardson RT, O'Leary SJ. Effects of round window dexamethasone on residual hearing in a Guinea pig model of cochlear implantation. Audiol Neurootol. 2008;13(2):86–96. doi: 10.1159/000111780. [DOI] [PubMed] [Google Scholar]
- Kelley MW. Regulation of cell fate in the sensory epithelia of the inner ear. Nat Rev Neurosci. 2006;7(11):837–849. doi: 10.1038/nrn1987. [DOI] [PubMed] [Google Scholar]
- Kiang NY, Moxon EC. Physiological considerations in artificial stimulation of the inner ear. Ann Otol Rhinol Laryngol. 1972;81(5):714–730. doi: 10.1177/000348947208100513. [DOI] [PubMed] [Google Scholar]
- Lane H, Bahan B. Ethics of cochlear implantation in young children: a review and reply from a Deaf-World perspective. Otolaryngology Head Neck Surgery. 1998;119(4):297–313. doi: 10.1016/S0194-5998(98)70070-1. [DOI] [PubMed] [Google Scholar]
- Leake-Jones PA, Rebscher SJ. Cochlear pathology with chronically implanted scala tympani electrodes. Annals of the NY Academy of Sciences. 1983;405:203–223. doi: 10.1111/j.1749-6632.1983.tb31634.x. [DOI] [PubMed] [Google Scholar]
- Merzenich MM, Michelson RP, Petit CR, Schindler RA, Reid M. Neural encoding of sound sensation evoked by electrical stimulation of the acoustic nerve. Ann Otolrhinollaryngol. 1973;82:486–503. doi: 10.1177/000348947308200407. [DOI] [PubMed] [Google Scholar]
- Merzenich MM, Schindler DN, White MW. Feasibility of multichannel scala tympani stimulation. Laryngoscope. 1974;84(11):1887–1893. doi: 10.1002/lary.5540841105. [DOI] [PubMed] [Google Scholar]
- Merzenich M, Kessler DK, Rebscher SJ, Schindler RA. Progress in Development and Application of the University of California at San Francisco/Storz Multichannel Cochlear Implant. Annals of Otology, Rhinology, and Laryngology. 1987;96:122–125. [Google Scholar]
- Michelson RP. The results of electrical stimulation of the cochlea in human sensory deafness. Ann Otolrhinollaryngol. 1971;80:914–919. doi: 10.1177/000348947108000618. [DOI] [PubMed] [Google Scholar]
- Middlebrooks JC, Snyder RL. Intraneural stimulation for auditory prosthesis: modiolar trunk and intracranial stimulation sites. Hear Res. 2008;242(1-2):52–63. doi: 10.1016/j.heares.2008.04.001. [DOI] [PubMed] [Google Scholar]
- Morgon A, Berger-Vachon C, Chanal JM, Kalfoun G, Dubreuil C. Cochlear implant: experience of the Lyon team. Acta Otolaryngol. 1984;(Suppl 411):195–203. [PubMed] [Google Scholar]
- Nadol JB, Jr, Shiao JY, Burgess BJ, Ketten DR, Eddington DK, Gantz BJ, Kos I, Montandon P, Coker NJ, Roland JT, Jr, Shallop JK. Histopathology of cochlear implants in humans. Ann Otol Rhinol Laryngol. 2001;110(9):883–891. doi: 10.1177/000348940111000914. [DOI] [PubMed] [Google Scholar]
- O'Leary MJ, Fayad J, House WF, Linthicum FH., Jr Electrode insertion trauma in cochlear implantation. Ann Otol Rhinol Laryngol. 1991;100(9 Pt 1):695–699. doi: 10.1177/000348949110000901. [DOI] [PubMed] [Google Scholar]
- Parker MA. Biotechnology in the treatment of sensorineural hearing loss: foundations and future of hair cellregeneration. J Speech Lang Hear Res. 2011;54(6):1709–1731. doi: 10.1044/1092-4388(2011/10-0149). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajguru SM, Hwang M, Moreno EL, Matic AI, Stock SR, Richter C-P. Optical path of infrared neural stimulation in the guinea pig and cat cochlea. In: Kollias N, Choi B, Zeng H, Kang HW, Knudsen BE, Wong BJ, Ilgner FR, Gregory KW, Tearney GJ, Marcu L, Hirschberg H, Madsen SJ, Mandelis A, Mahadevan-Jansen A, Jansen ED, editors. Photonic Therapeutics and Diagnostics VII. SPIE; 2011. [Google Scholar]
- Rajguru SM, Matic AI, Richter C-P. Optical stimulation of neurons. In: Pavone FS, editor. Laser Imaging and Manipulation in Cell Biology. John Wiley and Sons Inc; Weinheim, Germany: 2010a. pp. 99–112. [Google Scholar]
- Rajguru SM, Matic AI, Robinson AM, Fishman AJ, Moreno LE, Bradley A, Vujanovic I, Breen J, Wells JD, Bendett M, Richter CP. Optical cochlear implants: Evaluation of surgical approach and laser parameters in cats. Hear Res 1. 2010b;269(1-2):102–111. doi: 10.1016/j.heares.2010.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roehm PC, Hansen MR. Strategies to preserve or regenerate spiral ganglion neurons. Curr Opin Otolaryngol Head Neck Surg. 2005;13(5):294–300. doi: 10.1097/01.moo.0000180919.68812.b9. [DOI] [PubMed] [Google Scholar]
- Rebscher SJ, Hetherington A, Bonham B, Wardrop P, Whinney D, Leake PA. Considerations for design of future cochlear implant electrode arrays: electrode array stiffness, size, and depth of insertion. J Rehabil Res Dev. 2008;45(5):731–747. doi: 10.1682/jrrd.2007.08.0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter CP, Matic AI, Wells JD, Jansen ED, Walsh JT. Neural stimulation with optical radiation. Laser and Photonics Reviews. 2011a;5:68–80. doi: 10.1002/lpor.200900044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter CP, Rajguru SM, Matic AI, Moreno EL, Fishman AJ, Robinson AM, Suh E, Walsh JT. Spread of cochlear excitation during stimulation with pulsed infrared radiation: inferior colliculus measurements. J Neural Eng. 2011b;8:056006. doi: 10.1088/1741-2560/8/5/056006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson AM, Hwang M, Rajguru SM, Matic AI, Richter CP. Abstr Assoc Res Otolaryngol. Vol. 34. Baltimore, MD.: 2011. Histological evaluation of the cochlea following chronic infrared neural stimulation. p. 491. [Google Scholar]
- Roehm PC, Hansen MR. Strategies to preserve or regenerate spiral ganglion neurons. Curr Opin Otolaryngol Head Neck Surg. 2005;13(5):294–300. doi: 10.1097/01.moo.0000180919.68812.b9. [DOI] [PubMed] [Google Scholar]
- Roland JT, Jr, Fishman AJ, Alexiades G, Cohen NL. Electrode to modiolus proximity: a fluoroscopic and histologic analysis. Am J Otol. 2000;21(2):218–225. doi: 10.1016/s0196-0709(00)80012-5. [DOI] [PubMed] [Google Scholar]
- Roland JT., Jr A model for cochlear implant electrode insertion and force evaluation: results with a new electrode design and insertion technique. Laryngoscope. 2005;115(8):1325–1339. doi: 10.1097/01.mlg.0000167993.05007.35. [DOI] [PubMed] [Google Scholar]
- Rose SP. Preparation of enriched fractions from cerebral cortex containing isolated, metabolically active neuronal and glial cells. Biochem J. 1967;102(1):33–43. doi: 10.1042/bj1020033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro MG, Homma K, Villarreal S, Richter CP, Bezanilla F. Infrared light excites cells via transient changes in membrane electrical capacitance. Nature Communications submitted. 2012 doi: 10.1038/ncomms1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimizu C, Akazawa C, Nakanishi S, Kageyama R. MATH-2, a mammalian helix-loophelix factor structurally related to the product of Drosophila proneural gene atonal, is specifically expressed in the nervous system. Eur J Biochem. 1995;229(1):239–248. doi: 10.1111/j.1432-1033.1995.tb20461.x. [DOI] [PubMed] [Google Scholar]
- Skinner MW, Clark GM, Whitford LA, Seligman PM, Staller SJ, Shipp DB, et al. Evaluation of a new spectral peak coding strategy for the Nucleus 22 Channel Cochlear Implant System. Am J Otol. 15 Suppl. 1994;2:15–27. [PubMed] [Google Scholar]
- Staecker H. Broadening the spectrum of treatment options for SNHL. Arch Otolaryngol Head Neck Surg. 2005;131(8):734. doi: 10.1001/archotol.131.8.734. [DOI] [PubMed] [Google Scholar]
- Staecker H, Praetorius M, Brough DE. Development of gene therapy for inner ear disease: Using bilateral vestibular hypofunction as a vehicle for translational research. Hear Res. 2011;276(1-2):44–51. doi: 10.1016/j.heares.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teissl C, Kremser C, Hochmair ES, Hochmair-Desoyer IJ. Cochlear implants: in vitro investigation of electromagnetic interference at MR imaging--compatibility and safety aspects. Radiology. 1998;208(3):700–708. doi: 10.1148/radiology.208.3.9722849. [DOI] [PubMed] [Google Scholar]
- Vivero RJ, Joseph DE, Angeli S, He J, Chen S, Eshraghi AA, Balkany TJ, Van de Water TR. Dexamethasone base conserves hearing from electrode trauma-induced hearing loss. Laryngoscope. 2008;118(11):2028–35. doi: 10.1097/MLG.0b013e31818173ec. [DOI] [PubMed] [Google Scholar]
- Volta A. Asimov's Biographical Encyclopedia of Science and Technology. Doubleday & Company; Garden City, New York: 1982. Historical records documenting the first galvanic battery, “The Volta Column.” Circa 1800. [Google Scholar]
- Von Wallenberg EL, Hochmair ES, Hochmair-Desoyer IJ. Initial results with simultaneous analog and pulsatile stimulation of the cochlea. Acta Otolaryngol Suppl. 1990;469:140–149. [PubMed] [Google Scholar]
- Wardrop P, Whinney D, Rebscher SJ, Roland JT, Jr, Luxford W, Leake PA. A temporal bone study of insertion trauma and intracochlear position of cochlear implant electrodes. I: Comparison of Nucleus banded and Nucleus Contour electrodes. Hear Res. 2005;203(1- 2):54–67. doi: 10.1016/j.heares.2004.11.006. [DOI] [PubMed] [Google Scholar]
- Weisenberger JM, Broadstone SM, Saunders FA. Evaluation of two multichannel tactile aids for the hearing impaired. J Acoust Soc Am. 1989;86(5):1764–1775. doi: 10.1121/1.398608. [DOI] [PubMed] [Google Scholar]
- Wells J, Kao C, Konrad P, Milner TE, Kim J, Mahadevan-Jansen A, Jansen ED. Biophysical mechanisms of transient optical stimulation of peripheral nerve. Biophys J. 2007;93:2567–2580. doi: 10.1529/biophysj.107.104786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells J, Kao C, Mariappan K, Albea J, Jansen ED, Konrad P, Mahadevan-Jansen A. Optical stimulation of neural tissue in vivo. Opt Lett. 2005;30:504–506. doi: 10.1364/ol.30.000504. [DOI] [PubMed] [Google Scholar]
- Wever EG, Bray CW. The nature of the acoustic response: the relation between sound frequency of impulses in the auditory nerve. J Exp Psychol. 1930;13:373–387. [Google Scholar]
- Welling DB, Hinojosa R, Gantz BJ, Lee JT. Insertional trauma of multichannel cochlear implants. Laryngoscope. 1993;103(9):995–1001. doi: 10.1288/00005537-199309000-00010. [DOI] [PubMed] [Google Scholar]
- Wilson BS, Finley CC, Farmer JC, Jr, Lawson DT, Weber BA, Wolford RD, et al. Comparative studies of speech processing strategies for cochlear implants. Laryngoscope. 1988;98(10):1069–77. doi: 10.1288/00005537-198810000-00009. [DOI] [PubMed] [Google Scholar]
- Wilson BS, Lawson DT, Finley CC, Wolford RD. Coding strategies for multichannel cochlear prostheses. Am J Otol. 1991;12(Suppl):56–61. [PubMed] [Google Scholar]
- Wilson BS, Dorman MF. Cochlear implants: a remarkable past and a brilliant future. Hear Res. 2008;242(1-2):3–21. doi: 10.1016/j.heares.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon PJ. Pediatric cochlear implantation. Curr Opin Pediatr. 2011;23(3):346–350. doi: 10.1097/MOP.0b013e32834618ec. [DOI] [PubMed] [Google Scholar]
- Zheng JL, Shou J, Guillemot F, Kageyama R, Gao WQ. Hes1 is a negative regulator of inner ear hair cell differentiation. Development. 2000;127(21):4551–60. doi: 10.1242/dev.127.21.4551. [DOI] [PubMed] [Google Scholar]
- Zierhofer C, Pohl P, Peter O, Czylok T, Hochmair-Desoyer I, Hochmair E. The 8-channel cochlear implant CAP: first results. Adv Otorhinolaryngol. 1993;48:253–257. doi: 10.1159/000422593. [DOI] [PubMed] [Google Scholar]
- Zierhofer MC, Hochmair ES. Transcutaneous transmission of digital data and energy in a cochlear prosthesis system. Int J Artif Organs. 1992;15(6):379–382. [PubMed] [Google Scholar]