Abstract
Purpose
Natural killer (NK) cells are well known to be the most important effector cells mediating antibody-dependent cellular cytotoxicity (ADCC) which is an important mechanism of action of antibody drugs. We evaluated the effects of chemotherapy on the cell number and activity of NK cells from patients who received the vincristine–cyclophosphamide–doxorubicin–prednisone (VCAP), doxorubicin–ranimustine–prednisone (AMP), and vindesine–etoposide–carboplatin–prednisone (VECP) (mLSG15) or mLSG15-like (-L) regimen, which is one of the standard of cares for newly diagnosed adult T-cell leukemia–lymphoma (ATL), or the cyclophosphamide–doxorubicin–vincristine–prednisone (CHOP) or CHOP-L regimen which is another standard of care for ATL and peripheral T-cell lymphoma (PTCL).
Methods
The number of lymphocytes and NK cells, and NK cell activity, were assessed using flow cytometry and a 51Cr release assay, respectively.
Results
A total of 26 patients with untreated ATL or PTCL were enrolled, and blood samples from 25 patients were evaluable. NK cell number in ATL decreased after mLSG15/-L treatment, and the degree of decrease in the NK cell number was more prominent just before VECP therapy (Day 15–17 of each cycle) than just before VCAP therapy (Day 1 of each cycle). The NK cell number in ATL after CHOP/-L treatment also decreased. Interestingly, the NK cell activity showed a tendency to increase after the treatment. NK cell number in PTCL did not decrease by CHOP/-L regimen, but the activity was slightly decreased after the treatment.
Conclusions
These results indicate that the effects of chemotherapeutic agents on NK cells vary according to the disease type and intensity of chemotherapy.
Keywords: Antibody, ATL, Chemotherapy, NK cell, PTCL
Introduction
ATL belongs to the category of mature T/NK-cell neoplasms [1] and occurs secondary to HTLV-1 infection [2–4]. ATL frequently occurs in the HTLV-1 endemic area in Kyushu islands, the western part of Japan [5], and its prognosis is the worst among common subtypes of mature T/NK-cell neoplasms [6]. Recently, VCAP–AMP–VECP regimen (mLSG15), which was a modified version of LSG15 [7], developed by the Japan Clinical Oncology Group (JCOG) has been established as a standard of care in newly diagnosed aggressive ATL [8]. However, the results are still not satisfactory, with a median survival of 13 months and a 3-year overall survival (OS) rate of only 24 % [9]. Other mature T/NK-cell neoplasms include peripheral T-cell lymphoma, not otherwise specified (PTCL-NOS), angioimmunoblastic T-cell lymphoma (AITL), and anaplastic large cell lymphoma (ALCL). These disease subtypes are collectively called PTCL [1]. The current standard of care for PTCL is CHOP therapy including the CHOP-L regimen [10]; however, it has been reported that PTCL shows a generally poor prognosis, with 5-year OS rates of only 32 % in PTCL-NOS and AITL, except for in anaplastic lymphoma kinase (ALK)-positive ALCL, which is associated with a 5-year OS rate of 70 % [6].
In recent years, the efficacies of various therapeutic monoclonal antibody (mAb)-based monotherapies have been investigated in PTCL. These mAbs include the anti-CD52 mAb alemtuzumab [11, 12], the anti-CC chemokine receptor 4 (CCR4) mAb mogamulizumab [13–15], and the anti-CD30 antibody drug conjugate mAb, brentuximab vedotin [16]. Based on evidence indicating that a combination of the anti-CD20 mAb rituximab [17], and chemotherapy including CHOP therapy achieved a marked improvement in therapeutic efficacy in patients with B-cell non-Hodgkin lymphomas, the combination of mAbs and chemotherapy is expected to represent a promising regimen for mature T/NK-cell neoplasms.
ADCC is an important tumor cell-killing mechanism of action of mAbs including the anti-CCR4 mAb mogamulizumab, which has been approved for CCR4-positive ATL and relapsed/refractory PTCL in Japan. Mogamulizumab is a defucosylated mAb, resulting in highly enhanced ADCC by increased binding affinity to the Fcγ III receptor (CD16) on effector cells [18–20]. It has been also shown that the ADCC of mogamulizumab mainly depends on the amount of effector cells such as CD16/CD56 double-positive NK cells [19]; however, to our knowledge, there have been no reports regarding the effects of various chemotherapeutic agents on CD16/CD56 double-positive NK cells cause high ADCC or other effector cells to date. In this regard, we carried out the present study to evaluate the effects of two first-line therapies, namely the mLSG15 or mLSG15-L (mLSG15/-L) and CHOP or CHOP-L (CHOP/-L) regimens, on NK cell number and activity in newly diagnosed ATL and PTCL patients.
Materials and methods
Study design
This study was carried out in four institutions (Nagoya Daini Red Cross Hospital, Nagoya City University Hospital, Nagasaki University Hospital, and Imamura Bun-in Hospital) in collaboration with Kyowa Hakko Kirin Co., Ltd. (Tokyo, Japan) from May 2009 to November 2010. As per the study protocol, blood samples were collected at specified time points from patients with newly diagnosed ATL or PTCL receiving the mLSG15/-L regimen or CHOP/-L regimen as the primary treatment. Cell numbers of lymphocytes and NK cells, and NK cell activity, were determined by flow cytometry, and 51Cr release assay, respectively [21]. Blood samples were obtained at eight time points before the VCAP and VECP therapies in the first to the fourth cycle of the mLSG15/-L regimen, and at eight points before the first to the eighth cycle of the CHOP/-L regimen. A blood sample of 10 mL was obtained at each time point, and the measurement was terminated when the treatment was discontinued or changed to another treatment.
Blood samples were also collected from healthy adult volunteers in a clinical research institution between November and December 2009, and their NK cell number and activity were measured in the same manner.
Patients and healthy adult volunteers
Patients with newly diagnosed and previously untreated ATL (acute, lymphoma, or unfavorable chronic type) or PTCL aged 20 years or older to whom it was planned to administer the mLSG15/-L or CHOP/-L regimen were eligible for the study. The unfavorable chronic type of ATL was defined by the presence of at least one of the following three factors: low serum albumin, high lactate dehydrogenase, or high blood urea nitrogen concentration [9].
The healthy adult volunteers were aged 40 or above who were negative for hepatitis B virus surface antigen, hepatitis C virus antibody, human immunodeficiency virus antibody, or syphilis test such as rapid plasma regain and treponema pallidum hemagglutination test. The blood test for HTLV-1 antibodies was not carried out for healthy adult volunteers. They had also no past history of allergic diseases such as atopic dermatitis, bronchial asthma, or hay fever. All patients and healthy adult volunteers signed written informed consent.
Evaluation criteria and endpoint
The immune status was evaluated in all eligible patients, and variations in NK cell number and activity before, during, and after chemotherapy were determined in order to speculate as to the usefulness of subsequent mAb therapy for these diseases.
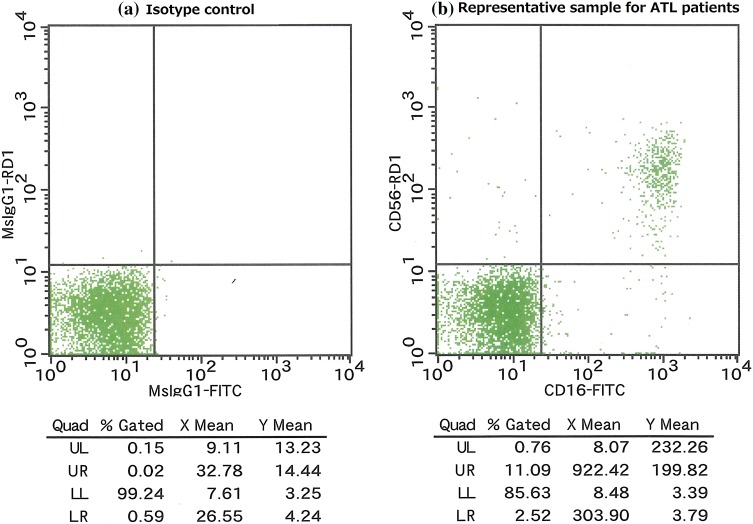
The NK cell number was obtained through measurement by flow cytometry (3-color assay for CD45/CD16/CD56 in CD3-negative fraction). Figure 4 in “Appendix” shows the representative FACS plot defined by CD16 and CD56. The lymphocyte gate was determined by side scatter-height (SSC-H) and CD45. The gated cells were displayed on a plot of CD16 versus CD56 expression. The double-positive fraction of CD16/CD56 was defined as the NK cell. The NK cell number was calculated according to the following formula:
Fig. 4.
Representative FACS plot defined by CD16 and CD56. a Isotype control and b representative sample for ATL patients
NK cell activity was obtained through measurement by 51Cr release assay (an assay using the reaction of peripheral blood mononuclear cells (monocyte and lymphocyte) and 51Cr-labeled K562 cells at an effector/target ratio of 20:1), and was calculated according to the following formula:
*(E - S)/(M - S) × 100, where E is the experimental release, S is the spontaneous release, and M is the maximum release.
Statistical analysis
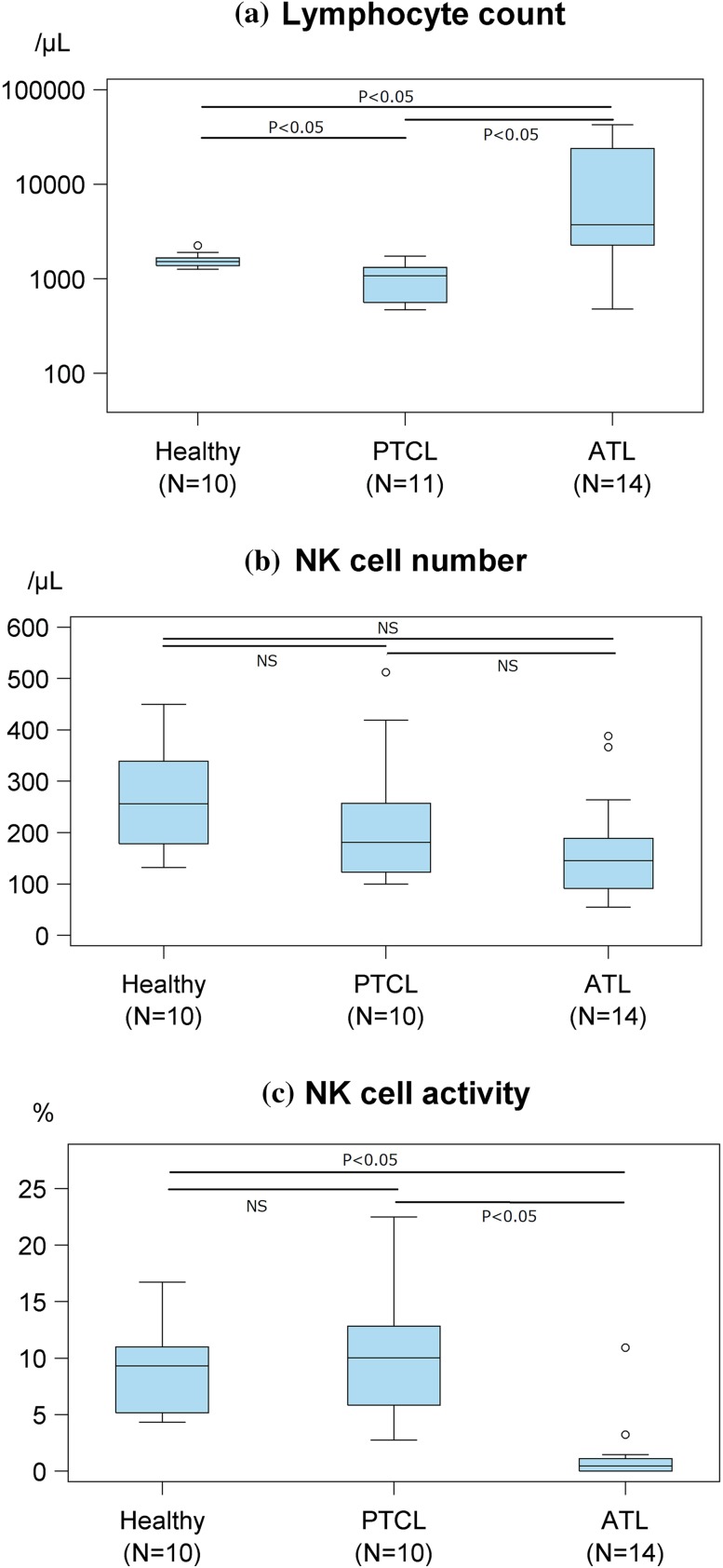
Data were shown as box plots. For multiple comparison, Dwass, Steel, Critchlow–Fligner multiple comparison analysis was used as shown in Fig. 1. All statistical analyses were conducted by SAS ver 9.4 (SAS Institute Inc., Cary, NC, USA).
Fig. 1.
Lymphocyte count, natural killer (NK) cell number, and NK cell activity before treatment initiation as determined using flow cytometry (cell number) and a 51Cr release assay (activity). a The mean lymphocyte count in healthy volunteers, peripheral T-cell lymphoma (PTCL) patients, and adult T-cell leukemia–lymphoma (ATL) patients were 1580, 991, and 11,618/μL, respectively. b The NK cell number in healthy volunteers, PTCL patients, and ATL patients, the corresponding mean values were 262, 224, and 166/μL, respectively. c The NK cell activity values in healthy volunteers, PTCL patients, and ATL patients, the corresponding mean values were 8.8, 10.4, and 1.4 %, respectively
Study oversight
The study was sponsored by Kyowa Hakko Kirin Co., Ltd. The academic investigators and the sponsor were jointly responsible for the study design. The protocol was approved by the institutional review boards at each participating site, and the study was conducted complying with the ethical guidelines on clinical research and in accordance with the Declaration of Helsinki 1995. The blood sample assays using flow cytometry and 51Cr release were outsourced to SRL Medisearch Inc. Data analysis was outsourced to Biostatistics center, Kurume university.
Results
Patient characteristics
The total number of patients enrolled was 26, and 25 patients (14 patients with ATL and 11 patients with PTCL) were included in the data analysis. One patient was excluded from analysis due to a low initial lymphocyte count of 80/μL. Data from this patient were rejected because it was judged to be inappropriate to use this value as the basis for examination of variations, and calculation of the NK cell number and activity. Table 1 shows the demographics and clinical characteristics of the 25 analyzed patients, and Table 2 shows the breakdown of patients on chemotherapy in relation to the disease subtype. The mLSG15/-L regimen was administered to 9 (64 %) patients with ATL. It should be noted that although the number of patients analyzed was limited, no marked difference was found in disease subtype according to the type of chemotherapy (mLSG15/-L vs. CHOP/-L). The CHOP/-L regimen was administered to all (100 %) patients with PTCL.
Table 1.
Patient demographics and clinical characteristics
| Characteristic | ATL patients (n = 14) | PTCL patients (n = 11) | |||
|---|---|---|---|---|---|
| n (%) | n (%) | ||||
| Age (years) | Median | 56 | 69 | ||
| Range | 47–72 | 36–78 | |||
| Sex | Male | 9 (64) | 9 (82) | ||
| Female | 5 (36) | 2 (18) | |||
| ECOG PS | 0 | 2 (14) | 5 (45) | ||
| 1 | 9 (64) | 4 (36) | |||
| 2 | 2 (14) | 2 (18) | |||
| 3 | 0 (0) | 0 (0) | |||
| 4 | 1 (7) | 0 (0) | |||
| Therapy | CHOP/-L | 5 (36) | 11 (100) | ||
| mLSG15/-L | 9 (64) | 0 (0) | |||
| Subtype | Acute | 10 (71) | AITL | 5 (45) | |
| Lymphoma | 1 (7) | PTCL-NOS | 3 (27) | ||
| Chronic | 3 (21) | ALCL ALK- | 1 (9) | ||
| EATL | 1 (9) | ||||
| SPTCL | 1 (9) | ||||
AITL angioimmunoblastic T-cell lymphoma, ALCL anaplastic large cell lymphoma, ALK anaplastic lymphoma kinase, ATL adult T-cell leukemia–lymphoma, CHOP cyclophosphamide, doxorubicin, vincristine, and prednisone, CHOP/-L CHOP or CHOP-like regimen, EATL enteropathy-associated T-cell lymphoma, ECOG Eastern Cooperative Oncology Group, mLSG15 vincristine, cyclophosphamide, doxorubicin, prednisone and doxorubicin, ranimustine, prednisone and vindesine, etoposide, carboplatin, prednisone, mLSG15/-L mLSG15 or mLSG15-like regimen, NOS not otherwise specified, PS performance status, PTCL peripheral T-cell lymphoma, SPTCL subcutaneous panniculitis-like T-cell lymphoma
Table 2.
Breakdown of patients on chemotherapy in relation to the disease subtype
| ATL subtype (n = 14) | n (%) | Therapy | |
|---|---|---|---|
| mLSG15/-L n (%) |
CHOP/-La
n (%) |
||
| Acute | 10 (71) | 6 (43) | 4 (29) |
| Lymphoma | 1 (7) | 1 (7) | 0 (0) |
| Chronic | 3 (21) | 2 (14) | 1 (7) |
| PTCL subtype (n = 11) | n (%) | Therapy | |
|---|---|---|---|
| CHOP n (%) |
CHOP-La
n (%) |
||
| AITL | 5 (45) | 1 (9) | 4 (36) |
| PTCL-NOS | 3 (27) | 1 (9) | 2 (18) |
| ALCL ALK- | 1 (9) | 1 (9) | 0 (0) |
| EATL | 1 (9) | 0 (0) | 1 (9) |
| SPTCL | 1 (9) | 0 (0) | 1 (9) |
AITL angioimmunoblastic T-cell lymphoma, ALCL anaplastic large cell lymphoma, ALK anaplastic lymphoma kinase, ATL adult T-cell leukemia–lymphoma, CHOP cyclophosphamide, doxorubicin, vincristine, and prednisone; CHOP-L CHOP-like regimen, CHOP/-L CHOP or CHOP-like regimen, EATL enteropathy-associated T-cell lymphoma, mLSG15 vincristine, cyclophosphamide, doxorubicin, prednisone and doxorubicin, ranimustine, prednisone and vindesine, etoposide, carboplatin, prednisone, mLSG15/-L mLSG15 or mLSG15-like regimen, NOS not otherwise specified, PTCL peripheral T-cell lymphoma, SPTCL subcutaneous panniculitis-like T-cell lymphoma
aTHP-COP, vincristine, pirarubicin, cyclophosphamide, and prednisone
Table 3 in “Appendix” shows the breakdown of ATL patients received with mLSG15/-L regimen and CHOP/-L regimen, and Table 4 in “Appendix” shows the breakdown of PTCL patients received with CHOP/-L regimen. Disease progressions were almost reasons for taken off these therapies. None of ATL patients received both mLSG15/-L and CHOP/-L regimens.
Table 3.
Breakdown of ATL patients received with (a) VCAP (Day 1 of each cycle) and VECP (Day 15–17 of each cycle: ※) of mLSG15/-L regimen, (b) CHOP/-L regimen
| Cycle number | ||||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 1※ | 2 | 2※ | 3 | 3※ | 4 | 4※ | |
| (a) | ||||||||
| Number of received patients | 9 | 8 | 8 | 8 | 7 | 6 | 5 | 2 |
| Number of analyzed patients | 9 | 8 | 8 | 8 | 7 | 6 | 5 | 2 |
| Number of missing data | – | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Number of taken off therapy | – | 0 | 1 | 1 | 2 | 3 | 4 | 7 |
| Cycle number | ||||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| (b) | ||||||||
| Number of received patients | 5 | 5 | 3 | 2 | 2 | 0 | 1 | 1 |
| Number of analyzed patients | 5 | 5 | 3 | 2 | 2 | 0 | 1 | 1 |
| Number of missing data | – | 0 | 0 | 0 | 0 | 2 | 0 | 0 |
| Number of taken off therapy | – | 0 | 2 | 3 | 3 | 3 | 4 | 4 |
Table 4.
Breakdown of PTCL patients received with CHOP/-L regimen
| Cycle number | ||||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| Number of received patients | 11 | 11 | 8 | 9 | 7 | 7 | 6 | 6 |
| Number of analyzed patients | 10 | 10 | 7 | 9 | 7 | 7 | 6 | 6 |
| Number of missing data | – | 0 | 2 | 0 | 1 | 1 | 1 | 0 |
| Number of taken off therapy | – | 0 | 1 | 1 | 2 | 2 | 3 | 4 |
Lymphocyte counts and NK cell number and activity before treatment initiation
Figure 1 shows the lymphocyte count, NK cell number, and NK cell activity determined in 14 patients with ATL, 11 patients with PTCL, and 10 healthy adult volunteers. The lymphocyte count before initiation of treatment was significantly higher by 1 log in ATL compared to in PTCL patients (Fig. 1a), which was probably attributable to the fact that patients with acute-type ATL who had ATL cells in the peripheral blood [22] accounted for 71 % of the patients with ATL (Table 2). There was no significant difference in the number of CD16/CD56 double-positive NK cells which can contribute to ADCC of mogamulizumab, before treatment initiation between ATL and PTCL patients, or between these patients and healthy adult volunteers (Fig. 1b). Although the NK cell activity before treatment initiation was markedly lower in ATL than in PTCL patients (Fig. 1c), there was no significant difference in the NK cell activity between patients with PTCL and healthy adult volunteers (Fig. 1c).
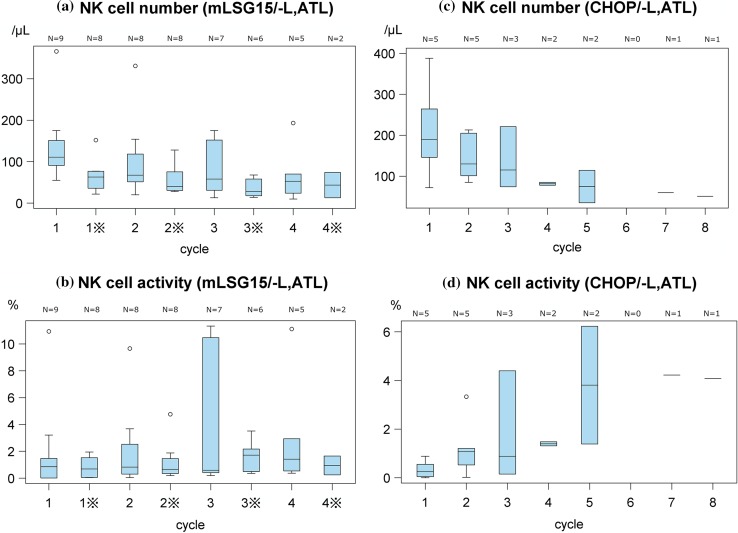
Variations in the NK cell number and activity in ATL patients after treatment initiation
The NK cell number in patients with ATL was decreased as a result of the mLSG15/-L regimen, and this decrease was more prominent before VECP therapy (Day 15–17 of each cycle) than before VCAP therapy (Day 1 of each cycle) (Fig. 2a). The NK cell number in patients with ATL also decreased by the CHOP/-L regimen (Fig. 2c). However, the NK cell activity by the CHOP/-L regimen showed a tendency to increase (Fig. 2d), although there was not marked difference by mLSG15/-L regimen (Fig. 2b).
Fig. 2.
Variations in natural killer (NK) cell number and NK cell activity in adult T-cell leukemia–lymphoma (ATL) patients. a NK cell number determined before (Pre) administration at VCAP (Day 1 of each cycle) and VECP (Day 15–17 of each cycle: ※) of mLSG15/-L treatment initiation. b NK cell activity determined before (Pre) administration at VCAP (Day 1 of each cycle) and VECP (Day 15–17 of each cycle: ※) of mLSG15/-L treatment initiation. c NK cell number determined before (Pre) administration at each cycle of CHOP/-L treatment initiation. d NK cell activity determined before (Pre) administration at each cycle of CHOP/-L treatment initiation
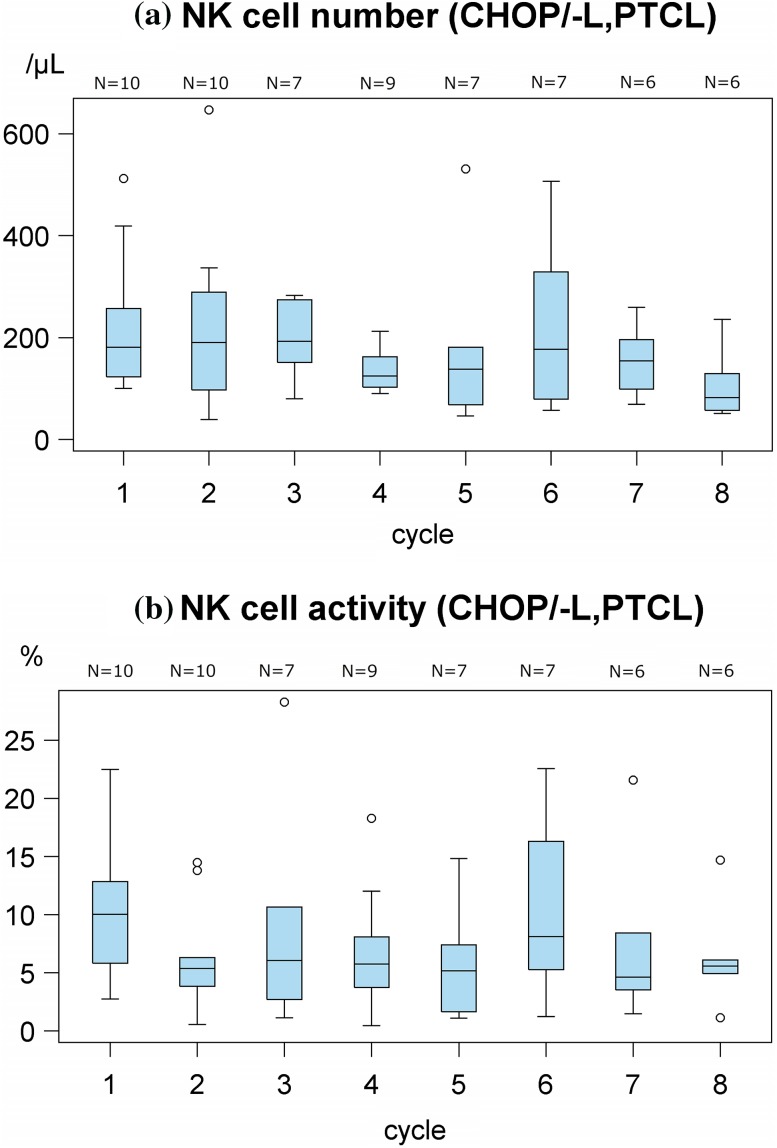
Variations in NK cell number and activity in PTCL patients after treatment initiation
In PTCL patients, the NK cell number did not decrease by the CHOP/-L regimen (Fig. 3a), though the NK cell number in patients with ATL decreased by this regimen (Fig. 2c). The NK cell activity in PTCL patients slightly decreased by the CHOP/-L regimen (Fig. 3b).
Fig. 3.
Variations in natural killer (NK) cell number and NK cell activity in peripheral T-cell lymphoma (PTCL) patients. a NK cell number determined before (Pre) administration at each cycle of CHOP/-L treatment initiation. b NK cell activity determined before (Pre) administration at each cycle of CHOP/-L treatment initiation
Discussion
In this study, the effects of first-line therapy for newly diagnosed ATL and PTCL patients on NK cells defined as CD16/CD56 double-positive ones can cause high ADCC for defucosylated antibodies such as mogamulizumab were evaluated using NK cell number and NK cell activity substitute functional cell vitality as indices. These data showed that the effects of chemotherapy on NK cells varied according to the disease (ATL or PTCL) and the regimen used and/or the number of courses of chemotherapy (mLSG15/-L regimen or CHOP/-L regimen). Furthermore, it was also found that the NK cell activity before treatment initiation was markedly lower in ATL than in PTCL patients. This low activity of NK cell in ATL may be caused by suppression of NK cells by a subset of ATL cells functioning as Treg cells [23–25]. These results suggest that it is more difficult for some therapeutic mAbs that require an effector function to exert their therapeutic effects in ATL compared to in PTCL, although the mechanism of NK cell activity may be different from that of ADCC. However, it cannot be directly concluded that therapeutic Abs are less likely to exert benefits in patients with ATL. In fact, the NK cell number in cases treated with the mLSG15/-L regimen tended to be restored before the initiation of each chemotherapeutic cycle (VCAP therapy) in comparison with before toward the end of each cycle (VECP therapy). This finding suggests that in cases where mAbs are combined with the mLSG15/-L regimen, some therapeutic mAbs may be more likely to exert their beneficial effects when they are used before the initiation of each cycle. Additionally, the NK cell activity tended to increase after the CHOP/-L regimen than after the mLSG15/-L regimen in patients with previously untreated ATL. Therapeutic effect of the administered chemotherapy against more suppressive ATL cells compared to PTCL may result in increased vitality per cell of survived NK cells in ATL patients. However, the details of why CHOP/-L treatment tended to produce better results compared to those of more potent intensive regimen, mLSG15/-L, are necessary to carefully consider, while paying heed to direct effects on NK cells by each chemotherapy itself. Therefore, it is not possible to determine which of the two regimens, both of which consist of drugs with different solitary effects, should be recommended as the most suitable chemotherapy to be combined with therapeutic Abs. However, the CHOP/-L regimen, which was associated with a less prominent decrease in totally NK cell activity, seems to be more promising, assuming that patients respond similarly to chemotherapy alone. Further investigations in a greater number of patients are needed, because this was a small-scale study.
Recently, it was carried out a phase II controlled clinical study (clinical trial information: NCT01173887) to examine the effects of combination treatment using the mLSG15 regimen and mogamulizumab in patients with untreated ATL [26]. In that phase II study, mogamulizumab was administered at intervals of 2 weeks (at the same time as VCAP and VECP administration) over four courses of the mLSG15 regimen (8 times in total), i.e., at the same times as the blood sampling was performed in the present study. The results showed that the complete response rate and overall response rate in the 29 patients administered mLSG15 + mogamulizumab versus the 24 patients administered the mLSG15 alone were 52 versus 33 % and 86 versus 75 %, respectively, with mLSG15 combined with mogamulizumab showing better efficacy in both indices. These data indicated that combining mogamulizumab with mLSG15 showed an additive effect with mLSG15, which tended to cause a greater decrease in NK cell number than the CHOP/-L regimen. Therefore, we speculate that mogamulizumab combination with the CHOP/-L regimen could also be beneficial for patients in whom the mLSG15 regimen is difficult to implement because of advanced age or for other reasons. Further investigations are needed to examine this presumption.
On the other hand, in patients with PTCL, the decrease in NK cell number and activity after the standard chemotherapy, i.e., the CHOP/-L regimen, was relatively small, as compared to the CHOP/-L treated patients with ATL, who would be immune suppressive condition as seen in Fig. 1c which shows significant lower activity of NK cells in ATL patients compared to PTCL. This result suggests that the effect of combining therapeutic Abs with chemotherapy is considerably more promising in PTCL patients. Indeed, a phase II clinical study of alemtuzumab in combination with CHOP demonstrated favorable effects, with complete response and overall response rates in 24 patients of 71 and 75 %, respectively [27]. The efficacy of mogamulizumab in combination with CHOP in patients with untreated primary PTCL is also expected.
In conclusion, the results of the present study provide an important basis for future investigations of the combined effects of chemotherapy and therapeutic Abs [18–20] whose activity is affected by CD16/CD56 double-positive NK cells. Further analysis of CD16-positive other effector cells which antibodies bind also remains to be explored to fully understand the combination effects.
Acknowledgments
We thank all the patients and their families, as well as the investigators who participated in this multicenter collaborative study.
Abbreviations
- ADCC
Antibody-dependent cellular cytotoxicity
- AITL
Angioimmunoblastic T-cell lymphoma
- ALCL
Anaplastic large cell lymphoma
- ALK
Anaplastic lymphoma kinase
- ATL
Adult T-cell leukemia–lymphoma
- CCR4
Chemokine receptor 4
- CD
Cluster of differentiation
- CHOP
Cyclophosphamide, doxorubicin, vincristine, and prednisone
- JCOG
Japan Clinical Oncology Group
- mLSG15
VCAP–AMP–VECP; vincristine, cyclophosphamide, doxorubicin, and prednisone; doxorubicin, ranimustine, and prednisone; and vindesine, etoposide, carboplatin, and prednisone
- NK
Natural killer
- OS
Overall survival
- PTCL
Peripheral T-cell lymphoma
- PTCL-NOS
Peripheral T-cell lymphoma, not otherwise specified
- SSC-H
Side scatter-height
Appendix
Compliance with ethical standards
Conflict of interest
Takeshi Takahashi is employee of Kyowa Hakko Kirin Co., Ltd.; Michinori Ogura serves as a consultant/advisory role to Mundipharma K.K., Meiji Seika Pharma Co., Ltd. and Celgene K.K.; Takashi Ishida and Atae Utsunomiya received honoraria from Kyowa Hakko Kirin Co., Ltd.; Takashi Ishida received research funding from Kyowa Hakko Kirin Co., Ltd., Bayer Pharma AG, and Celgene K.K.; Kunihiro Tsukasaki received research funding from Kyowa Hakko Kirin Co., Ltd.
References
- 1.The International Agency for Research on Cancer . WHO classification of tumors of hematopoietic and lymphoid tissues. 4. Lyon: International Agency for Research on Cancer (IARC); 2008. [Google Scholar]
- 2.Uchiyama T, Yodoi J, Sagawa K, et al. Adult T-cell leukemia: clinical and hematologic features of 16 cases. Blood. 1977;50:481–492. [PubMed] [Google Scholar]
- 3.Poiesz BJ, Ruscetti FW, Gazdar AF, et al. Detection and isolation of type C retrovirus particles from fresh and cultured lymphocytes of a patient with cutaneous T-cell lymphoma. Proc Natl Acad Sci USA. 1980;77:7415–7419. doi: 10.1073/pnas.77.12.7415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hinuma Y, Nagata K, Hanaoka M, et al. Adult T-cell leukemia: antigen in an ATL cell line and detection of antibodies to the antigen in human sera. Proc Natl Acad Sci USA. 1981;78:6476–6480. doi: 10.1073/pnas.78.10.6476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chihara D, Ito H, Matsuda T, et al. Differences in incidence and trends of haematological malignancies in Japan and the United States. Br J Haematol. 2014;164:536–545. doi: 10.1111/bjh.12659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vose J, Armitage J, Weisenburger D. International T-cell Lymphoma project. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J Clin Oncol. 2008;26:4124–4130. doi: 10.1200/JCO.2008.16.4558. [DOI] [PubMed] [Google Scholar]
- 7.Yamada Y, Tomonaga M, Fukuda H, et al. A new G-CSF-supported combination chemotherapy, LSG15, for adult T-cell leukaemia-lymphoma: Japan clinical oncology group study 9303. Br J Haematol. 2001;113:375–382. doi: 10.1046/j.1365-2141.2001.02737.x. [DOI] [PubMed] [Google Scholar]
- 8.Tsukasaki K, Tobinai K, Hotta T, et al. Lymphoma study group of JCOG. Jpn J Clin Oncol. 2012;42:85–95. doi: 10.1093/jjco/hyr168. [DOI] [PubMed] [Google Scholar]
- 9.Tsukasaki K, Utsunomiya A, Fukuda H, et al. VCAP–AMP–VECP compared with biweekly CHOP for adult T-cell leukemia–lymphoma: Japan Clinical Oncology Group Study JCOG9801. J Clin Oncol. 2007;25:5458–5464. doi: 10.1200/JCO.2007.11.9958. [DOI] [PubMed] [Google Scholar]
- 10.National Comprehensive Cancer Network (2014) NCCN Clinical practice guidelines in oncology (NCCN Guidelines®). Non-Hodgkin’s lymphomas, version 2
- 11.Enblad G, Hagberg H, Erlanson M, et al. A pilot study of alemtuzumab (anti-CD52 monoclonal antibody) therapy for patients with relapsed or chemotherapy-refractory peripheral T-cell lymphomas. Blood. 2004;103:2920–2924. doi: 10.1182/blood-2003-10-3389. [DOI] [PubMed] [Google Scholar]
- 12.Zinzani PL, Alinari L, Tani M, et al. Preliminary observation of a phase II study of reduced-dose alemtuzumab in patients with pretreated T-cell lymphoma. Haematologica. 2005;90:702–703. [PubMed] [Google Scholar]
- 13.Yamamoto K, Utsunomiya A, Tobinai K, et al. Phase I study of KW-0761, a defucosylated humanized anti-CCR4 antibody, in relapsed patients with adult T-cell leukemia–lymphoma and peripheral T-cell lymphoma. J Clin Oncol. 2010;28:1591–1598. doi: 10.1200/JCO.2009.25.3575. [DOI] [PubMed] [Google Scholar]
- 14.Ishida T, Joh T, Uike N, et al. Defucosylated anti-CCR4 monoclonal antibody (KW-0761) for relapsed adult T-cell leukemia–lymphoma: a multicenter phase II study. J Clin Oncol. 2012;30:837–842. doi: 10.1200/JCO.2011.37.3472. [DOI] [PubMed] [Google Scholar]
- 15.Ogura M, Ishida T, Hatake K, et al. Multicenter phase II study of mogamulizumab (KW-0761) a defucosylated anti-CC chemokine receptor 4 antibody, in patients with relapsed peripheral T-cell lymphoma and cutaneous T-cell lymphoma. J Clin Oncol. 2014;32:1157–1163. doi: 10.1200/JCO.2013.52.0924. [DOI] [PubMed] [Google Scholar]
- 16.Pro B, Advani R, Brice P, et al. Brentuximab vedotin (SGN-35) in patients with relapsed or refractory systemic anaplastic large-cell lymphoma: results of a phase II study. J Clin Oncol. 2012;30:2190–2196. doi: 10.1200/JCO.2011.38.0402. [DOI] [PubMed] [Google Scholar]
- 17.Coiffier B, Lepage E, Briere J, et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med. 2002;346:235–242. doi: 10.1056/NEJMoa011795. [DOI] [PubMed] [Google Scholar]
- 18.Niwa R, Shoji-Hosaka E, Sakurada M, et al. Defucosylated chimeric anti-CC chemokine receptor 4 IgG1 with enhanced antibody-dependent cellular cytotoxicity shows potent therapeutic activity to T-cell leukemia and lymphoma. Cancer Res. 2004;64:2127–2133. doi: 10.1158/0008-5472.CAN-03-2068. [DOI] [PubMed] [Google Scholar]
- 19.Ishii T, Ishida T, Utsunomiya A, et al. Defucosylated humanized anti-CCR4 monoclonal antibody KW-0761 as a novel immunotherapeutic agent for adult T-cell leukemia/lymphoma. Clin Cancer Res. 2010;16:1520–1531. doi: 10.1158/1078-0432.CCR-09-2697. [DOI] [PubMed] [Google Scholar]
- 20.Yamane-Ohnuki N, Kinoshita S, Inoue-Urakubo M, et al. Establishment of FUT8 knockout Chinese hamster ovary cells: an ideal host cell line for producing completely defucosylated antibodies with enhanced antibody-dependent cellular cytotoxicity. Biotechnol Bioeng. 2004;87:614–622. doi: 10.1002/bit.20151. [DOI] [PubMed] [Google Scholar]
- 21.Seto M, Takahashi T, Nakamura S, et al. In vivo antitumor effects of monoclonal antibodies with different immunoglobulin classes. Cancer Res. 1983;43:4768–4773. [PubMed] [Google Scholar]
- 22.Shimoyama M. Diagnostic criteria and classification of clinical subtypes of adult T-cell leukaemia lymphoma: a report from the Lymphoma Study Group (1984–87) Br J Haematol. 1991;79:428–437. doi: 10.1111/j.1365-2141.1991.tb08051.x. [DOI] [PubMed] [Google Scholar]
- 23.Yano H, Ishida T, Inagaki A, et al. Regulatory T-cell function of adult T-cell leukemia/lymphoma cells. Int J Cancer. 2007;120:2052–2057. doi: 10.1002/ijc.22536. [DOI] [PubMed] [Google Scholar]
- 24.Trzonkowski P, Szmit E, Myśliwska J, et al. CD4+CD25+ T regulatory cells inhibit cytotoxic activity of T CD8+ and NK lymphocytes in the direct cell-to-cell interaction. Clin Immunol. 2004;112:258–267. doi: 10.1016/j.clim.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 25.Smyth MJ, Teng MW, Swann J, et al. CD4+CD25+ T regulatory cells suppress NK cell-mediated immunotherapy of cancer. J Immunol. 2006;176:1582–1587. doi: 10.4049/jimmunol.176.3.1582. [DOI] [PubMed] [Google Scholar]
- 26.Ishida T, Jo T, Takemoto S, et al. Dose-intensified chemotherapy alone or in combination with mogamulizumab in newly diagnosed aggressive adult T-cell leukaemia-lymphoma: a randomized phase II study. Br J Haematol. 2015;169:672–682. doi: 10.1111/bjh.13338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gallamini A, Zaja F, Patti C, et al. Alemtuzumab (Campath-1H) and CHOP chemotherapy as first-line treatment of peripheral T-cell lymphoma: results of a GITIL (Gruppo Italiano Terapie Innovative nei Linfomi) prospective multicenter trial. Blood. 2007;110:2316–2323. doi: 10.1182/blood-2007-02-074641. [DOI] [PubMed] [Google Scholar]