Abstract
Ovarian hyperstimulation syndrome is a disorder associated with ovulation induction and is rarely seen in pregnant women. Very few cases of spontaneous ovarian hyperstimulation syndrome have been reported in a woman who is neither pregnant nor undergoing ovulation therapy. This case report describes how spontaneous ovarian hyperstimulation syndrome is associated with primary hypothyroidism in a 25-year-old, nonpregnant woman who is not on ovulation induction therapy. Imaging and laboratory findings confirmed the diagnosis of this rare entity, which aided the clinicians in providing prompt management and in preventing further complications.
Introduction
Ovarian hyperstimulation syndrome (OHSS) is a complication usually seen in women undergoing ovulation induction therapy for in vitro fertilization, with an incidence of 0.2–1%. It can rarely occur spontaneously in patients not undergoing ovulation induction therapies (1). The symptoms include bilateral symmetric enlargement of ovaries with multiple cysts of varying sizes, associated with ascites, pleural effusion, or pericardial effusion. This case report describes how spontaneous ovarian hyperstimulation syndrome is associated with primary hypothyroidism in a 25-year-old, nonpregnant woman who was not on ovulation induction therapy. Only a handful of such cases have been reported in the published literature (2). We report this case to emphasize how radiological findings played a major role in prompt diagnosis, which led in turn to appropriate treatment and prevented further complications.
Case report
A 25-year-old woman presented to our hospital with abdominal pain and abdominal distension, with associated breathlessness, for the past 2 weeks. On examination, she exhibited short stature with abdominal tenderness. She was admitted for further management. Initial blood and biochemical investigations revealed low hemoglobin of 6.8 gm/dl (normal value, 12–15 gm/dl), a raised thyroid stimulating hormone (TSH) level of more than 150.0 micro IU/ml, (normal value, 0.35 – 4.0 micro IU/ml), and low free thyroxine (T4) levels, measuring 0.21 (normal value, 0.8 – 1.8 ng/dl), suggesting primary hypothyroidism.
Ultrasound (US) examination of the abdomen showed bilateral, grossly enlarged ovaries with multiple enlarged cysts and thin septations. The right ovary measured 7 × 8.7 × 10.7 cms (AP × TRANS × CC), with a volume of 325.8 cc; the left ovary measured 7.3 × 10.3 × 10.2 cms (AP × TRANS × CC), with a volume of 383.4 cc (Figs. 1A and 1B). Contrast-enhanced CT (CECT) of the abdomen confirmed bilaterally enlarged ovaries and ascites (Fig. 2). In addition, bilateral, stippled femoral epiphyses were seen, probably secondary to chronic hypothyroid status (Fig. 3). CT of the thorax showed moderate pericardial effusion (Fig. 4).
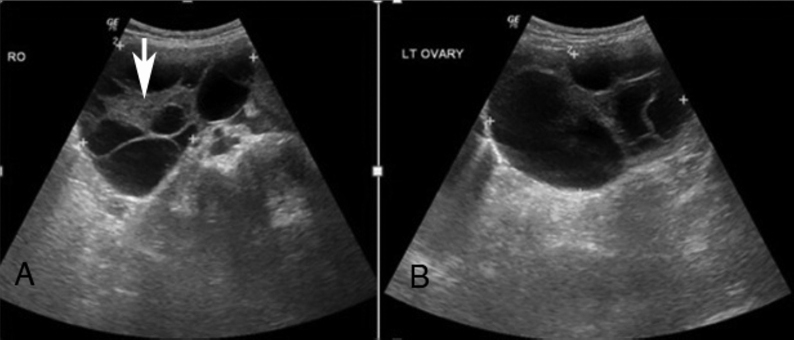
Fig. 1.
25-year-old woman with abdominal pain and distension diagnosed with spontaneous OHSS. US of the abdomen shows bilateral, grossly enlarged ovaries with multiple, enlarged cysts and thin septations. A hemorrhagic cyst is seen in the right ovary (down arrow). [Right ovary measured 7 × 8.7 × 10.7 cms (AP × TRANS × CC), volume: 325.8 cc. Left ovary measured 7.3 × 10.3 × 10.2 cms (AP × TRANS × CC), volume: 383.4 cc].
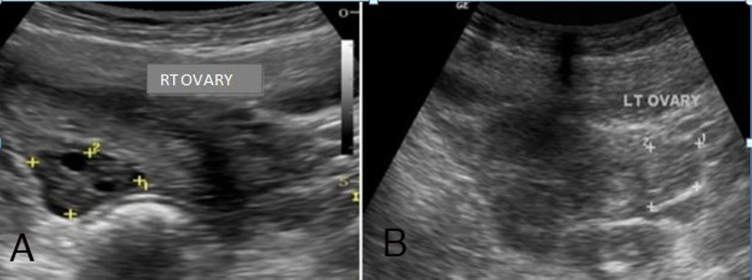
Fig. 2.
25-year-old woman with abdominal pain and distension diagnosed with spontaneous OHSS. Contrast-enhanced axial CT image of the abdomen shows bilateral, grossly enlarged ovaries with multiple, enlarged cysts and thin septations (asterix). Minimal ascites was also seen.
Fig. 3.

25-year-old woman with abdominal pain and distension diagnosed with spontaneous OHSS. Noncontrast coronal reformatted image of the pelvis shows stippled femoral epiphyses involving bilateral femoral head (black arrows), probably secondary to chronic hypothyroid status.
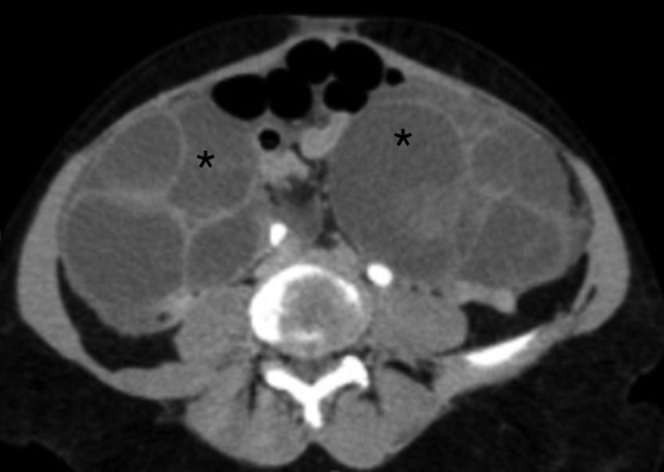
Fig. 4.
25-year-old woman with abdominal pain and distension diagnosed with spontaneousOHSS. Contrast-enhanced coronal reformatted image of the thorax shows moderate pericardial effusion (asterix).
Based on the radiological findings, the patient was evaluated for ovarian malignancies. Alpha feto protein and CA-125 tests were done and found to be negative. Due to the abnormal thyroid function tests, additional hormonal investigations were carried out that showed raised estradiol, measuring 848.93 (normal value, < 56 pg/ml ). FSH was mildly raised, measuring 12.84 (normal value, 2.5–10.2 mIU/ml). LH was mildly reduced, measuring less than 0.07 (normal value, 1.9 – 12.5 mIU/ml). The beta HCG value was also normal, measuring less than 2.0 (normal value, < 5.0).
Based on the clinical, laboratory, and radiological findings, a diagnosis of spontaneous ovarian hyperstimulation syndrome (spontaneous OHSS) was made. The patient was started on T. Thyroxine, at 100 mcg/day. The patient was not willing to undergo further investigations and was hence discharged. She was asked to come for regular followup.
The thyroid function tests were repeated after 2 weeks and showed mild reduction in the free thyroxine (FT4) but a sustained increase in the TS (FT4 – 0.60 [0.8 – 1.8 ng/dl], TSH3 >150.000 [0.35 – 4 micro IU/ml]).
Compared with the previous US scan of her pelvis, the first followup scan showed significant reduction in the volume of both ovaries. (Right ovary: 5.0 × 3.3 × 3.6 cm, volume 37cc; left ovary: 5.1 × 3.0 × 4.8cm, volume 38cc). There was complete resolution of ascites.
The patient was advised to continue with the same dose of thyroxine and was asked to come for review after a month. US, repeated after 1.5 months, showed near-complete resolution of the bilaterally enlarged ovaries: a normal right ovary and a mildly enlarged left ovary (Figs. 5A and B). Her abdominal distension and tenderness resolved, and her symptoms improved significantly. The patient was discharged and was advised to continue her medications and come for regular followup.
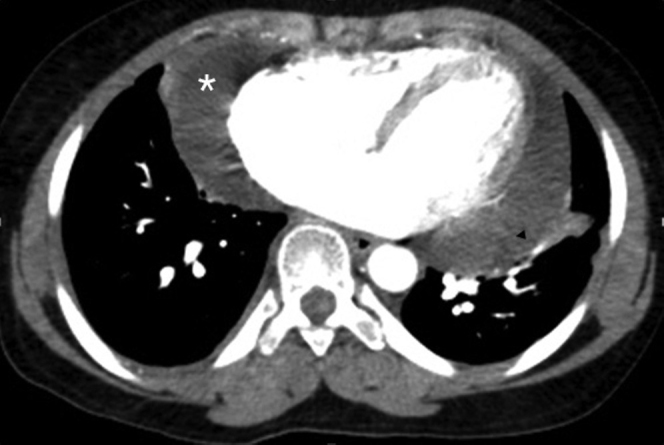
Fig. 5.
25-year-old woman with abdominal pain and distension diagnosed with spontaneous OHSS. US of the abdomen shows complete resolution of bilateral enlarged ovaries.
Discussion
All women undergoing ovarian stimulation are at the risk of developing OHSS. It can rarely also occur spontaneously in pregnancy. In this case, spontaneous OHSS was associated with primary hypothyroidism in a 25-year-old, nonpregnant female who was not on any ovulation induction therapy. There is very little published literature on spontaneous OHSS occurring in such patients.
The possible risk factors for the development of OHSS include young age, polycystic ovarian syndrome, asthenic habitus, luteal supplementation of hCG, protocols with GnRH, a high level of serum estradiol, and multiple follicles (3).
Spontaneous forms of OHSS have been reported between 8 and 14 weeks of pregnancy and also with follicle-stimulating hormone (FSH) producing pituitary adenoma. The syndrome has been previously reported in rare instances of increased production of human chorionic gonadotropin (hCG), which is commonly seen in multiple pregnancies, polycystic ovary disease, hydatidiforme mole, and elevated levels of thyroid-stimulating hormone (TSH) in hypothyroidism (4).
The etiology and pathogenesis of spontaneous OHSS are poorly understood. It is usually associated with ovulation induction therapy. Only a handful of cases of OHSS associated with pregnancy have been reported.
HCG belongs to a family of glycoproteins that includes FSH, luteinizing hormone (LH), and thyroid-stimulating hormone (TSH). These four hormones have two subunits—a common alpha subunit, and a beta subunit that is specific to each molecule. More than 40% of amino acid homology is shared by these subunits. The receptors for these glycoprotein hormones have a similar structure. Under normal circumstances, hCG and LH bind to the LH receptor, while FSH and TSH bind to separate FSH and TSH receptors, respectively. Once the hormone binds to the receptor, the downstream signaling events are activated (1, 3).
Spontaneous OHSS has been classified into three types in a study done by De Leener et al, based on the clinical presentation and FSH receptor mutation.
* Type I corresponds to the mutated FSHr cases.
* Type II corresponds to the spontaneous OHSS secondary to high levels of hCG. This type is probably the most frequently encountered.
* Type III is related to hypothyroidism (5).
This classification could be useful for clinicians and scientists. The clinicians will rapidly extend our knowledge on the precise origins of spontaneous OHSS, which could result in delineation of new types of spontaneous OHSS and certainly help with future counseling and treatment of patients. Our case was admitted as type III.
The exact mechanism by which ovarian hyperstimulation syndrome might occur in hypothyroid patients is not clearly understood. A possible explanation was suggested by Rotmensch and Scommegna, on the basis of preferential formation of estriol via the 16-hydroxylation pathway instead of the normal 2-hydroxylation that has been demonstrated in hypothyroid patients (5). Excessive gonadotropin release, due to decreased feedback regulation caused by substitution of estradiol by the less potent estriol, would result in excessive ovarian stimulation (6).
Cardoso et al described a case of consistent regression of large bilateral ovarian cysts in a hypothyroid patient after the institution of thyroid hormone replacement therapy, suggesting the causal relationship between primary hypothyroidism and spontaneous ovarian hyperstimulation syndrome (6). Nappi et al. presented a case of untreated hypothyroidism associated with spontaneous OHSS. In their patient, thyroid replacement therapy and fluid administration also led to prompt resolution of the spontaneous OHSS (7).
In our case, the patient had increased TSH with a decrease in the free thyroxine levels. This could be explained if the patient had a mutated FSH receptor. But we couldn't investigate receptor mutation in our case.
The clinical symptoms of OHSS vary depending on their severity. The symptoms can be classified as mild, moderate, and severe. Mild OHSS is characterized by uncomplicated ovarian enlargement with multiple cysts, moderate disease is characterized by ascites, and severe disease is associated with pleural or pericardial effusion, hemoconcentration, thrombosis, and oliguria (8).
Most of the symptoms are due to accumulation of fluid in the extra vascular space and the third space due to increased capillary permeability. This may cause hypo-albuminemia, hemoconcentration, electrolyte imbalance, decreased renal perfusion, oliguria, ascites, and pleural or pericardial effusions, which may in turn cause significant morbidity and mortality from thrombosis, renal, liver, and respiratory failure (ARDS) (9).
Imaging findings can be similar in US, CT, and MRI. The classical findings of this rare entity include bilateral enlarged ovaries with multiple cysts, ascites, and pleural effusion. Ovarian torsion or rupture may complicate OHSS (10). The differential diagnosis includes polycystic ovarian disease, but this can be differentiated with clinical and other laboratory findings.
Mild to moderate forms of OHSS are treated with analgesic and antiemetic therapy. Severe forms of OHSS are treated with rapid replacement of depleted body fluids with ringer lactate or normal saline. The underlying cause must be identified and treated accordingly. In our case, spontaneous OHSS was mainly caused by primary hypothyroidism, and the patient was treated with thyroxine.
Conclusion
This report suggests that spontaneous ovarian hyperstimulation syndrome can happen even in nonpregnant women who are not on ovulation induction therapy. It is necessary to evaluate all spontaneous OHSS patients for hypothyroidism, as this by itself can be a cause for this rare entity. Appropriate diagnosis at the right time can aid clinicians in providing prompt management and also help in preventing further complications.
Footnotes
Published: March 29, 2015
References
- 1.Akbay E, Uzunçakmak C, Sevdaİdil N, Akçiğ Z, Özel G, Yaşra L. Recurrent spontaneous ovarian hyperstimulation syndrome with hypothyroidism: A case report. Bakirkoy Dr. SadiKonuk Training and Research Hospital, Obstetrics and Gynecology Clinic, Istanbul. Bakırköy Tıp Dergisi, Cilt 6, Sayı 1, 2010 / Medical Journal of Bakırköy. 2010;6:1. [Google Scholar]
- 2.Kanza RE, Gagnon S, Villeneuve H, Laverdiere D, Rousseau I, Bordeleau E, Berube M. Spontaneous ovarian hyperstimulation syndrome and pituitary hyperplasia mimicking macro adenoma associated with primary hypothyroidism. World J Radiol. Jan 28, 2013;5(1):20–24. doi: 10.4329/wjr.v5.i1.20. Published online Jan 28, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chae HD, Park EJ, Kim SH, Kim CH, Kang BM, Chang YS. Ovarian hyperstimulation syndrome complicating a spontaneous singleton pregnancy: a case report. J Assist Reprod Genet. 2001 Feb;18(2):120–123. doi: 10.1023/A:1026543027300. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kasum M, Oreskovic S, Jezek D. Spontaneous ovarian hyperstimulation syndrome. Coll. Antropol. 2013 Jun;37(2):653–656. [PubMed] [PubMed] [Google Scholar]
- 5.Rotmensch S, Scommegna A. Spontaneous ovarian hyperstimulation syndrome associated with hypothyroidism. Am J Obstet Gynecol. 1989 May;160(5 Pt 1):1220–1222. doi: 10.1016/0002-9378(89)90196-8. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Cardoso CG, Graca LM, Dias T, Clode N, Soares L. Spontaneous ovarian hyperstimulation and primary hypothyroidism with a conceived pregnancy. Obstet Gynecol. 1999 May;93(5 Pt 2):809–811. doi: 10.1016/s0029-7844(98)00435-9. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Nappi RG, Di Naro E, D’Aries AP, Nappi L. Natural pregnancy in hypothyroid woman complicated by spontaneous ovarian hyperstimulation syndrome. Am J Obstet Gynecol. 1998 Mar;178(3):610–611. doi: 10.1016/s0002-9378(98)70448-x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Aboulghar MA, Mansour RT. Ovarian hyperstimulation syndrome: classifications and critical analysis of preventive measures. Hum Reprod Update. 2003 May-Jun;9(3):275–289. doi: 10.1093/humupd/dmg018. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Clinical practice guidelines: OHSS guidelines and management. Institute of Obstetricians and Gynaecologists, Royal College of Physicians of Ireland. April 2012.
- 10.Lalwani N, Patel S, Ha KY, Shanbhogue AK, Nagar AM, Chintapalli KN, Prasad SR. Miscellaneous tumour-like lesions of the ovary: cross-sectional imaging review. Br Journal Radiol. 2012 May;85(1013):477–486. doi: 10.1259/bjr/92819127. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]