Abstract
Parathyroid carcinoma is a rare cause of primary hyperparathyroidism. Clinical indicators of carcinoma include the severity of hyperparathyroidism and presence of a palpable neck mass. Definitive diagnosis requires surgical resection and specimen histology, or documentation of metastatic disease. We present a case of parathyroid carcinoma in a young female patient with severe hyperparathyroidism, who was also found to have subclinical hyperthyroidism in the setting of an intercurrent, solitary, functioning thyroid adenoma. A diagnostic approach to parathyroid disease, combining multimodality imaging and clinicopathologic features, is discussed.
Case report
A 39-year-old female presented with 1 week of vomiting and abdominal pain. She was dehydrated and lethargic, but hemodynamically stable. Clinical examination revealed a palpable neck mass. Serum biochemistry showed severe primary hyperparathyroidism [Corrected calcium 5.46mmol/L (range 2.17–2.46mmol/L); PTH 666pg/ml (range 10–65pg/ml)]. Serum phosphate [0.96mmol/l (range 0.79–1.37mmol/L)] and creatinine [80µmol/L (range 60–100µmol/L)] were normal, although urea was elevated [6.8mmol/L (range 2.6–6.4mmol/L)]. Thyroid function tests also indicated subclinical hyperthyroidism [TSH 0.33mU/L (range 0.4–4.0µU/L); fT4 21.2pmol/L (range 11.4–23.9)]. The patient reported no prior history of thyroid disease.
A chest radiograph (Fig. 1) showed an opacity at the base of the neck, displacing the trachea to the left. There were no plain-film musculoskeletal manifestations of hyperparathyroidism.
Fig. 1.
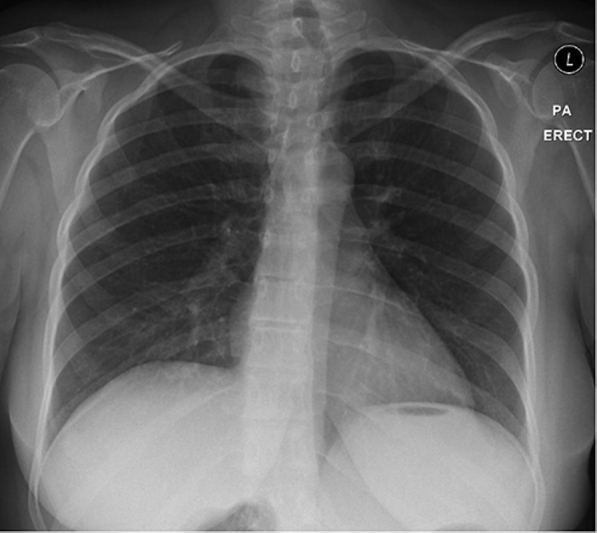
39-year-old female with parathyroid carcinoma. Chest radiograph.
Neck ultrasound (Fig. 2) revealed a 4.3-cm, complex, predominantly cystic mass below the right thyroid lobe with echogenic, hypervascular internal projections (Fig. 2, A and B). A second, circumscribed isoechoic nodule was also seen within the adjacent right thyroid lobe (Fig. 2C, arrow). There was no regional lymphadenopathy.
Fig. 2.
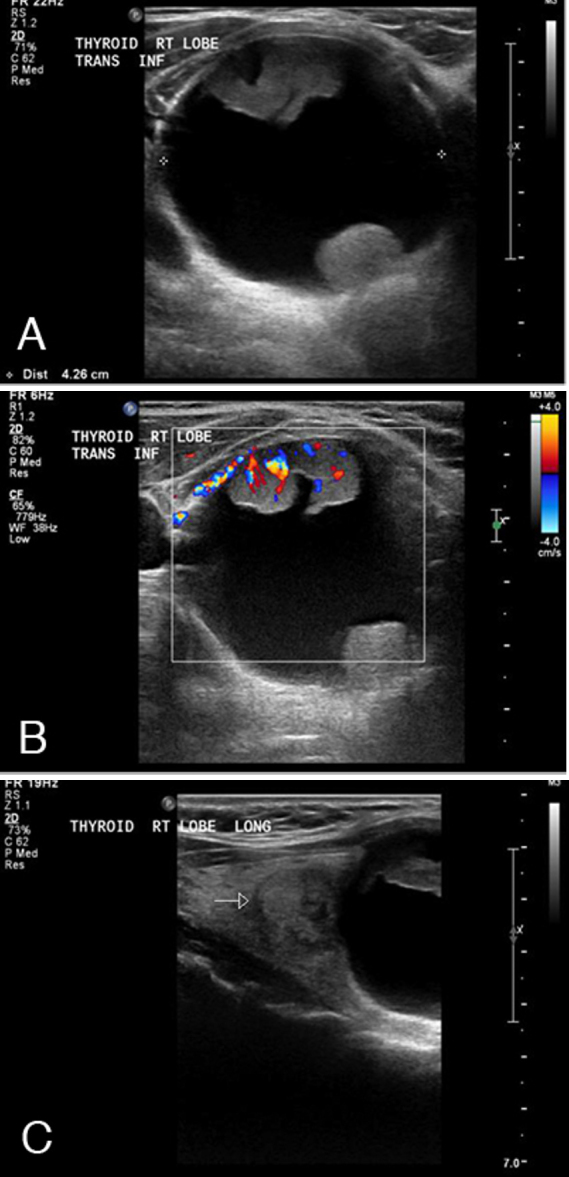
39-year-old female with parathyroid carcinoma. Neck sonogram.
Dual-tracer nuclear parathyroid imaging (Fig. 3) was then performed. The anterior pinhole Technetium-99m-Pertechnetate (72MBq/1.9mCi) image (Fig. 3A) showed focal tracer uptake within the right thyroid lobe, corresponding to the circumscribed thyroid nodule identified on ultrasound. Mild suppression of uptake was seen throughout the remainder of the thyroid gland. A large photopenic defect was seen below the right lobe, corresponding to the palpable complex cystic neck mass. The anterior pinhole technetium-99m-sestamibi (802MBq/21.7mCi) image (Fig. 3B) (injected with the patient lying on the camera bed in the same position as for the thyroid scan) showed focally avid concordant uptake corresponding to the right thyroid lesion. Low-grade, discordant sestamibi uptake was seen below the right thyroid lobe in the region of the palpable complex cystic neck mass. This uptake was confirmed on a pertechnetate-subtracted sestamibi image (Fig. 3C, arrow) and was found to localize to the solid components of the complex cystic neck mass on coregistered single photon emission computed tomography/computed tomography (SPECT/CT) (Fig. 4). Delayed 4-hour sestamibi images showed no significant preferential retention of sestamibi in either of the two lesions (images not shown). The combined scan findings suggested dual pathology with a functioning thyroid nodule showing avidity for both tracers, and a predominantly cystic parathyroid lesion with only mild sestamibi uptake and no pertechnetate uptake.
Fig. 3.
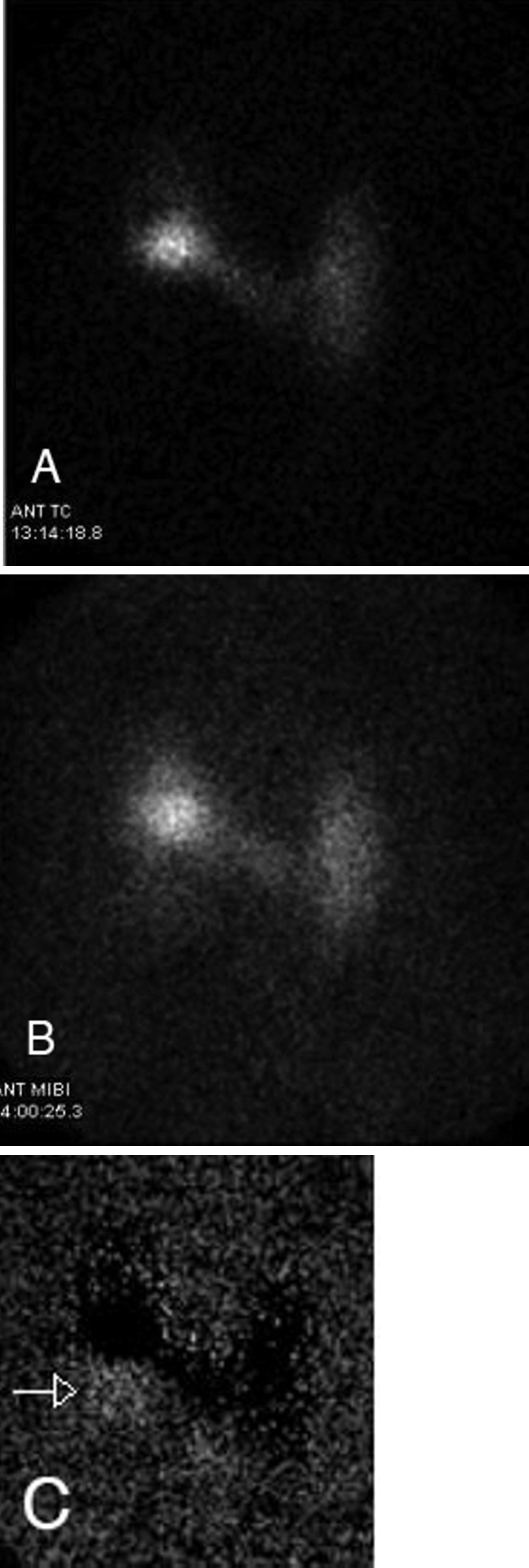
39-year-old female with parathyroid carcinoma. Dual-tracer nuclear parathyroid scan. A. Anterior pertechnetate image. B. Anterior sestamibi image. C. Anterior sestamibi image (pertechnetate subtracted).
Fig. 4.
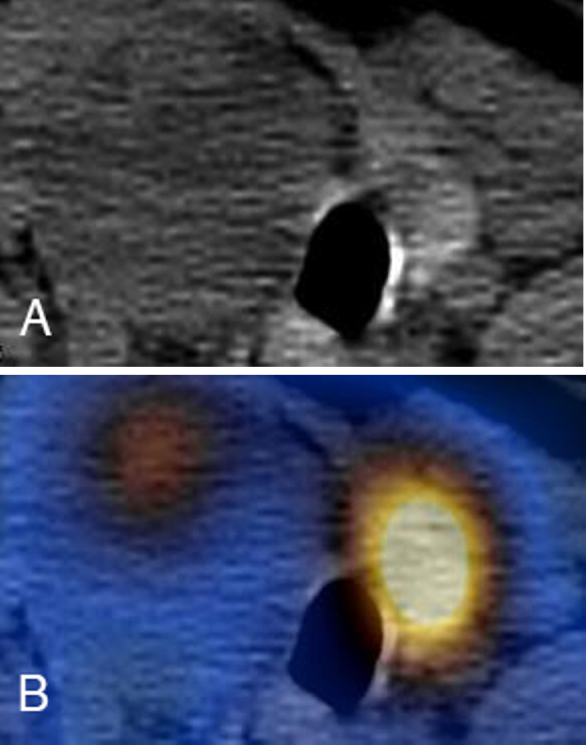
39-year-old female with parathyroid carcinoma. Axial CT (A) and coregistered SPECT/CT (B) of the neck.
The patient subsequently underwent right hemithyroidectomy and inferior/superior right parathyroidectomy, with normalization of calcium homeostasis postoperatively. Gross pathology (Fig. 5A) revealed a 43x30-mm circumscribed mass with a smooth gray external surface. Internally, the mass showed haemorrhagic cystic contents with small, firm, white excrescences. Specimen histology (Fig. 5B) confirmed a parathyroid neoplasm with a hyaline fibrous capsule, showing minimally pleomorphic cells. The foci of vascular (Fig. 5B, arrow) and capsular invasion were identified, consistent with parathyroid carcinoma. The surgical margins, and central neck compartment node sampling, were clear. The right thyroid lobe specimen also confirmed a circumscribed adenoma (images not shown).
Fig. 5.
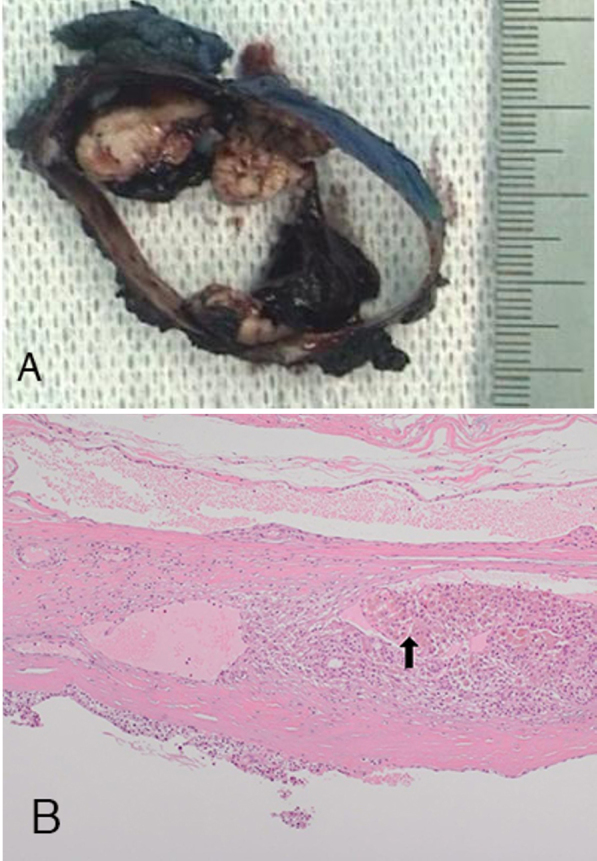
39-year-old female with parathyroid carcinoma. (A) Macrocopic parathyroid specimen and (B) histopathology (haematoxylin and eosin, x100) (arrow).
Discussion
Although it is a rare cause of PTH-dependent hypercalcemia, parathyroid carcinoma is being diagnosed with increasing frequency (1). Clinical indicators of carcinoma include severe hyperparathyroidism, a palpable neck mass, or parathyroid gland size greater than 3 cm (2, 3). Typical sonographic features of parathyroid carcinoma include nonhomogeneous lesion morphology and frequent cystic degeneration (3). In addition to characterizing parathyroid lesions, preliminary ultrasound also enables assessment of thyroid architecture. Definitive histologic features of carcinoma include vascular or capsular invasion (4).
Dual-tracer parathyroid imaging is extremely useful in pre-operative localization of parathyroid adenoma (sensitivity 89%-98%), although it is less reliable in distinguishing adenoma from carcinoma (5, 6). Mitochondrial uptake of sestamibi in abnormal parathyroid tissue is the primary mechanism underpinning lesion localization (7). The parathyroid lesion in our case showed only subtle sestamibi uptake, confined to the small-volume solid components of the tumor. Cystic parathyroid lesions are a recognized cause of false-negative sestamibi imaging, and accuracy is vastly improved when SPECT imaging is acquired and interpreted in conjunction with ultrasound (8). Sestamibi uptake within the thyroid gland is a potential source of false-positive imaging (6), and initial pertechnetate imaging performed in our case was useful for localizing the most intense focus of sestamibi uptake to the pertechnetate-avid right thyroid lobe adenoma. The thyroid lesion was also readily apparent on the preliminary ultrasound, and accounted for the patient's subclinical hyperthyroidism. This case underlines the importance of concurrent imaging of the thyroid gland, and emphasizes the additional value of SPECT/CT when performing a nuclear parathyroid study, particularly in areas with a high prevalence of goiter or thyroid disease.
Our patient also underwent whole-body Fluorine-18-Fluorodeoxyglucose positron emission tomography (F-18-FDG-PET; images not shown) following surgical resection, without evidence of metastases. Early experience suggests that F-18-FDG-PET is sensitive in staging and restaging parathyroid carcinoma (9). Parathyroid carcinoma is generally indolent, but progressive, with overall relative survival at 5 and 10 years in one large series being 85.5% and 49.1%, respectively (10).
Footnotes
Published: March 28, 2015
References
- 1.Lee PK, Jarosek SL, Virnig BA, Evasovich M, Tuttle TM. Trends in the incidence and treatment of parathyroid cancer in the United States. Cancer. 2007;109(9):1736–1741. doi: 10.1002/cncr.22599. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.DeLellis RA, Mazzaglia P, Mangray S. Primary hyperparathyroidism: a current perspective. Arch Pathol Lab Med. 2008;132(8):1251–1262. doi: 10.5858/2008-132-1251-PHACP. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Halenka M, Karasek D, Frysak Z. Four ultrasound and clinical pictures of parathyroid carcinoma. Case Rep Endocrinol. 2012;2012:363690. doi: 10.1155/2012/363690. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Åkerström G, Hellman P, Björklund P. Parathyroid Carcinoma. In: Hay ID, Wass JAH, editors. Clinical Endocrine Oncology. 2nd ed. Blackwell Publishing; 2008. pp. 180–184. [Google Scholar]
- 5.Abdelgadir Adam M, Untch BR, Olson JA., Jr. Parathyroid carcinoma: Current understanding and new insights into gene expression and intraoperative parathyroid hormone kinetics. Oncologist. 2010;15(1):61–72. doi: 10.1634/theoncologist.2009-0185. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen CC, Holder LE, Scovili WA, Tehan AM, Gann DS. Comparison of parathyroid imaging with technetium-99m-pertechnetate/sestamibi subtraction, double-phase technetium-99m-sestamibi and technetium-99m-sestamibi SPECT. J Nucl Med. 1997;38(6):834–839. [PubMed] [PubMed] [Google Scholar]
- 7.Hetrakul N, Civelek AC, Stagg CA, Udelsman R. In vitro accumulation of technetium-99m-sestamibi in human parathyroid mitochondria. Surgery. 2001;130(6):1011–1018. doi: 10.1067/msy.2001.118371. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Johnson NA, Yip L, Tiblin ME. Cystic parathyroid adenoma: sonographic features and correlation with 99mTc-sestamibi SPECT findings. Am J Roentenol. 2010;195(6):1385–1390. doi: 10.2214/AJR.10.4472. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Evangelista L, Sorgato N, Torresan F. FDG-PET/CT and parathyroid carcinoma: Review of literature and illustrative case series. World J Clin Oncol. 2011;2(10):348–354. doi: 10.5306/wjco.v2.i10.348. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hundahl SA, Fleming ID, Fremgen AM, Menck HR. Two hundred eighty-six cases of parathyroid carcinoma treated in the U.S between 1985-1995: a National Cancer Data Base Report. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer. 1999;86(3):538–544. doi: 10.1002/(sici)1097-0142(19990801)86:3<538::aid-cncr25>3.0.co;2-k. [PubMed] [DOI] [PubMed] [Google Scholar]


