Abstract
Background
It is unknown if low back pain (LBP) outcomes are enhanced by classification-specific treatment based on the Movement System Impairment classification system. The moderating effect of adherence to treatment also is unknown.
Objectives
Compare the efficacy of a classification-specific treatment (CS) and a non-classification specific (NCs) treatment and examine the moderating effect of adherence on outcomes.
Design
2 center, 2 parallel group, prospective, randomized, clinical trial.
Method
Participants with chronic LBP were classified and randomized. Self-report data was obtained at baseline, post-treatment, and 6 and 12 months post-treatment. The primary outcome was the modified Oswestry Disability Index (mODI; 0–100%). Treatment effect modifiers were exercise adherence and performance training adherence. An intention to treat approach and hierarchical linear modeling were used.
Results
47 people received CS treatment, 54 people received NCs treatment. Treatment groups did not differ in mODI scores (p>.05). For both groups, scores improved with treatment (p<.05), plateaued at 6 months (p>.05), and minimally regressed at 12 months (p<.05). Performance training adherence had a unique, independent effect on mODI scores above and beyond the effect of exercise adherence (p<.05). There were no treatment group effects on the relationship between mODI scores and the two types of adherence (p<.05).
Conclusions
There were no differences in function between the two treatment groups (CS and NCs). In both treatment groups, people with chronic LBP displayed clinically important long-term improvements in function. When both forms of adherence were considered, the improvements were uniquely related to adherence to performance training.
Keywords: Classification, Low Back Pain, Adherence
INTRODUCTION
At least 60%–80% of adults will experience mechanical low back pain (LBP) in their lifetime [1] and almost 50% of them will have had an episode of LBP by age 30.[2] Recurrence rates within a year of LBP onset are as high as 78% [3] and recovery rates are poor.[4, 5] Chronic LBP is the most common type of chronic pain in adults[5] and its prevalence is increasing.[6, 7] Thus, for many people LBP is a long-term, function-limiting condition rather than a short-term, self-limiting condition.[4, 8–11]
Currently exercise is one of the primary non-surgical approaches used for managing LBP.[12–15] For chronic LBP exercise is as efficacious, if not more efficacious than (1) no treatment, (2) usual care, and (3) many other treatments such as massage or laser therapy.[12, 13, 16–19] Despite the accumulating evidence for the beneficial effects of exercise in chronic LBP there is no evidence that any particular type of exercise is clearly and consistently more efficacious than any other, particularly with regard to long-term outcomes.[15] Some have suggested that the lack of evidence for any one treatment is the result of investigators studying imprecisely defined groups of people with LBP [20–23] and prescribing inadequate doses.[16, 24, 25] The proposed solution is to focus on people with LBP who have been classified based on clinically-relevant variables[21, 23, 26] and to provide effective doses of treatments.
One system that was developed to classify a person’s LBP is the Movement System Impairment (MSI) classification system.[27, 28] The premise underlying the classification system is that LBP develops because people repeatedly use direction-specific, stereotypic movement and alignment patterns of the lumbar spine across their day. The patterns are characterized by the lumbar spine moving more readily than other joints during performance of movements or assumption of postures. Use of the same patterns is proposed to contribute to sub-failure magnitude loading that, over time, contributes to LBP symptoms. Patterns are identified during a defined examination[29–31] as well as during performance of symptom-provoking functional activities. The findings are then used to classify the person’s LBP.[29, 32–34] The LBP categories are named for the altered movements and alignments that are (1) displayed consistently across clinical tests, and (2) associated with symptoms.[27, 28] Modification of the specific patterns associated with the person’s LBP classification is addressed through exercises and training to change performance of direction-specific movements and alignments during functional activities. Reliability of examiners to classify using the system has been documented.[32–36] Various aspects of the validity of the system also have been tested.[28, 35–38] The system is used widely but there is no evidence that outcomes are enhanced by classifying and providing classification-specific treatment.
One factor that affects the dose of treatment in people with chronic LBP is treatment adherence. [39] There is evidence that emphasizing adherence to activity-based treatments results in higher doses of treatment and better outcomes than are achieved without an emphasis on adherence.[16, 40] Despite improved outcomes and recommendations to examine the effects of adherence on outcomes[13, 16, 17, 24, 41] examination of the moderating effects of adherence on outcomes in people with chronic LBP is rarely examined.
The purpose of this study was to (1) compare the efficacy of Classification-Specific (CS) treatment and Non Classification-Specific (NCs) treatment, and (2) examine the moderating effects of adherence on outcomes in people with chronic LBP. We hypothesized that the (1) CS group would demonstrate greater improvement in function than the NCs group, (2) the classification subgroups receiving CS treatment would demonstrate greater improvement in function than the classification subgroups receiving NCS treatment, and (3) adherence would moderate the effect of treatment on outcomes.
METHODS
Study Design
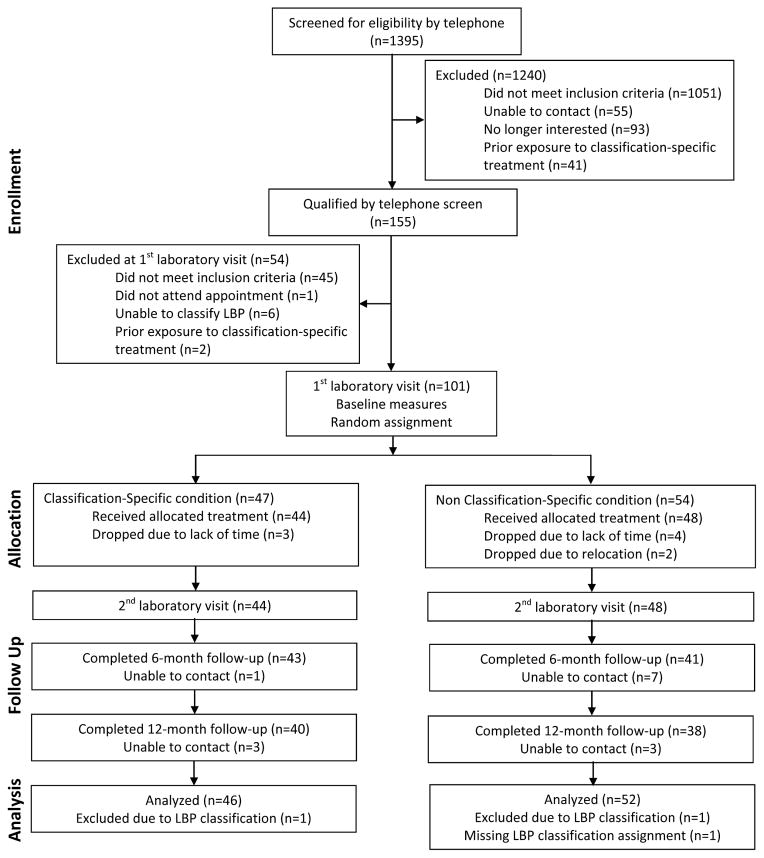
Our study was a 2-parallel group, 2-center, prospective, single blind, randomized clinical trial in people with chronic LBP. Duration of treatment was 6 weeks; data were collected before and immediately after treatment, and 6 and 12 months later. Recruitment spanned February 2007 through August 2009. Final follow-up outcomes were collected in October 2011. The study events are in Figure 1. The trial was funded by grant R01 HD047709-04 from the National Institute of Child Health and Human Development. The protocol used for the trial was approved by the Human Research Protection Office at X (IRB #: 201107034). The trial ended upon attainment of all of the 12 month outcomes. There were no changes to the trial design after commencement of the study. The trial was registered on Clinicaltrials.gov (NCT00802724).
Figure 1.
Study flow diagram.
Setting and Participants
Recruitment strategies included placing flyers in the local community and in physician offices, and placing ads in local media. Testing was conducted in the X. Data were collected using self-report measures, laboratory instruments, and a defined clinical exam.[29–31] When treatment visits were completed, self-report data were collected via electronic mail 6 and 12 months later.
People included were between 18 and 60 years, had chronic LBP for at least 12 months, were able to (1) stand and walk without assistance, (2) understand and read English, and (3) understand and sign a consent form. People excluded were in an acute flare-up,[9] had a history or diagnosis of spinal deformity, disc herniation, pain or paresthesia below the knee,[42, 43] systemic inflammatory condition, primary hip problem, other serious medical condition, reported any spinal fracture or surgery, displayed magnified symptom behavior,[44] were pregnant, receiving worker’s compensation or disability benefits, were involved in pending litigation for their LBP, or referred from a specialized pain clinic.
Classification of Low Back Pain
The MSI LBP categories that could be included were lumbar flexion, lumbar extension, lumbar rotation, lumbar flexion-rotation, and lumbar extension-rotation.[27] Each participant’s LBP was classified based on the results of a trained therapist’s clinical exam.[32–34, 36] Six people whose LBP the therapist could not classify were not enrolled.
Randomization
The sample was stratified based on LBP category. Randomization was conducted separately for each clinic using a computer-generated list of random numbers provided by an investigator (MJS) who was not involved in outcome assessment. The randomization scheme was prepared before the trial began and was followed throughout the trial. For each clinic, group assignments were placed in sequentially-numbered, sealed envelopes. Envelopes were separated into 5 groups corresponding to the 5 LBP classifications. Upon completion of the initial visit, the participant was assigned to a clinic. Then the clinic’s office assistant drew the participant’s treatment assignment based on the LBP classification and scheduled the clinic visit. Participants were not masked to treatment assignment.
Treating Therapists
Table 1 provides the characteristics of the therapists. Each therapist was trained by one of the investigators (LVD) to implement one of the treatment protocols (CS or NCs). Training included 8 hours of review of a procedure manual and practice in treatment implementation, progression, and documentation. Each therapist was required to pass a written and practical exam annually. Charts were audited for treatment fidelity by a person not involved in outcome assessment. NCs therapists were masked to LBP classification. Therapists were not masked to treatment assignment.
TABLE 1.
Characteristics of Therapists Providing Treatment in the Two Treatment Conditions
| Treatment Condition
|
||
|---|---|---|
| Classification-Specific (n=2) | Non Classification-Specific (n=4) | |
| Characteristics | ||
|
| ||
| Male, % | 50 | 25 |
| Entry-level physical therapy education, % | ||
| BSPT* | 50 | 25 |
| MSPT** | 50 | 75 |
| Years in practice (SD) | 7.5 (3.4) | 12.5 (7.5) |
| Exposure to classification system and treatment (%)¶ | 0 | 100 |
| Number of therapists: Clinic 1 | 1 | 2 |
| Number of therapists: Clinic 2 | 1 | 2 |
Bachelor’s degree in physical therapy
Master’s degree in physical therapy
One method to control for bias was to use therapists in the Non Classification-Specific condition that had no exposure to the concept of classification or the specific details of treatment based on the Movement System Impairment Classification system.
Overview of Treatment Conditions
Treatment was provided at 2 outpatient physical therapy clinics; a university-based clinic and a private hospital. Both treatment conditions included 3 components: education, exercise, and training to modify how functional activities were performed, hereinafter referred to as performance training. In the CS condition, treatment items were selected based on the participant’s LBP classification; in the NCs condition, analogous generic items were used. Participants in both treatment groups attended 1 hour sessions weekly for 6 weeks. Equal time was devoted to the 3 treatment components until participants learned the educational principles. Time then was divided equally between exercise and performance training.
Progression was based on the participant’s ability to perform the appropriate number of repetitions of an item independently.[45] At the 1st visit, participants were given a home program. The program was progressed based on defined criteria (Supplemental Digital File 1).[45, 46] For exercises that could no longer be increased in difficulty, the participant was instructed to perform the exercise repeatedly to increase endurance based on ACSM guidelines. At the final treatment visit, participants were instructed to continue their home program (Supplemental Digital File 1).
Classification-Specific Condition
The 3 components of the CS treatment were aimed at the movement and alignment patterns consistent with a participant’s specific LBP classification. Exercises and positioning were prescribed for control of symptoms and for movement control. Performance training included instruction and practice in modifying the patterns used with specific, symptom-provoking activities. The primary goals of training were to teach each participant to (a) move the lumbar spine later and reduce the amount of lumbar spine movement in the directions related to the participant’s classification, (b) increase use of other joints such as the hips and knees, and (3) avoid end-range positioning of the lumbar spine in the directions related to the participant’s classification.
Non Classification-Specific Treatment Condition
The 3 components of the NCs prescription were derived from the literature.[47–53] Exercise was directed at improving the strength of all of the trunk muscles and improving trunk and lower limb flexibility in all planes of motion. All exercises were progressed based on ACSM guidelines.[46] Performance training involved instruction and practice of activities described in a booklet entitled “Managing Back Pain”.[54] The primary goal of training was to teach the participant to maintain the “normal spinal curves” during performance of activities and assumption of postures.
Outcomes and Follow-up
Outcomes were measured at baseline, after the last treatment visit, and 6 and 12 months later (Table 2). Testers were masked to treatment assignment throughout the study duration. A subset of the self-report outcomes also was completed at each treatment visit. The primary outcome was LBP-related functional limitation measured with the modified Oswestry Disability Index (mODI).[55] The treatment effect modifiers were adherence to (1) exercise, and (2) performance training.
TABLE 2.
Outcome and Treatment Effect Modifier Summary Table
| Time and Location of Collection
|
|||||
|---|---|---|---|---|---|
| Baseline (Laboratory Visit 1) | Each Treatment (Clinic) | Immediately Post-Treatment | 6 Months Post-Treatment (Email) | 12 Months Post-Treatment (Email) | |
| Outcome | |||||
|
| |||||
| modified Oswestry Disability Index[55] (0–100%) | X | X | X | X | X |
| Numeric Rating Scale of pain intensity[56] (0–10) | |||||
| Current | X | X | X | X | X |
| Average over prior 7 days | X | X | X | X | X |
| Worst over prior 7 days | X | X | X | X | X |
| Best over prior 7 days | X | X | X | X | X |
| Medication use (yes, no) | X | X | X | X | X |
| Days of LBP-related time off in prior 6 months[57] (number)* | X | X | X | ||
| Baecke Habitual Activity Questionnaire[58,59] (3–15) | X | X | X | X | |
| Fear Avoidance Beliefs Questionnaire Work (0–42) and Physical Activity (0–24) Subscales[60–63] | X | X | X | X | |
| SF-36 Health Status Questionnaire: Physical and Mental Component Summaries[64–66] (0–100%) | X | X | X | X | |
| Satisfaction with care[767] (15–75) | X | ||||
|
| |||||
| Treatment Effect Modifier | |||||
|
| |||||
| Adherence (0–100%) | |||||
| Exercise | X# | X | X | ||
| Functional activities | X# | X | X | ||
Question number 5 of the Graded Chronic Pain Scale.[57]
During treatment phase adherence measured at each treatment visit after treatment visit 1.
Secondary outcomes included (1) the Numeric Pain Rating Scale,[56] (2) medication use, (3) LBP-related time off,[57] (4) activity level,[58, 59] (5) the Fear Avoidance Beliefs Questionnaire (FABQ),[60–63] (6) the Short Form-36,[64–66] and (7) satisfaction with care.[67]
Adherence
A self-report measure was used to assess adherence. Each day during the treatment phase, participants recorded their adherence to (1) exercise, and (2) performance training separately. Specifically, they recorded the percentage (0–100%) of exercises and the percentage of performance training activities they performed as instructed by their therapist. In addition, at the beginning of each treatment visit, the therapist asked the participant to provide a verbal estimate of his ‘average’ adherence (0–100%) to each of the treatment components since the prior visit. Consistency between the two adherence reports was examined. Adherence measures for exercise and performance training also were obtained by self-report at 6 and 12 months after treatment.
Statistical Analysis
The sample size was based on a power analysis using a general linear model framework. Because there were no prior studies that had examined the effect of treatment based on the MSI model the effect size chosen was based on a range of effect sizes obtained in past research.[47, 49, 68, 69] The assumption was that, given the targeted nature of a classification-based treatment, the MSI-directed treatment would have at least the same effect size as obtained in past studies. The basic design assumed a treatment effect within any time period equal to 10% of the primary outcome variance explained, with 8 degrees of freedom in the model (2 treatment groups (1 df), 3 classifications (2 df), and an interaction component reflecting how treatment could depend on classification (2 df)). In addition, the analysis assumed that 3 additional variables would be controlled. A .05 level of significance (2-tailed), a minimum power of .80, and a dropout rate of 20% was assumed. The required sample size was approximately 100 cases (17/cell of the basic 2X3 design).
We used an intention to treat approach and hierarchical linear modeling (HLM) to examine longitudinal effects.[70–73] HLM is appropriate for longitudinal data that contains differing intervals between measurements, different patterns of missing data, inclusion of time-varying covariates, and outcomes that can be either continuous or categorical. Missing data were addressed via maximum likelihood estimation and multiple imputation. Because conclusions were similar using each approach, the results from the simpler maximum likelihood approach are reported.[74, 75]
HLM is a regression modelling approach that seeks to represent the probable path for participants over time. It does this by constructing a model of response at (in our case) two levels. For each measure, individual outcomes over time were modeled at Level 1 and moderators of individual outcome trajectories (i.e., treatment and LBP classification; adherence) were modeled at Level 2. Each Level 1 analysis estimated each individual’s intercept, linear component, and quadratic component for the outcome (e.g., mODI scores) trajectory over time. At Level 2, the variability in the coefficients for the intercept, the linear component, and the quadratic component from Level 1 were modeled as a function of group membership (using dummy variables). Specific contrasts of the Level 2 dummy variables were calculated to test for the (1) main effects of treatment and classification, and (2) interaction between them. Models were tested using 3 locations for the time variable. This has the effect of changing the interpretation of the intercept (it is the estimated outcome at the time locations) and the linear parameter (it is the instantaneous rate of change at the time location).
Results for the HLM analyses for mODI scores and the 2 types of adherence are provided in Tables 3–5 and Figures 2–4, and for the secondary outcomes in Tables 1–11 and Figures 1–11 (Supplemental Digital File 2). Within each table, results for the 3 Level 1 parameters (intercept, linear, and quadratic) of the model are provided for the 4 groups (CS Rot, CS ExtRot, NCs Rot, NCs ExtRot ) at each of 3 data collection points (post-treatment, 6 and 12 months post-treatment). The beta coefficients for the intercept are the expected scores for the outcome measure at the data collection point. The beta coefficients for the linear component are the slopes of the tangents to the curves at the data collection point and can be interpreted as the rate of change in the outcome at that point. That is, the coefficients indicate for a specific time point (1) whether the outcome scores are increasing or decreasing, and (2) the rate of that increase or decrease. The beta coefficients for the quadratic component indicate the rate at which the linear component of the curve is changing; these results are not dependent on the time point analyzed and indicate the nature and magnitude of curvilinearity. Each parameter has a standard error as well as a significance test indicating if the parameter is different from zero. These are relevant for the linear and quadratic components (the intercepts will usually be different from zero given the scaling of the measures). It is also possible to compare the parameters estimated for the 4 different groups; these comparisons (chi square tests in HLM) are indicated by superscripts to the subsection headings. The particular comparisons reported correspond to the main effects and the interaction of treatment group and classification group. Also reported is a test of significance for the grand mean of the linear component and of the quadratic component. These collapse across all groups and indicate the significance of the overall outcome trajectory parameters.
TABLE 5.
Results of Hierarchical Linear Modeling Analyses of the Exercise Adherence Scores over Time and Specific Contrasts of Treatment Group and Classification Group at Post-Treatment and 6 and 12 Month Follow-up
| Post-Treatment | |||||
|---|---|---|---|---|---|
| Fixed Effect | Beta Coefficient | SE | t-ratio | df | p-value |
| Level 1 Intercept | |||||
| CS Rot | 73.807 | 3.944 | 18.716 | 90 | <0.001 |
| CS ExtRot | 71.113 | 5.065 | 14.039 | 90 | <0.001 |
| NCs Rot | 74.387 | 2.879 | 25.841 | 90 | <0.001 |
| NCs ExtRot | 74.028 | 2.986 | 24.793 | 90 | <0.001 |
| Level 1 Lineard | |||||
| CS Rot | −0.976 | 0.228 | −4.289 | 90 | <0.001 |
| CS ExtRot | −1.290 | 0.410 | −3.143 | 90 | 0.002 |
| NCs Rot | −1.598 | 0.393 | −4.068 | 90 | <0.001 |
| NCs ExtRot | −1.665 | 0.411 | −4.054 | 90 | <0.001 |
| Level 1 Quadraticd | |||||
| CS Rot | 0.003 | 0.005 | 0.559 | 409 | 0.576 |
| CS ExtRot | 0.011 | 0.009 | 1.209 | 409 | 0.227 |
| NCs Rot | 0.018 | 0.009 | 2.096 | 409 | 0.037 |
| NCs ExtRot | 0.019 | 0.010 | 1.863 | 409 | 0.063 |
| 6 Month | |||||
|---|---|---|---|---|---|
| Fixed Effect | Coefficient | SE | t-ratio | df | p-value |
| Level 1 Intercept | |||||
| CS Rot | 57.232 | 5.140 | 11.135 | 90 | <0.001 |
| CS ExtRot | 51.378 | 8.107 | 6.337 | 90 | <0.001 |
| NCs Rot | 51.627 | 6.529 | 7.907 | 90 | <0.001 |
| NCs ExtRot | 50.405 | 6.089 | 8.279 | 90 | <0.001 |
| Level 1 Lineard | |||||
| CS Rot | −0.869 | 0.117 | −7.452 | 90 | <0.001 |
| CS ExtRot | −0.907 | 0.144 | −6.322 | 90 | <0.001 |
| NCs Rot | −0.936 | 0.149 | −6.292 | 90 | <0.001 |
| NCs ExtRot | −0.965 | 0.148 | −6.517 | 90 | <0.001 |
| Level 1 Quadraticd | |||||
| CS Rot | 0.003 | 0.005 | 0.559 | 409 | 0.576 |
| CS ExtRot | 0.011 | 0.009 | 1.209 | 409 | 0.227 |
| NCs Rot | 0.018 | 0.009 | 2.096 | 409 | 0.037 |
| NCs ExtRot | 0.019 | 0.010 | 1.863 | 409 | 0.063 |
| 12 Month | |||||
|---|---|---|---|---|---|
| Fixed Effect | Coefficient | SE | t-ratio | df | p-value |
| Level 1 Intercept | |||||
| CS Rot | 41.906 | 5.600 | 7.483 | 90 | <0.001 |
| CS ExtRot | 38.056 | 8.292 | 4.590 | 90 | <0.001 |
| NCs Rot | 40.525 | 6.912 | 5.863 | 90 | <0.001 |
| NCs ExtRot | 39.121 | 6.264 | 6.246 | 90 | <0.001 |
| Level 1 Lineard | |||||
| CS Rot | −0.757 | 0.229 | −3.301 | 90 | 0.001 |
| CS ExtRot | −0.506 | 0.284 | −1.781 | 90 | 0.078 |
| NCs Rot | −0.242 | 0.313 | −0.772 | 90 | 0.442 |
| NCs ExtRot | −0.231 | 0.414 | −0.560 | 90 | 0.577 |
| Level 1 Quadraticd | |||||
| CS Rot | 0.003 | 0.005 | 0.559 | 409 | 0.576 |
| CS ExtRot | 0.011 | 0.009 | 1.209 | 409 | 0.227 |
| NCs Rot | 0.018 | 0.009 | 2.096 | 409 | 0.037 |
| NCs ExtRot | 0.019 | 0.010 | 1.863 | 409 | 0.063 |
CS Rot = Classification-Specific, Rotation, CS ExtRot = Classification-Specific, Extension-Rotation, NCs Rot = Non Classification-Specific, Rotation, NCs ExtRot = Non Classification-Specific, Extension-Rotation.
Superscripts indicate the results of tests of Level 2 effects.
Treatment Group Effect: (CS Rot + CS ExtRot) vs. (NCs Rot + NCs ExtRot), p<.05.
Classification Group Effect: (CS Rot + NCs Rot) vs. (CS ExtRot + NCs ExtRot), p<.05.
Treatment × Classification Group Interaction: (CS Rot + NCs ExtRot) vs. (CS ExtRot + NCs Rot), p<.05.
Grand Mean, p<.05. (Tested for the linear and quadratic component)
TABLE 3.
Results of Hierarchical Linear Modeling Analyses of the Modified Oswestry Disability Index Scores over Time and Specific Contrasts of Treatment Group and Classification Group at Post-Treatment and 6 and 12 Month Follow-up
| Post-Treatment | |||||
|---|---|---|---|---|---|
| Fixed Effect | Beta Coefficient | SE | t-ratio | df | p-value |
| Level 1 Intercept | |||||
| CS Rot | 15.092 | 1.586 | 9.518 | 90 | <0.001 |
| CS ExtRot | 14.301 | 2.030 | 7.045 | 90 | <0.001 |
| NCs Rot | 17.219 | 1.421 | 12.122 | 90 | <0.001 |
| NCs ExtRot | 13.695 | 1.813 | 7.553 | 90 | <0.001 |
| Level 1 Lineard | |||||
| CS Rot | −0.609 | 0.116 | −5.268 | 90 | <0.001 |
| CS ExtRot | −0.625 | 0.143 | −4.365 | 90 | <0.001 |
| NCs Rot | −0.702 | 0.141 | −4.968 | 90 | <0.001 |
| NCs ExtRot | −0.878 | 0.120 | −7.318 | 90 | <0.001 |
| Level 1 Quadraticd | |||||
| CS Rot | 0.014 | 0.003 | 4.256 | 688 | <0.001 |
| CS ExtRot | 0.017 | 0.004 | 4.875 | 688 | <0.001 |
| NCs Rot | 0.014 | 0.004 | 3.441 | 688 | <0.001 |
| NCs ExtRot | 0.025 | 0.004 | 5.936 | 688 | <0.001 |
| 6 Month | |||||
|---|---|---|---|---|---|
| Fixed Effect | Beta Coefficient | SE | t-ratio | df | p-value |
| Level 1 Intercept | |||||
| CS Rot | 8.812 | 1.817 | 4.849 | 90 | <0.001 |
| CS ExtRot | 8.605 | 2.315 | 3.718 | 90 | <0.001 |
| NCs Rot | 9.004 | 2.364 | 3.808 | 90 | <0.001 |
| NCs ExtRot | 6.107 | 2.179 | 2.803 | 90 | 0.006 |
| Level 1 Linearb,d | |||||
| CS Rot | −0.091 | 0.061 | −1.49 | 90 | 0.140 |
| CS ExtRot | −0.009 | 0.051 | −0.181 | 90 | 0.857 |
| NCs Rot | −0.213 | 0.043 | −4.936 | 90 | <0.001 |
| NCs ExtRot | 0.033 | 0.082 | 0.408 | 90 | 0.685 |
| Level 1 Quadraticd | |||||
| CS Rot | 0.014 | 0.003 | 4.256 | 688 | <0.001 |
| CS ExtRot | 0.017 | 0.004 | 4.875 | 688 | <0.001 |
| NCs Rot | 0.014 | 0.004 | 3.441 | 688 | <0.001 |
| NCs ExtRot | 0.025 | 0.004 | 5.936 | 688 | <0.001 |
| 12 Month | |||||
|---|---|---|---|---|---|
| Fixed Effect | Beta Coefficient | SE | t-ratio | df | p-value |
| Level 1 Intercept | |||||
| CS Rot | 12.226 | 2.574 | 4.751 | 90 | <0.001 |
| CS ExtRot | 14.523 | 2.316 | 6.271 | 90 | <0.001 |
| NCs Rot | 9.816 | 1.634 | 6.007 | 90 | <0.001 |
| NCs ExtRot | 15.750 | 3.243 | 4.856 | 90 | <0.001 |
| Level 1 Linearb,d | |||||
| CS Rot | 0.453 | 0.159 | 2.841 | 90 | 0.006 |
| CS ExtRot | 0.637 | 0.134 | 4.737 | 90 | <0.001 |
| NCs Rot | 0.299 | 0.162 | 1.849 | 90 | 0.068 |
| NCs ExtRot | 0.990 | 0.222 | 4.461 | 90 | <0.001 |
| Level 1 Quadraticd | |||||
| CS Rot | 0.014 | 0.003 | 4.257 | 688 | <0.001 |
| CS ExtRot | 0.017 | 0.004 | 4.875 | 688 | <0.001 |
| NCs Rot | 0.014 | 0.004 | 3.441 | 688 | <0.001 |
| NCs ExtRot | 0.025 | 0.004 | 5.936 | 688 | <0.001 |
CS Rot = Classification-Specific, Rotation, CS ExtRot = Classification-Specific, Extension-Rotation, NCs Rot = Non Classification-Specific, Rotation, NCs ExtRot = Non Classification-Specific, Extension-Rotation.
Superscripts indicate the results of tests of Level 2 effects.
Treatment Group Effect: (CS Rot + CS ExtRot) vs. (NCs Rot + NCs ExtRot), p<.05.
Classification Group Effect: (CS Rot + NCs Rot) vs. (CS ExtRot + NCs ExtRot), p<.05.
Treatment × Classification Group Interaction: (CS Rot + NCs ExtRot) vs. (CS ExtRot + NCs Rot), p<.05.
Grand Mean, p<.05. (Tested for the linear and quadratic component)
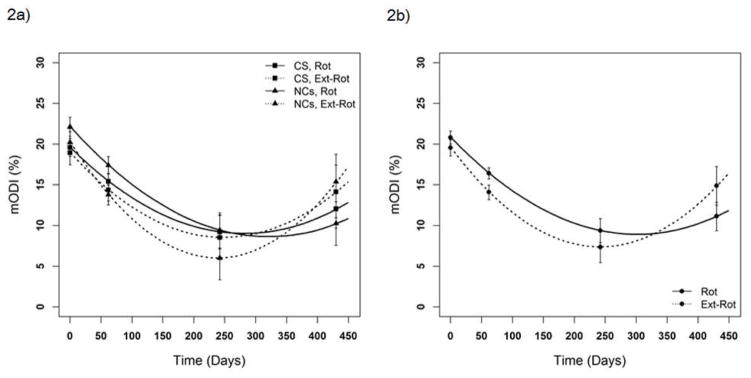
Figure 2.
Figure 2a. Predicted values and 95% confidence intervals based on hierarchical linear modeling analyses of the modified Oswestry Disability Index (mODI) scores for the classification-specific (CS) rotation (Rot) and extension-rotation (ExtRot) groups and the non-classification-specific (NCs) Rot and ExtRot groups at baseline, post-treatment, and 6 and 12 months later. Overall, both groups were improving post-treatment, plateauing at 6 months, and regressing at 12 months (significant overall curvilinearity and significant overall linear effects, i.e., slopes, at each time point; ps<.05). There was no treatment group difference (p>.05).
Figure 2b. Predicted values and 95% confidence intervals based on hierarchical linear modeling analyses of the modified Oswestry Disability Index (mODI) scores for the rotation (Rot) group and the extension-rotation (ExtRot) group at baseline, post-treatment, and 6 and 12 months later. At 6 months the Rot group was continuing to improve while the ExtRot group was plateauing; at 12 months the Rot group was regressing slower than the ExtRot group (significant classification group effect for the linear components, i.e., slopes, at 6 and 12 months; ps<.05).
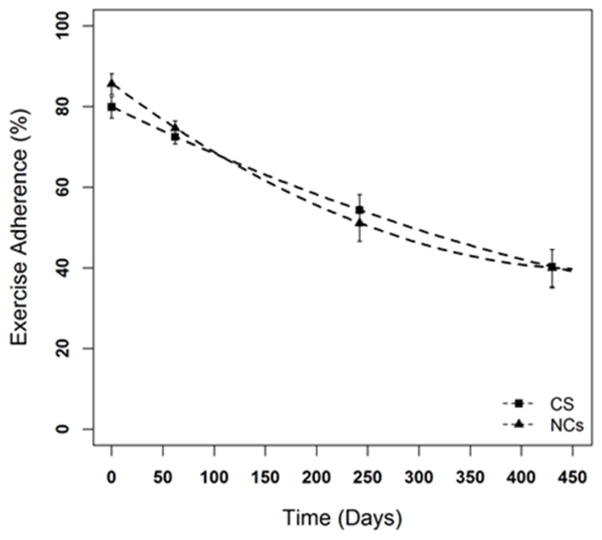
Figure 4.
Predicted values and 95% confidence intervals based on hierarchical linear modeling analyses of the adherence to exercise for the classification-specific (CS) group and the non-classification-specific (NCs) group at the 2nd treatment visit, post-treatment, and 6 and 12 months later. Overall, adherence decreased for both groups over time (significant overall curvilinearity and significant overall linear effects, i.e., slopes, at each time point; ps<.05). There were no treatment or classification group differences (ps>.05).
In addition to these basic analyses, other analyses included adherence as a time-varying predictor of treatment outcome at Level 1. Average individual levels of adherence were also explored in the Level 2 analyses as a moderator of Level 1 parameters.
RESULTS
Study Recruitment and Follow-up
Of the 1395 volunteers who were interviewed (Fig. 1) 155 were eligible for inclusion. After the initial testing at baseline, 54 volunteers were excluded. The remaining 101 participants were assigned to groups randomly. The drop-out rate across the study was 23%. There was no significant difference in the percentages of drop-out between the 2 treatment groups (t=−2.08, df=4, p=.15). Three participants were excluded after completion of all data collection; one because he was missing the classification assignment and 2 classified as lumbar flexion-rotation. These participants were not included in the data analyses (Fig. 1).
Baseline Characteristics and Satisfaction with Care
There were no significant differences in characteristics among the four treatment/classification groups (Table 6). The NCs Rot group reported less satisfaction with care after the treatment phase compared to the CS Rot group (p<.05).
TABLE 6.
Characteristics of Participants With Low Back Pain at Baseline Randomized to Classification-Specific Treatment or Non Classification-Specific Treatment Condition
| Treatment/Classification Subgroupa
|
Statistic Value | p-value | ||||
|---|---|---|---|---|---|---|
| CSb, Rot (n =30) | CSb, Ext-Rot (n = 16) | NCsc, Rot (n= 30) | NCsc, Ext-Rot (n= 22) | |||
| Demographic Variables | ||||||
|
| ||||||
| Male, % | 50 | 63 | 57 | 36 | χ2(3) = 2.81 | .42 |
| White race, % | 90 | 75 | 77 | 91 | χ2(3) = 3.68 | .30 |
| Age (SD), y | 42 (11) | 45 (11) | 42 (11) | 43 (11) | F(3,97) = .35 | .79 |
| Body mass index (SD), kg/m2 | 24 (3) | 25 (3) | 26 (3) | 26 (3) | F(3,97) = 1.11 | .35 |
| Married, % | 63 | 50 | 77 | 73 | χ2(3) = 3.88 | .27 |
| Completed at least some college, % | 93 | 94 | 96 | 90 | χ2(3) = .62 | .89 |
| Employment status, % | ||||||
| Employed full-time | 77 | 75 | 70 | 82 | χ2(12) = 6.10 | .91 |
| Employed part-time | 10 | 12.5 | 13 | 14 | ||
| Student | 7 | 0 | 7 | 0 | ||
| Other employment status | 7 | 12.5 | 7 | 4 | ||
| Not employed | 0 | 0 | 3 | 0 | ||
|
| ||||||
| LBP-Related Variables | ||||||
|
| ||||||
| Duration of LBP (SD), y | 12 (10) | 12 (9) | 8 (6) | 13 (9) | F(3,94) = 1.05 | .37 |
| Original cause of LBP known, % | 43 | 50 | 63 | 36 | χ2(3) = 4.26 | .23 |
| LBP symptoms constant, % | 43 | 38 | 53 | 18 | χ2(3) = 6.78 | .08 |
| Location of symptoms, % | ||||||
| Low back only | 80 | 88 | 93 | 77 | χ2(3) = 3.23 | .35 |
| Low back & proximal LE | 20 | 13 | 7 | 23 | ||
| Number of acute flare-ups in the prior 12 months, % | ||||||
| 0 | 0 | 0 | 0 | 0 | χ2(9) = 1.94 | .22 |
| 1–3 | 48 | 50 | 55 | 52 | ||
| 4–6 | 24 | 36 | 30 | 7 | ||
| 7–9 | 0 | 7 | 5 | 7 | ||
| 10+ | 28 | 7 | 10 | 34 | ||
| Prior treatment for LBP, % | 73 | 56 | 77 | 86 | χ2(3) = 4.53 | .21 |
| Medication use for LBP, % | 67 | 56 | 80 | 68 | χ2(3) = 3.01 | .39 |
| Activity that makes LBP worst, % | ||||||
| Sitting | 43 | 38 | 37 | 18 | χ2(18) = 21.66 | .25 |
| Standing | 23 | 38 | 10 | 27 | ||
| Face lying | 13 | 6 | 30 | 14 | ||
| Back lying | 3 | 0 | 7 | 9 | ||
| Walking | 3 | 6 | 7 | 0 | ||
| Combination of activities | 12 | 6 | 3 | 27 | ||
| Other | 3 | 6 | 7 | 5 | ||
|
| ||||||
| Outcome Measures | ||||||
|
| ||||||
| modified Oswestry Disability Index (SD), 0–100% | 22 (9) | 18 (8) | 25 (7) | 24 (10) | F(3,96) = 2.07 | .11 |
| Numeric Rating Scale of pain intensity (SD) | ||||||
| Current | 3 (2) | 3 (2) | 3 (2) | 3 (2) | F(3,97) = .82 | .49 |
| Average over prior 7 days | 4 (2) | 4 (2) | 4 (2) | 4 (1) | F(3,97) = .20 | .90 |
| Worst over prior 7 days | 6 (2) | 6 (2) | 6 (2) | 6 (2) | F(3,97) = .20 | .90 |
| Best over prior 7 days | 2 (1) | 2 (2) | 2 (1) | 2 (1) | F(3,97) = .61 | .61 |
| Days of LBP-related time off (SD) | 12 (26) | 5 (10) | 7 (10) | 3 (4) | F(3,97) = 1.70 | .20 |
| Baecke Habitual Activity measure (SD), 3–15 | 8 (2) | 8 (1) | 8 (1) | 8 (1) | F(3,93) = .18 | .91 |
| Fear Avoidance Beliefs Questionnaire Subscales | ||||||
| Physical Activity (SD), 0–24 | 12 (4) | 13 (7) | 13 (3) | 14 (5) | F(3,97) = 1.01 | .39 |
| Work Subscale (SD), 0–42 | 13 (8) | 13 (10) | 14 (7) | 11 (7) | F(3,87) = .491 | .69 |
| SF-36 Component Summary Scores | ||||||
| Physical (SD), 0–100% | 46 (8) | 48 (6) | 43 (8) | 47 (7) | F(3,97) = 2.27 | .09 |
| Mental (SD), 0–100% | 56 (6) | 53 (8) | 55 (8) | 54 (7) | F(3,97) = .68 | .56 |
| Satisfaction with care (SD), 15–75de | 67 (5) | 63 (8) | 62 (8) | 63 (8) | F(3,87) = 3.26 | .03 |
Boldface indicates a significant difference between groups.
Low back pain classification subgroups within each treatment condition (Classification-Specific and Non Classification-Specific). Two participants classified as Flex-Rot are not included in sample because there were not enough people to include in the analyses.
Classification-Specific.
Non Classification-Specific.
Higher score indicates more satisfaction with care.
Measured at the end of the 6 week treatment phase.
Adherence
The self-reported estimates of average adherence obtained during clinic visits were very consistent with the participants’ daily logs. The correlations between the mean values of daily reported adherence and the participant’s ‘average’ estimate were .96 and .94 for performance training adherence and exercise adherence, respectively. The mean values were likewise very similar: (performance training adherence: daily: 79±15%; average: 78±15%, t=2.26, df= 92, p=.03; exercise adherence: daily: 79±17%; average: 79±16%, t= 0.58, df= 92, p=.56).
Treatment Effects
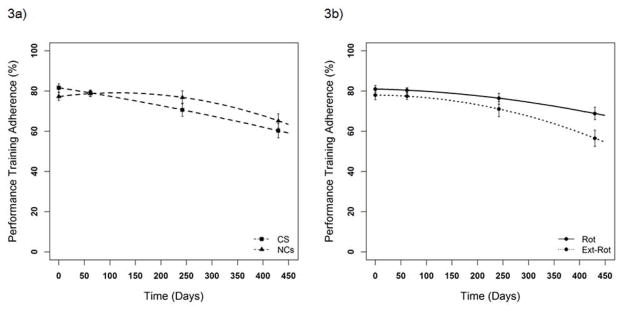
mODI-related analyses (Table 3). The tests of the grand means indicated significant overall curvilinearity and significant overall linear effects at each of the 3 time points (ps<.05; Fig. 2a). The effects were a result of mODI scores improving at post-treatment (significant negative linear slopes for all 4 groups), plateauing at 6 months (linear slopes no longer significant for 3 of the groups and much less negative for the remaining group), and regressing at 12 months (positive slopes for all groups; significantly so for 3 of the groups). The specific group comparisons (group parameter comparisons indicated by superscripts in Tables) indicated that there were no significant treatment group differences, but there were 2 classification group differences in the slopes (ps<.05; Fig. 2b). At 6 months the ExtRot group was plateauing whereas the Rot group was still improving (ExtRot: mean β=−.012; Rot: mean β=−.152, p<.05), and at 12 months the ExtRot group was regressing more rapidly than the Rot group (ExtRot: mean β=.814; Rot: mean β=.376, p<.05). Thus, compared to the Rot group, the pattern of plateauing and regressing was occurring earlier for the ExtRot group. Adherence-related analyses (Table 4 and 5). Performance training adherence declined less (~ 79% to 62%) than exercise adherence (~ 80% to 40%). Performance training. The test of the grand mean for overall curvilinearity was significant (p<.05). The effect was the result of no change in performance training adherence at post-treatment (non-significant overall linear effect, p>.05), followed by decreasing adherence at 6 and 12 months (significant negative overall linear effects, ps<.05). There were 3 significant group differences (ps<.05). At post-treatment, performance training adherence was decreasing for the CS group (negative linear effect: mean β=−0.420) but increasing slightly for the NCs group (positive linear effect: mean β=0.160, p<.05; Fig. 3a). At 12 months, performance training adherence was decreasing at a faster rate for the ExtRot group than for the Rot group (negative linear effect: ExtRot: mean β=−1.003, Rot: mean β=−0.495, p<.05). At 6 months, the ExtRot group had a lower expected adherence score (intercept value) than the Rot group (ExtRot: mean β=71%; Rot: mean β=76%, p<.05; Fig. 3b). Exercise. The tests of the grand means indicated significant overall curvilinearity and significant linear effects at each of the 3 time points (ps<.05; Fig. 4). Exercise adherence began to decline immediately in the treatment phase and the decline was significant at each follow-up. The decrease in adherence, however, lessened over time (post-treatment, mean β=−1.382; 6 months, mean β=−0.919; 12 months, mean β=−0.434). There were no significant treatment or classification group differences (ps>.05). Taken together, the results indicate that participants in both treatment groups adhered more, and longer, to the performance training than to exercise. Moderating effects. Because treatment effects are dependent on adherence[39] we examined the relationship between adherence and mODI scores by including adherence as a Level 1 predictor. When each adherence measure was analyzed separately, both exercise adherence (β=−.042) and performance training adherence (β=−.091) were related to mODI scores significantly (ps<.05) and independently of time-based changes in mODI. The more a participant adhered, the greater the improvement in mODI scores. When both forms of adherence were considered together in the same model, however, only the effect of performance training adherence on mODI scores was significant (β=−.082, p<.05). Exercise adherence did not have a significant relationship (β=−.020, p>.05) with mODI scores separate from performance training adherence. There were no significant treatment group, classification group, or treatment × classification group interaction effects on the relationship of mODI scores and adherence (ps>.05). Additional analyses indicated that, independent of time-based changes, the two forms of adherence shared only 10% of their variance, indicating relative independence. Also, when individual-level adherence averages were created, the two forms of adherence correlated .47, also suggesting that the two forms of adherence are relatively unique.
TABLE 4.
Results of Hierarchical Linear Modeling Analyses of the Performance Training Adherence Scores over Time and Specific Contrasts of Treatment Group and Classification Group at Post-Treatment and 6 and 12 Month Follow-up
| Post-Treatment | |||||
|---|---|---|---|---|---|
| Fixed Effect | Beta Coefficient | SE | t-ratio | df | p-value |
| Level 1 Intercept | |||||
| CS Rot | 79.561 | 2.789 | 28.522 | 90 | <0.001 |
| CS ExtRot | 78.423 | 3.495 | 22.439 | 90 | <0.001 |
| NCs Rot | 81.042 | 2.829 | 28.650 | 90 | <0.001 |
| NCs ExtRot | 76.261 | 3.056 | 24.954 | 90 | <0.001 |
| Level 1 Lineara | |||||
| CS Rot | −0.288 | 0.221 | −1.306 | 90 | 0.195 |
| CS ExtRot | −0.553 | 0.460 | −1.202 | 90 | 0.233 |
| NCs Rot | 0.042 | 0.155 | 0.270 | 90 | 0.788 |
| NCs ExtRot | 0.277 | 0.238 | 1.164 | 90 | 0.247 |
| Level 1 Quadraticd | |||||
| CS Rot | −0.004 | 0.006 | −0.651 | 410 | 0.515 |
| CS ExtRot | −0.001 | 0.011 | −0.116 | 410 | 0.908 |
| NCs Rot | −0.006 | 0.004 | −1.539 | 410 | 0.125 |
| NCs ExtRot | −0.022 | 0.007 | −3.162 | 410 | 0.002 |
| 6 Month | |||||
|---|---|---|---|---|---|
| Fixed Effect | Beta Coefficient | SE | t-ratio | df | p-value |
| Level 1 Interceptb | |||||
| CS Rot | 73.218 | 4.179 | 17.520 | 90 | <0.001 |
| CS ExtRot | 68.065 | 7.062 | 9.638 | 90 | <0.001 |
| NCs Rot | 79.699 | 3.355 | 23.753 | 90 | <0.001 |
| NCs ExtRot | 74.075 | 3.252 | 22.775 | 90 | <0.001 |
| Level 1 Lineard | |||||
| CS Rot | −0.418 | 0.124 | −3.362 | 90 | 0.001 |
| CS ExtRot | −0.600 | 0.151 | −3.985 | 90 | <0.001 |
| NCs Rot | −0.191 | 0.101 | −1.892 | 90 | 0.062 |
| NCs ExtRot | −0.520 | 0.115 | −4.506 | 90 | <0.001 |
| Level 1 Quadraticd | |||||
| CS Rot | −0.004 | 0.006 | −0.651 | 410 | 0.515 |
| CS ExtRot | −0.001 | 0.011 | −0.116 | 410 | 0.908 |
| NCs Rot | −0.006 | 0.004 | −1.539 | 410 | 0.125 |
| NCs ExtRot | −0.022 | 0.007 | −3.162 | 410 | 0.002 |
| 12 Month | |||||
|---|---|---|---|---|---|
| Fixed Effect | Beta Coefficient | SE | t-ratio | df | p-value |
| Level 1 Intercept | |||||
| CS Rot | 64.056 | 5.625 | 11.387 | 90 | <0.001 |
| CS ExtRot | 56.297 | 7.420 | 7.587 | 90 | <0.001 |
| NCs Rot | 73.781 | 4.303 | 17.148 | 90 | <0.001 |
| NCs ExtRot | 56.380 | 5.107 | 11.039 | 90 | <0.001 |
| Level 1 Linearb,d | |||||
| CS Rot | −0.554 | 0.256 | −2.161 | 90 | 0.033 |
| CS ExtRot | −0.649 | 0.412 | −1.573 | 90 | 0.119 |
| NCs Rot | −0.436 | 0.212 | −2.054 | 90 | 0.043 |
| NCs ExtRot | −1.357 | 0.323 | −4.195 | 90 | <0.001 |
| Level 1 Quadraticd | |||||
| CS Rot | −0.004 | 0.006 | −0.652 | 410 | 0.515 |
| CS ExtRot | −0.001 | 0.011 | −0.116 | 410 | 0.908 |
| NCs Rot | −0.006 | 0.004 | −1.539 | 410 | 0.124 |
| NCs ExtRot | −0.022 | 0.007 | −3.162 | 410 | 0.002 |
CS Rot = Classification-Specific, Rotation, CS ExtRot = Classification-Specific, Extension-Rotation, NCs Rot = Non Classification-Specific, Rotation, NCs ExtRot = Non Classification-Specific, Extension-Rotation.
Superscripts indicate the results of tests of Level 2 effects.
Treatment Group Effect: (CS Rot + CS ExtRot) vs. (NCs Rot + NCs ExtRot), p<.05.
Classification Group Effect: (CS Rot + NCs Rot) vs. (CS ExtRot + NCs ExtRot), p<.05.
Treatment × Classification Group Interaction: (CS Rot + NCs ExtRot) vs. (CS ExtRot + NCs Rot), p<.05.
Grand Mean, p<.05. (Tested for the linear and quadratic component)
Figure 3.
Figure 3a. Predicted values and 95% confidence intervals based on hierarchical linear modeling analyses of the adherence to performance training for the classification-specific (CS) group and the non-classification-specific (NCs) group at the 2nd treatment visit, post-treatment, and 6 and 12 months later. Overall, both treatment groups showed no change in adherence at post-treatment (non-significant overall linear effect, i.e., slope; p>.05), and decreasing adherence at 6 and 12 months (significant negative overall linear effects, i.e., slopes; ps<.05). There was no treatment group difference (p>.05).
Figure 3b. Predicted values and 95% confidence intervals based on hierarchical linear modeling analyses of the adherence to performance training for the rotation (Rot) group and the extension-rotation (ExtRot) group at the 2nd treatment visit, post-treatment, and 6 and 12 months later. At 6 months the Rot group was adhering more than the ExtRot group (significant classification group difference in intercepts, i.e., predicted score; p<.05). At 12 months adherence was decreasing at a faster rate for the ExtRot group than for the Rot group (significant classification group effect for linear components, i.e., slopes; p<.05).
Secondary Outcomes
Three patterns of results emerged from the HLM analysis for each secondary outcome (Supplemental Digital File 2). For Pattern 1, the outcome improved at post-treatment, plateaued at 6 months, and regressed to varying degrees at 12 months; relevant outcomes were the numeric pain ratings and the FABQ work subscale. For Pattern 2, the outcome improved over time; relevant outcomes were medication use, LBP-related time off, and the SF-36 physical component summary. For Pattern 3, the outcome changed minimally over time; relevant outcomes were the Baecke activity questionnaire, the FABQ physical activity subscale, and the SF-36 mental component summary.
Additional Exploratory Analyses
The individual-level adherence averages referred to previously also were explored as individual moderators of outcomes and as moderators in combination with treatment and classification groups. These analyses, using analysis-wide protection of the Type I error rate, produced no consistent results and are not reported further.
Adverse Events
No serious adverse events were reported. The one non-serious, treatment-related, adverse event was a worsening of LBP with exercise for one of the NCs participants. The 4 other non-serious adverse events included 2 bouts of influenza, 1 increase in stress, and 1 injury unrelated to LBP.
DISCUSSION
Although there were no differences in function between the two treatment groups (CS vs. NCs) people in both groups displayed a clinically meaningful improvement in LBP-related function during the treatment phase, and at 6 and 12 months despite a slight regression in the final 6 months (Fig. 2a).[76, 77] There was a difference in function between the two LBP classification groups. Compared to the ExtRot group, the Rot group was improving at a faster rate at 6 months and regressing at a slower rate at 12 months (Fig. 2b). Adherence to exercise differed from adherence to performance training. In both treatment groups, exercise adherence declined more and faster than performance training adherence. In addition, compared to the ExtRot group, adherence to performance training for the Rot group was (1) higher at 6 months, and (2) declining at a slower rate at 12 months; these effects parallel the differential effects of classification group on function. Thus, the group that adhered more to performance training at 6 and 12 months also had better function at those time points. Finally, adherence to performance training had a unique, independent effect on function that was above and beyond the effect of exercise adherence; specifically, the more a person adhered to performance training the more the mODI scores improved and vice versa. The relationship between mODI scores and performance training adherence was the same irrespective of a participant’s treatment or classification group assignment. These findings are important because people with chronic LBP not only benefited from practicing precise performance of everyday activities, but they also did it more and longer than they did the exercises.
Our study is the first to examine the differential effect of a CS treatment based on the MSI classification system for LBP and a generic, NCs treatment. We did not find the differences we hypothesized between the 2 groups. The unexpected similarity in outcomes for the 2 treatment groups may have been related to unanticipated similarities in performance training. For both groups decreasing the amount of lumbar spine movement and avoiding end-range positioning of the lumbar spine[78] was emphasized. The differences were that people in the CS group were told (1) the specific direction(s) of lumbar spine movement or alignment to modify, and (2) to modify performance of individual activities to decrease symptoms. The likelihood that the similarity in performance training across groups confounded our results is increased given the differential levels of adherence; for both treatment groups levels of adherence to performance training were relatively high, but levels of exercise adherence dropped sharply across time. Thus, participants adhered most to the aspects of treatment that were similar across groups and adhered least to those that were dissimilar.
In a study of people with chronic LBP Henry et al[79] examined the effects of treatments that were either matched or unmatched to a person’s LBP category. First, each participant was classified as “stabilization eligible or ineligible” based on the Treatment-Based Classification (TBC) System criteria and then everyone in each TBC group also was classified into an MSI LBP subgroup.[27, 80, 81] People in 3 of the 4 groups received matched treatment as follows: (1) people classified as TBC-stabilization eligible received the TBC stabilization treatment, (2) people classified as TBC-stabilization eligible were treated based on their MSI classification, and (3) people classified as TBC-stabilization ineligible were treated based on their MSI classification. The unmatched group received the TBC stabilization treatment. The authors reported that (1) both the matched and the unmatched treatment groups improved, and (2) there were no differences in outcomes between the 2 groups either immediately or 12 months after treatment. Given the complexity of the study’s design, we assume the authors intended to test the differential effects of treatment matched to each system, TBC and MSI, but they were unable to do so because of inadequate statistical power. Thus, the results are confounded and the specific effect on outcomes of matching treatment to an MSI category cannot be inferred based on the Henry study. Furthermore, all of the matched treatments appear to have been focused on the same goal of improving control of trunk movement and posture so it is unclear why differences would be expected. By contrast, we compared exercise for control of trunk movement and posture based on a participant’s MSI classification to exercise for strength and flexibility. Based on post-hoc examination of the treatment protocols, however, we discovered that people in both groups received instructions for performance training that both emphasized reducing the amount of lumbar spine movement and avoiding end-range positioning of the lumbar spine during activities, which may account for attenuated differences between groups. Finally, although adherence to treatment was measured in the Henry study, no data was reported for (1) levels of adherence across the study period, (2) adherence to exercise versus performance training, or (3) the moderating effect of adherence on outcomes. Consequently, it is not clear if the lack of differences in outcomes between the matched and unmatched treatments were the result of differences in adherence between the two treatment conditions.
Recall bias is an intentional or unintentional differential recall of past events or experiences. The difference in amount and rate of decline between the two types of adherence could be a result of differential recall. The repetitive nature of performing everyday functional activities could have made performance training more salient to the participants than exercise. The result would be reports of higher and more long-lasting adherence to performance training. On the other hand, the repetitive nature of everyday functional activities suggests that participants would have had multiple opportunities to practice performance across the day. Given such circumstances, the participants would be adhering more to the performance training than to the exercise. Thus, a potential advantage of performance training as a component of treatment is that the participant can achieve a high dose, having the potential to contribute more to improvement in outcomes than exercise.
To our knowledge, this is the first study to examine the effects of adherence to separate components of treatment, exercise versus performance training. Separate measures allowed us to examine which component people adhered to the most, and the potential impact of each type of adherence. Only performance training adherence had a unique, independent effect on modified Oswestry scores. The critical importance of this unique effect is evident in the comparisons between the Rot and ExtRot groups, wherein, differential changes in mODI scores paralleled the differences in performance training adherence over time (Fig. 2b and 3b). In addition, at the individual level the relationship between performance training and exercise is small, with less than 10% of shared variance between the two types of adherence. Thus, the two adherence measures are capturing relatively unique behaviors.
Although we examined all people with LBP that met our inclusion criteria, the sample primarily consisted of people classified as Rot or ExtRot (Table 6). There were two people classified as FlexRot. The small number, however, prohibited including the FlexRot cases in the analyses. The distribution of classifications is not atypical of other studies that classified people using the MSI system.[28, 32, 33, 79] The narrow distribution of LBP classifications may be because the focus of studies has been on people with chronic LBP that were not acutely involved. Generalizability of our findings, therefore, is limited to the LBP classifications studied.
One limitation is that therapists administered explicitly defined treatments that may not be used typically. All therapists also used a defined set of criteria for progression.[45] The effects obtained, however, indicate that use of defined treatments and specific criteria for progression for any treatment protocol may be important for attaining a consistent and long-lasting improvement in outcomes. A second limitation is the sample included people who were not in an acute flare-up, had moderate levels of functional limitation and pain, and did not report elevated levels of fear avoidance behavior (Table 6). Thus, we do not know the generalizability of the findings to people with (1) specific pathoanatomical conditions, (2) more severe LBP or functional limitation, or (3) substantial behavioral and psychological co-morbidities.[44] A third limitation is that we did not include a no-treatment group. Thus, we cannot exclude the possibility that a no-treatment group would have had similar outcomes as obtained in the 2 treatment conditions provided.
CONCLUSIONS
There were no differences in function between the two treatment groups (CS and NCs). In both treatment groups people with chronic LBP displayed clinically important long-term improvements in function, and the improvements were uniquely related to performance training. These findings suggest that attention should be given to training people with chronic LBP to modify how they perform everyday functional activities by avoiding extremes of lumbar spine posture and reducing the amount of lumbar spine movement used while increasing use of other joints to accomplish tasks. Attention to performance training is particularly key because (1) people adhere to the training for prolonged periods of time, and (2) the training results in improved short-term, but more importantly, long-term outcomes. Such an outcome is important for a condition often characterized by an extended clinical course of fluctuating functional limitations and persistent or recurrent symptoms.
Supplementary Material
Highlights.
Outcomes were similar for the two treatment groups
Both treatments included exercise and performance training to modify functional activities
Both groups adhered more to performance training than to exercise
Adherence to performance training had a unique and independent effect on outcomes above and beyond adherence to exercise
Acknowledgments
The authors wish to acknowledge Kate Baxter and Dr. Shannon Hoffman for assistance with participant recruitment, data collection, and data analysis. We also would like to thank Sara Bohall and Kristen Roles for assistance with formatting of figures and tables and Jennifer Jarvis and Sara Bohall for overall formatting of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Frymoyer JW. Back pain and sciatica. New England Journal of Medicine. 1988;318(5):291–300. doi: 10.1056/NEJM198802043180506. [DOI] [PubMed] [Google Scholar]
- 2.Papageorgiou AC, Croft PR, Thomas E, Ferry S, Jayson MI, Silman AJ. Influence of previous pain experience on the episode incidence of low back pain: results from the South Manchester Back Pain Study. Pain. 1996;66(2–3):181–5. doi: 10.1016/0304-3959(96)03022-9. [DOI] [PubMed] [Google Scholar]
- 3.Wahlgren DR, Atkinson JH, Epping-Jordan JE, et al. One-year follow-up of first onset low back pain. Pain. 1997;73(2):213–21. doi: 10.1016/S0304-3959(97)00106-1. [DOI] [PubMed] [Google Scholar]
- 4.Croft PR, Macfarlane GJ, Papageorgiou AC, Thomas E, Silman AJ. Outcome of low back pain in general practice: a prospective study. British Medical Journal. 1998;316(7141):1356–9. doi: 10.1136/bmj.316.7141.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pizzo PA, Clark NM. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 6.Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sinnott P, Wagner TH. Low back pain in VA users. Archives of Internal Medicine. 2009;169(14):1338–9. doi: 10.1001/archinternmed.2009.201. [DOI] [PubMed] [Google Scholar]
- 8.Hestbaek L, Leboeuf-Yde C, Kyvik KO, Manniche C. The course of low back pain from adolescence to adulthood: eight-year follow-up of 9600 twins. Spine. 2006;31(4):468–72. doi: 10.1097/01.brs.0000199958.04073.d9. [DOI] [PubMed] [Google Scholar]
- 9.Von Korff M. Studying the natural history of back pain. Spine. 1994;19(18 Suppl):2041S–6S. doi: 10.1097/00007632-199409151-00005. [DOI] [PubMed] [Google Scholar]
- 10.Hestbaek L, Leboeuf-Yde C, Manniche C. Low back pain: what is the long-term course? A review of studies of general patient populations. European Spine Journal. 2003;12(2):149–65. doi: 10.1007/s00586-002-0508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hestbaek L, Leboeuf-Yde C, Manniche C. Is low back pain part of a general health pattern or is it a separate and distinctive entity? A critical literature review of comorbidity with low back pain. Journal of Manipulative and Physiological Therapeutics. 2003;26(4):243–52. doi: 10.1016/s0161-4754(03)00003-4. [DOI] [PubMed] [Google Scholar]
- 12.Van Middelkoop M, Rubinstein SM, Kuijpers T, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. European Spine Journal. 2011;20(1):19–39. doi: 10.1007/s00586-010-1518-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Middelkoop M, Rubinstein SM, Verhagen AP, Ostelo RW, Koes BW, van Tulder MW. Exercise therapy for chronic nonspecific low-back pain. Best Practice and Research in Clinical Rheumatology. 2010;24:193–204. doi: 10.1016/j.berh.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 14.van Tulder M, Malmivaara A, Esmail R, Koes B. Exercise therapy for low back pain: a systematic review within the framework of the Cochrane collaboration back review group. Spine. 2000;25(21):2784–96. doi: 10.1097/00007632-200011010-00011. [DOI] [PubMed] [Google Scholar]
- 15.Hayden JA, van Tulder MW, Malmivaara A, Koes BW. Meta Analysis: Exercise therapy for treatment of non-specific low back pain. Annals of Internal Medicine. 2005;142(9):765–75. doi: 10.7326/0003-4819-142-9-200505030-00013. [DOI] [PubMed] [Google Scholar]
- 16.Hayden JA, van Tulder M, Tomlinson G. Systematic review: Strategies for using exercise therapy to improve outcomes in chronic low back pain. Annals of Internal Medicine. 2005;142(9):776–85. doi: 10.7326/0003-4819-142-9-200505030-00014. [DOI] [PubMed] [Google Scholar]
- 17.Rackwitz B, de Bie R, Limm H, von Garnier K, Ewert T, Stucki G. Segmental stabilizing exercises and low back pain. What is the evidence? A systematic review of randomized controlled trials. Clinical Rehabilitation. 2006;20(7):553–67. doi: 10.1191/0269215506cr977oa. [DOI] [PubMed] [Google Scholar]
- 18.Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Annals of Internal Medicine. 2007;147(7):478–91. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 19.Macedo LG, Maher CG, Latimer J, McAuley JH. Motor control exercise for persistent, nonspecific low back pain: a systematic review. Physical Therapy. 2009;89(1):9–25. doi: 10.2522/ptj.20080103. [DOI] [PubMed] [Google Scholar]
- 20.Spitzer WO, LeBlanc FE, Dupuis M. Scientific approach to the assessment and management of activity related spinal disorders: A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine. 1987;12(7 Suppl):S1–S59. [PubMed] [Google Scholar]
- 21.Borkan JM, Cherkin DC. An agenda for primary care research on low back pain. Spine. 1996;21(24):2880–4. doi: 10.1097/00007632-199612150-00019. [DOI] [PubMed] [Google Scholar]
- 22.Croft P, Papageorgiou A, McNally R. Health Care Needs Assessment. New York, NY: Radcliffe Medical Press Oxford; 1997. Low back pain; pp. 129–82. [Google Scholar]
- 23.Bouter LM, Pennick V, Bombardier C. Cochrane back review group. Spine. 2003;28(12):1215–8. doi: 10.1097/01.BRS.0000065493.26069.1C. [DOI] [PubMed] [Google Scholar]
- 24.Jordan JL, Holden MA, Mason EE, Foster NE. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Systematic Review. 2010;(1):CD005956. doi: 10.1002/14651858.CD005956.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dimatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Medical Care. 2002;40(9):794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Spitzer WO, et al. Chapter 3: Diagnosis of the problem (the problem of diagnosis) Spine. 1987;12(7 Supplement):S16–S20. [Google Scholar]
- 27.Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. 1. St. Louis, MO: Mosby, Inc; 2002. Movement impairment syndromes of the lumbar spine; pp. 51–118. [Google Scholar]
- 28.Van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, McDonnell MK, Bloom NJ. Movement system impairment-based categories for low back pain: stage 1 validation. Journal of Orthopaedic and Sports Physical Therapy. 2003;33(3):126–42. doi: 10.2519/jospt.2003.33.3.126. [DOI] [PubMed] [Google Scholar]
- 29.Van Dillen LR, Sahrmann SA, Norton BJ, et al. Reliability of physical examination items used for classification of patients with low back pain. Physical Therapy. 1998;78(9):979–88. doi: 10.1093/ptj/78.9.979. [DOI] [PubMed] [Google Scholar]
- 30.Van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, McDonnell MK, Bloom N. The effect of modifying patient-preferred spinal movement and alignment during symptom testing in patients with low back pain: a preliminary report. Arch Phys Med Rehabil. 2003;84(3):313–22. doi: 10.1053/apmr.2003.50010. [DOI] [PubMed] [Google Scholar]
- 31.Van Dillen LR, Maluf KS, Sahrmann SA. Further examination of modifying patient-preferred movement and alignment strategies in patients with low back pain during symptomatic tests. Manual Therapy. 2009;14(1):52–60. doi: 10.1016/j.math.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Trudelle-Jackson E, Sarvaiya-Shah SA, Wang SS. Interrater reliability of a movement impairment-based classification system for lumbar spine syndromes in patients with chronic low back pain. Journal of Orthopaedic and Sports Physical Therapy. 2008;38(6):371–6. doi: 10.2519/jospt.2008.2760. [DOI] [PubMed] [Google Scholar]
- 33.Harris-Hayes M, Van Dillen LR. Inter-tester reliability of physical therapists classifying low back pain problems based on the movement system impairment classification system. Physical Medicine and Rehabilitation. 2009;1(2):117–26. doi: 10.1016/j.pmrj.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Henry SM, Van Dillen LR, Trombley AL, Dee JM, Bunn JY. Reliability of novice raters in using the movement system impairment approach to subgroup people with low back pain. Manual Therapy. 2013;18(1):31–40. doi: 10.1016/j.math.2012.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Norton BJ, Sahrmann SA, Van Dillen LR. Differences in measurements of lumbar curvature related to gender and low back pain. Journal of Orthopaedic and Sports Physical Therapy. 2004;34(9):524–34. doi: 10.2519/jospt.2004.34.9.524. [DOI] [PubMed] [Google Scholar]
- 36.Kim MH, Yoo WG, Choi BR. Differences between two subgroups of low back pain patients in lumbopelvic rotation and symmetry in the erector spinae and hamstring muscles during trunk flexion when standing. J Electromyogr Kinesiol. 2013;23(2):387–93. doi: 10.1016/j.jelekin.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 37.Gombatto SP, Collins DR, Engsberg JR, Sahrmann SA, Van Dillen LR. Patterns of lumbar region movement during trunk lateral bending in two different subgroups of people with low back pain. Physical Therapy. 2007;87(4):441–54. doi: 10.2522/ptj.20050370. [DOI] [PubMed] [Google Scholar]
- 38.Van Dillen LR, Gombatto SP, Collins DR, Engsberg JR, Sahrmann SA. Symmetry of timing of hip and lumbopelvic rotation motion in 2 different subgroups of people with low back pain. Archives of Physical Medicine and Rehabilitation. 2007;88(3):351–60. doi: 10.1016/j.apmr.2006.12.021. [DOI] [PubMed] [Google Scholar]
- 39.World Health Organization. Adherence to Long-Term Therapies: Evidence for action. Switzerland: 2003. [Google Scholar]
- 40.Liddle SD, Baxter GD, Gracey JH. Exercise and chronic low back pain: What works? Pain. 2004;107(1–2):176–90. doi: 10.1016/j.pain.2003.10.017. [DOI] [PubMed] [Google Scholar]
- 41.Liddle SD, David BG, Gracey JH. Physiotherapists’ use of advice and exercise for the management of chronic low back pain: A national survey. Manual Therapy. 2008;14(2):189–96. doi: 10.1016/j.math.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 42.Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? J Am Med Assoc. 1992;268(6):760–5. [PubMed] [Google Scholar]
- 43.van der Windt DAWM, Simons E, Riphagen II, et al. Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain. Cochrane Database of Systematic Reviews. 2010;(2):1–83. doi: 10.1002/14651858.CD007431.pub2. Art. No.: CD007431. [DOI] [PubMed] [Google Scholar]
- 44.Waddell G, McCulloch JA, Kummel E, Venner RM. Nonorganic physical signs in low-back pain. Spine. 1980;5(2):117–25. doi: 10.1097/00007632-198003000-00005. [DOI] [PubMed] [Google Scholar]
- 45.Harris-Hayes M, Holtzman GW, Early J, Van Dillen LR. Development and preliminary reliability testing of physical therapists to assess a patient’s independence in performing a treatment program: Standardized patient scenarios. Journal of Rehabilitation Medicine. 2010;42(3):221–7. doi: 10.2340/16501977-0505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Franklin BA, Whaley MH, Howley ET, et al. Section III: Exercise Prescription. In: Johnson EP, Napora LS, editors. ACSM’s Guidelines for Exercise Testing and Prescription. 6. Baltimore, MD: Lippincott Williams & Wilkins; 2000. pp. 137–234. [Google Scholar]
- 47.Taimela S, Diederich C, Hubsch M, Heinricy M. The role of physical exercise and inactivity in pain recurrence and absenteeism from work after active outpatient rehabilitation for recurrent or chronic low back pain: a follow-up study. Spine. 2000;25(14):1809–16. doi: 10.1097/00007632-200007150-00012. [DOI] [PubMed] [Google Scholar]
- 48.Friedrich M, Cermak T, Maderbacher P. The effect of brochure use versus therapist teaching on patients performing therapeutic exercise and on changes in impairment status. Physical Therapy. 1996;76(10):1082–8. doi: 10.1093/ptj/76.10.1082. [DOI] [PubMed] [Google Scholar]
- 49.Friedrich M, Gittler G, Halberstadt Y, Cermak T, Heiller I. Combined exercise and motivation program: effect on the compliance and level of disability of patients with chronic low back pain: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 1998;79(5):475–87. doi: 10.1016/s0003-9993(98)90059-4. [DOI] [PubMed] [Google Scholar]
- 50.Mannion AF, Muntener M, Taimela S, Dvorak J. A randomized clinical trial of three active therapies for chronic low back pain. Spine. 1999;24(23):2435–8. doi: 10.1097/00007632-199912010-00004. [DOI] [PubMed] [Google Scholar]
- 51.Moffett JK, Torgerson D, Bell-Syer S, et al. Randomized controlled trial of exercise for low back pain: clinical outcomes, costs, and preferences. British Medical Journal. 1999;319(7205):279–83. doi: 10.1136/bmj.319.7205.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moseley GL, Nicholas MK, Hodges PW. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clinical Journal of Pain. 2004;20(5):324–30. doi: 10.1097/00002508-200409000-00007. [DOI] [PubMed] [Google Scholar]
- 53.Hansen FR, Bendix T, Skov P, et al. Intensive, dynamic back-muscle exercises, conventional physiotherapy, or placebo-control treatment of low-back pain. A randomized, observer-blind trial. Spine. 1993;18(1):98–108. doi: 10.1097/00007632-199301000-00015. [DOI] [PubMed] [Google Scholar]
- 54.Melnik M, Saunders HD, Saunders R. Managing Back Pain. Chaska, MN: The Saunders Group Incorporated; 1998. pp. 1–31. [Google Scholar]
- 55.Fritz JM, Irrgang JJ. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Physical Therapy. 2001;81(2):776–88. doi: 10.1093/ptj/81.2.776. [DOI] [PubMed] [Google Scholar]
- 56.Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58(3):387–92. doi: 10.1016/0304-3959(94)90133-3. [DOI] [PubMed] [Google Scholar]
- 57.Von Korff M. Epidemiologic and survey methods: chronic pain assessment. In: Turk D, Melzack R, editors. Handbook of Pain Assessment. 2. New York, NY: Guildford Press; 2001. pp. 603–18. [Google Scholar]
- 58.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. American Journal of Clinical Nutrition. 1982;36(5):936–42. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 59.Ono R, Hirata S, Yamada M, Nishiyama T, Kurosaka M, Tamura Y. Reliability and validity of the Baecke physical activity questionnaire in adult women with hip disorders. BMC Musculoskeletal Disorders. 2007;8:61. doi: 10.1186/1471-2474-8-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lethem J, Slade PD, Troup JD, Bentley G. Outline of a Fear-Avoidance Model of exaggerated pain perception--I. Behaviour Research and Therapy. 1983;21(4):401–8. doi: 10.1016/0005-7967(83)90009-8. [DOI] [PubMed] [Google Scholar]
- 61.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–68. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 62.Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. Journal of Behavioral Medicine. 2007;30(1):77–94. doi: 10.1007/s10865-006-9085-0. [DOI] [PubMed] [Google Scholar]
- 63.Jacob T, Baras M, Zeev A, Epstein L. Low back pain: reliability of a set of pain measurement tools. Archives of Physical Medicine and Rehabilitation. 2001;82(6):735–42. doi: 10.1053/apmr.2001.22623. [DOI] [PubMed] [Google Scholar]
- 64.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30(6):473–83. [PubMed] [Google Scholar]
- 65.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care. 1993;31(3):247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 66.Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB. Assessing health-related quality of life in patients with sciatica. Spine. 1995;20(17):1899–908. doi: 10.1097/00007632-199509000-00011. [DOI] [PubMed] [Google Scholar]
- 67.Cherkin D, Deyo RA, Berg AO. Evaluation of a physician education intervention to improve primary care for low-back pain. II. Impact on patients. Spine. 1991;16(10):1173–8. doi: 10.1097/00007632-199110000-00008. [DOI] [PubMed] [Google Scholar]
- 68.O’Sullivan PB, Phyty GD, Twomey LT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine. 1997;22(24):2959–67. doi: 10.1097/00007632-199712150-00020. [DOI] [PubMed] [Google Scholar]
- 69.Torstensen TA, Ljunggren AE, Meen HD, Odland E, Mowinckel P, Geijerstam S. Efficiency and costs of medical exercise therapy, conventional physiotherapy, and self-exercise in patients with chronic low back pain. A pragmatic, randomized, single-blinded, controlled trial with 1-year follow-up. Spine. 1998;23(23):2616–24. doi: 10.1097/00007632-199812010-00017. [DOI] [PubMed] [Google Scholar]
- 70.Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 71.Heck RH, Thomas SL. An Introduction to Multilevel Modeling Techniques. 2. New York, NY: Routledge; 2009. [Google Scholar]
- 72.Hox JJ. Multilevel Analysis: Techniques and Applications. 2. New York, NY: Routledge Academic; 2010. [Google Scholar]
- 73.Snijders T, Bosker R. Multilevel Analysis: An Introduction to Basic and Advanced multilevel Modeling. 2. Thousand Oaks, CA: Sage Publications; 2012. [Google Scholar]
- 74.Allison PD. Statistical Horizons. Vol. 312. Haverford, PA, USA, SAS global forum: 2012. Handling Missing Data by Maximum Likelihood. [Google Scholar]
- 75.Dziura JD, Post LA, Zhao Q, Fu Z, Peduzzi P. Strategies for dealing with missing data in clinical trials: from design to analysis. Yale J Biol Med. 2013;86(3):343–58. [PMC free article] [PubMed] [Google Scholar]
- 76.Beurskens AJ, de Vet HC, Koke AJ. Responsiveness of functional status in low back pain: a comparison of different instruments. Pain. 1996;65(1):71–6. doi: 10.1016/0304-3959(95)00149-2. [DOI] [PubMed] [Google Scholar]
- 77.Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976 ) 2008;33(1):90–4. doi: 10.1097/BRS.0b013e31815e3a10. [DOI] [PubMed] [Google Scholar]
- 78.McGill S. Ultimate back fitness and performance. Waterloo, Ontario: Wabuno Publishers; 2004. [Google Scholar]
- 79.Henry SM, Van Dillen LR, Ouellette-Morton RH, et al. Outcomes are not different for patient-matched versus nonmatched treatment in subjects with chronic recurrent low back pain: a randomized clinical trial. Spine Journal. 2014 doi: 10.1016/j.spinee.2014.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. Journal of Orthopaedic and Sports Physical Therapy. 2007;37(6):290–302. doi: 10.2519/jospt.2007.2498. [DOI] [PubMed] [Google Scholar]
- 81.Stanton TR, Fritz JM, Hancock MJ, et al. Evaluation of a treatment-based classification algorithm for low back pain: a cross-sectional study. Physical Therapy. 2011;91(4):496–509. doi: 10.2522/ptj.20100272. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.