Abstract
Background
Atypical squamous cells of undetermined significance (ASCUS) is the term in cervical cytology reporting where the changes are suggestive of a sqamous extraepithelial lesion but lack criteria for definition interpretation. Its clinical significance is variable.
Methods
A one year study in a zonal hospital evaluating all cervical smears received for cytology by two pathologists independently and subsequently reported as per the Bethesda guidelines. The patients were folloed up for six months.
Result
A total of 24 (4%) smears were reported as ASCUS out of 604 examined. Of these, 15 were followed up for one year. Mean age was 39 years and 60% were premenopausal. After six months, 11 cases were reported negative for intraepithelial lesion or malignancy and four showed ASCUS on repeat pap smear.
Conclusion
ASCUS shows a repression rate of 73%. Colpscopic evaluation should be done only if ASCUS persists. Diligent follow up and biopsy, when indicated is a must.
Key Words: Atypical squamous cells, Squamous intraepithelial lesion, Pap smear
Introduction
Cervical cytology reporting has been plagued by a plethora of terminologies which make the process all the more confusing for the cytologist and the clinician. The Bethesda system of reporting hoped to clarify and simplify the issue by using standard terminology.
The term “atypical squamous cells” (ASC) was introduced by the 1988 Bethesda system for reporting cervical/vaginal cytologic diagnoses whose cellular abnormalities are more marked than those attributable to reactive/inflammatory cellular changes but that quantitatively or qualitatively fall short of a definitive diagnosis of a squamous intraepithelial lesion (SIL) [1]. Subsequently it was recommended to further qualify the lesions as atypical squamous cells-undetermined significance (ASCUS) where the cytologic changes are suggestive of a squamous intraepithelial lesion, but lack criteria for a definitive interpretation and atypical squamous cells- cannot exclude high grade squamous intraepithelial lesion (HSIL) where cytologic changes are suggestive of HSIL, but lack criteria for definitive interpretation.
The clinical significance of ASCUS in terms of outcome is variable. ASCUS has been said to be predictive of viral changes or dysplasia in 25–55% (the average of 12 studies was 34%) of cases and HSIL in about 5–20% of cases (average 9%), depending on the mechanism of follow-up [2, 3, 4, 5, 6, 7].
The clinical management of women with such cytological modification remains controversial. Some investigators have advocated elimination of the terminology due to over usage and low reproducibility. Inter observer variation has also been reported to be considerable [8].
Clinical data from ASCUS/low grade squamous intraepithelial lesion (LSIL) triage study (ALTS) have demonstrated that two repeat cytologic examinations performed at six-month intervals, testing for human papillomavirus (HPV) and a single colposcopic examination are all safe and effective approaches to managing women with ASCUS [9].
Material and Methods
The study was conducted over a one year period in a zonal hospital. All smears received in the cytology laboratory were evaluated by two cytopathologists independently for adequacy and subsequently examined and reported as per the guidelines of the Bethesda system. An attempt was made to keep the patients under follow up for six months.
Cervical smears were taken using the conventional Ayres spatula and wet fixed in 50% ether alcohol. Transportation to the lab was in a Coplin jar containing the fixative solution. Subsequently smears were stained using a Rapid PAP technique.
A total of 630 smears were collected of which 26 were inadequate due to insufficient squamous cellularity and obscuring inflammation/haemorrhage. Of the remaining 604 smears 327 were adequate and 277 were adequate but limited due to absence of endocervical cells. These 604 smears were evaluated for cy to logical abnormalities. Twenty three of these smears were reported as ASCUS and one was reported as ASC-H.
A follow up was performed on the 24 cases of ASC (including the one case of ASC-H) with repeat Pap smears at an interval of 4- 6 months. Cases showing ASC even on repeat smears were evaluated further with directed biopsies.
Results
The distribution of diagnoses in all the reported cervical smears (Table 1) shows that there were a total of 24 smears (4%) reported as ASCUS in the first Pap report. Each of these patients was advised a repeat Pap after 4–6 months but 9 (37.5%) were lost to follow up. The remaining 15 patients were followed up for one year.
Table 1.
Distribution of diagnoses amongst all cases
| Diagnosis | Number of cases (%) |
|---|---|
| Negative for intraepithelial lesion or malignancy | 11 (73.3) |
| ASCUS | 04 (26.6) |
| Total | 15 |
The mean age of the patients was 39 years (range 32–61 years). Nine out of the 15 (60%) patients were premenopausal. Follow up for these patients was done with repeat Pap smears rather than colposcopy due to the lack of facility and expense involved. Out of the 15 patients followed up, 11 cases were reported as negative for intraepithelial lesion or malignancy and four showed ASCUS on repeat Pap smear after 4–6 months Table 2. 73.3% of the cases thus showed regression.
Table 2.
Diagnosis on second Pap smear on IS followed up cases of ASCUS
| Diagnosis | No of cases |
|---|---|
| Negative for intraepithelial lesion or malignancy | 553 |
| ASCUS | 24 (ASCUS 23, ASC-H 1) |
| LSIL | 23 |
| HSIL | 02 |
| Invasive carcinoma | 02 |
| Total | 604 |
Directed biopsy (on aceto-white epithelium) was performed on four patients showing ASC (including the one case of ASC-H) on repeat smear. Among these cases, three showed chronic cervicitis and one case (ASC-H on first Pap smear) showed cervical intraepithelial neoplasia (CIN) -3 on histology.
Discussion
ASCUS as an entity was first described in The Bethesda System (TBS) in 1988. The poor reproducibility of ASCUS interpretations provided the foundation for recommending a simplified system of qualifiers in TBS 2001. A definition for the newly created category of atypical squamous cells (ASC) was proposed: “Cytologic changes suggestive of a squamous intraepithelial lesion that are quantitatively or qualitatively insufficient for a definitive interpretation”. Also, it was thought prudent to qualify the lesion as either ‘atypical squamous cells-undetermined significance (ASCUS)’ and ‘atypical squamous cells- cannot exclude HSIL (ASC-H) [10].
It is pertinent to remember that atypical squamous cells (ASC) is not a diagnostic entity in itself, but rather reflects the limitation in technique/limitation in interpretative ability of the cytologist. Hence it
represents a vast spectrum of cases ranging from benign reactive processes to invasive cancer.
The incidence of ASCUS in the present study was found to be 4% which is similar to studies by Williams et al [7] in 1997 and Gerber et al [11] in 2001. In the present study the patients were all followed up by repeat pap smears since colposcopy was not available within the institution. Seven out of 15 cases regressed to normal on repeat Pap smear after 4–6 months and four out of 15 cases were reported as showing inflammatory changes on repeat smears. Hence a total of 11 out of 15 (73.3%) cases showed regression. This figure is comparable to other studies [6].
Cytological criteria for the diagnosis of ASCUS included nuclear enlargement to size 2.5–3 times that of an intermediate cell with a slightly increased ratio of nuclear/cytoplasmic area, mild variation in nuclear size or contour, and slight hyperchromasia with even chromatin (Fig. 1). Cytologic changes that were suggestive of HSIL, but lacked criteria for definitive interpretation were considered ASC-H (Fig. 2).
Fig. 1.
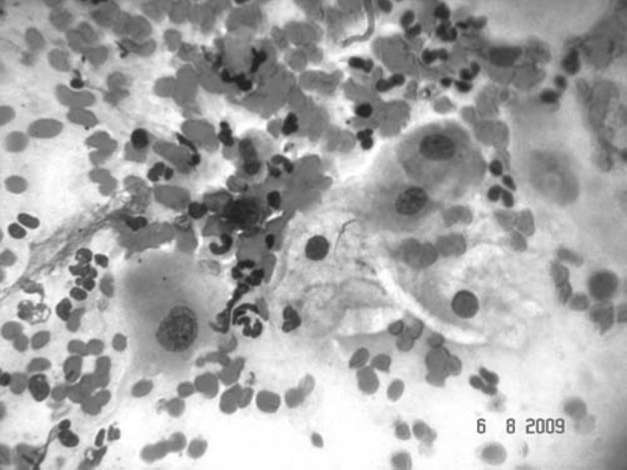
ASCUS. Squamous cells showing mild karyomegaly, hyperchromasia and mildly irregular nuclear contours. (Pap. X 40).
Fig. 2.
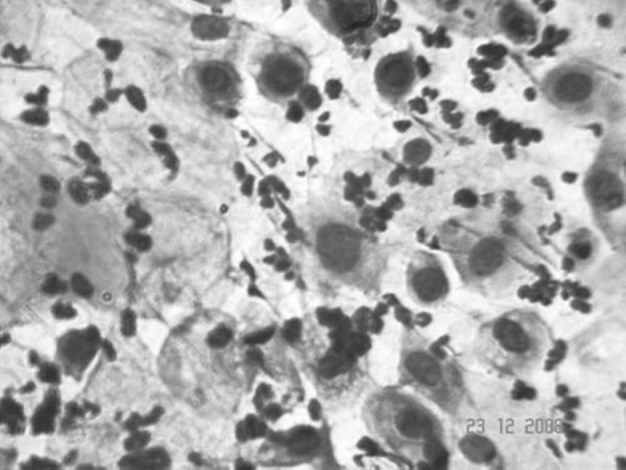
ASC-H Squamous cell with enlarged nuclei and scant cytoplasm with irregular nuclear contours. (Pap, X 40). (Table 2). 73.3% of the cases thus showed regression.
The diagnosis of ASCUS in post menopausal women is especially difficult due to drying artefact, extensive inflammation and degeneration due to atrophic vaginitis. Other age related changes which have been described to cause difficulty in diagnosis include prominent perinuclear halos, nuclear hyperchromasia and variation in nuclear size and multinucleation [12].
Colposcopy as a routine option to evaluate these patients was not considered due to lack of facilities in the institution and expense involved. Considering the fact that most (73.3%) of these lesions regressed, it was probably not a viable option. It is important to follow up these lesions with repeat cytology since HSIL and further progression are known to occur. However, with two consecutive negative Pap smears, these patients were brought to routine screening. Also, with two consecutive Pap smears showing ASCUS (four cases in the present study), the patient was taken up for directed biopsy. This lead to the detection of a case of CIN 3. This underlines the importance of keeping these patients on diligent follow up with repeat smears.
In conclusion, ASCUS as an entity shows a regression rate of up to 73%. Hence the need for a colposcopic evaluation arises only if ASCUS persists. However, as the progression to higher lesions is a known entity, especially with ASC-H, it is of utmost importance that these patients are diligently followed up and biopsied when indicated.
Conflicts of Interest
None identified
Intellectual Contribution of Authors
Study Concept : Col A Chaudhary
Drafting & Manuscript Revision : Lt Col R Tewari
Statistical Analysis : Lt Col R Tewari, Col A Chaudhary
Study Supervision : Col A Chaudhary
References
- 1.Kurman R, Solomon D. The Bethesda system for reporting cervical/vaginal cytologic diagnoses: definitions, criteria and explanatory notes for terminology and specimen adequacy. Springer Verlag; New York: 1994. [Google Scholar]
- 2.Raab SS, Bishop NS, Zaleski MS. Long-term outcome and relative risk in women with atypical squamous cells of undetermined significance. Am J Clin Pathol. 1999;112:57–62. doi: 10.1093/ajcp/112.1.57. [DOI] [PubMed] [Google Scholar]
- 3.Dvorak KA, Finnemore M, Maksem JA. Histology correlation with atypical squamous cells of undetermined significance (ASCUS) and low-grade squamous intraepithelial lesion (LSIL) cytology diagnoses: an argument to ensure ASCUS follow-up that is as aggressive as that for LSIL. Diagn Cytopathol. 1999;21:292–295. doi: 10.1002/(sici)1097-0339(199910)21:4<292::aid-dc13>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 4.Melnikow J, Nuovo J, Willan AR, Chan BK, Howell LP. Natural history of cervical squamous intraepithelial lesions: a metaanalysis. Obstet Gynecol. 1998;92:727–735. doi: 10.1016/s0029-7844(98)00245-2. [DOI] [PubMed] [Google Scholar]
- 5.Howell LP, Davis RL. Follow-up of Papanicolaou smears diagnosed as atypical squamous cells of undetermined significance. Diagn Cytopathol. 1996;14:20–24. doi: 10.1002/(SICI)1097-0339(199602)14:1<20::AID-DC5>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 6.Alanen KW, Elit LM, Molinaro PA, McLachlin CM. Assessment of cytologic follow-up as the recommended management for patients with atypical squamous cells of undetermined significance or low grade squamous intraepithelial lesions. Cancer. 1998;84:5–10. [PubMed] [Google Scholar]
- 7.Williams ML, Rimm DL, Pedigo MA, Frable WJ. Atypical squamous cells of undetermined significance: correlative histologic and follow- up studies from an academic medical center. Diagn Cytopathol. 1997;16:1–7. doi: 10.1002/(sici)1097-0339(199701)16:1<1::aid-dc2>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 8.Gatscha Rose Marie, Abadi Maria, Babore Silvia. Smears diagnosed as ASCUS: Interobserver variation and follow-up. Diagn Cytopathol. 2001;25:138–140. doi: 10.1002/dc.2022. [DOI] [PubMed] [Google Scholar]
- 9.Results of a randomized trial on the management of cytology interpretations of atypical squamous cells of undetermined significance. ASCUS-LSIL Triage Study (ALTS) Group. Am J Obstet Gynecol. 2003;188:1383–1392. doi: 10.1067/mob.2003.457. [DOI] [PubMed] [Google Scholar]
- 10.Solomon D, Davey D, Kurman R. The 2001 Bethesda System: terminology for reporting results of cervical cytology. JAMA. 2002;287:2114–2119. doi: 10.1001/jama.287.16.2114. [DOI] [PubMed] [Google Scholar]
- 11.Gerber S, DeGrandi P, Petignat P. Colposcopic evaluation after a repeat atypical squamous cells of undertermined significance (ASCUS) smear. Int J Gynaecol Obstet. 2001;75:251–255. doi: 10.1016/s0020-7292(01)00479-9. [DOI] [PubMed] [Google Scholar]
- 12.Jovanovic AS, McLachlin CM, Shen L, Welch WR, Crum CP. Postmenopausal squamous atypia: a spectrum including ‘pseudo-koilocytosis.’. Mod Pathol. 1995;8:408–412. [PubMed] [Google Scholar]


