Abstract
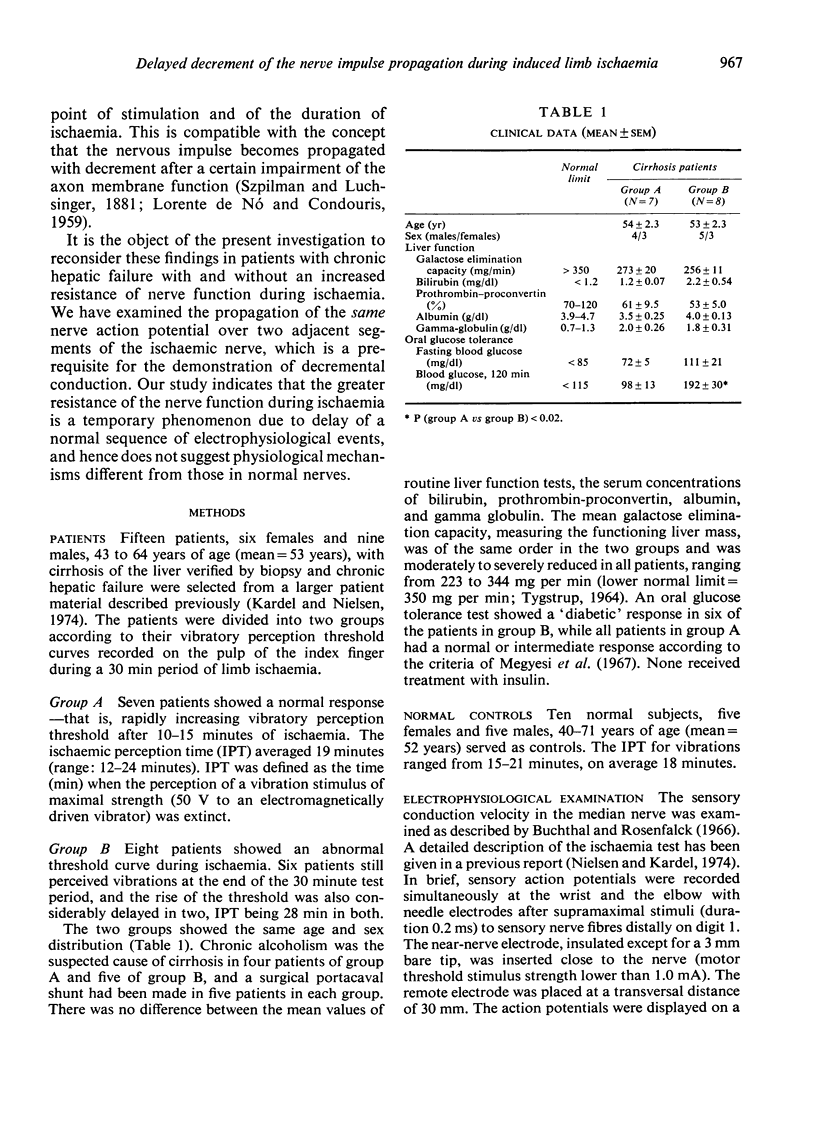
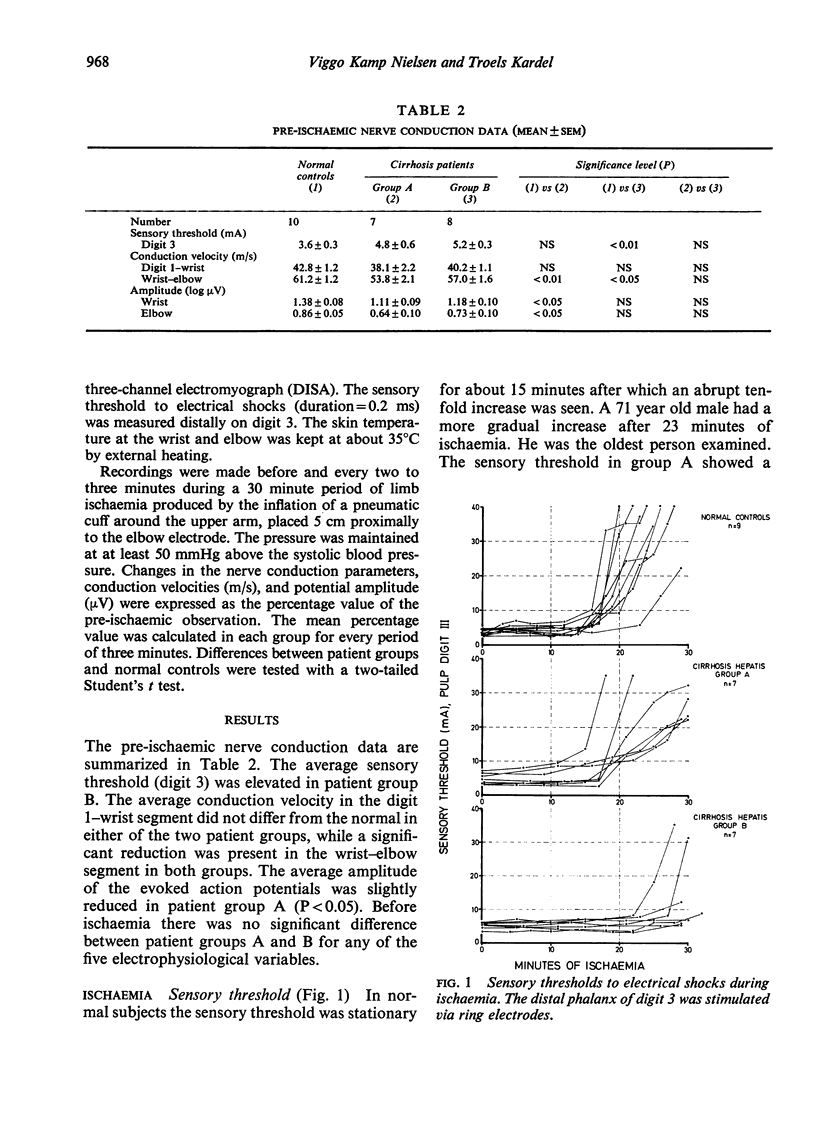
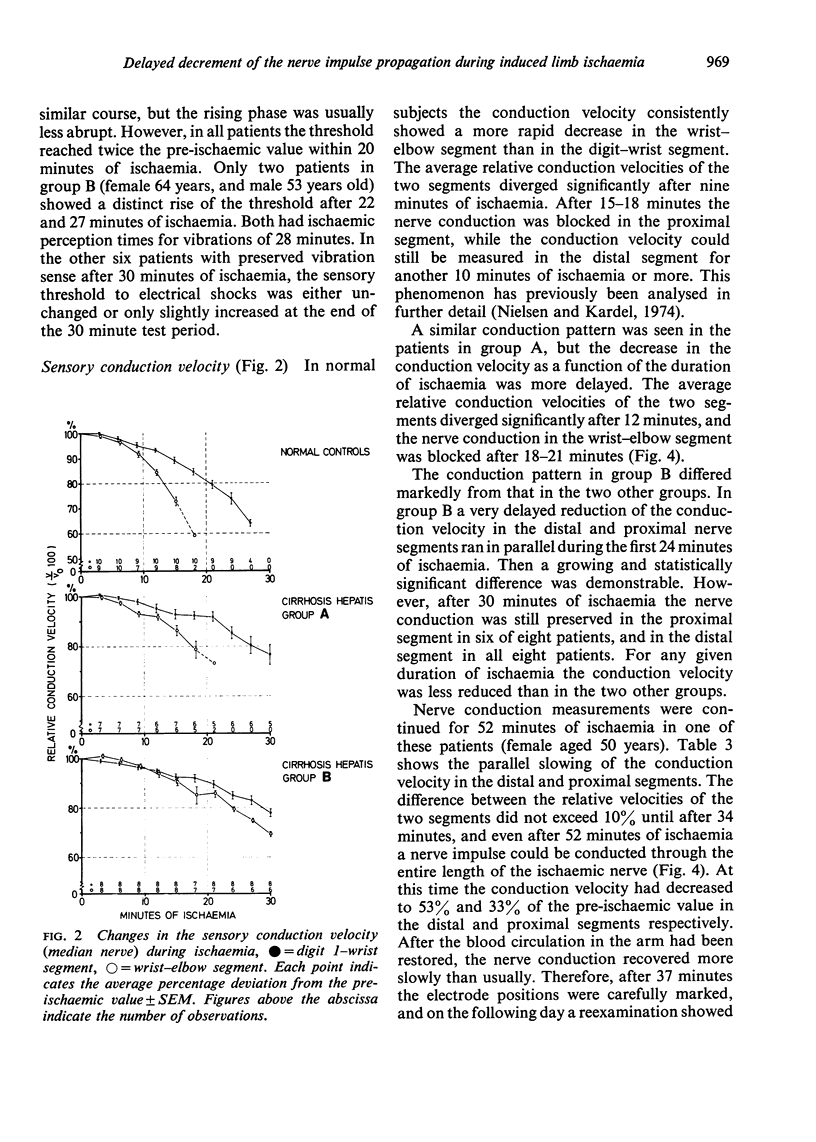
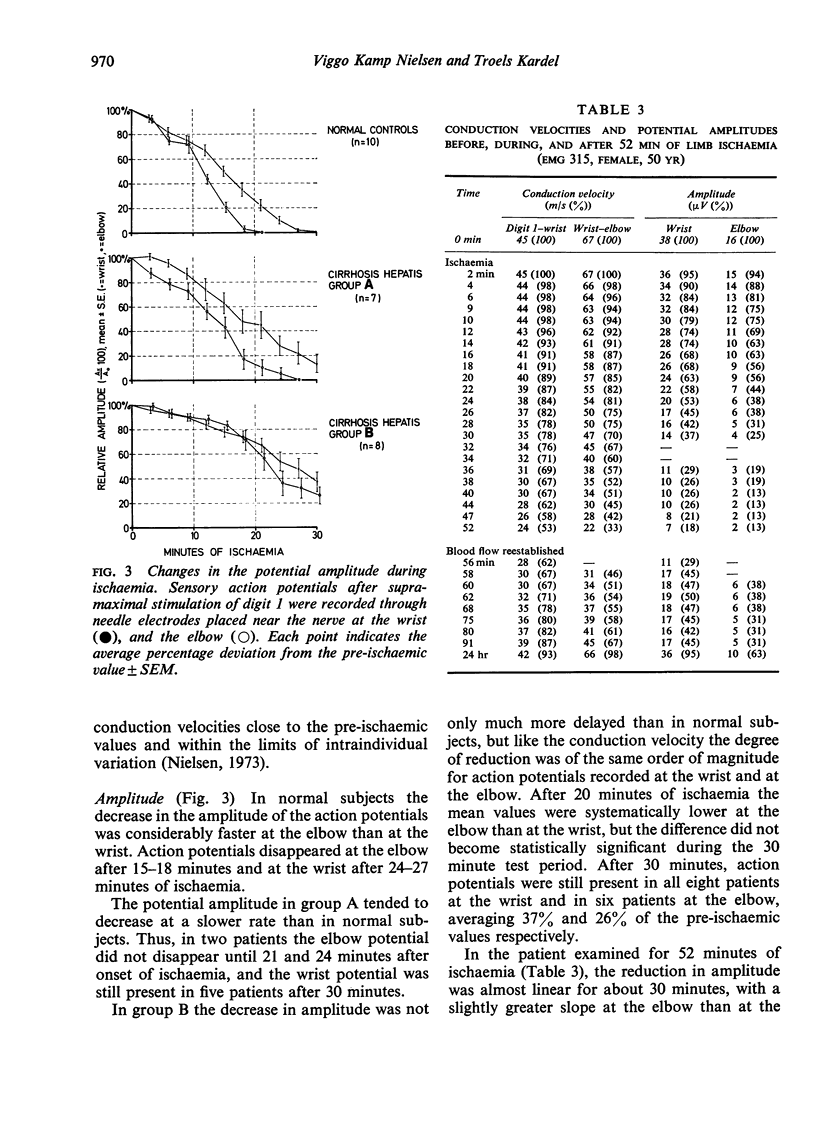
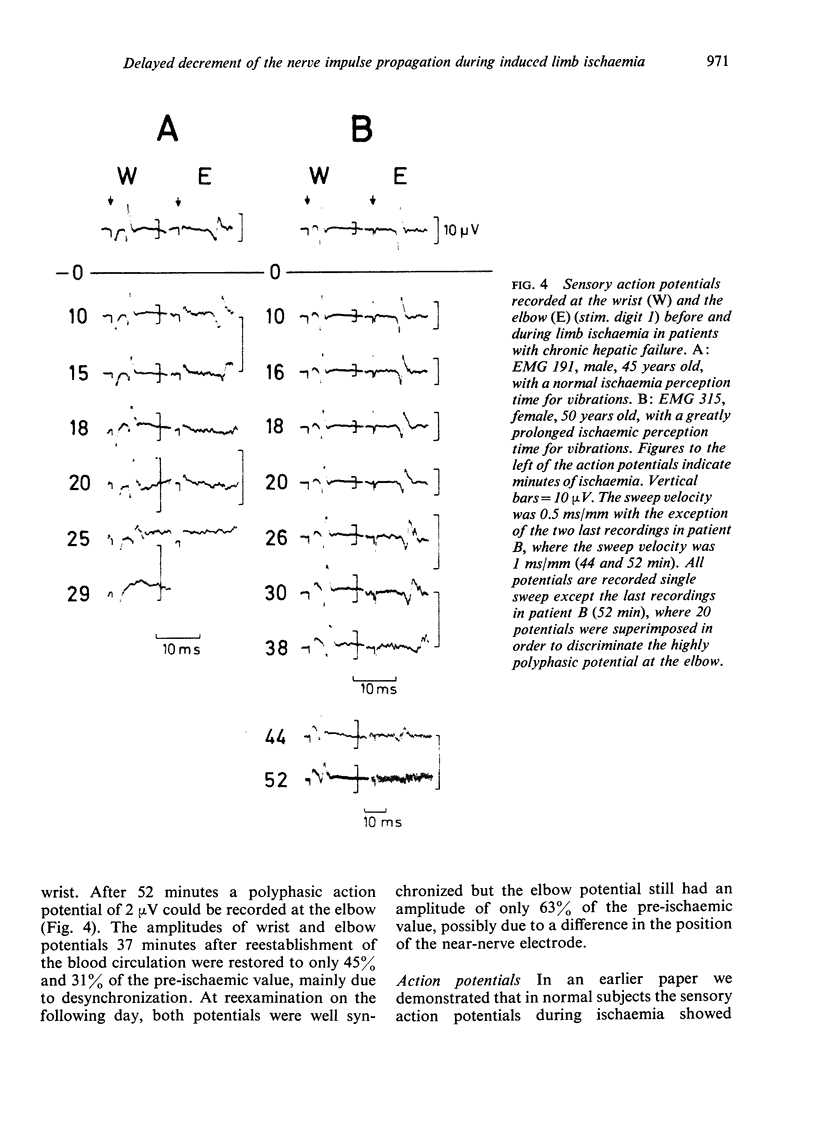
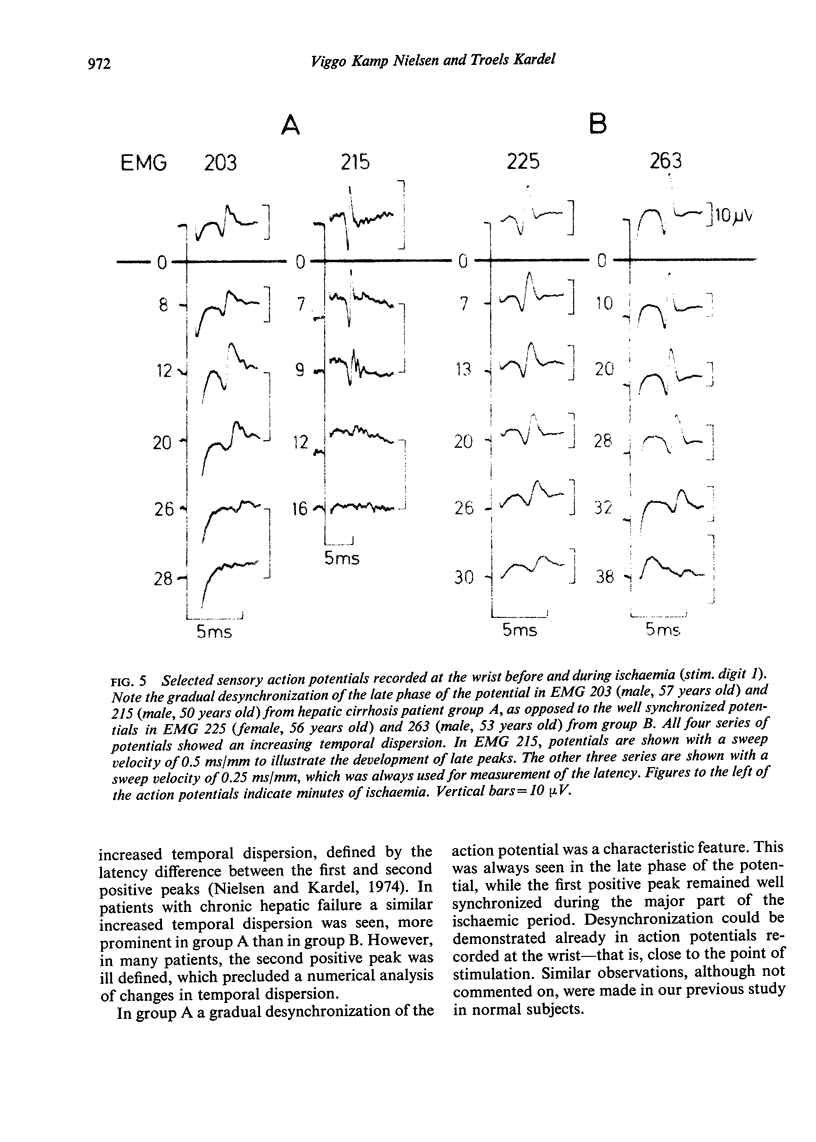
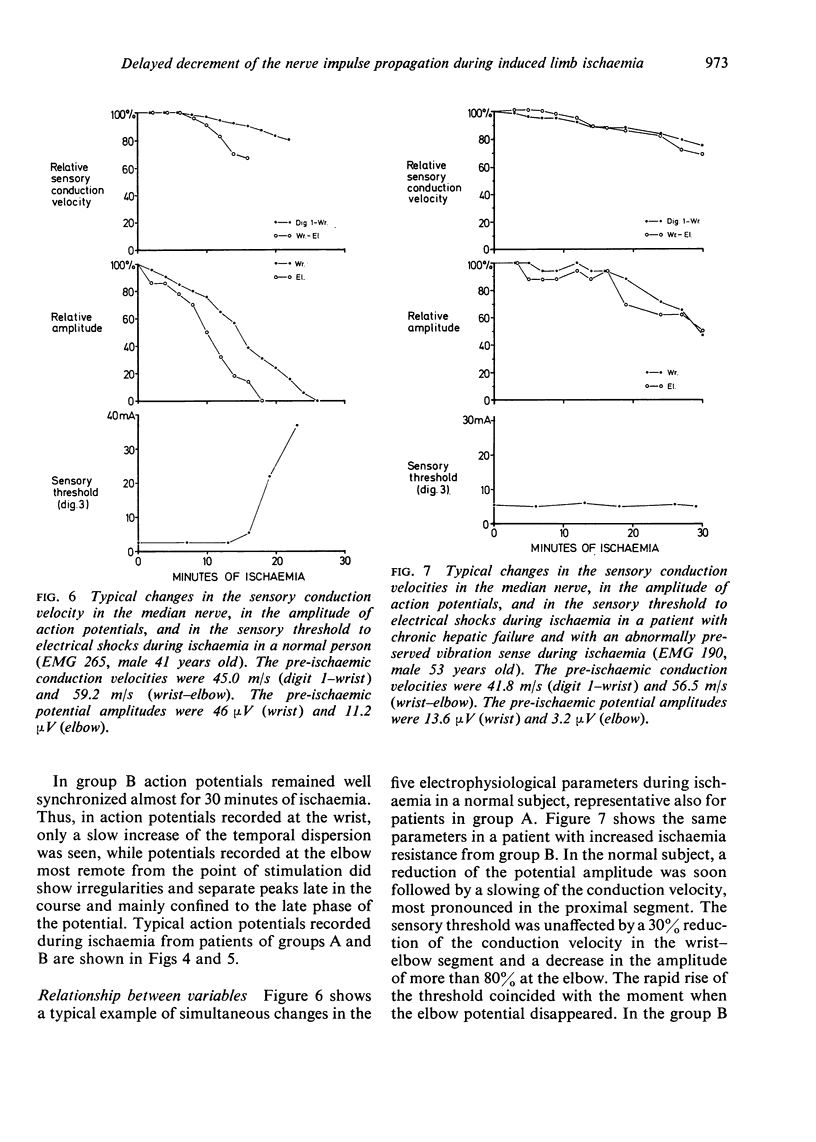
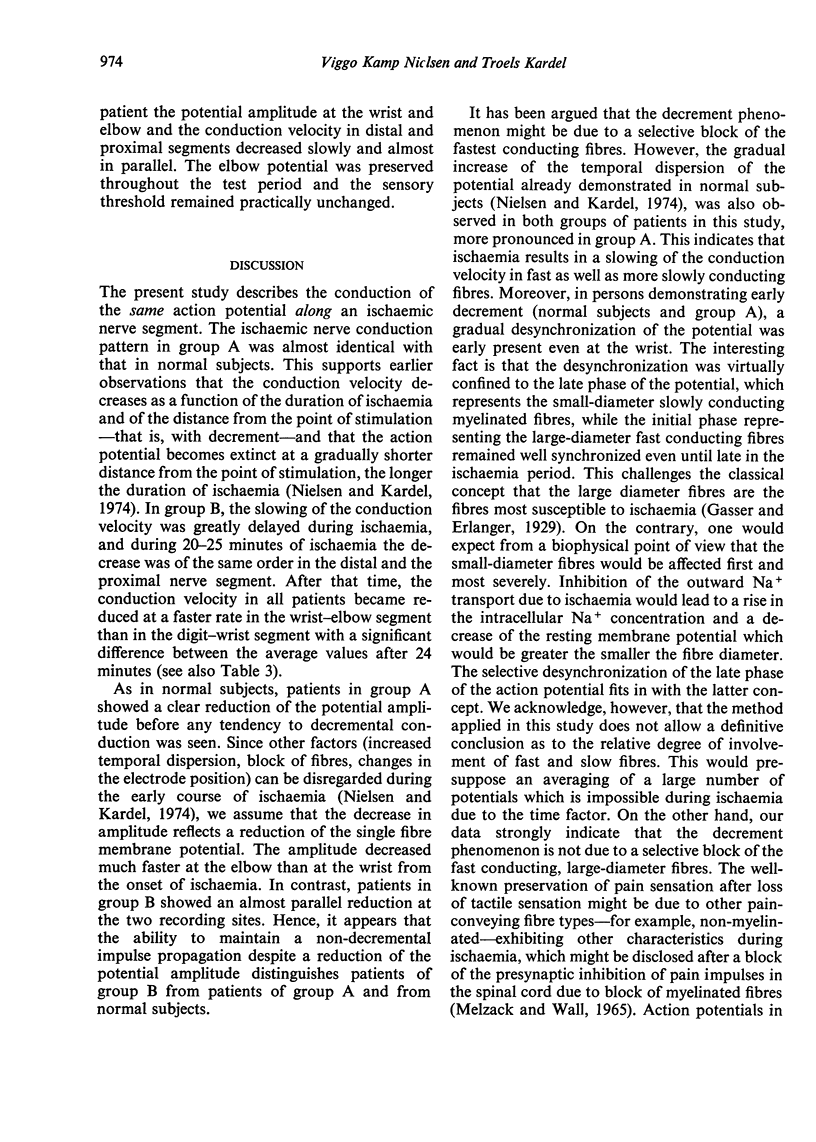
Sensory thresholds for vibrations and electrical shocks and the sensory nerve conduction velocity (median nerve) were measured during 30 minutes of induced limb ischaemia in 10 normal subjects and 15 patients with chronic hepatic failure. Sensory action potentials were recorded simultaneously at the wrist and elbow. Seven patients (group A) had a normal perception time for vibrations. As in normal subjects, the potential amplitude decreased from the onset of ischaemia, more pronounced at the elbow than at the wrist, and the conduction velocity became reduced more rapidly in the wrist-elbow than the first digit-wrist segment, indicating impulse propagation with decrement. Eight patients (group B) had a markedly prolonged perception time for vibrations. The reduction of potential amplitude and conduction velocity was considerably delayed, and the impulse propagation showed no evidence of decrement for 20-25 minutes of ischaemia. A rise of the threshold for electrical shocks was absent or very delayed. As in the two other groups, the rise was abrupt and occurred at the moment when the potential below the occluding cuff (elbow) was extinct. In both groups of patients there was an increasing temporal dispersion of action potentials and in patient group A a desynchronization of the late phase of the potential took place early in the course of ischaemia. Differences between groups A and B could not be predicted from the pre-ischaemic nerve conduction data.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Christensen N. J., Orskov H. Vibratory perception during ischaemia in uraemic patients and in subjects with mild carbohydrate intolerance. J Neurol Neurosurg Psychiatry. 1969 Dec;32(6):519–524. doi: 10.1136/jnnp.32.6.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FULLERTON P. M. THE EFFECT OF ISCHAEMIA ON NERVE CONDUCTION IN THE CARPAL TUNNEL SYNDROME. J Neurol Neurosurg Psychiatry. 1963 Oct;26:385–397. doi: 10.1136/jnnp.26.5.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GILLIATT R. W., WILSON T. G. Ischaemic sensory loss in patients with peripheral nerve lesions. J Neurol Neurosurg Psychiatry. 1954 May;17(2):104–114. doi: 10.1136/jnnp.17.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregersen G. A study of the peripheral nerves in diabetic subjects during ischaemia. J Neurol Neurosurg Psychiatry. 1968 Apr;31(2):175–181. doi: 10.1136/jnnp.31.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregersen G., Pilgaard S. The effect of ischaemia on vibration sense in hypo- or hypercalcaemia and in demyelinated nerves. Acta Neurol Scand. 1971;47(1):71–79. doi: 10.1111/j.1600-0404.1971.tb07465.x. [DOI] [PubMed] [Google Scholar]
- Kardel T., Nielsen V. K. Hepatic neuropathy. A clinical and electrophysiological study. Acta Neurol Scand. 1974;50(4):513–526. [PubMed] [Google Scholar]
- Megyesi C., Samols E., Marks V. Glucose tolerance and diabetes in chronic liver disease. Lancet. 1967 Nov 18;2(7525):1051–1056. doi: 10.1016/s0140-6736(67)90334-0. [DOI] [PubMed] [Google Scholar]
- Melzack R., Wall P. D. Pain mechanisms: a new theory. Science. 1965 Nov 19;150(3699):971–979. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- Moore E. W. Studies with ion exchange calcium electrodes. 3. The state of serum calcium in patients with cirrhosis. Gastroenterology. 1971 Jan;60(1):43–54. [PubMed] [Google Scholar]
- Nielsen V. K., Kardel T. Decremental conduction in normal human nerves subjected to ischemia? Acta Physiol Scand. 1974 Oct;92(2):249–262. doi: 10.1111/j.1748-1716.1974.tb05742.x. [DOI] [PubMed] [Google Scholar]
- Nielsen V. K., Kardel T. Sensory nerve conduction during ischaemia in normal subjects and patients with chronic liver diseases. Acta Neurol Scand Suppl. 1972;51:467–469. [PubMed] [Google Scholar]
- Nielsen V. K. Sensory and motor nerve conduction in the median nerve in normal subjects. Acta Med Scand. 1973 Nov;194(5):435–443. doi: 10.1111/j.0954-6820.1973.tb19469.x. [DOI] [PubMed] [Google Scholar]
- Nó R. L., Condouris G. A. DECREMENTAL CONDUCTION IN PERIPHERAL NERVE. INTEGRATION OF STIMULI IN THE NEURON. Proc Natl Acad Sci U S A. 1959 Apr;45(4):592–617. doi: 10.1073/pnas.45.4.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SHANES A. M. Factors in nerve functioning. Fed Proc. 1951 Sep;10(3):611–621. [PubMed] [Google Scholar]
- STEINESS I. Vibratory perception in diabetics during arrested blood flow to the limb. Acta Med Scand. 1959 Mar 4;163(3):195–205. doi: 10.1111/j.0954-6820.1959.tb10400.x. [DOI] [PubMed] [Google Scholar]
- Seneviratne K. N., Peiris O. A. Peripheral nerve function in chronic liver disease. J Neurol Neurosurg Psychiatry. 1970 Oct;33(5):609–614. doi: 10.1136/jnnp.33.5.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seneviratne K. N., Peiris O. A., Weerasuriya A. Effects of hyperkalaemia on the excitability of peripheral nerve. J Neurol Neurosurg Psychiatry. 1972 Apr;35(2):149–155. doi: 10.1136/jnnp.35.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seneviratne K. N., Weerasuriya A. Nodal gap substance in diabetic nerve. J Neurol Neurosurg Psychiatry. 1974 May;37(5):502–513. doi: 10.1136/jnnp.37.5.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TYGSTRUP N. THE GALACTOSE ELIMINATION CAPACITY IN CONTROL SUBJECTS AND IN PATIENTS WITH CIRRHOSIS OF THE LIVER. Acta Med Scand. 1964 Mar;175:281–289. doi: 10.1111/j.0954-6820.1964.tb00576.x. [DOI] [PubMed] [Google Scholar]