Abstract
Boys appear to engage in eating disorder behavior, particularly nonpurging compensatory behaviors such as driven exercise and fasting, at higher rates than previously thought. Little is known about the development of these behaviors in adolescent boys. In a sample of 631 non-binge eating and non-purging boys studied once in 5th grade and 6 times over the 3 years of middle school (grades 6 through 8), we found that (a) for some youth, driven exercise and fasting were present from grade 6; (b) different boys progressed along different trajectories of engagement in driven exercise and fasting, with some boys engaging in no driven exercise or fasting (65.8% and 83.5%, respectively), some boys engaging in driven exercise and fasting throughout middle school (25.2% and 16.5%, respectively), and other boys discontinuing engagement in driven exercise (9%); (c) 5th grade depression, eating expectancies, and thinness expectancies predicted subsequent trajectory group membership; and (d) boys engaging in driven exercise and fasting in 8th grade remained distressed. Boys’ engagement in driven exercise and fasting behavior merits the attention of researchers and clinicians.
Keywords: eating disorders, driven exercise, fasting, adolescence, males
Although female patients account for most eating disorder diagnoses (Leon, Fulkerson, Perry, & Early-Zald, 1995), recognition of eating disorder behaviors in males has increased in recent years (Hay, Mond, Buttner, & Darby, 2008), with studies reporting that males account for 10-25% of eating disorder cases (Rosen, 2010; Sigel, 2008). In particular, males are more likely to engage in nonpurging compensatory behaviors such as driven exercise (Allen, Crosby, Oddy, & Byrne, 2013; Stiles-Shields, Goldschmidt, Boepple, Glunz, & le Grange, 2011) and fasting (Allen et al., 2013; Pisetsky, Chao, Dierker, May, & Striegel-Moore, 2008) compared to purging behaviors such as self-induced vomiting, for weight control. Driven exercise refers to intense physical activity designed to control one's weight or shape, or in response to an episode of excessive food consumption, and that is described as compelled or compulsive (Fairburn & Cooper, 1993). Fasting is generally defined as not eating for at least 8 waking hours for the purpose of controlling one's weight and/or shape (Cooper & Fairburn, 1987).1
Emerging research suggests that syndromes characterized by nonpurging compensatory behaviors in the absence of binge eating and purging in women are associated with body image disturbance (Davis, Holland, & Keel, 2014), anxiety (Davis et al., 2014), functional impairment (Mond et al., 2006), and increased likelihood of psychiatric hospitalization among adults (Tobin, Griffing, & Griffing, 1997). These findings indicate the need for increased research on nonpurging compensatory behaviors. In adolescent girls, these behaviors are harmful and distressing in the absence of binge eating and purging (Davis, Guller, & Smith, 2014). One study found that adolescent girls engaging in driven exercise or fasting reported similar impairment and distress to girls experiencing anorexia nervosa (AN: Wade & O'shea, 2015). However, little is known about the emergence and development of these behaviors in adolescent boys.
Because traditional eating disorder symptoms often emerge during the middle school years (grades 6-8 in the current sample; Bulik, 2002; Pearson, Zapolski, & Smith, 2015) and because boys do seem to engage in disordered eating behavior at young ages (Pinhas, Morris, Crosby, & Katsman, 2011), it is important to understand the presence and developmental course of nonpurging compensatory behaviors in boys this age. We therefore investigated if these behaviors occur in middle school-aged boys, engagement in the behaviors follows different developmental courses for different boys across the middle school years, and if it is possible to predict the behaviors from the presence of elementary school risk factors.
To predict these behaviors, we studied four risk factors. The first was depressive symptomatology, which tends to co-occur with eating pathology in adolescent girls and boys (Godart et al., 2007) and is a risk factor for the development of disordered eating in the transition from childhood to adolescence (Ferreiro, Wichstrøm, Seoane, & Senra, 2014). The second was the expectancy that eating helps manage negative affect, and third was the expectancy that thinness leads to overgeneralized life improvement (Hohlstein, Smith, & Atlas, 1998).
We studied these two types of expectancies as risk factors for two reasons. First, expectancies are understood to be summaries of individuals’ learning histories. They guide future behavioral choices because they are learned anticipations of the likely consequences of possible behaviors (Goldman, Brown, Christiansen, & Smith, 1991). Eating and thinness expectancies are understood to be precursors to other important eating disorder risk factors (Pearson, Wonderlich, & Smith, 2015). Endorsement of the expectancy that eating helps manage negative affect can be understood to reflect a summary of learning experiences relating eating to negative reinforcement that contributes to emotional eating, and hence to loss of control eating. Endorsement of the expectancy that thinness leads to overgeneralized life improvement reflects a summary of learning experiences relating thinness to a wide range of reinforcers, and thus contributes to internalization of the thin ideal as well as body dissatisfaction that so frequently results from comparisons of the self to the ideal (Pearson et al., 2015).
Second, there is good reason to think that expectancies for reinforcement from eating and from thinness relate to nonpurging compensatory behaviors. Strong endorsement of the expectancy that thinness brings overgeneralized life improvement could well precipitate engagement in behaviors such as driven exercise or fasting. Endorsement of expectancies for reinforcement from eating has been shown to lead to excessive food consumption (Pearson et al., 2015), which can increase the likelihood of compensatory behaviors such as driven exercise or fasting. It is perhaps relevant that the two expectancies predict the subsequent onset of, and increases in, binge eating and purging in adolescent girls and boys (Pearson, Combs, Zapolski, & Smith, 2012; Smith, Simmons, Flory, Annus, & Hill, 2007).
Both genders report the desire to alter shape or weight (Ricciardelli & McCabe, 2001), and approximately 33% of adolescent boys desire a leaner body (McCabe & Ricciardelli, 2001). Expectancies for reinforcement from both eating and thinness may thus prove useful in predicting the development and maintenance of nonpurging compensatory behaviors in adolescent boys. Boys who expect high levels of reinforcement from thinness may be disposed to exercise in a driven way or to fast, and boys who expect high levels of reinforcement from eating may consume more food than others, thus increasing their risk for subsequent driven exercise or fasting behavior.
The fourth risk factor we studied was pubertal onset. Although pubertal onset has been shown to be related to heritable risk for bulimic behaviors in girls (Culbert, Burt, McGue, Iacono, & Klump, 2009), the evidence for an association between pubertal onset and increased risk for eating disordered behavior in boys is mixed (Klump, 2013). To our knowledge, no prior study has examined the effect of pubertal status on the development of nonpurging compensatory behaviors in the absence of binge eating and purging in adolescent boys. Thus, we viewed investigation of this risk factor as exploratory.2
Two trajectory analyses were conducted on a sample of 631 adolescent boys across six time points over the 3 years of middle school: one each for driven exercise and fasting. Trajectory analysis is a statistical method that seeks to identify different subgroups of boys who proceed along different developmental pathways over time (Nagin, 2005). We investigated trajectories because we had no reason to assume that all boys progressed along the same paths in relation to these behaviors. We had no a priori hypothesis for what trajectories might emerge from analyses given that little is known about the developmental course of these behaviors over time. To determine if engagement in, or the development of, driven exercise and fasting behaviors can be predicted from traditional eating disorder risk factors measured earlier in time, we tested whether depressive symptoms and eating and thinness expectancies measured 6 months prior to the start of the trajectory period (in the spring of fifth grade) predicted trajectory group membership. To determine if ongoing engagement in driven exercise or fasting is associated with depression symptoms and elevated eating and thinness expectancies, we compared trajectory groups to each other at the end of the trajectory period in the spring of eighth grade.
An additional question is whether driven exercise and fasting can be understood as two symptoms of a common nonpurging compensatory disorder (see Tobin et al., 1997). We therefore investigated the co-occurrence of the two behaviors. If they covary highly, the possible utility of defining a single, nonpurging compensatory disorder would merit further investigation.
Method
Sample
Participants were drawn from a longitudinal sample of 972 boys who were assessed at seven time points: Spring of the last year of elementary school (fifth grade; Wave 0), and fall and spring of each year of middle school (sixth through eighth grades; Waves 1-6). The mean age of the participants at the initiation of the study was 10.33 years. Most were European American (60.9%), followed by African American (18.7%); the remainder of the sample identified themselves as Hispanic (8.2%), Asian (2.9%), Middle Eastern (0.4%), or other (8.8%). To study the presence and development of driven exercise and fasting behavior in the absence of binge eating and purging in these youth, we selected a subsample comprising all participants who did not report binge eating or purging during any of the seven waves. The subsample included 631 boys and it did not differ from the larger sample on any demographic variable.
Measures
Demographic and Background Questionnaire
This measure provided the assessment of the following demographic information: school, age, grade, and racial/ethnic background.
Eating Disorder Examination- Questionnaire (EDE-Q; Fairburn & Beglin, 1994)
We used the EDE-Q, which is a self-report version of the Eating Disorders Examination semi-structured interview (Cooper & Fairburn, 1987) to assess fasting and driven exercise. The EDE-Q has been shown to have good reliability and validity, particularly in clinical samples (Cooper & Fairburn, 1993; Mond, Hay, Rodgers, Owen, & Beumont, 2004). Following existing recommendations for use of the measure with youth, we adapted the EDE-Q by using age-appropriate wording, defining concepts that might be difficult to understand, and shortening the length of time referred to in the questions to the past 14 days (Carter, Stewart, & Fairburn, 2001), although we note that other researchers have preserved the 28 day interval used with adults (Theim, Wilfley, Beach, Tanofsky-Kraff, & Goldschmidt, 2014). We were unable to compute a global EDE-Q score. We measured driven exercise with a sequence of two questions. The first was “Over the past 2 weeks, have you exercised a lot as a way to control your weight or because you ate a lot?” The item was dichotomous. Participants who responded “yes” then completed a second item: “If yes, on how many days of the last 14 have you done this?” There were six response options, ranging from “1-2 days” through “14 days or every day.” We combined the two items, such that 0 reflected no driven exercise, one reflected having done so 1-2 days of the last 14, and so on. To measure fasting behavior, we used the item “Over the past 2 weeks, have you gone for long periods of time (8 hours or more) without eating in order to control your shape or weight?” Responses were dichotomous.
Center for Epidemiological Studies-Depression Scale (CES-D; Radloff, 1977)
We used the CES-D to measure individual differences in depressive symptomology. The scale has proven reliable and valid in numerous studies; it is frequently used with children, adolescents, and adults (Clarke et al., 2005; Radloff, 1977). The possible range of scores is zero to 30, with higher scores indicating more depression symptoms in the previous week (Radloff, 1977). We used CES-D scores as interval scale indicators of depressive symptomology (α = .76 in Wave 0 and higher in subsequent waves). Test-retest reliability was .87 in one study (Miller, Anton, Townson, 2008).
Eating Expectancy Inventory (EEI; Hohlstein et al., 1998)
From this five-factor measure, we used the scale reflecting the expectancy that eating helps one manage negative mood states. Total scores range from 8 to 32, with higher scores indicating greater endorsement of the expectancy that eating alleviates negative affect. This scale has been shown to differentiate women with BN from women with AN and both psychiatric and normal controls (Hohlstein et al., 1998); the scale also predicts the subsequent onset of binge eating in both boys and girls (Pearson et al., 2012; Smith et al., 2007). In the current sample the scale was internally consistent (Wave 0 α = .93 and higher in subsequent waves).
Thinness and Restricting Expectancy Inventory (TREI; Hohlstein et al., 1998)
This measure reflects overgeneralized expectancies about the life benefits of dieting and thinness. It consists of eight items in Likert format. Total scores range from eight to 32, with higher scores indicating greater endorsement of the expectancy that dieting and thinness lead to a better life. Items include such statements as “I would feel like I could do whatever I wanted to if I were thin.” The scale has been shown to be unidimensional, correlated with eating disorder symptoms in adolescent and adult female samples, and predictive of eating disorder symptom onset (Hohlstein et al., 1998; MacBrayer, Smith, McCarthy, Demos, & Simmons, 2001; Smith et al., 2007). In boys, it correlates with binge eating and purging (Pearson, Combs, & Smith, 2010). Scores were internally consistent in this sample (Wave 0 α = .91 and higher in subsequent waves).
The Pubertal Development Scale (PDS; Petersen, Crockett, Richards, & Boxer, 1988)
The PDS consists of five questions in a Likert-type rating format. An example item is “Has your skin started to change yet?” This measure correlates highly with physician ratings and other forms of self-report (Coleman & Coleman, 2002). As is common, we dichotomized pubertal status (Culbert et al., 2009).
Procedure
Data collection
Each wave, the questionnaires were administered in public schools during school hours (23 elementary schools at Wave 0; 15 middle schools, which included the children from the 23 elementary schools, at Waves 1-6). A passive consent procedure was used. Each family was sent a letter, through the U.S. Mail, introducing the study. Families were asked to return an enclosed, stamped letter or call a phone number if they did not want their child to participate. Out of 1,011 students whose families approached by letter, 96.1%, or 972, of the students participated in the study. Reasons for non-participation were as follows: 16 families declined participation for their child (1.6%), 11 students declined assent (1.1%), and 12 did not participate for a variety of other reasons, such as language disabilities that precluded completing the questionnaires (1.1%).
Data collections took place in the spring of fifth grade and then the fall and spring in the 3 consecutive years of sixth, seventh, and eighth grades (the 3 years of middle school in the participating school systems). Questionnaires were administered in school classrooms or cafeterias. It was made clear to the students that their responses to the measures were to be kept confidential and no one outside of the research team would see them. The research team introduced the federal certificate of confidentiality for the project and emphasized that they were legally bound to keep all responses confidential. After each participant signed the assent form, the researchers then passed out packets of questionnaires. Participants who moved out of the study's school districts were contacted and asked to complete the forms by mail and were paid $30 for doing so. The questionnaire administration took 60 minutes or less. This procedure was approved by the University's IRB and by the participating school systems. There was no compensation for participants (except for those who moved out of district).
Data analytic method
The primary analyses for this study were two trajectory analyses. We examined trajectories of the development of driven exercise behavior and fasting behavior across the six waves capturing the 3 middle school years. We applied finite mixture modeling (Nagin, 2005), using SAS Version 9.1 PROC TRAJ, to model trajectories as a function of measurement wave. We used zero inflated poisson (ZIP) modeling because a large number of participant responses were zeros (reflecting non-engagement in driven exercise or fasting). When using this method, one assumes that the target population can accurately be described as a mixture of distinct groups defined by their developmental trajectories. In brief, longitudinal data are used to identify the number of groups that best fits the data and to describe the shape of the trajectory for each group. One can then calculate the probability of each individual belonging to each of the trajectory groups that make up the model; individuals can then be assigned to the group to which the probability of their belonging is the highest.
Several fit indices are used to determine the optimal number of groups and the validity of the grouping result. The Bayesian Information Criterion (BIC) and the Akaike Information Criterion (AIC) become increasingly less negative with improvements in the fit of the group structure. Those statistics can be supplemented by additional statistics and guidelines for selecting the best trajectory solution. When the average probability of group membership is greater than .70 for each group (Nagin, 2005), the identified group structure is thought to fit well. One also avoids group structures with extremely small group sizes, out of concern for the stability of the structure (Nagin, 2005).
Once we had determined trajectory group structure and assigned individuals to groups, we conducted analysis of variance (ANOVA) and planned contrasts within ANOVA to compare the groups on measures of depression, eating expectancies, thinness expectancies, and pubertal status measured in the spring of fifth grade, 6 months prior to the onset of the trajectory period, and again in the spring of eighth grade, Wave 6 of the trajectory period. Doing so enabled us to see if elementary school elevations on any of these risk factors predicted subsequent trajectory group membership, and whether elevations persisted with continued engagement in the behaviors. Finally, we used chi-square analysis to examine covariation between membership in driven exercise and fasting trajectory groups.
Results
Participant Attrition Analysis and Treatment of Missing Data
Retention rates did not differ between the 631 boys on whom we conducted the trajectory analyses and the full longitudinal sample of 972 boys. Of the full sample, the percentage who participated ranged from 97.0% at Wave 03 and 94.5% at Wave 1 to 80.0% at Wave 6. Analyses comparing those who participated and those who did not on all study variables indicated no significant differences and Little's missing completely at random test produced a non-significant result. Thus, data appeared to be missing at random, and we used the expectation maximization procedure to impute values for the missing data points. This procedure has been shown to produce relatively unbiased population parameter estimates and to be superior to traditional methods (Little & Rubin, 1989). As a result, we were able to make full use of the sample of 631.
Possible Effects due to School Membership
In order to determine whether there was significant covariance among the study variables due to participants attending the same school, we calculated intraclass coefficients for each variable (using elementary school membership, n = 23, as the nesting variable). Intraclass coefficients ranged from .03 to .00. We therefore concluded that school membership was essentially unrelated to study variables.
Descriptive Statistics
Table 1 presents the frequencies of driven exercise and fasting over the 2 weeks preceding the assessments. As Table 1 shows, from Waves 1 through 6, over 8% of boys reported at least some driven exercise and over 3% of boys reported at least some fasting over the preceding 2 weeks. Table 2 presents the means and standard deviations for depression, eating expectancies, and thinness expectancies in the spring of fifth grade (Wave 0) and in the spring of eighth grade (Wave 6), as well as the percentage of boys who had experienced pubertal onset. Table 3 presents correlations among all study variables at Wave 0.
Table 1.
Descriptive Statistics: Driven Exercise and Fasting (N=631).
| Frequency (%) Endorsing Driven Exercise in Last 14 Days | ||||||
|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 5 | Wave 6 | |
| None | 497 (78.8) | 485 (76.9) | 514 (81.5) | 518 (82.1) | 498 (78.9) | 497 (78.8) |
| 1-2 days | 54 (8.6) | 60 (9.5) | 54 (8.6) | 64 (10.1) | 87 (13.8) | 85 (13.5) |
| 3-4 days | 34 (5.4) | 30 (4.8) | 23 (3.6) | 22 (3.5) | 26 (4.1) | 34 (5.4) |
| 5-7 days | 24 (3.8) | 27 (4.3) | 19 (3.0) | 9 (1.4) | 6 (1.0) | 6 (1.0) |
| 8-10 days | 5 (0.8) | 12 (1.9) | 10 (1.6) | 5 (0.8) | 6 (1.0) | 1 (0.2) |
| 11-13 days | 1 (0.2) | 4 (0.6) | 2 (0.3) | 5 (0.8) | 3 (0.5) | 2 (0.3) |
| >14 days | 16 (2.5) | 13 (2.1) | 9 (1.4) | 8 (1.3) | 5 (0.8) | 6 (1.0) |
|
Number of Participants (%) Endorsing Fasting in Last 14 Days During Trajectory Period | ||||||
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 5 | Wave 6 | |
| 36 (5.7) | 42 (6.7) | 30 (4.8) | 24 (3.8) | 30 (4.8) | 21 (3.3) | |
Table 2.
Descriptive Statistics: Study Variables at Wave 0 (spring, 5th grade) and Wave 6 (spring, 8th grade)
| Factor and Wave | M | SD |
|---|---|---|
| Depression Symptoms- Wave 0 | 13.50 | 7.75 |
| Depression Symptoms- Wave 6 | 12.72 | 7.71 |
| Eating Expectancies- Wave 0 | 2.11 | 1.26 |
| Eating Expectancies- Wave 6 | 1.62 | 0.97 |
| Thinness Expectancies- Wave 0 | 2.94 | 1.55 |
| Thinness Expectancies- Wave 6 | 2.16 | 1.45 |
| Pubertal Onset Status-Wave 0 | 20.6% | |
| Pubertal Onset Status- Wave 6 | 75.9% | |
Note. CES-D scores can range from 0 - 30. EEI and TREI scores are mean item scores, where 2 = not like me and 3 = somewhat like me.
Table 3.
Correlations among Study Variables at Wave 0, spring of 5th grade
| Driven Exercise | Fasting | Depression | Eating Expectancies | Thinness Expectancies | |
|---|---|---|---|---|---|
| Driven Exercise | - | - | - | - | - |
| Fasting | .33** | - | - | - | - |
| Depression | .15** | .21* | - | - | - |
| Eating Expectancies | .08 | .01 | .19** | - | - |
| Thinness Expectancies | .23** | .18** | .19** | .25** | - |
| Pubertal Status | .14** | .09 | .13** | −.01 | .07 |
Note. N = 631
p ≤ .01
p ≤ .001
Developmental Trajectories of Driven exercise
We used Nagin's (2005) procedure to determine (a) whether individual differences in boys’ trajectories of driven exercise could be characterized in terms of subgroups and (b) what the number and shapes of the resulting trajectory groups were.
Driven exercise Trajectories: Selection of Trajectory Model
The BIC and AIC values became progressively less negative from the two-group solution to the three-group solution, but worsened with the four-group solution. The four-group solution included groups with very small samples sizes and did not involve groups with substantively different trajectories from those apparent in the three-group solution. We therefore adopted the three-group solution. The three-group solution for driven exercise among boys had average group membership probabilities from .93 to .98.
Driven Exercise Behavior Trajectories
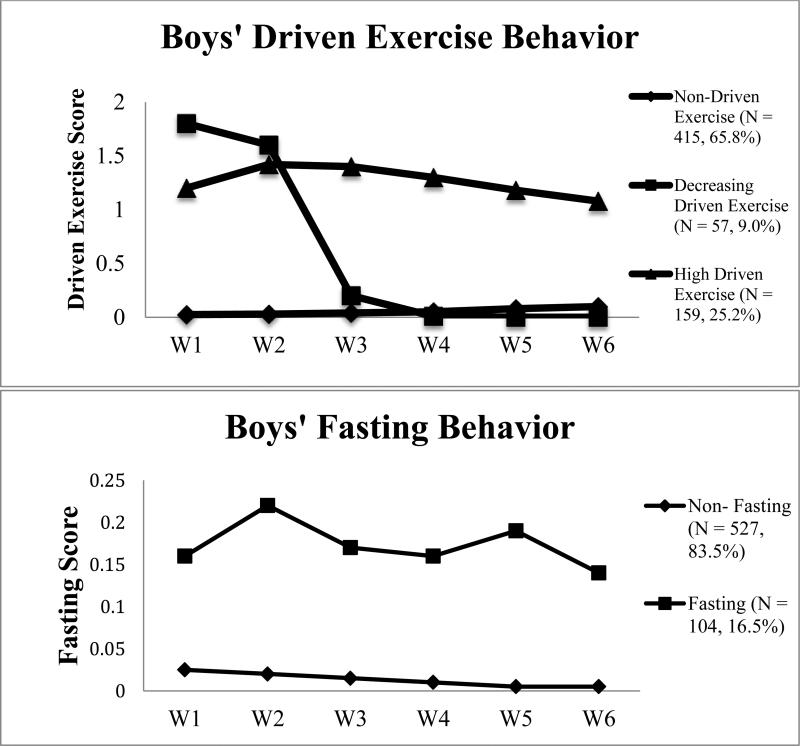
As shown in the top panel of Figure 1, of the 631 boys, 415 consistently reported very little driven exercise behavior across the 3-year, six-wave trajectory period. We refer to this group as the non-driven exercise group. The rate of linear increase for this group was statistically significant: t(414)=5.50, p < .001; it appears that as these boys progressed through middle school, they became a little more likely to engage in exercise behavior to control weight or shape, but did not do so at a high level, as the average value in the spring of eighth grade is still near zero. A group of 57 boys reported high levels of engagement in driven exercise in sixth grade, with a dramatic decrease to essentially no driven exercise in eighth grade. While the average boy in this group reported driven exercise 3-4 times over the last 14 days in sixth grade, the average boy reported no driven exercise by the end of eighth grade. We refer to this group as the decreasing group: the rate of linear decrease was statistically significant, t(56) = −2.18, p < .05. The final group of 159 boys is characterized by a trajectory of driven exercise that remained consistently high across all 3 years of middle school. We refer to this group as the high driven exercise group. The reported behavior of this group of boys followed a statistically significant quadratic slope, t(158)=−2.81, p < .01, reflecting a concave trend.
Figure 1.
Results of trajectory analyses on reported driven exercise and fasting behavior among boys, semiannually from 6th through 8th grades. The top panel presents trajectories of driven exercise behavior and the bottom panel presents trajectories of fasting behavior among boys. W1 – W6: wave 1 through wave 6. The Y axis reflects mean number of occasions in the preceding two weeks.
Prediction of Driven Exercise Group Membership
At Wave 0 (spring of fifth grade), the three groups differed significantly on depression, F(2, 628) = 7.58, p < .001, expectancies that eating helps alleviate negative affect, F(2, 628) = 3.79, p < .02, and expectancies for overgeneralized life improvement from thinness, F(2, 628) = 18.51, p < .001. Table 4 summarizes these and the following results. We followed these overall ANOVA tests with planned comparisons.
Table 4.
Driven Exercise Group Comparisons at Wave 0, spring of 5th grade, and Wave 6, spring of 8th grade
| Driven Exercise Trajectory Group Means (SD) | Contrast 1 (Decreasing and High vs. Non-Driven Exercise) | Contrast 2 (Decreasing vs. High) | Contrast 3 (Decreasing vs. Non-Driven Exercise) | |||
|---|---|---|---|---|---|---|
| Study Variable | None | Decreasing | High | t(d) | t(d) | t(d) |
| Depression- Wave 0 | 12.77 (7.16) | 14.05 (8.17) | 15.54 (8.69) | 2.88** (0.30) | 1.26 (0.18) | --- |
| Eating Expectancies- Wave 0 | 2.03 (1.18) | 2.43 (1.43) | 2.25 (1.36) | 2.75** (0.21) | 0.96 (0.13) | --- |
| Thinness Expectancies- Wave 0 | 2.68 (1.47) | 3.27 (1.54) | 3.50 (1.60) | 5.10*** (0.50) | 1.01 (0.43) | --- |
| Depression- Wave 6 | 11.75 (7.28) | 12.53 (7.50) | 15.30 (8.31) | 0.73 (0.11) | 2.37* (0.35) | 0.73 (0.11) |
| Eating Expectancies- Wave 6 | 1.58 (0.94) | 1.42 (1.03) | 1.81 (1.00) | 1.16 (0.16) | 2.60** (0.38) | 1.16 (0.16) |
| Thinness Expectancies- Wave 6 | 2.02 (1.43) | 1.91 (1.41) | 2.62 (1.43) | 0.54 (0.07) | 3.20*** (0.50) | 0.54 (0.07) |
| None | Decreasing | Increasing | x2 (Φ) | x2 (Φ) | x2 (Φ) | |
| Pubertal Status- Wave 0 | 16.4% | 33.3% | 27.0% | 13.18*** (0.14) | 0.81 (0.06) | --- |
| Pubertal Status- Wave 6 | 73.5% | 82.5% | 79.9% | 2.12 (0.07) | 0.03 (0.06) | 2.12 (0.07) |
Note. N = 631; t: t-test; d: measure of effect size; Φ: phi coefficient, which is a measure of magnitude for chi-square.
p < .05
p <. 01
p <. 001
High and Decreasing groups vs. Non-Driven Exercise group
We first compared the combination of the high driven exercise and decreasing driven exercise trajectory groups to the non-driven exercise group on each variable in fifth grade (Wave 0). Those two groups were higher in depression symptoms, expectancies that eating helps alleviate negative affect, expectancies for overgeneralized life improvement from thinness, and were more likely to have undergone pubertal onset at Wave 0 than were boys in the non-driven exercise group.
Decreasing group vs. High group
We next compared the decreasing driven exercise group to the high driven exercise group to see if those groups, though both engaging in driven exercise at Wave 1 (fall of sixth grade), could be differentiated on any symptom and risk variables. The two groups did not differ in depression, expectancies for reinforcement from eating, expectancies for reinforcement from thinness, or pubertal status at Wave 0. Thus, the decreasing and high driven exercise groups are virtually indistinguishable, not only by level of engagement in driven exercise in sixth grade (Wave 1), but also by depression level, eating expectancies, thinness expectancies, and pubertal status in fifth grade (Wave 0).
Driven Exercise Group Comparisons at the End of the Trajectory period
Because engagement in driven exercise behavior changed a great deal for the decreasing group from the start of middle school (sixth grade) to the end of middle school (eighth grade), we compared the decreasing driven exercise group to a) the non-driven exercise group and b) the high driven exercise group at the end of the trajectory period (Wave 6; spring of eighth grade) on each study variable. By Wave 6, boys in the decreasing driven exercise group did not differ from boys in the non-driven exercise group on depression, eating expectancies, thinness expectancies, or pubertal status. Also at Wave 6, boys in this group reported fewer depression symptoms, weaker expectations for reinforcement from thinness, and weaker expectations for reinforcement from eating compared to boys in the high driven exercise group. That is, boys who began middle school by engaging in driven exercise 3-4 times per week and decreased to less than one time per week by the end of eighth grade (Wave 6) went from being similar to boys in the high driven exercise group in depressive symptoms, eating expectancies, and thinness expectancies at Wave 0 to being similar to the non-driven exercise group on those variables. Boys in the decreasing group did not differ from the high driven exercise group on pubertal status at the end of eighth grade (Wave 6). Table 4 summarizes these results.
Developmental Trajectories of Fasting
We again used Nagin's (2005) procedure to determine (a) whether individual differences in boys’ trajectories of fasting could be characterized in terms of subgroups and (b) what the number and shapes of the fasting trajectory groups were.
Fasting Trajectories: Selection of Trajectory Model
As noted above, we conducted trajectory analyses on six semi-annual time points. The 3-group solution produced BIC and AIC values that were less negative than those of the 2-group solution, but it included groups with very small samples sizes and did not involve groups with substantively different trajectories from those apparent in the 2-group solution. We therefore adopted a 2-group trajectory solution. The 2-group solution for fasting among boys had average group membership probabilities from .83 to .89. Thus, there was clear, straightforward assignment of individuals to trajectory groups.
Fasting Behavior Trajectories
As shown in Figure 1, bottom panel, 527 of the 631 boys reported little to no fasting behavior at each of the six semi-annual trajectory data collections spanning the period from the fall of sixth grade through the spring of eighth grade. We refer to this group as the non-fasting group. The rate of linear decrease for the non-fasting trajectory group was not statistically significant: t(526)=−1.74, p =.08. A group of 104 boys exhibited fasting behavior that was consistently high across the six measurement waves. We refer to this group as the fasting group. Thus, a substantial minority of boys who do not binge eat or purge consistently reported fasting for 8 or more hours to control their shape or weight. The rate of linear change for the fasting group was also not statistically significant: t(103)=−0.53, p = .60. Similar to the boys’ high driven exercise trajectory group, this finding indicates that this group of boys was engaging in fasting behavior by the fall of sixth grade (Wave 1) and engagement in the behavior neither increased nor decreased across the middle school years (Waves 1-6).
Prediction of Fasting Group Membership
At Wave 0 (spring of fifth grade), boys in the fasting group reported higher depressive symptom scores and stronger endorsement of the expectancy that thinness leads to overgeneralized life improvement than non-fasting boys. The two groups did not differ on the expectancy that eating helps alleviate negative affect or on pubertal status at Wave 0. Table 5 summarizes these results.
Table 5.
Fasting Trajectory Group Comparisons: Wave 0, spring of 5th grade and Wave 6, spring of 8th grade
| Fasting Trajectory Group Means (SD) | t- tests | |||
|---|---|---|---|---|
| Study Variable | Non-Fasting | Fasting | t | d |
| Depression- Wave 0 | 12.93 (7.14) | 16.93 (9.65) | 4.90** | 0.47 |
| Eating Expectancies- Wave 0 | 2.10 (1.23) | 2.24 (1.39) | 1.05 | 0.11 |
| Thinness Expectancies- Wave 0 | 2.85 (1.50) | 3.40 (1.71) | 3.33** | 0.34 |
| Depression- Wave 6 | 11.87 (6.79) | 17.00 (10.30) | 6.39** | 1.04 |
| Eating Expectancies- Wave 6 | 1.61 (0.96) | 1.66 (1.02) | 0.49 | 0.05 |
| Thinness Expectancies- Wave 6 | 2.07 (1.34) | 2.62 (1.84) | 3.58** | 0.34 |
| Non-Fasting | Fasting | x 2 | Φ | |
| Pubertal Status- Wave 0 | 19.9% | 31.6% | 0.90 | 0.04 |
| Pubertal Status- Wave 6 | 75.9% | 76.0% | 0.00 | 0.00 |
Note. N = 631; d is measure of effect size; Φ: phi coefficient, which is a measure of magnitude for chi-square.
*p < .01
p < .001
Fasting Group Comparisons at the End of the Trajectory Period
At Wave 6 (spring of eighth grade), boys in the fasting trajectory group continued to report higher depressive symptom scores and stronger endorsement of the expectancy that thinness leads to overgeneralized life improvement. As was true at Wave 0, boys did not differ on the expectancy that eating helps alleviate negative affect or on pubertal status at Wave 6. Table 5 summarizes these results.
Covariation between Fasting and Driven Exercise Trajectory Group Membership
We conducted chi-square analyses to determine the degree to which membership in a symptomatic group for one behavior covaried with membership in a symptomatic group for the other behavior. As shown in Table 6, membership in the two types of trajectory groups covaried: χ2 (2) = 16.16, p < .001, phi coefficient = .16. As the table shows, 57.6% of boys were in the non-driven exercise and non-fasting groups. Among the boys in the non-fasting trajectory group, 64.7% were in either the decreasing or non-driven exercise group. Of the 104 boys in the fasting group, more than half (53) were in a group that engaged in driven exercise during middle school. Of these 53 boys, 77% (41) were in the high driven exercise group.
Table 6.
Covariation Between Membership in Boys’ Fasting and Driven Exercise Trajectories
| Non-Fasting | Fasting | Total | |
|---|---|---|---|
| Non-Driven Exercise | 364 (57.6%) | 51 (8.1%) | 415 |
| Decreasing Driven Exercise | 45 (7.1%) | 12 (1.9%) | 57 |
| High Driven Exercise | 118 (18.7%) | 41 (6.5%) | 159 |
| Total | 527 | 104 | 631 |
We tested whether membership in trajectory groups characterized by both driven exercise and fasting was associated with greater dysfunction than was membership in a trajectory group characterized by just one of the two behaviors. We conducted a series of planned contrasts at Wave 6 (spring of eighth grade), comparing boys in both the high driven exercise and fasting groups to boys in (a) the high driven exercise but non-fasting group and (b) the fasting but decreasing or non-driven exercise groups. We found that boys in both the high driven exercise and fasting groups reported more depression symptoms than boys in the high driven exercise but non-fasting group, t(1, 625) = 3.94, p < .001. There were no differences between these two groups of boys for either expectancy. We found no differences in depression, eating expectancies, or thinness expectancies in the comparison between boys in the high driven exercise and fasting group and boys in the fasting but decreasing or non-driven exercise groups. Last, we compared boys in the fasting and decreasing driven exercise groups to boys in the fasting and high driven exercise groups. There were no differences between those groups in depression or either expectancy.
Discussion
The present study is the first to identify developmental trajectories for driven exercise and fasting behaviors in middle school boys. Further, this investigation is the first to reveal dysfunction associated with these behaviors in the absence of binge eating and purging. We found that (a) boys reported different trajectories of development of fasting and driven exercise throughout middle school; (b) membership in these trajectory groups could, in large part, be predicted by elementary school levels of depressive symptoms, expectancies for reinforcement from eating, expectancies for reinforcement from thinness, and, in some cases pubertal status; (c) membership in trajectory groups characterized by engagement in driven exercise or fasting was clearly associated with dysfunction; and (d) driven exercise and fasting covaried, such that engagement in one of the behaviors increased the likelihood that one was engaging in the other.
Concerning driven exercise, middle school did not appear to be a developmental period in which boys developed the tendency to engage in driven exercise; there was no group characterized by increases in the behavior. However, 216 boys reported frequent engagement in driven exercise to control weight at the start of the trajectory period, which was the beginning of sixth grade. Of those, 57 came to engage in the behavior less often over time, dropping to near zero levels by the end of eighth grade. Both those who decreased and those who maintained the behavior had elevated levels of depression, eating expectancies, and thinness expectancies, and were more likely to have experienced pubertal onset, compared to non-driven exercise boys in elementary school (6 months prior to the trajectory period). In addition, those two groups could not be distinguished in their risk profiles. Interestingly, by the end of eighth grade, the 57 boys who essentially stopped engaging in driven exercise had become significantly lower than the 159 boys who maintained driven exercise behavior in depressive symptoms and expectancy endorsement. In fact, they had become indistinguishable from the non-driven exercise group of boys. There were no differences among all three trajectory groups in pubertal status at the end of eighth grade.
It also appeared to be true that the middle school years were not a time in which boys developed fasting behavior. Rather, 104 boys reported already fasting by the start of sixth grade and continuing to engage in the behavior across the middle school years. Fifth grade endorsement of depression and expectancies for reinforcement from thinness predicted subsequent membership in the high fasting trajectory group. Pubertal status in fifth grade was not a predictor of fasting behavior as it was for driven exercise behavior, and there were no differences between the non-fasting and fasting groups on pubertal status at the end of the trajectory period, at the end of eighth grade.
Boys were already engaging in driven exercise and fasting behavior at the start of middle school. We infer that, for boys, the elementary school years are an important time for the development of nonpurging compensatory behaviors. This result is consistent with previous findings that boys tend to engage in other forms of eating disorder behavior as early as childhood and the beginning of adolescence (Pinhas et al., 2011). In the context of this apparent early onset, identification of a subgroup of boys who stopped engaging in one of the behaviors over the course of middle school is important. Research to determine how members of this group differed from boys who maintained engagement in nonpurging behaviors over this period may prove fruitful.
Engagement in nonpurging compensatory behaviors is associated with distress in middle school boys. Boys who reported high levels of driven exercise or fasting at the end of middle school had higher levels of depression, thinness expectancies, and eating expectancies than boys who did not engage in nonpurging compensatory behaviors. Thus, engagement in nonpurging compensatory behaviors by young boys merits the attention of both clinicians and researchers. Research to develop targeted prevention or intervention programs for elementary school boys is indicated.
With regard to pubertal status, our study is the first to show a relationship between early pubertal onset and early engagement in driven exercise among boys. Although the relationship between pubertal onset and eating disorder behaviors among girls is well established (Klump, 2013), other studies have failed to find a relationship between early pubertal onset and eating disorder symptoms in boys (Leon et al., 1995).
Endorsement of driven exercise and fasting co-varied. Over half the boys in the high fasting group also engaged in driven exercise, and more than half of those boys maintained both behaviors across the 3-year period. Given that previous studies have reported driven exercise and fasting to be the most common weight control behaviors reported by boys (Allen et al., 2013; Pisetsky et al., 2008), this co-occurrence may not be surprising. Perhaps boys are particularly at risk for syndromes characterized by both nonpurging compensatory behaviors. At the same time, it is important to note that the degree of co-variation was modest.
Driven exercise has been theorized as a gateway behavior to binge eating and purging by other investigators (Stiles-Shields et al., 2011). Unfortunately, our design does not permit a strong test of that possibility because our longitudinal window spanned only the 3 years of middle school. In girls, the average ages of the emergence of binge eating and purging are 16 and 18, respectively (le Grange & Loeb, 2007; Stice, Marti, & Rohde, 2013). If the same time window applies to boys, it would be necessary to follow boys through high school to determine whether those who engaged in driven exercise or fasting in middle school tended to binge and purge later in development.
It is important to note the limitations of this study. First, all risk and behavioral symptom data were self-reported by questionnaire. Although the measures used demonstrated good psychometric properties in this and previous studies of adolescents, face-to-face interviews provide the opportunity for clarification of terms, which may be particularly useful in a sample of youth. Second, we did not include a measure of body mass index (BMI). Although BMI did not discriminate between adolescents who did and did not engage in nonpurging compensatory behaviors in prior work (Stiles-Shields et al., 2011), we were not able to test this finding in the current study. In addition, the inclusion of BMI might also have clarified whether any of the participants were suffering from an established eating disorder (such as AN). However, the lifetime prevalence of AN in adolescent boys is below 1.0 per 100,000 persons per year (Hoek, 2006). Third, boys were asked to report engagement in the behaviors over the 2 weeks preceding the assessment. Although this procedure is the recommended one when using the EDE-Q in youth, it may lead to underestimates of engagement in the behaviors. Fourth, fasting was measured dichotomously. We cannot know if different patterns of fasting behavior would have been apparent had it been measured on an interval scale. Fifth, because boys more often report a desire for muscularity than girls (Cafri et al., 2005), thinness expectancies may not have completely captured boys’ body image expectancies. Sixth, we hypothesized that eating expectancies would predict nonpurging compensatory behaviors, but we did not investigate eating behavior as a mediator between expectancy endorsement and those behaviors. Seventh, because this study focused on risk and maintenance factors for nonpurging compensatory behaviors in the absence of binge eating and purging, it is a limitation of our study that we cannot know how binge eating effects the emergence and maintenance of nonpurging compensatory behaviors.
Adolescent boys appear to engage in nonpurging compensatory behaviors throughout middle school. While some boys discontinue engagement in driven exercise during these years, many continue to engage in this behavior, as well as fasting behavior. These behaviors are associated with depressive symptoms and maladaptive expectancies for reinforcement from eating and from thinness. Research to further understand these behaviors and their development in youth is needed to inform prevention and intervention efforts.
Acknowledgments
This research was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (NIAAA), R01 AA 016166.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
It is not yet clear why boys are more likely to engage in nonpurging compensatory behaviors rather than purging behaviors, such as self-induced vomiting and laxative use. Although important, this question was not addressed in the current study.
There are additional risk factors we could have studied. For example, this longitudinal data set did not include collection of body mass index (BMI), which might have been a useful predictor of driven exercise or fasting trajectories. Although BMI did not discriminate between adolescents who did and did not engage in nonpurging compensatory behavior in prior research (Stiles-Shields, Labuschagne, Golschmidt, Doyle, & Le Grange, 2012; Wade & O'shea, 2015), that prior sample included only 35 boys, and we could not replicate that finding in this larger sample. In addition, the current data set did not include the complete Eating Disorder Examination Questionnaire, so we could not assess if the scales of that measure add to the predictive power of depression, eating expectancies, and thinness expectancies.
All participants were invited to participate at each wave, even if they did not participate in the wave prior. For example, this includes Wave 0, in which 3% of consenting participants were absent or otherwise unable to participate in that wave. These participants were still invited to participate in future waves of the study.
References
- Allen KL, Crosby RD, Oddy WH, Byrne SM. Eating disorder symptom trajectories in adolescence: effects of time, participant sex, and early adolescent depressive symptoms. Journal of Eating Disorders. 2013;1:1–14. doi: 10.1186/2050-2974-1-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulik CM. Eating disorders in adolescents and young adults. Child and Adolescent Psychiatric Clinics of North America. 2002;11:201–218. doi: 10.1016/s1056-4993(01)00004-9. [DOI] [PubMed] [Google Scholar]
- Cafri G, Thompson JK, Ricciardelli L, McCabe M, Smolak L, Yesalis C. Pursuit of the muscular ideal: Physical and psychological consequences and putative risk factors. Clinical Psychology Review. 2005;25:215–239. doi: 10.1016/j.cpr.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Carter JC, Stewart DA, Fairburn CG. Eating disorder examination questionnaire: norms for young adolescent girls. Behaviour Research and Therapy. 2001;39:625–632. doi: 10.1016/s0005-7967(00)00033-4. [DOI] [PubMed] [Google Scholar]
- Clarke G, Debar L, Lynch F, Powell J, Gale J, O'Connor E, Hertert S. A randomized effectiveness trial of brief cognitive-behavioral therapy for depressed adolescents receiving antidepressant medication. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44:888–898. [PubMed] [Google Scholar]
- Coleman L, Coleman J. The measurement of puberty: a review. Journal of Adolescence. 2002;25:535–550. doi: 10.1006/jado.2002.0494. [DOI] [PubMed] [Google Scholar]
- Cooper MJ, Fairburn CG. Demographic and clinical correlates of selective information-processing in patients with bulimia nervosa. International Journal of Eating Disorders. 1993;13:109–116. doi: 10.1002/1098-108x(199301)13:1<109::aid-eat2260130113>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Cooper Z, Fairburn C. The eating disorder examination: A semi-structured interview for the assessment of the specific psychopathology of eating disorders. International Journal of Eating Disorders. 1987;6:1–8. [Google Scholar]
- Culbert KM, Burt SA, McGue M, Iacono WG, Klump KL. Puberty and the genetic diathesis of disordered eating attitudes and behaviors. Journal of Abnormal Psychology. 2009;118:788–796. doi: 10.1037/a0017207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis HA, Guller L, Smith GT. Developmental trajectories of fasting behavior and excessive exercise. Poster presented at the Eating Disorders Research Society meeting in San Diego, CA. 2014 Oct; [Google Scholar]
- Davis HA, Holland LA, Keel PK. A preliminary examination of a nonpurging compensatory eating disorder. International Journal of Eating Disorders. 2014;47:239–243. doi: 10.1002/eat.22191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day J, Schmidt U, Collier D, Perkins S, Van den Eynde F, Treasure J, Winn S, Robinson P, Murphy R, Keville S, Johnson-Sabine E, Jenkins M, Frost S, Dodge L, Berelowitz M, Eisler I. Risk factors, correlates, and markers in early- onset bulimia nervosa and EDNOS. International Journal of Eating Disorders. 2011;44:287–294. doi: 10.1002/eat.20803. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire?. International Journal of Eating Disorders. 1994;16:363–370. [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. Vol. 12. Guilford Press; New York: 1993. pp. 317–360. [Google Scholar]
- Ferreiro F, Wichstrøm L, Seoane G, Senra C. Reciprocal associations between depressive symptoms and disordered eating among adolescent girls and boys: A multiwave, prospective study. Journal of Abnormal Child Psychology. 2014;42:803–812. doi: 10.1007/s10802-013-9833-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godart NT, Perdereau F, Rein Z, Berthoz S, Wallier J, Jeammet P, Flament MF. Comorbidity studies of eating disorders and mood disorders. Critical review of the literature. Journal of Affective Disorders. 2007;97:37–49. doi: 10.1016/j.jad.2006.06.023. [DOI] [PubMed] [Google Scholar]
- Goldman MS, Brown SA, Christiansen BA, Smith GT. Alcoholism and memory: broadening the scope of alcohol-expectancy research. Psychological Bulletin. 1991;110:137–146. doi: 10.1037/0033-2909.110.1.137. [DOI] [PubMed] [Google Scholar]
- Hay PJ, Mond J, Buttner P, Darby A. Eating disorder behaviors are increasing: findings from two sequential community surveys in South Australia. PloS one. 2008;3:e1541. doi: 10.1371/journal.pone.0001541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoek HW. Incidence, prevalence and mortality of anorexia nervosa and other eating disorders. Current Opinion in Psychiatry. 2006;19:389–394. doi: 10.1097/01.yco.0000228759.95237.78. [DOI] [PubMed] [Google Scholar]
- Hohlstein LA, Smith GT, Atlas JG. An application of expectancy theory to eating disorders: Development and validation of measures of eating and dieting expectancies. Psychological Assessment. 1998;10:49–58. [Google Scholar]
- Klump KL. Puberty as a critical risk period for eating disorders: A review of human and animal studies. Hormones and Behavior. 2013;64:399–410. doi: 10.1016/j.yhbeh.2013.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Grange D, Loeb KL. Early identification and treatment of eating disorders: prodrome to syndrome. Early Intervention in Psychiatry. 2007;1:27–39. doi: 10.1111/j.1751-7893.2007.00007.x. [DOI] [PubMed] [Google Scholar]
- Leon GR, Fulkerson JA, Perry CL, Early-Zald MB. Prospective analysis of personality and behavioral vulnerabilities and gender influences in the later development of disordered eating. Journal of Abnormal Psychology. 1995;104:140–149. doi: 10.1037//0021-843x.104.1.140. [DOI] [PubMed] [Google Scholar]
- Little RJ, Rubin DB. The analysis of social science data with missing values. Sociological Methods & Research. 1989;18:292–326. [Google Scholar]
- MacBrayer EK, Smith GT, McCarthy DM, Demos S, Simmons J. The role of family of origin food-related experiences in bulimic symptomatology. International Journal of Eating Disorders. 2001;30:149–160. doi: 10.1002/eat.1067. [DOI] [PubMed] [Google Scholar]
- McCabe MP, Ricciardelli LA. Body image and body change techniques among young adolescent boys. European Eating Disorders Review. 2001;9:335–347. [Google Scholar]
- Miller WC, Anton HA, Townson AF. Measurement properties of the CESD scale among individuals with spinal cord injury. Spinal Cord. 2008;46:287–292. doi: 10.1038/sj.sc.3102127. [DOI] [PubMed] [Google Scholar]
- Mond JM, Hay PJ, Rodgers B, Owen C, Beumont PJV. Validity of the Eating Disorder Examination Questionnaire (EDE-Q) in screening for eating disorders in community samples. Behaviour Research and Therapy. 2004;42:551–567. doi: 10.1016/S0005-7967(03)00161-X. [DOI] [PubMed] [Google Scholar]
- Mond J, Hay P, Rodgers B, Owen C, Crosby R, Mitchell J. Use of extreme weight control behaviors with and without binge eating in a community sample: Implications for the classification of bulimic-type eating disorders. International Journal of Eating Disorders. 2006;39:294–302. doi: 10.1002/eat.20265. [DOI] [PubMed] [Google Scholar]
- Nagin DS. Group-based modeling of development. Harvard University Press; Cambridge, MA: 2005. [Google Scholar]
- Pearson CM, Combs JL, Smith GT. A risk model for disordered eating in late elementary school boys. Psychology of Addictive Behaviors. 2010;24:696–704. doi: 10.1037/a0020358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson CM, Combs JL, Zapolski TC, Smith GT. A longitudinal transactional risk model for early eating disorder onset. Journal of Abnormal Psychology. 2012;121:707–718. doi: 10.1037/a0027567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson CM, Wonderlich SA, Smith GT. A risk and maintenance model for bulimia nervosa: From impulsive action to compulsive behavior. Psychological Review. 2015;122:516–535. doi: 10.1037/a0039268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson CM, Zapolski TC, Smith GT. A longitudinal test of impulsivity and depression pathways to early binge eating onset. International Journal of Eating Disorders. 2015;48:230–237. doi: 10.1002/eat.22277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence. 1988;17:117–133. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Pinhas L, Morris A, Crosby RD, Katsman DK. Incidence and age-specific presentation of restrictive eating disorders in children: a Canadian Paediatric Surveillance Program study. Archives of Pediatric and Adolescent Medicine. 2011;165:895–899. doi: 10.1001/archpediatrics.2011.145. [DOI] [PubMed] [Google Scholar]
- Pisetsky EM, Chao YM, Dierker LC, May AM, Striegel-Moore RH. Disordered eating and substance use in high-school students: Results from the Youth Risk Behavior Surveillance System. International Journal of Eating Disorders. 2008;41:464–470. doi: 10.1002/eat.20520. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Ricciardelli LA, McCabe MP. Dietary restraint and negative affect as mediators of body dissatisfaction and bulimic behavior in adolescent girls and boys. Behaviour Research and Therapy. 2001;39:1317–1328. doi: 10.1016/s0005-7967(00)00097-8. [DOI] [PubMed] [Google Scholar]
- Rosen DS. Identification and management of eating disorders in children and adolescents. Pediatrics. 2010;126:1240–1253. doi: 10.1542/peds.2010-2821. [DOI] [PubMed] [Google Scholar]
- Sigel E. Eating disorders. Adolescent Medicine: State of the Art Reviews. 2008;19:547–572. [PubMed] [Google Scholar]
- Smith GT, Simmons JR, Flory K, Annus AM, Hill KK. Thinness and eating expectancies predict subsequent binge-eating and purging behavior among adolescent girls. Journal of Abnormal Psychology. 2007;116:188–197. doi: 10.1037/0021-843X.116.1.188. [DOI] [PubMed] [Google Scholar]
- Stice E, Marti CN, Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. Journal of Abnormal Psychology. 2013;122:445–457. doi: 10.1037/a0030679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiles-Shields EC, Goldschmidt AB, Boepple L, Glunz C, le Grange D. Driven exercise among treatment-seeking youth with eating disorders. Eating Behaviors. 2011;12:328–331. doi: 10.1016/j.eatbeh.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiles-Shields CE, Labuschagne Z, Goldschmidt AB, Doyle AC, le Grange D. The use of multiple methods of compensatory behaviors as an indicator of eating disorder severity in treatment-seeking youth. International Journal of Eating Disorders. 2012;45:704–710. doi: 10.1002/eat.22004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theim KR, Wilfley DE, Beach E, Tanofsky-Kraff M, Goldschmidt AB. Content of Children's Loss of Control Eating Episodes Assessed by Self-Report and Laboratory Test Meal. European Eating Disorders Review. 2014;22:72–76. doi: 10.1002/erv.2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin DL, Griffing A, Griffing S. An examination of subtype criteria for bulimia nervosa. International Journal of Eating Disorders. 1997;22:179–186. doi: 10.1002/(sici)1098-108x(199709)22:2<179::aid-eat10>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- Wade TD, O'Shea A. DSM-5 unspecified feeding and eating disorders in adolescents: What do they look like and are they clinically significant?. International Journal of Eating Disorders. 2015;48:367–374. doi: 10.1002/eat.22303. [DOI] [PubMed] [Google Scholar]