Abstract
Background
A reduction or cessation of fetal movements (FMs) is frequently reported by pregnant women resulting in anxiety and concern. Formal counting of FMs by the pregnant woman could possibly identify the fetuses at risk.
Methods
A prospective study was carried out over 500 booked cases after introducing daily fetal movement count (DFMC) Chart in the ninth month of pregnancy. Prior ultrasound (USG) was done in all cases. DFMC chart was used to record number of fetal movements perceived by patient for one hour after food (breakfast, lunch, dinner). Fetal movements were considered satisfactory if the count was three or more on each occasion.
Result
During the study period, no fetus was lost after introduction of DFMC chart in the 250 cases that were given DFMC chart and delivered in our hospital (Nil perinatal mortality). This was compared with 250 booked cases that were not given DFMC chart but had normal ultrasound done after completion of eight months of pregnancy and followed up. Five intrauterine deaths occurred in the ninth month in control group (2% perinatal mortality). In the DFMC chart group, 15 patients were admitted with decreased fetal movements. Out of these, 12 were discharged after monitoring for three days and three cases were delivered.
Conclusion
DFMC chart in ninth month of pregnancy helps in identifying at risk fetus in low risk pregnancies in absence of any other adverse factors necessitating early delivery.
Key Words: Daily fetal movements count chart (DFMC), Perinatal mortality, Intrauterine death
Introduction
The predominant goal of ante partum fetal monitoring is to reduce perinatal morbidity and mortality rates. At present, the beneficial effects of ante partum testing have created a situation in which the likelihood of fetal death in high-risk, tested populations is lower than that in low-risk, untested populations. This paradox has forced us to consider the option of routine ante partum monitoring in all pregnancies.
Various methods have been described to quantify the fetal movements to predict fetal well-being, which include use of a cardiotocograph, visualization with real time ultrasound and maternal subjective perceptions. Most investigators have reported excellent correlation between maternally perceived fetal motion and movement documented by instrumentation. Although several fetal movement counting protocols have been used, neither the optimal number of movements nor the ideal duration of counting them has been defined. A particularly bothersome clinical situation occurs when women present in the third trimester with a chief complaint of subjectively reduced fetal movement [1]. Harrington et al [2] reported that 7% of 6793 women delivered at a London Hospital presented with a complaint of decreased fetal movement. Others have concluded that informal maternal perceptions were as good as formally counted and recorded fetal movement but the evidence of a clinical benefit is limited [3].
Material and Methods
The study group of 250 pregnant women underwent ultrasonography (USG) study and then they were given daily fetal movements count (DFMC) charts (Fig. 1) at the end of eight months of pregnancy. They were given routine antenatal care and delivered at term. Their outcome was compared with the control group of 250 pregnancies who were not given DFMC charts after USG screening. The patients who reported with loss of or reduced fetal movements were admitted and observed. Reduced fetal movement was defined as less than three fetal movements in one hour after taking food.
Fig. 1.
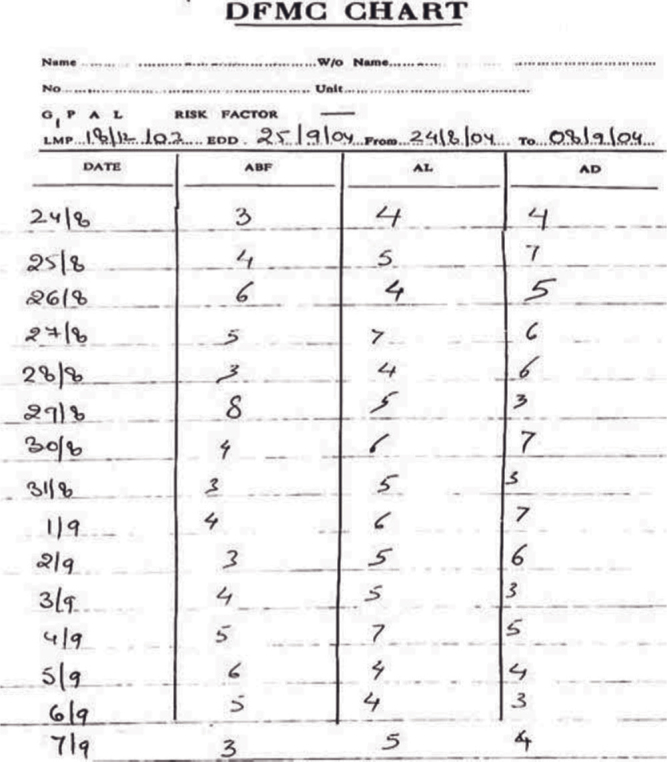
DFMC chart
Results
Out of the 250 patients in the study group (DFMC group), 15 were admitted for loss of fetal movements. They were screened by USG and nonstress test (NST) and 12 were discharged after they started having satisfactory fetal movements. Three patients had persistent reduced fetal movements and they were delivered vaginally.
Out of the control group, eight patients were admitted with loss of fetal movements in ninth month though they had a normal ultrasound scan at completion of eight months of pregnancy. Of these five (2%) had intrauterine fetal death. Other three cases were screened by USG and NST. They were discharged after having satisfactory fetal movements (Table 1).
Table 1.
Number of intrauterine deaths and admissions for loss of fetal movements in study and control group
| DFMC chart group n=250 | Control group n=250 | Chi Square value | p value | |
|---|---|---|---|---|
| Intrauterine deaths | 0.0 | 5 (2.00%) | 5.0505 | < 0.025** |
| Admissions with loss of fetal movements | 15 (6.0%) | 8 (3.20%) | 2.2331 | < 0.2 |
| No of mothers with live fetuses with loss of movements | 15 (6.0%) | 3 (1.20%) | 8.0530 | < 0.01** |
Significant
The results for intrauterine deaths were statistically analyzed using chi square test and the difference was found to be significant at the value of p<0.025. The difference between number of admissions for loss of fetal movements was statistically insignificant. However, it was statistically significant (p<0.01) if number of pregnancies with live babies, reporting with loss of fetal movements were considered.
Discussion
Maternal perception of fetal movement is an inexpensive, noninvasive method of assessing fetal well-being. Monitoring fetal movement serves as an indirect measure of central nervous system integrity and function. Short-term observations of the fetus are best performed using real-time ultrasound imaging or Doppler ultrasound [4]. For home monitoring daily fetal kick count may be required. Advocating the use of DFMC chart requires counseling for awareness. Kick count or mild flicker can be explained along with variation due to muscle spasm in winter and liquor quantity.
A healthy fetus should move approximately three to five times within one hour. An alternative method is the Cardiff Count-to-Ten chart, whereby the patient records fetal movements during the course of usual daily activity. A period of 12 hours without at least 10 perceived movements is considered a warning signal [6]. If the test result is not reassuring, the patient should be evaluated with NST and USG [4].
In this study, we found that fetal mortality reduced from 20.4 per 1000 live births in control group to nil in study group. Though this was a small study, the results are statistically significant. It is clear that complaints of decreased fetal movement are significant and warrant further evaluation [6]. The Society of Obstetrician and Gynecologists of Canada has recommended that DFMC could be used in cases identified to be at risk for fetal asphyxia [7].
Conflicts of Interest
None identified
Intellectual Contribution of Authors
Study Concept : Lt Col G Singh
Drafting & Manuscript Revision : Lt Col G Singh, Maj K Sidhu
Study Supervision : Lt Col G Singh
References
- 1.Yogev Y, Ben-Haroush A, Horowitz ER, Chen R, Hod M, Kaplan B. PGE2 induction of labor for consistent decreased perception of fetal movements at term. Int J Gynaecol Obstet. 2003;82:173–178. doi: 10.1016/s0020-7292(03)00197-8. [DOI] [PubMed] [Google Scholar]
- 2.Harrington K, Thompson O, Jorden L. Obstetric outcome in women who present with reduction in fetal movements in third trimester of pregnancy. J Perinat Med. 1998;26:77. doi: 10.1515/jpme.1998.26.2.77. [DOI] [PubMed] [Google Scholar]
- 3.Olesen AG, Svare JA. Decreased fetal movements: background, assessment, and clinical management. Acta Obstet Gynecol Scand. 2004;83:818–826. doi: 10.1111/j.0001-6349.2004.00603.x. [DOI] [PubMed] [Google Scholar]
- 4.Christensen FC, Rayburn WF. Fetal movement counts. Obstet Gynecol Clin North Am. 1999;26:607–621. doi: 10.1016/s0889-8545(05)70102-9. [DOI] [PubMed] [Google Scholar]
- 6.Sergent F, Lefevre A, Verspyck E, Marpeau L. Decreased fetal movements in the third trimester: what to do? Gynecol Obstet Fertil. 2005;33:861–869. doi: 10.1016/j.gyobfe.2005.07.041. [DOI] [PubMed] [Google Scholar]
- 7.Davies Gregory AL. Antenatal fetal assessment. J Soc Obstet Gynaecol Can. 2000;22:456–462. [Google Scholar]
Uncited Reference
- 5.Froen JF. A kick from within-fetal movement counting and the cancelled progress in antenatal care. J Perinat Med. 2004;32:13–24. doi: 10.1515/JPM.2004.003. [DOI] [PubMed] [Google Scholar]


