Introduction
Bowing of tibia refers to bending of diaphysis with apex of curve directed anterolaterally, anteromedially or posteromedially. Posteromedial bowing of tibia is a congenital condition often associated with calcaneovalgus deformity of ipsilateral foot. This condition undergoes spontaneous resolution to a major extent, often leaving only leg length inequality. The latter may result in abnormal gait and backache. We present a rare case of unilateral posteromedial bowing of tibia.
Case Report
A five day old male child with dorsiflexion of left foot underwent radiological examination of left leg. No other abnormality was detected clinically in the body. The mother was G2P2A0. Record of single antenatal ultrasound examination done at the periphery in the ninth month was not available but according to mother, it was unremarkable. The child was delivered vaginally at the primary health centre with no history of obstructed labor. The other child was normal. No history of similar deformity was elicited on maternal or paternal side.
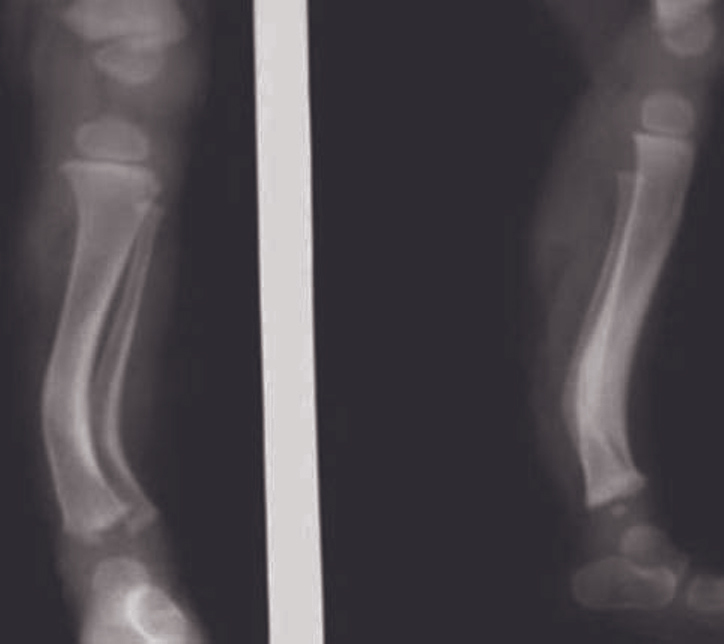
Radiographs of left leg were taken in the AP and lateral projection (foot was manually plantar flexed). It revealed bowing of tibia and fibula with the apex of curve directed posteromedially. Cortical thickening with narrowing of the medullary cavity on the concave side of the curve was evident (Fig. 1). Based on the clinicoradiologic findings, the diagnosis of prenatal bowing of tibia and fibula was made.
Fig. 1.

An AP and lateral radiograph of left leg (with manual plantar flexion of foot) at 5-days show posteromedial bowing of tibia and fibula with thickening of cortex on inner side of curve with narrowing of medullary cavity
Plaster cast was applied to left leg and foot in plantar flexed position (similar to normal foot) for six months with intermittent clinical examinations and plaster-release for few days to ensure correction of deformity and no complication arises. By six months, dorsiflexion abnormality was minimal and radiograph of left leg revealed reduction in bowing of tibia and fibula (Fig. 2). Further radiographs taken at the end of first and second years revealed further reduction in bowing and sclerosis. By second year, dorsiflexion of left foot was completely corrected clinically. Radiographs at five year revealed near-complete disappearance of the tibial and fibular bowing, however, the shortening of the left tibia was noted relative to the right side by 2.6 cm (Fig. 3). There was no abnormality of the foot. The child was using a shoe lift for proper walking. However, there was noticeable reduction in the muscle mass on the left side.
Fig. 2.
An AP and lateral radiograph of the left leg (at six months) shows reduction in the posteromedial bowing and thickening of the cortex of tibia and fibula
Fig. 3.

An AP radiograph of the both legs (at five years) shows minimal medial bowing and thickening of the cortex of tibia and fibula with significant shortening of left leg length
Discussion
Tibial bowing refers to bending of tibial shaft, major causes of which are congenital, fibular hypoplasia, pseudoarthrosis of tibia, Blount's disease and miscellaneous (physiological, rickets, osteogenesis imperfecta, fibrous dysplasia, post-traumatic).
Posteromedial bowing, a congenital anomaly with associated calcaneovalgus deformity is an infrequent disorder mostly identified after birth [1]. Few cases of prenatal detection have been reported [2]. If detected antenatally, the sonologist should record position, movement and shortening of affected limb and compare subsequently. Major part of this deformity resolves spontaneously and ultimately limb length discrepancy persists that may require treatment [3]. Calcaneovalgus deformity is seen as an ipsilateral dorsiflexed foot touching the shin. A skin dimple on the posterior aspect of the curve is seen clinically in tibial bowing [4]. Most authors believe that cramped fetal positioning, with the dorsiflexed foot plastered against the anterior aspect of the tibia is responsible for the deformity, hence known as prenatal bowing of tibia and fibula [5].
Shortening of affected limb by 3-4 cm is usual. This is treated by shoe lift or shoe built up. Inequalities > 5 cm usually require foot-in foot prosthesis or surgical correction. Surgical procedures target either retarding growth of normal limb by epiphysiodesis (typically 11 years in females and 13 years in males) or accelerating the growth of short limb by Ilizarov's technique. Calcaneovalgus deformity resolves spontaneously within two years but splinting, casting or stretching of the affected foot can accelerate resolution. Some degree of tibial torsion and muscular atrophy may persist. Thorough clinical and radiological examination helps in the differential diagnosis. Metabolic diseases like rickets and osteogenesis imperfecta are associated with findings elsewhere while in focal diseases like fibrous dysplasia, the cause is usually evident.
Anteromedial bowing is associated with congenital absence or severe hypoplasia of fibula, equinovalgus deformity, absence of lateral rays of foot, tarsal aplasia or fusion and shortening of ipsilateral femur [6]. Anterolateral bowing is often associated with a pseudoarthrosis of the tibia or von Recklinghausen's neurofibromatosis. In about 40% cases, family history is present. Anterior bowing with dysplastic-sclerotic bone changes results in the “high risk tibia” [7]. If associated with ipsilateral polydactyly of great toe, spontaneous resolution without progression to pseudoarthrosis is seen [8]. Lateral bowing is also associated with Melnick-Needles syndrome, characterized by small face, large ears, protruding eyes, micrognathia, short arms and narrow thorax. The cortex of tubular bones is undulating with multiple constrictions in medullary cavity, sclerosis of skull and mastoid bones with small anterior cranial fossa [9]. Blount's disease (tibia vara) is a local growth disturbance in the medial aspect of the proximal tibial epiphysis. The infantile type is seldom evident before two years of age while adolescent type appears between 8-12 years of age [10].
To summarize, congenital bowing of tibia and fibula is a benign and easily differentiable condition that corrects with subsequent growth leaving limb shortening.
Conflicts of Interest
None identified
References
- 1.Maio FD, Corsi A, Roggini M, Riminucci M, Bianco P, Ippolito E. Congenital unilateral posteromedial bowing of the tibia and fibula: Insights regarding pathogenesis from prenatal pathology. A case report. The Journal of Bone and Joint Surgery (American) 2005;87:1601–1605. doi: 10.2106/JBJS.D.02551. [DOI] [PubMed] [Google Scholar]
- 2.Zollinger PE, Wessels MW, Wladimiroff JW, Diepstraten AFM. Prenatal ultrasonographic diagnosis of posteromedial bowing of the leg: Two case reports. Ultrasound in Obstetrics and Gynecology. 2000;15:150–153. doi: 10.1046/j.1469-0705.2000.00048.x. [DOI] [PubMed] [Google Scholar]
- 3.Hofmann A, Wenger DR. Posteromedial bowing of the tibia. Progression of discrepancy in leg lengths. J Bone Joint Surg Am. 1981;63:384–388. [PubMed] [Google Scholar]
- 4.Pappas AM. Congenital posteromedial bowing of the tibia and fibula. J Pediatr Orthop. 1984;4:525–531. [PubMed] [Google Scholar]
- 5.Silverman FN. Congenital malformations. In: Silverman FN, Kuhn JP, editors. Caffey's Pediatric X-Ray Diagnosis: An Integrated Imaging Approach. 9th ed. Mosby; 1993. pp. 1547–1548. [Google Scholar]
- 6.Resnick D, Kransdorf MJ. Additional congenital or heritable anomalies and syndromes. In: Resnick D, Kransdorf MJ, editors. Bone and Joint Imaging. 3rd ed. Elsevier Saunders; 2005. p. 1338. [Google Scholar]
- 7.Hofmann P, Galanski M. Congenital bowing of the tibia in neurofibromatosis von Recklinghausen (author's transl) Rofo. 1976;125:417–421. doi: 10.1055/s-0029-1230491. [DOI] [PubMed] [Google Scholar]
- 8.Kitoh H, Nogami H, Hattori T. Congenital anterolateral bowing of tibia with ipsilateral polydactyly of the great toe. American Journal of Medical Genetics (online) 1998;73:404–407. [PubMed] [Google Scholar]
- 9.McAlister WH, Herman TE. Osteochondrodysplasias, Dysostoses, Chromosomal Aberrations, Mucopolysaccharidoses and Mucolipidoses. In: Resnick D, Kransdorf MJ, editors. Bone and Joint Imaging. 3rd ed. Elsevier Saunders; 2005. p. 1308. [Google Scholar]
- 10.Resnick D, Kransdorf MJ. Osteochondoses. In: Resnick D, Kransdorf MJ, editors. Bone and Joint Imaging. 3rd ed. Elsevier Saunders; 2005. pp. 1100–1101. [Google Scholar]


