Introduction
Cervical tuberculosis accounts for 0.1-0.65% of all cases of tuberculosis (TB) [1]. Tuberculosis more frequently affects the upper genital tract-namely, the fallopian tubes and endometrium [2]. TB of the cervix is present in about 5% of the cases [3]. We present such a case due to the rarity of this condition and that it clinically mimics carcinoma of cervix.
Case Report
A 50 year old Para 5 lady, menopausal for 10 years reported to the gynaecological outpatient department with history of gradually increasing, white coloured, foul smelling discharge per vaginum since last two months. There was no history of bleeding per vaginum, itching or any local lesion. She gave history of mass descending per vaginum. There was no history of any bowel or bladder disturbance. She gave no history of weight loss, fever, night sweats, exposure to tuberculosis or past history of tuberculosis. On examination, she was thinly built, averagely nourished weighing 45 kg. General examination was normal with no evidence of pallor or lymphadenopathy. Per abdomen examination was normal with no organomegaly.
Speculum examination revealed an unhealthy looking cervix which was grossly erythematous, congested and bled on touch (Fig.1). There was no hypertrophy, growth or ulceration. There was white colored discharge which was foul smelling. Grade II / IV uterovaginal prolapse with cystocoele was present. No stress urinary incontinence was demonstrable. Vaginal walls were clinically healthy. Vaginal examination revealed a normal sized retroverted uterus which was freely mobile. There was no adnexal mass or forniceal tenderness.
Fig. 1.

Photograph of cervix prior to treatment.
Laboratory investigations revealed a raised ESR of 35 mm fall in first hour and positive Mantoux test (23 mm). All other hematological and biochemical parameters were normal. Chest radiograph was normal. Pap smear showed cytology suggestive of granulomatous cervicitis suspicious of being tubercular in nature (Fig. 2). Cervical and endometrial biopsies were done which confirmed tuberculosis of cervix and endometrium respectively (Fig. 3, Fig. 4). Scanned acid fast bacilli were found on microscopy. Special staining for fungus was carried out which was negative. Based on this diagnosis patient was put on four drugs anti tubercular therapy according to Directly Observed Treatment Schedule (DOTS). Patient remained under regular follow up and was compliant with her treatment.
Fig. 2.

Photograph of Pap smear showing granulomas with slipper shaped nuclei and peripheral lymphocytic infiltration.
Fig. 3.

Medium power view showing pale epithelioid granulomas with Langhans’ giant cells (arrow) and surrounding lymphocytic infiltrations (blue areas).
Fig. 4.
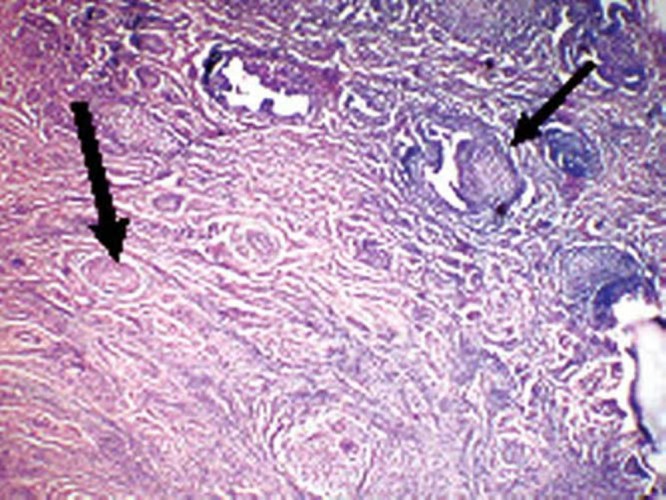
Scanner view showing endocervical glands (thin arrow) and discrete granulomas (thick arrow).
Discussion
Tuberculosis of the upper genital tract is a rare disease. Pelvic tuberculosis is produced primarily by Mycobacterium tuberculosis or Mycobacterium bovis. Pelvic organs are infected from a primary focus, usually the chest, by hematogenous spread. The cervix is infected as part of this process, by lymphatic spread or by direct extension. In rare cases, cervical TB may be a primary infection, introduced by a partner with tuberculosis epididymitisor other genitourinary disease. Sputum, used as a sexual lubricant, may also be a route of transmission [2].
Symptomatic genital tuberculosis can present with abnormal vaginal bleeding, menstrual irregularities, abdominal pain, and constitutional symptoms [4]. The macroscopic findings of papillary or vegetative growths, a miliary appearance, and ulceration may be misinterpreted as invasive cancer of cervix. Microscopically caseating granulomas are diagnostic but are also found in amoebiasis, schistosomiasis, brucellosis, tularemia, sarcoidosis, and foreign body reaction [1].
The diagnosis of cervical TB is usually made by histological examination of a cervical biopsy specimen. Staining for acid fast bacilli may not be very useful in making a diagnosis [5]. Although isolation of mycobacterium is the gold standard for diagnosis, but one third of cases are culture negative, therefore presence of typical granulomata is sufficient for diagnosis if other causes of granulomatous cervicitis are excluded. Newer modalities of diagnosis like ELISA can aid in the diagnosis [1].
The incidence of TB has increased recently and is partly attributable to the HIV pandemic. Therefore an abnormal cervical appearance, should invite high index of suspicion for tuberculosis.
Conflicts of Interest
None identified
References
- 1.Lamba H, Byrne M, Goldin R, Jenkins C. Tuberculosis of the cervix: Case presentation and a review of the literature. Sex Transm Inf. 2002;78:63–66. doi: 10.1136/sti.78.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chowdhury NNR. Overview of tuberculosis of the female genital tract. J Indian Med Assoc. 1996;94:345–361. [PubMed] [Google Scholar]
- 3.Rock JA, Jones HW, editors. Te Linde's Operative Gynaecology. 9th ed. Lippincot Williams & Wilkins; 2003. pp. 697–698. [Google Scholar]
- 4.Carter J, Peat B, Dalrymple C. Cervical tuberculosis – case report. Aust NZ J Obstet Gynaecol. 1989;29:270–271. doi: 10.1111/j.1479-828x.1989.tb01739.x. [DOI] [PubMed] [Google Scholar]
- 5.Agarwal J, Gupta JK. Female genital tuberculosis – A retrospective clinico-pathologic study of 501 cases. Indian J Pathol Microbiol. 1993;36:389–397. [PubMed] [Google Scholar]


