Abstract
Background
The surgical treatment of adult anterior urethral strictures is constantly evolving. Controversy exists over the best means of reconstructing the anterior urethra.
Methods
Twelve patients underwent buccal mucosal urethroplasty for long segment anterior urethral stricture between 2003 and 2005 . Eleven patients with a salvageable urethral plate were treated with one stage dorsal onlay urethroplasty, using a perineal or circumcoronal incision. One patient with a severely scarred urethral plate underwent two-stage urethroplasty.
Results
At a mean follow up of 14.2 months (range 2 to 26) one (8.3%) patient had short recurrent stricture, which was treated with optical urethrotomy. The mean maximal urine flow rate improved from 8.3 ml/sec to 18.1 ml/sec after the surgery. There were no donor site complications. All patients had a normal slit like meatus and none had chordee or erectile dysfunction.
Conclusion
In long stricture of anterior urethra, dorsal onlay buccal mucosa urethroplasty provides excellent intermediate term results with a normal, wide caliber urethra.
Key Words: Stricture urethra, Buccal mucosa urethroplasty
Introduction
The surgical treatment of adult anterior urethral strictures is constantly evolving. However in recent times there has been a wider use of buccal mucosal graft versus other substitutes such as genital or extragenital skin. We present our experience of dorsal onlay urethroplasty using buccal mucosal graft in long segment stricture of the anterior urethra.
Material and Methods
It is a prospective study, involving 12 patients of long stricture of the anterior urethra who underwent buccal mucosa graft dorsal onlay urethroplasties between 2003 and 2005. Preoperatively, demographic data and clinical features were recorded. Uroflowmetry was done in patients who were not in retention. Retrograde urethrogram (RGU) and micturiting cysto-urethrogram (MCU) were obtained in all patients (Figs. 1,2). All patients underwent dorsal onlay buccal mucosa urethroplasty, nine by Barbagli's technique, two by ventral saggital urethrotomy approach and one underwent two staged procedure. The Barbagli's technique involved mobilisation of strictured urethra through perineal approach, dorsal splitting of the diseased urethra, placement of prepared graft on perineal cavernosal bed, fixing of graft by quilting sutures and suturing of graft edges to urethral edges with 4/0 vicryl over a 16 Fr silicone catheter [1]. The ventral saggital urethrotomy involved degloving of penis from circumcoronal part to the root of penis at the level of Buck's fascia, ventral saggital urethrotomy, incision of dorsal urethra in the mid line through the strictured area, suturing of buccal mucosa strip in dorsal urethrotomy using 4/0 vicryl and giving few quilting sutures to fix the graft in its bed and closure of urethra over a 16 Fr silicone catheter. A 1-1.5 cm strip of buccal mucosa was harvested after sub mucosal injection of 1:1,00,000 adrenaline, to facilitate dissection and reduce bleeding. Subdermal fat was removed and the graft trimmed to size and fenestrated. The catheter was left in place for 2-3 weeks. Post operatively, at least one uroflowmetry, urine culture and retrograde urethrography was done in all patients and they were followed up at six monthly intervals. Thereafter the retrograde urethrography was only repeated if the symptoms or a deteriorating flow rate suggested a recurrent stricture.
Fig 3.
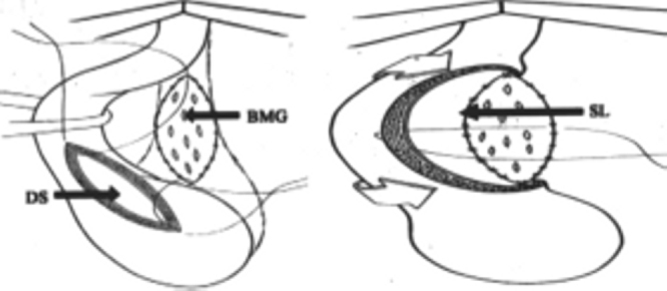
Sketches showing steps in Barbagli's technique of Dorsal Onlay Bucccal Mucosa Graft Urethroplasty. (BMG: Buccal Mucosa Graft, DS: Dorsal Slit in Bulbar Urethra Through strictured portion, SL: Suture Line between Buccal Mucosa Patch and edge of split open bulbar uretha)
Fig 1.
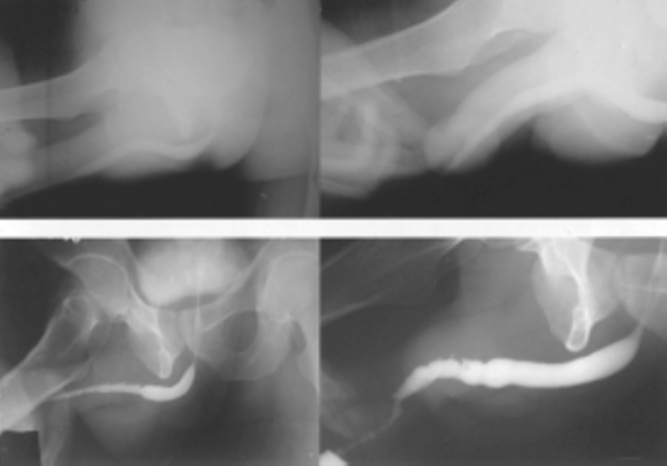
Pre operative (left) and post operative (right) retrograde urethrograms (RGUs) of two patients with long strictures of penile urethra showign marked improvement in caliber of penile urethra
Fig 2.
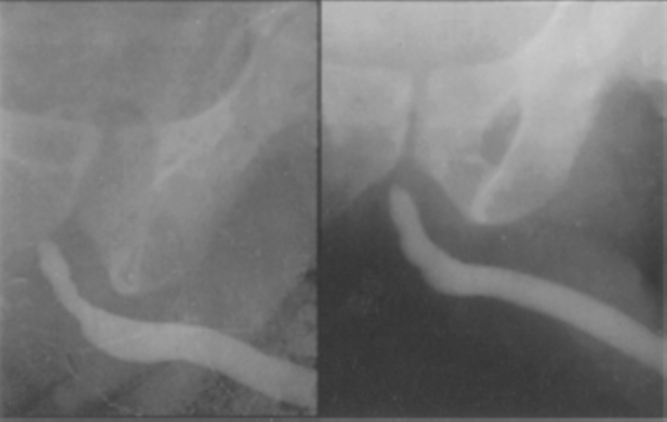
Preoperative and postoperative retograde urethrograms showing significant increase in caliber of lumen of bulbar urethra following Barbagli's technique of dorsal onlay buccal mucosa graft urethroplasty
Results
A total of 12 patients were included in this study. The mean age of these men was 38.9 years (range17-58 years). The mean duration of symptoms was 5.6 months (range 1-14 months). Nine (75%) patients presented with weak urinary stream and three (25%) had retention of urine with a suprapubic cystostomy (SPC) in situ. The mean maximum urinary flow rate (Q max) among the patients who were not on SPC was 8.3 ml/sec (range 6.4–10.1 ml/sec). The mean length of the stricture was 10.1 cm (range 6-18cm). Only bulbar urethra was involved in two (16.7 %) while the stricture was pendular and bulbopendular in six (50%) and four (33.3 %) cases respectively. The meatus was involved in four (33.3 %) patients. Inflammation was the commonest aetiology of the stricture (Table 1).
Table 1.
Distribution of the urethral strictures in terms of location and aetiology
| Pendular | Bulbopendular | Bulbar | |
|---|---|---|---|
| Inflammatory | 4 | 2 | 1 |
| Traumatic | 1 | 1 | 1 |
| Ischaemic | 0 | 1 | 0 |
| Idiopathic | 1 | 0 | 0 |
Single stage urethroplasty was done in 11 cases while one patient underwent a two-stage procedure. The approach was perineal in nine (for Barbagli's technique) while a circumcoronal incision with degloving of the penis at the level of Buck's fascia was done in two cases (for ventral saggital urethrotomy approach). In two-stage procedure, the first stage involved opening of urethra ventrally from the meatus through the strictured part of the urethra, excision of unhealthy urethral mucosa and replacement by a 2.5 cm wide buccal mucosa strip. The second stage involved tubularisation of the grafted buccal mucosa after three months over a 16 Fr silicone Foley's catheter.
The mean follow up period was 14.2 months (range 2-26 months) and the procedure was successful with no indication for a secondary procedure in 11 (91.7%) cases. The mean maximum urinary flow rate (Qmax) in this group was 18.1 ml/ sec (range 14.2–24.5 ml/sec). Re-stricture was defined as the development of symptoms suggesting recurrent obstruction which is confirmed by RGU/MCU. One patient developed recurrence of stricture at proximal anastomotic site requiring an internal urethrotomy. The other complications recorded are shown in Table 2. No major donor site complications were noted. Patients could take cold liquids same evening and soft diet after 24 hours.
Table 2.
The significant complications in the study group. The only case with fistula closed spontaneously on conservative management
| Complications | Number of patients |
|---|---|
| Wound infection | 2 |
| Fistula | 1 |
| Post void dribble | 2 |
| Ejaculatory dysfunction | 2 |
Discussion
In adult male patients, the urethral stricture of the anterior urethra may be inflammatory, traumatic, ischaemic, iatrogenic or idiopathic in origin. A long segment stricture of the anterior urethra continues to be a challenge for the reconstructive urologist. The best approach in such cases is a substitution urethroplasty [2]. A number of techniques using various candidate tissues have evolved to deal with this problem. These include split skin and full thickness grafts, bladder mucosa, buccal mucosa and now tissue engineered substitutes available over the shelf. Initially, scrotal skin was used but fell into disfavour because of high rate of complications. Similarly, after the initial enthusiasm with the bladder mucosa as a urethral substitute there were problems with harvesting tissue for substitution and of meatal exuberance [3].
Buccal mucosa grafts (BMG) are emerging as new gold standard in the treatment of long segment stricture urethra [4]. The BMG appears to be the most versatile urethral substitute, as it can be successfully used for both one and two stage reconstruction [5]. The dorsal placement of BMG results in better outcome than ventral patch as the corporeal bodies have an excellent blood supply and good mechanical support. Also the spreading of the graft, making use of the tensile strength in the corporeal bodies reduces the risk of graft shrinkage and chordee [6]. The success rate for dorsal onlay buccal mucosa graft is reported to be 96-100%, that is comparable to our experience (Table 3). Buccal mucosa graft has an advantage over skin flaps or other grafts, in that they are easier and quicker to harvest and leave no genital scars. In addition buccal mucosa grafts are resistant to infectious skin conditions such as Balanitis Xerotica Obliterans (BXO). Oral complications after buccal mucosal graft harvest for urethroplasty are infrequent and mild in nature [7].
Table 3.
The outcome in this study in comparison to the other major series reported in the literature
Ventral sagittal urethrotomy approach for dorsal free graft urethroplasty as described by Asopa et al [8], which we performed in the last two cases is easy. Another Indian study [9], found dorsal buccal mucosa graft urethroplasty via a minimal access perineal approach did not require urethral dissection and mobilization thus preserving the blood supply.
Buccal mucosa is receiving increased attention in the urological literature for penile and bulbar urethroplasty [10]. The advantages of buccal mucosa include ease of harvesting, superior donor site cosmesis, resilience to infections and better long-term stability [11]. The skin flap urethroplasty has a significantly higher rate of urinary tract infection and pouch formation as compared to buccal mucosa graft urethroplasty [12].
Conflicts of Interest
None identified
References
- 1.Barbagli G, Palminteri E, Guazzoni G, Cavalcanti A. Bulbar urethroplasty using the dorsal approach: current techniques. Int Braz J Urol. 2003;29:155–161. doi: 10.1590/s1677-55382003000200012. [DOI] [PubMed] [Google Scholar]
- 2.Andrich DE, Leach CJ, Mundy AR. The Barbagli procedure gives the best results for patch urethroplasty of the bulbar urethra. Br J Urol. 2001;88:185–189. doi: 10.1046/j.1464-410x.2001.02344.x. [DOI] [PubMed] [Google Scholar]
- 3.Bhargava S. Tissue-engineered buccal mucosa for substitution urethroplasty. BJU Int. 2004;93:807–811. doi: 10.1111/j.1464-410X.2003.04723.x. [DOI] [PubMed] [Google Scholar]
- 4.Bhargava S, Chapple CR. Buccal Mucosa urethroplasty: Is it the new gold standard? Br J Urol. 2004:1191–1193. doi: 10.1111/j.1464-410X.2003.04860.x. [DOI] [PubMed] [Google Scholar]
- 5.Dubey D, Kumar A, Srivastava A, Kapoor R, Bhandari M. Buccal Mucosa Urethroplasty: a versatile technique for all urethral segments. BJU. 2005;95:625–629. doi: 10.1111/j.1464-410X.2005.05352.x. [DOI] [PubMed] [Google Scholar]
- 6.Barbagli G, Palminteri E, Rizzo M. Dorsal onlay graft urethroplasty using penile skin or buccal mucosa in adult bulbo- urethral strictures. J Urol. 1998;160:1307–1309. [PubMed] [Google Scholar]
- 7.Dublin N, Stewart LH. Oral complications after buccal mucosal graft harvest for urethroplasty. BJU Int. 2004;94:867–869. doi: 10.1111/j.1464-410X.2004.05048.x. [DOI] [PubMed] [Google Scholar]
- 8.Asopa HS, Garg M, Singhal GG, Singh L, Asopa J, Nischal A. Dorsal free graft urethroplasty for urethral stricture by ventral sagittal urethrotomy approach. Urology. 2001;58:657–659. doi: 10.1016/s0090-4295(01)01377-2. [DOI] [PubMed] [Google Scholar]
- 9.Gupta NP, Ansari MS, Dogra PN, Tandon S. Dorsal buccal mucosal graft urethroplasty by a ventral sagittal urethrotomy and minimal-access perineal approach for anterior urethral stricture. BJU Int. 2004;93:1287–1290. doi: 10.1111/j.1464-410X.2004.04822.x. [DOI] [PubMed] [Google Scholar]
- 10.Barbagli G. When and how to use buccal mucosa grafts in penile and bulbar urethroplasty. Minerva Urol Nefrol. 2004;56:189–203. [PubMed] [Google Scholar]
- 11.Andrich DE, Mundy AR. Urethral strictures and their surgical management. Br J Urol. 2000;86:571–580. doi: 10.1046/j.1464-410x.2000.00878.x. [DOI] [PubMed] [Google Scholar]
- 12.Mundy AR. The long-term results of skin inlay urethroplasty. Br J Urol. 1995;75:59–61. doi: 10.1111/j.1464-410x.1995.tb07233.x. [DOI] [PubMed] [Google Scholar]
- 13.Rosenstein DI, Jordan GH. Dorsal onlay graft urethroplasty using buccal mucosa in bulbar urethral reconstruction. J Urol. 2002;167:16. [Google Scholar]
- 14.Pansodoro V, Emiliozzi P, Gaffi M. Buccal mucosa urethroplasty in the treatment of bulbar urethral strictures. Urology. 2003;61:1008–1010. doi: 10.1016/s0090-4295(02)02585-2. [DOI] [PubMed] [Google Scholar]


