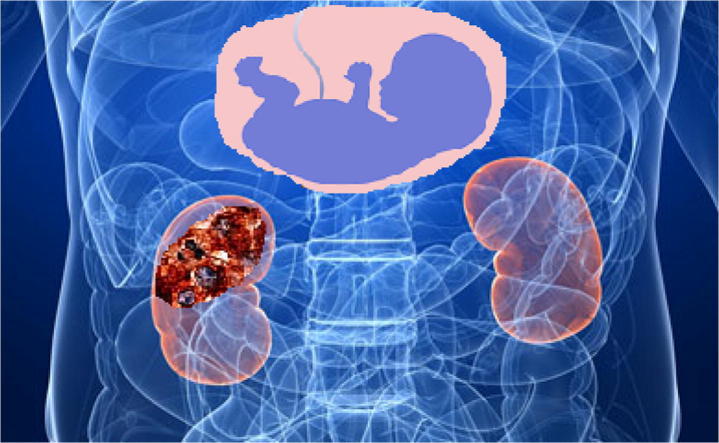
Graphical abstract
Keywords: Renal cancer, Pregnancy, Pregnancy related disorders, Oncology
Abstract
Renal cell carcinoma is rarely diagnosed during pregnancy. Its management is a real challenge due to the sparse literature and lack of standard guidelines. In this situation, the diagnosis is often delayed as the clinical presentation might resemble other pregnancy-related disorders but it should be one of the diagnostic possibilities in women with recurrent or refractory urinary tract symptoms, renal pain, or mass that could be palpated. Diagnostic approach may include ultrasound examination and sometimes magnetic resonance imaging. If localized, surgery would be the preferred line of treatment. Other treatment modalities, end results of treatment, and review of literature of this rare association will be presented.
Introduction
Cancer diagnosis during pregnancy is a rare event. An oncologist can encounter this case in one of two clinical scenarios; either cancer is diagnosed for the first time in a pregnant female or incidental pregnancy occurs during cancer treatment.Treatment of cancer during pregnancy represents a medical dilemma. As pregnant women are usually excluded from clinical trials and due to the rarity of the event, no solid data can support the treatment decision in such setting [1]. Also, the impact of abortion or keeping pregnancy till labor, on prognosis of cancer together with the safety and efficacy of cancer treatment on the maternal and fetal health is not known in many occasions [2].
The landscape of renal cell carcinoma management has changed during the past few years, but surgery remains the main stay modality, and currently there is no role for adjuvant therapy. New targeted agents with proven efficacy in advanced, or metastatic renal cell carcinoma have been developed. However, the effect of these new agents on fetal and maternal outcomes is poorly studied [3].
The aim of this article was to revise the medical literature for data pertinent to this group of patients, aiming to provide answers to questions regarding management of these patients.
Epidemiology and risk factors
Renal cell carcinoma represents about 3% of solid tumors in adults with a slight male predominance [4]. An increase in incidence has been observed during the last two decades, with reports of downward shift of tumor stage and size in many clinical series [4]. Obesity, smoking and hypertension are established risk factors for renal cell carcinoma [5]. High parity among women and other reproductive and hormonal factors has been studied as potential risk factors, but no direct causal effect is evident up till now [4], [5]. Since 1980s, steroid receptors were found on normal and cancerous renal cell tissue. Estrogen can induce renal cell carcinoma in laboratory mice. Adipose tissue in obese women is a source of estrogen that may play a role in increasing the risk for RCC [6]. Treatment with progesterone was explored in the past for treatment of metastatic RCC, but abandoned due to unproved efficacy [7]. Accordingly; it was assumed that a possible correlation between hormonal factors and RCC development exists, although the underlying mechanism is not fully understood.
During pregnancy, estrogen and progesterone reach to a high peak. High parity (⩾5 pregnancies lasting for more than 4 months) was associated with almost doubling of risk for RCC in comparison with nulliparous women in many reports [8], [9], [10]. However, other studies did not show the same association [11], [12]. Only one trial showed a strong association for clear cell adenocarcinoma subtype, although the same trial did not show association with live births [13].
A meta-analysis including 14 studies (5 cohort studies, one nested case control, and 8 case control studies) that were published in 2013 concluded that ever parity, i.e. with a history of at least one pregnancy and increased parity numbers are associated with an increased risk of kidney cancer [14].
Oral contraceptives were associated with risk reduction in some series [12], and age of menarche, hysterectomy and age of first live birth were also studied with contradictory results [8], [9], [10], [11], [12]. Hypertension is a well-established risk factor for RCC [4], [5]. About 18% of cases diagnosed with RCC during pregnancy presented with hypertension [15]. The risk of RCC is dependent on the duration of hypertension; secondary hypertension during pregnancy is of short duration as it develops during the second trimester [4], [5]. It is so unlikely to consider gestational hypertension a risk factor for RCC. In some cases, RCC may induce hypertension with improvement in blood pressure levels after nephrectomy. In a case report of a patient with hypertension during the first trimester of pregnancy, hypertension was reported to be a result of extrinsic compression of renal artery by the tumor. This conclusion was supported by the resolution of hypertension after nephrectomy [16].
VHL and Xp11.2 translocations are among the most commonly noted chromosomal apparitions in renal cell carcinoma. Only two cases harboring Xp11.2 translocations were reported with one of them presented with placental metastases [17], [18]. However, the number of cases is too small to generate a hypothesis regarding the association between these genetic factors and RCC during pregnancy.
Diagnosis and radiology
The choice of radiological modality in a pregnant woman has to take two factors into consideration; the acuity of staging with the least radiation exposure to the fetus.
Proper radiological staging requires CT scan for chest, abdomen and pelvis. MRI can replace CT when in staging of the primary tumor and in detection of renal vein involvement. The role of PET-CT is not well established for staging of RCC. Isotopic bone scan and CT brain are symptom guided investigations and are not required as a part of the initial staging [19]. Finally after diagnosis, renal scintigraphy may be needed to assess kidney function reserve before nephrectomy [19]. The safest diagnostic imaging test during pregnancy is ultrasound, with no teratogenicity or carcinogenesis. There is an increase in cases diagnosed as incidental finding during routine ultrasound examination for antepartum care. Ultrasound has a sensitivity to detect lesions more than 3 cm comparable to that of CT [15]. Plain X ray can be performed with minimal radiation exposure to the fetus if the abdomen was properly shielded. A CT scan that does not include the gravid uterus in the field-of-view results in negligible fetal dose and may be performed in pregnancy without risk to the fetus. A standard single CT scan through the gravid uterus results in a fetal dose of 25 mGy or less [20]. However, the possible teratogenic effect in this non-emergency setting is not preferred. The sensitivity of MRI in detecting pulmonary lesions is inferior to CT. Gadolinium contrast medium is better avoided, as it can cross the placenta and may induce fetal hypothyroidism [21].
PET-CT with an 18F-2-fluoro-2-deoxy-D-glucose injection (FDG) is also contraindicated during pregnancy because of the fetal radiation exposure associated with the CT component of the study. Generally, PET-CT is not a well-established staging method with any significant benefit that may outweigh the risks [22].
Whole body MRI is an emerging method for staging of solid tumors; it has sensitivity comparable to skeletal Scintigraphy for assessment of skeletal deposits [21]. However, its sensitivity in detecting pulmonary lesions in comparison with CT chest remains unknown. Lastly, Doppler studies can be used to substitute renal scintigraphy for patient planned to be submitted to nephrectomy for assessment of function of the other kidney.
Biopsy is not mandatory for diagnosis, as radiological studies usually provide sufficient findings for diagnosis prior to surgery. Core biopsy is recommended in selected cases, mainly in patients with small tumors who are candidates for active surveillance, local ablative therapies (i.e. radiofrequency ablation and cryosurgery), patients with solitary kidney and patients with metastatic disease before initiating targeted therapies [23].
The differential diagnosis of renal masses includes inflammatory, benign and malignant lesions other than renal cell carcinoma. Cystic lesions are usually benign.
Clinical picture and tumor characteristics
A series of review articles were published studying the clinical presentation and management of renal cell carcinoma with pregnancy [15], [21], [22]. The last report included articles published till April 2013, with a total of 102 cases reported. We searched the literature published till February 2015, and additional four cases were found, a case of renal cell carcinoma during pregnancy presented with IVC tumor thrombus [23], a case of rapidly enlarging chromophobe renal cell carcinoma [24], a case of renal cell carcinoma diagnosed during the 14th week of gestation [25] and a case of metastatic renal cell carcinoma that became pregnant and experienced massive disease progression during pregnancy [26] (Table 1).
Table 1.
Clinical and histopathological features of cases diagnosed with RCC during pregnancy.
| No. | % | ||
|---|---|---|---|
| Maternal age at diagnosis | (21–52)y | ||
| Pathology | |||
| Adenocarcinoma | 89 | 84 | |
| Chromophobic | 3 | 2.8 | |
| Nephroblastoma | 8 | 7.7 | |
| Othersa | 6 | 5.7 | |
| Stage at diagnosis | |||
| Localized | 103 | 98.7 | |
| Metastatic | 2b | 1.3 | |
| Gestational age at diagnosis | |||
| First trimester | 6 | 5.7 | |
| Second trimester | 11 | 9.6 | |
| Third trimester | 3 | 2.7 | |
| Not reported | 85 | 82 | |
| Timing of surgery | |||
| Before labor | 13 | 12.5 | |
| Spontaneously with labor | 2 | 2.7% | |
| After labor | 4 | ||
| Termination of pregnancy | 2 | ||
Other histopathological types include the following: two cases with Angiosarcoma, one case with Carcinoid, one with capsular osteoadenocarcinoma, one with Renal pelvis carcinoma and one with lymphoma.
One case diagnosed with renal cell carcinoma 4 years before gestation, presented during pregnancy with rapid increase in size of previously existed metastases.
Incidental finding during routine antepartum examination was reported in many cases [17], [24], [27]. The incidence of accidently discovered cases is expected to increase due to increased utilization of ultrasonography for antepartum care. On the other hand, the clinical presentation with abdominal pain, distension, urinary tract infection and hypertension could be obscured by pregnancy and cause delay in diagnosis. The main reported presenting symptoms are as follows: pain (50% of cases), hematuria (47%), hypertension (18%) and the classical triad of hematuria, pain and palpable mass (26%). Other less frequent presentations (hemolytic anemia, hypercalcemia, rupture of tumoral cyst) were also reported.
Five cases were reported with metastatic disease during pregnancy [18], [28], and the remaining were diagnosed with less advanced disease, usually during the second and third trimesters of pregnancy, and few cases were reported during the first trimester [24], [27].
Histopathological subtypes included 89 cases with clear cell carcinoma, 3 cases with chromophobe RCC, nephroblastomas in 8 cases, angiosarcomas in 2, and carcinoid, capsular osteoadenocarcinoma, renal pelvis carcinoma and lymphoma in one patient each [15].
Management
Standardized guidelines for management are unavailable due to the rarity of this diagnosis and the decision is individualized for each case, putting in consideration the welfare of mother and fetus. A multidisciplinary team including oncologist (surgical and medical), gynecologist, radiologist and urologist is mandatory for decision making. A full and thorough discussion with the mother and the explanation of expected risks for each treatment modality is a must, with respect to her wishes and concerns regarding the fetal safety.
It is unknown whether abortion may improve the outcome of treatment or not, and the scarce number of reported cases is not allowing for a comparative study with their matched stage to draw a conclusion on the impact of pregnancy on tumor behavior. However, in most of the reported cases the patients had a smooth treatment course with good maternal outcomes. Most of them gave birth to healthy viable children. In a review article published in Nature 2010, termination of pregnancy was advised once diagnosis is established. This recommendation is contradicting the conclusion drawn by many authors, together with the outcomes of treatment reported in the literature where smooth recovery with treatment outcomes comparable to those non pregnant patients. However, termination of pregnancy could be considered in patients with metastatic disease [29].
Surgery
Nephrectomy (radical or nephron sparing surgery) remains a pivotal part of management of RCC, even in metastatic disease, where radical nephrectomy is done before systemic treatment. Nephron sparing surgery could be carried out in patients with small tumors.
During pregnancy, the timing and the approach of surgery are two important issues. Fetal maturity and the relatively slow doubling time of RCC (300–500 days) are the main factors guiding the timing for surgery. Patient diagnosed during the first and the third trimester could go for surgical resection immediately after diagnosis, and for patients diagnosed during the second trimester the decision is not straightforward. During second trimester, surgical manipulations may induce uterine contractions causing spontaneous abortion; also hypotension during surgery caused by blood loss can lead to fetal hypoxia with detrimental effect on the fetus [30]. The surgery could be delayed till fetal lung became mature by the 28th week of gestation or even postpartum in some reports [27], [30]. Only two cases had spontaneous cesarean section and surgical resection of the tumor, as the cesarean section and nephrectomy were performed through different incisions and different positions [31], [32], [33].
However, second trimester is considered by some authors as the safest time for surgical intervention. Surgical intervention becomes difficult as the uterus enlarges, and many authors prefer to delay surgery when the patient presented with RCC during the late second trimester, while surgery could be considered safe during early second trimester [34].
The surgical approach either laparoscopic or open surgery, trans peritoneal or retroperitoneal is governed by the tumor site, size and the expertise of the surgical team.
Systemic treatment
The landscape of treatment for metastatic renal cell carcinoma has changed over the past decade. Chemotherapy and hormonal treatment (progesterone) have been abandoned and replaced with targeted therapy. Choice of treatment depends on the pathology (clear versus non-clear), and the presence of short survival predictors. The current treatment options are multikinase inhibitors (sunitinib, sorafenib, axitinib and pazopanib), mTOR inhibitors (everolimus and temsirolimus), anti-angiogenic agents (bevacizumab) and immunological agents (high dose interleukin 2 and recently check-point inhibitors). The safety of these drugs during pregnancy is poorly studied; data are available only from animal studies. The US FDA categorizes drugs according to their safety during pregnancy into five main categories. Drugs classified as category D shall be avoided during pregnancy as there is positive evidence of human fetal risk [35].
Sunitinib [36], sorafenib [37], axitinib [38], pazopanib [39] and temsirolimus [40] are classified as group D, while bevacizumab [41] and everolimus [42] are categorized C and D. Indeed; these drugs are used for other indications besides RCC. For example, everolimus is used as immunosuppressant for patients undergoing allogenic organ (hepatic and renal) transplantation. Bevacizumab is used for intravenous injection while interferon is used for the treatment of HCV. These agents are categorized as group C for these indications but not for oncological indications.
This double categorization could be confusing; the safety of bevacizumab was not studied for RCC during pregnancy [43]. The literature studied the safety of intravenous usage only. The same for everolimus, as there is case report reported its safety during pregnancy in renal transplant patient. No literature is currently available for their usage for RCC in pregnant women.
Chemotherapy is usually avoided during the first trimester of pregnancy but can be safely administered during the second and the third trimesters. On the contrary, monoclonal antibodies can be used during the first trimester and must be avoided during the second and the third trimesters. This is explained by the transportation mechanism for monoclonal antibodies that is not established during the first trimester, but is established later on [44]. Proleukin [45] (Interleukin) is categorized as category C, with no evidence of teratogenicity. However, the significant toxicity noted with the use of IL-2 must be considered.
Conclusions
Renal cell carcinoma during pregnancy is a rare clinical situation. Its diagnosis is often delayed and its management is a real challenge. Termination of pregnancy is not advised except in patients with rapidly growing tumors; otherwise surgery could be postponed till after or during delivery. In case of a localized disease, surgery is the standard line of treatment. For systemic disease, the role of chemotherapy, IL-2, and hormonal treatment has been abandoned and replaced with targeted therapy. However, TKIs, mTOR inhibitors and anti-angiogenesis must be avoided during pregnancy and lactation, and after giving birth.
Conflict of interest
The authors have declared no conflict of interest.
Compliance with Ethics requirements
This article does not contain any studies with human or animal subjects.
Biographies

Dr. Hussein Khaled is a Professor of medical oncology at the National Cancer Institute of Cairo University. He was the former minister of higher education of Egypt (2012), former vice president of Cairo University for post graduate studies and research (2008–2011), and the former dean of the Egyptian National Cancer Institute (2002–2008). Last year (2015), he won the State Recognition Prize for advanced technological sciences in the medical field. His research activities are focused mainly on bladder cancer (both biological and clinical aspects), breast cancer, and malignant lymphomas, with more than 150 national and international publications (total impact factor of 470, total citations of 1741, and h-index of 22).

Dr. Nasr Allahloubi is a Professor of medical oncology at the National Cancer Institute, Cairo University. He is a member of many international societies: ESMO, ASCO, ASH, EASO, and the Secretory of the Egyptian Universities Promotion Committees (EUPC, Committee number 83). He has many publications and national educational presentations and international poster in SABCS, ASCO, and ESMO. He is leading the scientific meetings of the medical oncology department. He is the MD program instructor and a member for external evaluation committee for the MD examination. He is also a member of the Higher Committee of Medical Specialties; Egyptian Fellowship Board; Medical Oncology; and Ministry of Health.

Dr. Noha Rashad is a medical oncology specialist-Maadi Armed Forces Medical Compound, Oncology Hematology Hospital. She passed the final examinations for MD degree of medical oncology and be a certified member of ESMO (2011).
Footnotes
Peer review under responsibility of Cairo University.
References
- 1.Azim H., Peccatori F., Pavlidis N. Treatment of the pregnant mother with cancer: a systematic review on the use of cytotoxic, endocrine, targeted agents and immunotherapy during pregnancy. Part I: solid tumors. Cancer Treat Rev. 2010;36(2):101–109. doi: 10.1016/j.ctrv.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 2.Moran B.J., Yano H., Al Zahir N., Farquharson M. Conflicting priorities in surgical intervention for cancer in pregnancy. Lancet Oncol. 2007;8(6):536–544. doi: 10.1016/S1470-2045(07)70171-7. [DOI] [PubMed] [Google Scholar]
- 3.Escudier B., Porta C., Schmidinger M., Algaba F., Patard J.J., Khoo V. Renal cell carcinoma ESMO clinical practice guidelines for diagnosis treatment and follow-up. Ann Oncol. 2014;25(no. Supplement 3):49–56. [Google Scholar]
- 4.Chow W.-H., Dong L.M., Devesa S.S. Epidemiology and risk factors for kidney cancer. Nat Rev Urol. 2010;7(5):245–257. doi: 10.1038/nrurol.2010.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chow W.H., Devesa S.S. Contemporary renal cell cancer epidemiology. Cancer J (Sudbury, Mass) 2008;14(5):288–301. doi: 10.1097/PPO.0b013e3181867628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ronchi E., Pizzocaro G., Miodini P., Piva L., Salvioni R., Di Fronzo G.J. Steroid hormone receptors in normal and malignant human renal tissue: relationship with progestin therapy. Steroid Biochem. 1984;21(3):329–335. doi: 10.1016/0022-4731(84)90287-5. [DOI] [PubMed] [Google Scholar]
- 7.Harris D.T. Hormonal therapy and chemotherapy of renal-cell carcinoma. Semin Oncol. 1983 Dec;10(4):422–430. [PubMed] [Google Scholar]
- 8.Lambe M., Lindblad P., Wuu J., Remler R., Hsieh C. Pregnancy and risk of renal cell cancer: a population-based study in Sweden. Br J Cancer. 2002;86(9):1425–1429. doi: 10.1038/sj.bjc.6600263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kabat G.C., Silvera S.A.N., Miller A.B., Rohan T.E. A cohort study of reproductive and hormonal factors and renal cell cancer risk in women. Br J Cancer. 2007;96(5):845–849. doi: 10.1038/sj.bjc.6603629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee J.E., Hankinson S.E., Cho E. Reproductive factors and risk of renal cell cancer: the Nurses’ health study. Am J Epidemiol. 2009;169(10):1243–1250. doi: 10.1093/aje/kwp030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zucchetto A., Talamini R., Dal Maso L., Negri E., Polesel J., Ramazzotti V. Reproductive, menstrual, and other hormone-related factors and risk of renal cell cancer. Int. J. Cancer. 2008;123:2213–2216. doi: 10.1002/ijc.23750. [DOI] [PubMed] [Google Scholar]
- 12.Karami S., Daugherty S.E., Schonfeld S.J., Park Y., Hollenbeck A.R., Grubb Reproductive factors and kidney cancer risk in 2 US cohort studies, 1993–2010. Am J Epidemiol. 2013;177(12):1368–1377. doi: 10.1093/aje/kws406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Purdue M.P., Colt J.S., Graubard B., Graubard B., Davis F., Ruterbusch J.J. A case-control study of reproductive factors and renal cell carcinoma among black and white women in the United States. Cancer Causes Control: CCC. 2011;22(11):1537–1544. doi: 10.1007/s10552-011-9830-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guan, Hong-Bo, Wu Qi-Jun, Gong Ting-Ting. Parity and kidney cancer risk: evidence from epidemiologic studies. Cancer Epidemiol Biomark Prev. 2013;22(12):2345–2353. doi: 10.1158/1055-9965.EPI-13-0759-T. [DOI] [PubMed] [Google Scholar]
- 15.Boussios S., Pavlidis N. Renal cell carcinoma in pregnancy: a rare coexistence. Clin Transl Oncol. 2014;16(2):122–127. doi: 10.1007/s12094-013-1105-2. [DOI] [PubMed] [Google Scholar]
- 16.Buda A., Pizzocaro G., Ceruti P., Salvioni R., Battistello M., Vergani P. Case report: renal cell carcinoma presenting as hypertension in pregnancy. Arch Gynecol Obstet. 2008;277(3):263–265. doi: 10.1007/s00404-007-0455-9. [DOI] [PubMed] [Google Scholar]
- 17.Armah H.B., Parwani A.V., Surti U., Bastacky S.I. Xp11.2 translocation renal cell carcinoma occurring during pregnancy with a novel translocation involving chromosome 19: a case report with review of the literature. Diagnost Pathol. 2009;4:15. doi: 10.1186/1746-1596-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bovio I.M., Allan R., Oliai B.R., Hampton T. Xp11. 2 translocation renal carcinoma with placental metastasis: a case report. Int J Surg Pathol. 2011;19(1):80–83. doi: 10.1177/1066896908331231. [DOI] [PubMed] [Google Scholar]
- 19.Vikram R, Caslino DD, Remer EM. ACR appropriateness criteria: renal cell carcinoma staging. 2014; 11(5): 443–9. [DOI] [PubMed]
- 20.Dubinsky CT in pregnancy: risks and benefits. Appl Radiol. 2013:6–16. [Google Scholar]
- 21.Wu Q., Yang R., Zhou F., Hu Y. Comparison of whole-body MRI and skeletal scintigraphy for detection of bone metastatic tumors: a meta-analysis. Surg Oncol. 2013;22(4):261–266. doi: 10.1016/j.suronc.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 22.Colletti, Patrick M. PET-CT in the Pregnant Patient. <http://www.imagewisely.org/~/media/ImageWisely%20Files/NucMed/PETCT%20in%20the%20Pregnant%20Patient.pdf>.
- 23.Muglia W.V., Prando A. Renal cell carcinoma: histological classification and correlation with imaging findings. Radiol Brasil. 2015;48(3):166–174. doi: 10.1590/0100-3984.2013.1927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walker J.L., Knight E.L. Renal cell carcinoma in pregnancy. Cancer. 1986;58(10):2343–2347. doi: 10.1002/1097-0142(19861115)58:10<2343::aid-cncr2820581031>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 25.Akpayak I.C. Renal cell carcinoma in pregnancy: still a management challenge. Afric J Urol. 2015;21(3):167–170. [Google Scholar]
- 26.Mangel L., Bíró K., Battyáni I., Göcze P., Tornóczky T., Kálmán E. A case study on the potential angiogenic effect of human chorionic gonadotropin hormone in rapid progression and spontaneous regression of metastatic renal cell carcinoma during pregnancy and after surgical abortion. BMC Cancer. 2015;15(1):1013. doi: 10.1186/s12885-015-2031-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pentheroudakis George., Pavlidis Nicholas. Springer; Berlin Heidelberg: 2008. Gastrointestinal, urologic and lung malignancies during pregnancy. Cancer and pregnancy; pp. 137–164. [DOI] [PubMed] [Google Scholar]
- 28.Katayama H., Ito A., Kakoi N., Shimada S., Saito H., Arai Y. A case of renal cell carcinoma with inferior vena cava tumor thrombus diagnosed during pregnancy. Urol Int. 2013;92(1):122–124. doi: 10.1159/000354351. [DOI] [PubMed] [Google Scholar]
- 29.Khochikar M.V. Management of urological cancers during pregnancy. Nat Rev Urol. 2010;7(4):195–205. doi: 10.1038/nrurol.2010.25. [DOI] [PubMed] [Google Scholar]
- 30.Tiang K.W., Ng K.L., Vega-Vega A., Wood S. Rapidly enlarging renal tumor during pregnancy: diagnostic and management dilemma. J Kidney Cancer VHL. 2014;1(1):12–16. doi: 10.15586/jkcvhl.2014.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pertia Ambrosi., Chkhotua Archil., Managadze Laurent. Simultaneous Nephron-Sparing Surgery and Caesarian Section for the Treatment of Renal Cell Carcinoma in Pregnancy: Case Report and Review of the Literature. INTECH Open Access Publisher. 2012:436–442. [Google Scholar]
- 32.Van der Veldt A.A., van Wouwe M., van den Eertwegh A.J., van Moorselaar R.J., van Geijn H.P. Metastatic renal cell cancer in a 20-year-old pregnant woman. Urology. 2008;72(4):775. doi: 10.1016/j.urology.2008.04.048. [DOI] [PubMed] [Google Scholar]
- 33.Kobayashi T., Fukuzawa S., Miura K., Matsui Y., Fujikawa K., Oka H., Takeuchi H. A case of renal cell carcinoma during pregnancy: simultaneous cesarean section and radical nephrectomy. J Urol. 2000;163(5):1515–1516. [PubMed] [Google Scholar]
- 34.Gladman M.A., MacDonald D., Webster J.J., Cook T., Williams G. Renal cell carcinoma in pregnancy. J R Soc Med. 2002;95(4):199–201. doi: 10.1258/jrsm.95.4.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Drug Use During Pregnancy – Women’s Health Issues – MSD Manual Consumer Version, http://www.msdmanuals.com/home/womens-health-issues/drug-use-during-pregnancy/drug-use-during-pregnancy> [accessed February 22, 2016].
- 36.Product Monograph: Sunitinib (Sutent®). Pfizer Canada Inc.; December 2014.
- 37.Product Monograph: Nexavar® (Sorafenib). Bayer Inc.; December 17, 2014.
- 38.Product Monograph: InlytaTM (axitinib). Pfizer Products Incorporated; June 6, 2014.
- 39.Product Monograph: Votrient® (pazopanib). GlaxoSmithKline Inc. (Canada); January 30, 2014.
- 40.Product Monograph: Torisel® (temsirolimus). Pfizer (US); May 2012.
- 41.Product Monograph: Avastin® (bevacizumab). Roche Canada; January 29, 2014.
- 42.Product monograph: Afinitor® (everolimus). Novartis Pharmaceuticals; November 3, 2014.
- 43.Avastin – FDA Prescribing Information, Side Effects and Uses,” <http://www.drugs.com/pro/avastin.html>, [accessed February 26, 2016].
- 44.Sarno M.A., Mancari R., Azim H.A., Jr, Colombo N., Peccatori F.A. Are monoclonal antibodies a safe treatment for cancer during pregancy? Immunotherapy. 2013;5(7):733–741. doi: 10.2217/imt.13.64. [DOI] [PubMed] [Google Scholar]
- 45.Proleukin® (aldesleukin/interleukin2) [[]product monograph]. Dorval, Quebec: Novartis Pharm‘aceuticals Canada Inc.; Sept 20, 2012.