Abstract
Background
Topical life long anti glaucoma medication forms the mainstay of treatment of primary open angle glaucoma. Their long term usage can cause changes in conjunctival epithelium.
Methods
Hundred cases of primary open angle glaucoma were divided into four groups of 25 patients each. Each group was put on Timolol, Pilocarpine, Brimonidine and Latanoprost respectively. Ocular surface changes were monitored using Schirmer's test, tear film break up time (BUT) and conjunctival impression cytology.
Result
Altered Schirmer's test value was seen in 40% of patients and reduced tear film BUT values in 26%, at the end of one year. These changes were more in patients treated with timolol. Changes in conjunctival cytology such as decrease in goblet cell density, squamous metaplasia and presence of inflammatory cells were seen in significant number of patients at the end of one year treatment. There was direct relation of duration of treatment to various ocular surface changes.
Conclusion
Ocular surface changes are seen in significant number of patients of primary open angle glaucoma at the end of one year follow up with topical anti glaucoma therapy. Conjunctival impression cytology is a non invasive technique to monitor these changes.
Key Words: Primary open angle glaucoma, Ocular surface changes, Goblet cell density, Squamous metaplasia
Introduction
Primary open angle glaucoma is the second most common cause of blindness all over the world. The exact patho physiology of optic nerve damage in glaucoma is not clearly understood but there is enough evidence to believe that raised intra ocular pressure (IOP) has direct relation to extent of optic nerve damage. Out of the various causative factors, IOP is the only modifiable factor in primary open angle glaucoma. Hence control of intra ocular pressure remains the mainstay of therapy for glaucoma. In the last two decades a range of newer topical medications have been introduced such as beta blockers, topical carbonic anhydrase inhibitors, prostaglandin analogues and alpha adrenergic agonist for management of glaucoma. Glaucoma therapy is life long and topical agents used over long time, are likely to cause changes in ocular surface particularly reduction in tear secretion, changes in tear film break up time (BUT) and changes in conjunctival epithelium.
This study was carried out to analyze the effects of four commonly used anti glaucoma drugs i.e timolol, pilocarpine, brimonidine and latanoprost on ocular surface by a simple non invasive technique of conjunctival impression cytology and to correlate them with IOP controlling effect of the drugs.
Material and Methods
Hundred new cases of primary open angle glaucoma reporting to the eye out patient department were included in the study. The diagnosis was confirmed by aplanation tonometry, gonioscopy, visual fields recording and fundus examination. Patients on long-term topical medication like artificial tear drops/disodium cromoglycate drops, those with primary or secondary ocular surface disorders like conjunctival xerosis, trachoma, chemical burns, intra or extra ocular surgery and lagophthalmos/ lid deformities were excluded.
The patients were divided into four groups of 25 each. Group A was put on commercially available preparation of timolol maleate 0.5% twice daily dose. Group B was put on 2% pilocarpine nitrate eye drops four times a day, Group C on 0.2% brimonidine tartarate eye drops thrice daily dose and Group D on 0.005% latanoprost eye drops once at bed time. All patients were followed up for a period of one year. Visual acuity and intra ocular tension (IOT) were recorded monthly. Schirmer's test and tear film break up time were carried out once in three months. Visual field recording was done by automated perimetry using 24-2 programme of Humphry visual field analyzer initially and at six monthly intervals. Conjunctival impression smear was taken at three monthly intervals. The technique was to apply 1×1 cm strip of cellulose acetate filter paper to upper temporal bulbar conjunctiva of each eye and keep it pressed firmly for five seconds. Each strip was transferred on to glass slides and fixed immediately using 1:1 mixture of absolute alcohol and ether. One of the smears thus fixed was subjected to Papanicolau stain and the other to Periodic Acid Schiff stain. The stained smears were studied and graded by an experienced pathologist (blind observer) into Goblet cells density of >75/HPF, 50-75/HPF, 15-50/HPF, <15/HPF; mild, moderate and severe squamous metaplasia and presence or absence of inflammatory cells.
Results
Out of 100 patients, four were lost to follow up. In another eight patients intra ocular pressure was not controlled and they were put on two-drug therapy and excluded from the study. A total of 88 patients completed the study. The group included 42 males and 46 females with a mean age of 53 years.
Timolol exhibited 34%, pilocarpine 32%, brimonidine 30% and latanoprost 32% reduction in baseline IOP at one month follow up. IOP lowering effect of all the drugs was consistent throughout the study. There was no deterioration of visual fields in all the 88 subjects.
Schirmer's test value was more than 15 mm in all except two (2.3%) patients where it was between 10-15 mm. At the end of the six months two patients of timolol group and one patient of pilocarpine group showed Schirmer's Test value between 6 to 10mm. At the end of one year, eight (38%) patients of timolol group, three(13%) patients from pilocarpine, and two (9%) each from brimonidine and latanoprost group showed Schirmer's Test value of less than 10 mm. In total out of 88 patients who completed the study, 35 (40%) patients had Schirmer's test value of less than 15mm at the end of one year as against two (2.6%) at the outset. Out of these 15 (42%) patients had Schirmer's test value of less than 10 mm and 53% of these belonged to timolol group (Table 1).
Table 1.
Schirmer's test results
| Drug Group | Number of patients |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 month |
6 months |
12 months |
|||||||
| >15 mm | 10-15 mm | <10 mm | >15mm | 10-15mm | <10mm | >15mm | 10-15mm | <10 mm | |
| Timolol (n=21) | 21 | 0 | 0 | 19 | 2 | 0 | 6 | 7 | 8 (38%) |
| Pilocarpine (n=22) | 21 | 1 | 0 | 20 | 2 | 0 | 14 | 5 | 3 (13%) |
| Brimonidine (n=22) | 21 | 1 | 0 | 21 | 1 | 0 | 17 | 3 | 2 (9%) |
| Latanoprost (n=23) | 23 | 0 | 0 | 22 | 1 | 0 | 16 | 5 | 2 (9%) |
The tear film BUT was more than 10 seconds in all patients at the beginning of the study. The values remained same at the end of the first quarter. At the end of the six months three (14%) patients of timolol group, two (9%) patients of pilocarpine group and one (4.5%) each from brimonidine and latanoprost group showed tear film BUT of less than 10 seconds. At the end of one year nine (43%) patients of timolol group, six (27%) patients of pilocarpine group and four (18%) each from brimonidine and latanoprost group showed tear film BUTof less than 10 seconds. None required tear substitute as they were asymptomatic. A total of 23 (26%) out of 88 patients showed reduced tear film BUT at the end of one year and 36% of these belonged to timolol group (Table 2).
Table 2.
Number of patients with tear film break up time <10 sec
| Drug Group | Number of patients |
12 months | ||
|---|---|---|---|---|
| 0 month | 3 months | 6 months | ||
| Timolol group (n=21) | 0 | 0 | 3 | 9 (43%) |
| Pilocarpine group (n=22) | 0 | 0 | 2 | 6 (27%) |
| Brimonidine group (n=22) | 0 | 0 | 1 | 4 (18%) |
| Latanoprost group (n= 23) | 0 | 0 | 1 | 4 (18%) |
Conjunctival impression smears at the beginning of the study showed presence of goblet cell density of more than 75 cells /HPF in 76 (86%) out of 88 patients, cell density of 50-75 cells per /HPF in 10 (11%) patients and cell density of 15-50 cells / HPF in two (2.2%) patients. At the end of six months goblet cell density between 15-50 cells /HPF was seen in six (28%) patients from timolol group, four (18%) of pilocarpine and two (9%) each of brimonidine and latanoprost group. At the end of one year goblet cell density between 15-50 cells / HPF was seen in 12 (57%) patients from timolol group, seven (32%) of pilocarpine group, five (23%) of brimonidine and four (17%) of latanoprost group. A total 28 (32%) patients showed moderate loss of goblet cell at end of one year treatment (Table 3, Fig. 1, Fig. 2).
Table 3.
Number of patients with goblet cell density of <50 cells /HPF
| Study Group | Number of patients |
|||
|---|---|---|---|---|
| 0 month | 3 months | 6 months | 12 months | |
| Timolol group (n=21) | 0 | 1 | 6 | 12 (57%) |
| Pilocarpine group (n=22) | 1 | 1 | 4 | 7 (32%) |
| Brimonidine group (n=22) | 1 | 1 | 2 | 5 (23%) |
| Latanoprost group (n=23) | 0 | 1 | 2 | 4 (17%) |
Fig. 1.
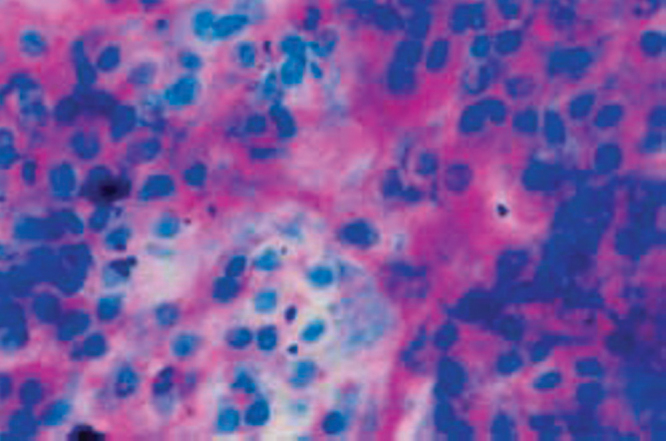
Normal conjunctival smear with plenty of goblet cells (PAS × 400)
Fig. 2.
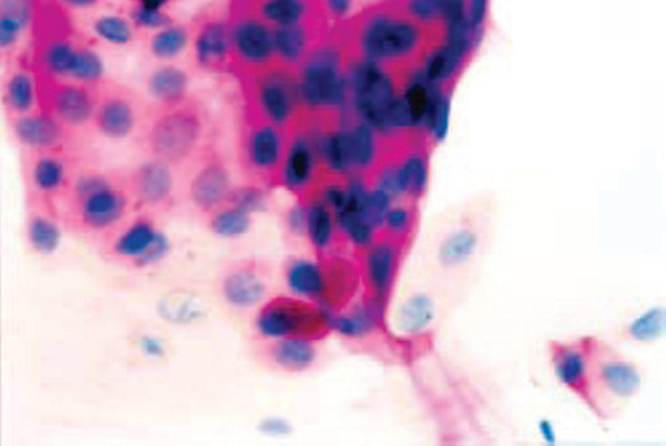
Conjunctival impression smear of patient from timolol group showing depletion in goblet cell density at six month follow up (Papanicolau × 400).
Presence of inflammatory cells was seen in eight (9%) patients out of 88 patients at the beginning of study. At the end of six months, four(19%) patients from timolol group, six (27%) of pilocarpine group, eight (36%) of brimonidine and four(17%) of latanoprost group showed the presence of inflammatory cells. At the end of one year, six (27%) patients from timolol group, nine (41%) from pilocarpine group, 12 (55%) from brimonidine and six (26%) from latanoprost group showed presence of inflammatory cells. Over all 37.5% of the patients showed the presence of inflammatory cells at the end of one year follow up. Out of these 36% patients belonged to brimonidine group (Table 4, Fig 3).
Table 4.
Number of patients showing presence of inflammatory cells
| Study Group | Number of patients |
|||
|---|---|---|---|---|
| 0 month | 3 months | 6 months | 12 months | |
| Timolol group (n=21) | 2 | 3 | 4 | 6 (27%) |
| Pilocarpine group (n=22) | 3 | 4 | 6 | 9 (41%) |
| Brimonidine group (n=22) | 2 | 5 | 8 | 12 (55%) |
| Latanoprost group (n=23) | 1 | 2 | 4 | 6 (26%) |
Fig. 3.
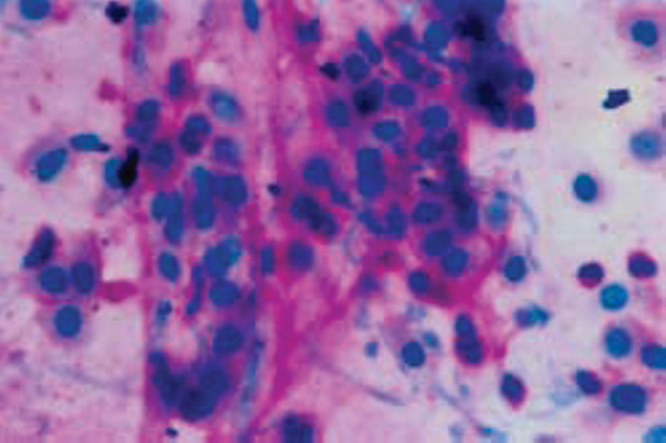
Conjunctival impression smear of patient from pilocarpine group showing numerous neutrophils with squamous metaplasia (PAS × 400).
Squamous metaplasia was seen in nine (10.2%) patients out of 88 patients at the beginning of study. At the end of six months, eight (38%) patients from timolol group, six (27%) from pilocarpine, five (23%) from brimonidine and eight (35%) from latanoprost group showed presence of squamous metaplasia. At the end of one year squamous metaplasia was seen in 12 (57%) patients from timolol group, nine (41%) of pilocarpine, eight (36%) of brimonidine and 11(48%) of latanoprost group. A total of 40 (45%) patients showed squamous metaplasia as against 10.2% at the beginning (Table 5, Fig 4).
Table 5.
Number of patients with moderate degree of squamous metaplasia
| Study Group | Number. of patients |
|||
|---|---|---|---|---|
| 0 month | 3 months | 6 months | 12 months | |
| Timolol group (n=21) | 3 | 6 | 8 | 12 (57%) |
| Pilocarpine group (n=22) | 2 | 4 | 6 | 9 (41%) |
| Brimonidine group (n=22) | 3 | 3 | 5 | 8 (36%) |
| Latanoprost group (n=23) | 1 | 5 | 8 | 11 (48%) |
Fig. 4.
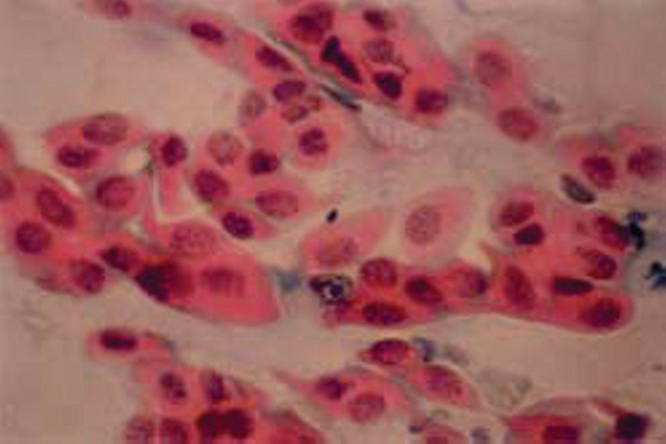
Conjunctival impression smear of patient from latanoprost group showing moderate degree of squamous metaplasia at the end of one year (Papanicolau × 400).
Comparison of cytological changes at the end of one year shows that decrease in goblet cell density was more in patients of timolol group, squamous metplasia was more in patients of latanoprost group and inflammatory response was more with pilocarpine and brimonidine (Fig 5). On review of conjunctival impression smear of patients with reduced tear film BUT, 80% smears showed decrease in goblet cell density and 60% had squamous metaplasia, but there was no significant correlation with the presence of inflammatory cells.
Fig. 5.
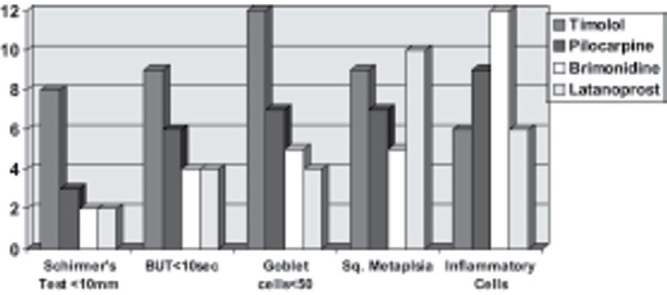
Comparison of ocular surface changes with various drugs at the end of one year.
No serious adverse reactions were noted with any of the drugs. Six patients from pilocarpine group complained initially of brow ache, which subsided later on. In the brimonidine group four patients had mild ocular irritation and two had conjunctival hyperaemia. In latanoprost group conjunctival hyperaemia was seen in three cases. None of the patients required discontinuation of drug.
Discussion
Decrease in Schirmer's test value and tear film BUT value was seen in significant number of patients from all four groups at the end of one year treatment. These findings were common in patients on timolol suggesting that long term use of timolol is likely to affect the tear secretion. Arici et al [1], observed a statistically significant decrease in the number of patients with normal Schirmer's test values after timolol administration for three years. Donocik et al [2], in their study of influence of beta adrenergic antagonist on tear secretion have observed significant decrease in Schirmer's test values in children treated with timolol twice daily for 12 months. Kuppens et al [3], have studied basal tear turnover rate using flurophotometry in patients who have used timolol 0.5% (with and without the preservative benzalkonium chloride) for a mean duration of 3.5 years and observed that the basal tear turnover rate is slightly decreased in timolol with benzalkonium chloride group as compared to controls and the group administered with timolol without benzalkonium chloride.
Decrease in goblet cell density was seen in conjunctival impression cytology specimens of patients with decrease in Schirmer's test value and reduced tear film BUT value, which explains the reason for changes in these values. Majority of these patients were from timolol group. Herreras et al [4], studied conjunctival impression cytology findings after treatment with topical 0.5% timolol for a mean duration of 25.1 months and observed a significant decrease in goblet cell density in the study group [4].
Squamous metaplsia was seen in most of the conjunctival smears with decrease in goblet cell densities. This shows that alteration in tear film is associated with squamous metaplasia of conjunctival epithelium. Priya et al [5], in their study of conjunctival impression cytology in contact lens wearers observed that decrease in goblet cell density with squamous metaplasia resulted in symptoms of dry eye in patients using contact lens. At end of one year, the percentage of patients with squamous metaplasia was higher in latanoprost group. This is in agreement with the findings of Costagliola et al [6], who attributed this to high concentration of benzalkonium chloride in latanoprost preparation and its bedtime administration.
The inflammatory response was more in patients from brimonidine and pilocarpine group indicating that these drugs when used over long periods are likely to cause sub clinical inflammation in conjunctiva. Katz et al [7], observed that incidence of ocular allergy is more common with patients using brimonidine as compared to those using timolol. Arici et al [1], observed that conjunctival impression cytology score was more in patients treated with 1% dipivefrin hydrochloride. Barbara et al [8], have found expression of inflammatory marker HLA-DR on epithelial cells and T lymphocytes in impression cytology of patients receiving topical anti glaucoma medication.
In this study all the drugs used had benzalkonium chloride as preservative. Therefore either the preservative alone or the drug alone or both together could be responsible for various ocular surface changes observed. Baudouin et al [9], observed that benzalkoniuum chloride which is used as preservative in anti glaucoma preparations has shown strong evidence of toxicity to ocular surface. Another study by the same workers have found better stability of tear film in patients using preservative free carteolol [10].
The changes seen in conjunctival impression cytology neither had any influence on IOP lowering effect of the drugs nor did they produce any objective findings in the patients eye. Their clinical significance is not known.
Squamous metaplasia and inflammatory cells were seen in about 8-10% of the eyes at the beginning of the study. Most of these patients were from rural area and were involved in out door occupations. Excessive exposure to sunlight, dust and environmental pollution in these patients might be responsible for these cytological changes.
In this study we found that conjunctival impression cytology is a useful tool in assessing changes in conjunctival epithelium. Thus it can serve as a diagnostic and prognostic parameter in assessing ocular surface disorders. In this study papanicolau stained smear was also found to be useful in the assessment of squamous metaplasia and presence of inflammatory cells. However periodic acid schiff stain brings out the presence of mucin even in metaplastic cells.
To conclude ocular surface changes such as decrease in Schirmer's test value, reduced tear film BUT, decrease in goblet cell density, squamous metaplasia and inflammatory response are seen in significant number of patients with topical anti glaucoma medication. These changes were more common in patients treated with timolol. Inflammatory response was seen in patients treated with brimonidine and pilocarpine where as squamous metaplasia was seen more often in patients treated with latanoprost. The effect of benzalkonium chloride as preservative in these drugs could not be clearly ascertained. A further study with preservative free drugs is required to confirm these findings. A fair number of patients engaged in out door activities also showed various ocular surface changes at the beginning of the study indicating the adverse effect of over exposure to environmental factors such as sunlight, dust and pollution on conjunctiva.
Conflicts of Interest
This study has been funded by the research grants from the office of DGAFMS.
References
- 1.Arici MK, Arici DS, Topalkara A, Guler C. Adverse effects of topical antiglaucomatous drugs on the ocular surface. Clin exp ophthalmol. 2000;28:113–117. doi: 10.1046/j.1442-9071.2000.00237.x. [DOI] [PubMed] [Google Scholar]
- 2.Donocik ES, Koraszewska M. Influence of beta adrenergic antagonist on tear secretion in children. Pol J Pharmacol. 2004;56:871–873. [PubMed] [Google Scholar]
- 3.Kuppens EVMJ, de Jong CA, Stolwijk TR, de Keizer RJW, Best JAV. Effect of timolol with and without preservative on the basal tear turnover in glaucoma. Br J Ophthalmol. 1995;79:339–342. doi: 10.1136/bjo.79.4.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herraras JM, Pastor CJ, Calonge M, Asenson VM. Ocular surface alteration after long-term treatment with an antiglaucomatous drug. Ophthalmology. 1992;99:1082–1088. doi: 10.1016/s0161-6420(92)31847-0. [DOI] [PubMed] [Google Scholar]
- 5.Priya S, Jaison SG, Chopra SK, Jacob S. Conjunctival impression cytology in contact lens wearers. Indian Journal of Ophthalmology. 2002;50:301–306. [PubMed] [Google Scholar]
- 6.Costagliola C, Prete AD, Incorvaia C, Fusco R, Parmeggianni F, Di Giovanni A. Ocular surface changes induced by topical application of latanoprost and timolol: A short-term study in glaucomatous patients with and without allergic conjunctivitis. Graefe's Arch Clin Exp Ophthalmol. 2001;239:809–814. doi: 10.1007/s004170100328. [DOI] [PubMed] [Google Scholar]
- 7.Katz LJ, and the Brimonidine Study Group Brimonidine Tartarate 0.2% twice daily vs Timolol 0.5% twice daily one year results in glaucoma patients. American Journal of Ophthalmology. 1999;127:20–26. doi: 10.1016/s0002-9394(98)00286-4. [DOI] [PubMed] [Google Scholar]
- 8.Barbara C, Aloiz I. Ocular surface changes induced by topical antiglaucoma monotherapy. Ophthalmologica. 2002;216:175–179. doi: 10.1159/000059624. [DOI] [PubMed] [Google Scholar]
- 9.Baudouin C. Side effects of antiglaucomatous drugs on the ocular surface. Current Opinion in Ophthalmology. 1996;7(2):80–86. doi: 10.1097/00055735-199604000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Baudouin C, De Lunardo C. Short term comparative study of topical 2% carteolol with or without benzalkonium chloride in healthy volunteers. Br J Ophthalmol. 1998;82:39–42. doi: 10.1136/bjo.82.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]


