Abstract
Background
Splanchnic hypoperfusion in sepsis leads to translocation of bacteria from gut and development of multi-organ dysfunction syndrome (MODS), with increased mortality in critically ill patients. Gastric tonometry can detect this hypoperfusion by measuring carbon dioxide tension (PgCO2) and intramucosal pH (pHi) from gastric mucosa. Therapeutic intervention aimed at improving gut perfusion can improve the outcome and prognosticate the mortality in sepsis patients.
Methods
100 patients with clinical diagnosis of sepsis were included and divided into two groups of 50 each. Group A patients were managed traditionally without gastric tonometry and in Group B gastric tonometry was used for therapeutic intervention. The intramucosal PCO2, pHi, end tidal carbon dioxide tension (EtCO2) and (PgCO2-EtCO2) differences were monitored at 0, 12 and 24 hours interval.
Result
Overall mortality in Group A was 64 % and 54 % in Group B. In Group B 45% patients developed MODS and 54 % died with low pHi. As an index of mortality low pHi had a sensitivity of 70% and specificity of 65%.
Conclusion
There is a good correlation between mortality prediction on the basis of pHi and PgCO2-EtCO2 difference and actual mortality in critically ill patients. The gastric tonometer should be used to predict mortality and guide resuscitation in septicemia.
Key Words: Sepsis, Splanchnic hypoperfusion, Multi-organ dysfunction syndrome, Gastric tonometry
Introduction
Splanchnic ischemia is postulated to be of major importance in the development of multiorgan failure, and death in critically ill patients [1]. The stomach is one of the first organs to suffer from hypoperfusion and the last to be restored to normality by resuscitation [2]. These alterations are reflected by increase in the gastric intramucosal pH (pHi) and carbon dioxide (CO2). Gastric tonometer measures pHi and carbon dioxide tension (PgCO2) in gastric mucosa (Fig. 1, Fig. 2). Gastric tonometry is based on the measurement of PgCO2 in gastric mucosa by inserting a multi lumen catheter with a semi permeable silicon balloon at the distal end. The carbon dioxide produced in the mucosal cells being freely diffusible, equilibrates across the semi-permeable membrane of the balloon. Low pHi is associated with poor out come [2, 3] and it can serve as a marker of inadequate tissue perfusion/ oxygenation (shock) and an end point of resuscitation [2, 4, 5, 6, 7]. Measurement of gastric intramucosal pH provides a measure of tissue acid base balance in a region of the body that is among the first to develop dysoxia in shock and sepsis [8, 9].
Fig. 1.
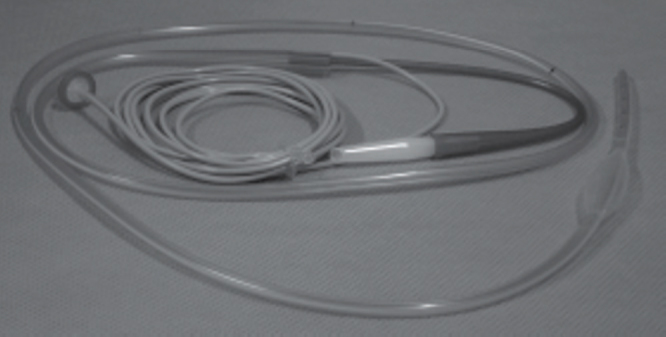
Gastric tonometer catheter
Fig. 2.
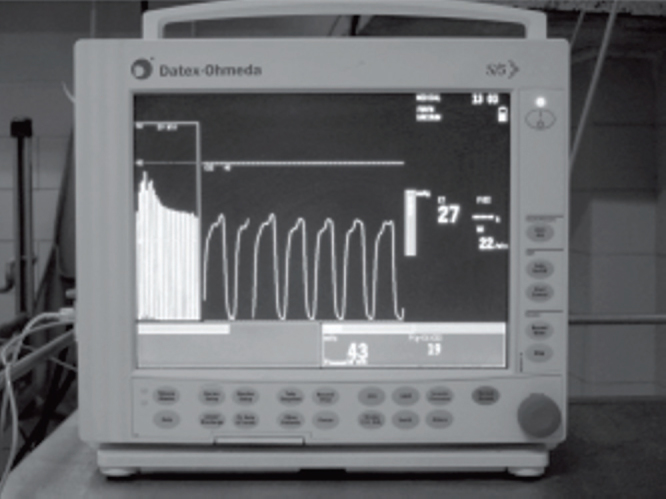
Datex Ohmeda S/5 monitor-gastric tonometer
Material and Methods
Hundred patients (52 male and 48 female) consisting of both medical and surgical groups having sepsis admitted to intensive care unit (ICU) were included in the study. The diagnosis of sepsis was based on patients having two or more clinical manifestations of systemic inflammatory response syndrome (Table 1). The patients were divided into two groups of 50 patients each. Group A formed the control group and these patients were managed traditionally without gastric tonometry. In Group B (study group) gastric tonometry was used to guide therapeutic intervention in the form of intravenous (IV) crystalloids/ colloids, inotropes (dopamine, dobutamine and noradrenaline) and antibiotics. Exclusion criteria were age less than 18 years, active gastrointestinal bleeding, bleeding diathesis, previous history of peptic ulcer, and more than 45 mm Hg PaCO2.
Table 1.
Sepsis Syndrome/ Systemic Inflammatory Response Syndrome (SIRS) Criteria [22]
The systemic inflammatory response to a wide variety of severe clinical insults, manifested by two or more of the following conditions:
|
Patients in both groups were monitored for temperature, heart rate, breath rate, mean blood pressure (BP), SpO2, total leucocytes count, and arterial blood gas. In Group B patients PgCO2, pHi and EtCO2 was monitored at 0, 12 and 24 hours using gastric tonometer. Once the diagnosis of sepsis was established gastric tonometer catheter was inserted like a standard nasogastric tube into stomach and time taken as zero hour. The position of the catheter was confirmed radiologically. Intramucosal pCO2 (partial pressure of carbon dioxide in arterial blood), pHi and EtCO2 were monitored using air gastric tonometer (Datex Ohmeda S/5 Compact Critical Care Monitor-Tonocap). The monitor fills the gastric balloon attached to the standard catheter with 5 ml of room air, which is kept there for 10 minutes for equilibration with gastric mucosal CO2. The sample is then withdrawn and analyzed for CO2 content. Tonocap calculates the pHi when PaCO2 and pH values are entered from arterial blood gas analysis. Normal pHi value is taken as >7.32. The monitor also calculates PgCO2 and EtCO2 difference. All patients received ranitidine 50 mg intravenously 8 hourly and were fasted for one hour before taking reading of PgCO2 and pHi. The catheter was removed after 48 hours. Patients on ventilator were kept well sedated with midazolam and opioid.
Results
The findings of Group A patients (Table 2) show a mortality rate of 64 %. It was noticed that tachycardia and tachypnea persisted in nonsurvivors despite adequate resuscitation. The findings of Group B (Table 3) show an overall mortality of 54%. It was seen that patients with low pHi developed multi-organ failure and had higher mortality. Table 4 shows changes in parameters in survivors and non survivors. The survival was better in the patients whose pHi returned back to normal value after treatment. In 67 % patients pHi remained low and in 35 % patients increased to normal value after treatment. The decrease in pHi in nonsurvivors was 7.2 and above 7.34 in survivors. The prediction of mortality with mean value of pHi and PgCO2-EtCO2 gap at 0, 12 and 24 hours is shown in Table 4. As an index of predicted mortality, low pHi had a sensitivity of 70 % and specificity of 65 %.
Table 2.
Group ‘A’ (Conventional treatment without gastric tonometer monitoring) (S= survivors, NS= non survivors, all mean values)
| Measured parameters | Mean value (zero hours) | Response to therapy (12 hours) |
Response to therapy (24 hours) |
||
|---|---|---|---|---|---|
| S | NS | S | NS | ||
| Heart rate (per minute) | 107.0 ± 4 | 104 | 110 ± 9 | 96 | 110 ± 10 |
| MAP (mm Hg) | 81.4 ± 5.0 | 88.5 | 58.9 ± 6.5 | 86.6 | 61.5 ± 6.0 |
| Temperature | 102.0 ± 0.75 | 100.5 | 102.5 ± 0.55 | 99.5 | 102.8 ± 0.55 |
| White cell count | 14,000 ± 1500 | 14,000 | 14,500 | 15,000 | 11,000 |
| PgCO2 | 44.6 | 43.5 | 59.0 | 40.5 | 56.4 |
| pHi | 7.29 | 7.34 | 7.22 | 7.36 | 7.25 |
| EtCO2 | 35.0 | 33.5 | 39.0 | 36.5 | 38.0 |
| PgCO2-EtCO2 | 9.6 | 9.5 | 20.0 | 8.5 | 18.4 |
(Temp=°F, white cell count = per cumm, PgCO2 and EtCO2 = mm Hg, MAP = mean arterial pressure)
Table 3.
Group ‘B’ (Therapy guided with gastric tonometer findings) (S= survivors, NS= non survivors, all mean values)
| Measured parameters | Mean value (zero hours) | Response to therapy (12 hours) |
Response to therapy (24 hours) |
||
|---|---|---|---|---|---|
| S | NS | S | NS | ||
| Heart rate (per minute) | 107.2 ± 4 | 102.4 | 108.5 ± 9 | 104 | 110 ± 10 |
| MAP (mm Hg) | 75.7 ± 5.5 | 87.5 | 62.3 ± 3.5 | 88.6 | 61.8 ± 3 |
| Temperature | 100.6 ± 0.75 | 100.2 | 102.8 ± 0.55 | 99.5 | 102.2 ± 0.55 |
| White cell count | 12600 ± 1500 | 1300 | 13500 | 10500 | 14000 |
| PgCo2 | 45.8 | 43.5 | 59.2 | 40.5 | 62.4 |
| pHi | 7.28 | 7.34 | 7.19 | 7.35 | 7.20 |
| EtCO2 | 35.6 | 33.5 | 39.0 | 34.5 | 40.0 |
| PgCO2-EtCO2 | 10.2 | 9.5 | 20.2 | 8.5 | 22.4 |
(Temp=°F, white cell count =per cu mm, PgCO2 and EtCO2=mm Hg)
Table 4.
Mean values in survivors and nonsurvivors
| Parameters | Time (hours) | Survivors | Nonsurvivors |
|---|---|---|---|
| pHi | 0 | 7.3 ± 0. 05 | 7.19 ± 0.055 |
| 12 | 7.32 ± 0.05 | 7.22 ± 0.05 | |
| 24 | 7.33 ± 0.05 | 7.24 ± 0.05 | |
| PgCO2-EtCO2 | 0 | 10 ± 2.5 | 15 ± 3.5 |
| (PgCO2 Gap) | 12 | 12 ± 2.75 | 18 ± 2.5 |
| 24 | 14 ± 3.5 | 15 ± 4.25 |
We did not find the CVP, temperature and SpO2 as the major determinant of outcome in critically ill patients.
Discussion
Measurements of gastric mucosal pH (pHi) at 0, 12 and 24 hours has predictive value in critically ill patients.
pHi and PgCO2-EtCO2 (PaCO2) are better indicators of splanchnic ischemia than pHi because the effect of systemic acid-base balance on gastric intramucosal acid-base balance is eliminated [7, 10]. Our results confirm findings of other workers that pHi can distinguish survivors from nonsurvivors in critically ill patients during early period [11, 12].
Patients with low pHi at zero hours have a higher mortality particularly if pHi does not improve with intervention within 24 hours [2, 11, 13, 14]. A large difference in the partial pressure of carbon dioxide between gastric mucosa and arterial blood (PgCO2-PaCO2) has been shown to be more specific indicator of splanchnic ischemia and predictors of outcome [15, 16]. Our study is in agreement with these findings. Santoso et al [17], documented the potential usefulness of pHi as a variable that might trigger therapeutic interventions during resuscitation in critically ill patients. A measure of the adequacy of gastric perfusion as determined by gastric tonometry is particularly attractive because of the importance of gut in the pathophysiology of critical illness [18]. Various studies have demonstrated neurohormonal responses to critical illness shunt blood away from the gut, which can leave the gut inadequately perfused and the pHi low at the time when other indices of perfusion show that the resuscitation is adequate [17, 19, 20].
Patients in whom therapeutic interventions failed to correct a low gastric intramucosal pH at zero and at 12 hours had the highest mortality rate (88.6%). Survival improved in those patients where pHi increased within this period (34%). These observations are similar to Doglio et al [2], who observed 86.7% and 36.45% mortality in similar groups. Our study shows that the initial low pHi value carried a high mortality and has a positive out come if it is corrected within 24 hours. The overall mortality as predicted, on the basis of low pHi value did not improve significantly with resuscitative measures. Gastrointestinal mucosal acidosis has been documented in both clinical and experimental studies of septic shock. In septic patients, development of gastric mucosal acidosis correlates with early death and the development of the multiple organ dysfunctions [6, 7, 21].
The higher survival rate of patients with normal gastric intramucosal pH during first 12 hours in ICU makes a strong argument for using gastric intramucosal pH as a monitor of local tissue hypoxia [2]. Doglio et al [2], supported the hypothesis that a substantial proportion of ICU patients benefit from pHi monitoring. However, Gomersall et al [12] did not recommend routine use of titrated treatment against pHi in the management of critically ill patients.
We monitored PgCO2 and pHi after stopping feed for one hour as in the study by Marik [23]. The measurement of intramucosal pH following a sudden change in arterial bicarbonate such as that induced by an IV injection of bicarbonate should be delayed [15]. Thorburn et al [24], found that gastric feeding decreased the gastric intramucosal PCO2 and PgCO2-PaCO2 difference with increase in pHi as compared with the unfed state, contrary to those found in adult studies.
Sepsis is known to induce ischemia at a higher level of oxygen delivery than that induced in the absence of sepsis [18]. Similarly, endotoxins induce a decrease in intramucosal pH while flow to the gut is maintained at control levels. Fiddian-Green RG [4], concluded that indirect measurement of actual pHi provides a sensitive and specific index of tissue oxygenation. Temperature correction is not required in air-gas tonometer [25]. Silva et al [26], have shown that the effects of fluid challenge on gastric mucosal PCO2 are variable and related to baseline PCO2 gap rather than to systemic variables. Oud et al [27] studied the effects of resuscitation of patients with severe sepsis to conventional hemodynamic end points and normal blood lactate levels on post resuscitation sequential assessments of gastric intramucosal pH (pHi) and concluded that gastric intramucosal acidosis develops and persists for at least 48 hours in patients resuscitated from septic shock to conventional resuscitative end points, including the normalization of lactate levels. These regional changes were not reflected in corresponding changes in systemic acid-base and oxygen utilization variables. Direct determinations of pHi and therapy directed toward the resolution of splanchnic ischemia may be required to improve the outcome in these patients.
Our findings suggest correlation between the mortality prediction on the basis of pHi and PgCO2-EtCO2 gap and actual mortality in critically ill patients. Resuscitation done on the basis of pHi and PgCO2-EtCO2 definitely affects the outcome. Identification of different sub groups of patients will make the study more accurate. Inspite of shortcomings the study provides a basis for use of gastric tonometer in critically ill patients to predict the outcome and guide the therapy in sepsis.
Conflicts of Interest
This study was financed by research grant from the office of Director General Armed Forces Medical Services.
References
- 1.Meakins JL, Marshall JC. The gastrointestinal tract: the motor of MOF. Archives of Surgery. 1986;121:197–201. [Google Scholar]
- 2.Doglio GR, Pusajo JF. Gastric mucosal pH as a prognostic index of mortality in critically ill patients. Critical care medicine. 1991;19:1037–1040. doi: 10.1097/00003246-199108000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Friedman G, Berlot G. Combined measurement of blood lactate concentrations and gastric intramucosal pH in patients with severe sepsis. Critical care medicine. 1995;23:1184–1193. doi: 10.1097/00003246-199507000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Fiddian-Green RG. Gastric intramucosal pH, tissue oxygenation and acid-base balance. British Journal of Anaesthesia. 1995;74:591–606. doi: 10.1093/bja/74.5.591. [DOI] [PubMed] [Google Scholar]
- 5.Nelson DP, King CE. Systemic and intestinal limits of O2 extraction in the dog. Journal of Applied Physiology. 1987;63:387–394. doi: 10.1152/jappl.1987.63.1.387. [DOI] [PubMed] [Google Scholar]
- 6.Fink MP. Adequacy of gut oxygenation in endotoxaemia and sepsis. Critical Care Medicine. 1993;21:4–8. doi: 10.1097/00003246-199302001-00002. [DOI] [PubMed] [Google Scholar]
- 7.Drazenovic R, Samel RW. Regulation of perfused capillary density in canine intestinal mucosa during endotoxaemia. Journal of Applied Physiology. 1992;72:259–265. doi: 10.1152/jappl.1992.72.1.259. [DOI] [PubMed] [Google Scholar]
- 8.Thorburn K, Durward A, Tibby SM, Murdoch IA. Effects of feeding on gastric tonometric measurements in critically ill children. Crit Care Med. 2004;32:246–249. doi: 10.1097/01.CCM.0000104115.03922.AC. [DOI] [PubMed] [Google Scholar]
- 9.Higgins D, Mythen MG, Webb AR. Low intramucosal pHi is associated with failure to acidify the gastric lumen in response to pentagastrin. Intensive Care Medicine. 1994;20:105–108. doi: 10.1007/BF01707663. [DOI] [PubMed] [Google Scholar]
- 10.Fiddian-Green RG. Splanchnic ischemia and multiple organ failure in the critically ill. Annals of the Royal College of Surgeons of England. 1988;70:128–134. [PMC free article] [PubMed] [Google Scholar]
- 11.Hatherill M, Tibby SM. Gastric tonometry in septic shock. Arch Dis Child. 1998;78:155–158. doi: 10.1136/adc.78.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gomersall CD, Joyant GM, Freebairn RC. Resuscitation of critically ill patients based on the results of gastric tonometry: a perspective, randomized, controlled trail. Crit Care Med. 2000;28:607–614. doi: 10.1097/00003246-200003000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Donati A, Battisti D. Predictive value of interleukin 6 (IL -6) and gastric intramucosal pH in major abdominal surgery. Intensive Care Medicine. 1998;24:329–335. doi: 10.1007/s001340050575. [DOI] [PubMed] [Google Scholar]
- 14.Gomersall CD, Joynt GM, Ho KM. Gastric tonometry and prediction of outcome in the critically ill, Arterial to intramucosal pH gradient and carbon dioxide gradient. Anaesthesia. 1997;52:619–623. doi: 10.1111/j.1365-2044.1997.146-az0150.x. [DOI] [PubMed] [Google Scholar]
- 15.Marik PE. Gastric intramucosal pH is a better predictor of multiorgan dysfunction syndrome and death than oxygen derived variables in septic patients. Chest. 1993;104:225–229. doi: 10.1378/chest.104.1.225. [DOI] [PubMed] [Google Scholar]
- 16.Gys T, Hubbens A, Neels H. The prognostic value of gastric intramural pH in surgical intensive care patients. Critical Care Medicine. 1998;16:1222. doi: 10.1097/00003246-198812000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Santoso JT, Wisner DH. Comparison of gastric mucosal pH and clinical judgment in Critically ill Patients. Eur Journal of surgery. 1998;164:521–524. doi: 10.1080/110241598750005877. [DOI] [PubMed] [Google Scholar]
- 18.Deitch EA. The role of intestinal barrier failure and bacterial translocation in the development of systemic infection and MOF. Arch Surgery. 1990;125:403–404. doi: 10.1001/archsurg.1990.01410150125024. [DOI] [PubMed] [Google Scholar]
- 19.Chang MC. Gastric tonometry supplements information provided by systemic indicators of oxygen transport. J Trauma. 1994;37:488–494. doi: 10.1097/00005373-199409000-00026. [DOI] [PubMed] [Google Scholar]
- 20.Ivatury RR, Simon RJ. Gastric mucosal pH and oxygen delivery and oxygen consumption indices in the assessment of adequacy of resuscitation after trauma, a prospective randomized study. J Trauma. 1995;39:128–134. doi: 10.1097/00005373-199507000-00017. [DOI] [PubMed] [Google Scholar]
- 21.Casado-Flores J, Mora E, Perez-Corral F. Prognostic value of gastric intramucosal pH in critically ill children. Crit Care Med. 1998;26:1122–1127. doi: 10.1097/00003246-199806000-00039. [DOI] [PubMed] [Google Scholar]
- 22.Bone RC, Balk RA, Cerra FB. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992;101:1644–1655. doi: 10.1378/chest.101.6.1644. [DOI] [PubMed] [Google Scholar]
- 23.Marik PE. Effect of feeding on the measurement of gastric intramucosal pH. Crit Care Med. 1996;24:1498–1500. doi: 10.1097/00003246-199609000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Thorburn K, Durward A, Tibby SM, Murdoch IA. Effects of feeding on gastric tonometric measurements in critically ill children. Crit Care Med. 2004;32:246–249. doi: 10.1097/01.CCM.0000104115.03922.AC. [DOI] [PubMed] [Google Scholar]
- 25.Hiroshi D, Azuhiro AK. Effect of temperature on gastric intramucosal pCo2 measurement by saline and air tonometry. Journal of Anaesthesia. 2003;17:284–286. doi: 10.1007/s00540-003-0190-8. [DOI] [PubMed] [Google Scholar]
- 26.Silva E, De Backer D, Creteur J, Vincent JL. Effects of fluid challenge on gastric mucosal PCO2 in septic patients. Intensive Care Med. 2004;30:423–429. doi: 10.1007/s00134-003-2115-2. [DOI] [PubMed] [Google Scholar]
- 27.Oud L, Haupt MT. Persistent gastric intramucosal ischemia in patients with sepsis following resuscitation from shock. Chest. 1999;115:1390–1396. doi: 10.1378/chest.115.5.1390. [DOI] [PubMed] [Google Scholar]


