Abstract
Hepatitis C virus (HCV) is a highly diverse pathogen that is classified into seven distinct genotypes. Simultaneous or sequential reinfection with multiple HCV genotypes is recognized in high-risk populations, such as injecting drug users (IDUs). Multiple infection is of clinical concern as different genotypes have various sensitivities to current antiviral therapies. Therefore, a better understanding of the frequency of multiple infection and of the genotypes currently being transmitted is clinically relevant. An Australian cohort of IDUs (n = 123), identified with primary incident infection, was followed for multiple infection by regular HCV RNA testing between 2005 and 2013. A total of 354 samples were tested. Sequencing of primary incident infections revealed that genotype 3a was the most common circulating genotype, followed by genotype 1a. Examination of longitudinally collected samples identified complex patterns of multiple infection, including reinfection and superinfection. In those with multiple infection, there was no apparent evidence of homotypic immunity conferring protection against reinfection of the same subtype. This study revealed frequent multiple infection in a high-risk prisoner cohort, illustrating the complex nature of HCV infection and reinfection and highlighting the need for pan-genotypic antiviral therapies.
INTRODUCTION
Hepatitis C virus (HCV) is a major cause of chronic liver disease globally. Current estimates suggest that between 130 and 170 million people worldwide are infected with HCV and that more than 350,000 people die from HCV-related illnesses each year (1–3). In Australia, approximately 320,000 people are estimated to have been infected with HCV, with intravenous drug use (IVDU) being the predominant source of infections (4, 5).
Acute infection is asymptomatic in the majority of individuals and hence commonly remains undiagnosed during the initial phase of illness (6). Following acute infection, approximately 25% of people clear the virus within approximately 6 months, whereas the remainder progress to chronic infection (7). Chronic HCV infection causes ongoing hepatic inflammation resulting in fibrosis and, ultimately, cirrhosis and an increased risk of hepatocellular carcinoma, with an annual mortality rate of 1% to 4% (8, 9). As the virus is predominantly transmitted by blood-to-blood contact, those most at risk are injecting drug users (IDU), via sharing of the injecting apparatus. A recent study of recent HCV infections in Australian prisons identified evidence of ongoing HCV transmission events in incarcerated IDUs (10). Other blood-to-blood modes of transmission are also recognized, including transmission via contaminated medical devices such as tattooing instruments, vertical transmission from infected mothers to the newborn, and sexual transmission among men who have sex with men (MSM), particularly among those who are coinfected with HIV (11, 12).
HCV strains are highly diverse, with seven major genotypes (genotypes 1 to 7), each further classified into 67 subtypes (labeled alphabetically [a, b, c, etc.]) (13). HCV taxonomy is defined by nucleotide sequence heterogeneity, with the genotypes showing 65% to 70% sequence identity and the subtypes showing 75% to 80% homology (14). HCV genotyping was originally performed on the highly conserved 5′ untranslated region (5′UTR), but genotyping based on the Core and envelope (E1 and E2) structural regions has more recently been shown to provide better resolution of subtypes and transmission clusters (10, 15, 16).
HCV genotypes and subtypes are differentially distributed across the world, with genotypes 1, 2, and 3 being the most prevalent globally. Genotype 4 is prevalent in the Middle East and Africa, and high prevalences of genotypes 5 and 6 have been reported in South Africa and Asia, respectively (17, 18). The genotypes most commonly reported among chronically infected individuals in Australia are genotypes 1 (52% to 65%) and 3 (20% to 38%), with low prevalences of genotypes 2, 4, and 6 (approximately 5% to 9%, 0% to 6%, and 0.6% to 2%, respectively) (19–25). It should be noted, however, that these prevalence surveys were conducted in the 1990s and predominantly screened chronically infected individuals who had likely contracted the virus years to decades prior to testing; therefore, the results of those studies do not necessarily represent the viruses currently being transmitted (26). No other investigations have been conducted since those studies were performed over 2 decades ago.
Multiple infections (i.e., simultaneous or sequential infections with two or more HCV strains) are common, with reported prevalence rates in Australia ranging from 0.7% to 25% (16, 19, 20, 22, 25, 27). The highly diverse nature of HCV strains and limited cross-genotype protective immunity (28), in combination with the high risk of reexposure through ongoing IVDU, are believed to contribute to the occurrence of multiple infections. As the existing interferon-based therapies and many of the direct-acting antivirals (DAAs) have genotype-specific activity, recognition of multiple infection is important in clinical decision-making—for both treatment type and duration (29, 30).
In the present study, the genotype distribution among incident case subjects from a prospective cohort study of high-risk IDU custodial inmates in Australia was investigated to describe the current incident genotypes and subtypes. The frequency of multiple infection was also analyzed by subject and by sample, following up analyses performed in a study published in 2010 (16), with an additional 36 subjects and an extra 3 years of longitudinal sampling providing an additional 239 samples.
MATERIALS AND METHODS
Subjects and samples.
Samples from a prospective cohort of 500 HCV seronegative high-risk inmates enrolled in the Hepatitis C Incidence and Transmission Study in prisons (HITS-p) collected between 2005 and 2013 were used in this study (31–33). Inmates were enrolled in 34 correctional centers across New South Wales, Australia. Blood samples were collected every 6 months to screen for seroconversion and for HCV RNA positivity, and upon diagnosis of incident infection, three to six samples were collected monthly. Details of the study protocol were reported elsewhere (16, 31–33). Interviews regarding risk behaviors were conducted by a research nurse and entered into a database created in SPSS Statistics (for Windows, Version 22.0) (IBM Corp. Armonk, NY) along with HCV antibody (Ab) and HCV RNA test results as described previously (31–33).
Ethics statement.
Ethical approvals were obtained from the Human Research Ethics Committees of Justice Health (reference number GEN 31/05), the New South Wales Department of Corrective Services (reference number 05/0884), and the University of New South Wales (reference numbers 05094 and 08081), all located in Sydney, Australia. Written informed consent was obtained from the participants.
Virological assessments.
All sera were tested for HCV antibodies using the Abbott Architect anti-HCV chemiluminescent microparticle immunoassay (Abbott Diagnostics, Abbott Park, IL, USA). HCV RNA detection was performed using either the Versant HCV RNA qualitative transcription-mediated amplification (TMA) assay (Bayer Diagnostics, Emeryville, CA, USA) (lower limit of detection, 3,200 copies/ml) for samples collected prior to July 2008 or the Cobas AmpliPrep/Cobas TaqMan HCV assay (Roche, Branchburg, NJ, USA) (lower limit of detection, 223 genome copies/ml) for samples collected from August 2008 to June 2013 (34).
RNA extraction, genotyping, and screening for multiple infection.
Viral RNA was extracted from all viremic samples, and screening for multiple infection was accomplished by amplifying the Core region with subtype-specific nested reverse transcriptase PCR (nRT-PCR) for subtype 1a, 1b, 2a, or 3a, as previously described (16). If the Core region failed to amplify, nRT-PCR analysis was performed to amplify E1/hypervariable region 1 as previously described (16, 25). If both Core and E1/HVR1 failed to amplify, the 5′UTR region was analyzed to determine the genotype (25). All PCR amplicons were purified with ExoSAP-IT (Affymetrix) and sequenced directly on an ABI 3730 DNA analyzer (Applied Biosystems) using dye terminator chemistry. The GenBank accession numbers for E1/HVR1 are KJ437271 to KJ437343.
E1/HVR1 nRT-PCR for detection of multiple infection with two viruses from the same subtype.
When the Core and/or 5′UTR sequences indicated a potential reinfection with the same subtype (e.g., 3a-3a), nRT-PCR analysis targeting the E1/HVR1 region was performed, as previously described (16). Longitudinal analysis of the sequence data was used to confirm a subtype reinfection. Where the sequences did not cluster (70% bootstrap cutoff for clusters), a new subtype infection was confirmed (35).
Phylogenetic analysis.
Phylogenetic analysis was used to determine genotype and subtype as well as to determine potential secondary infection with the same subtype. This analysis was performed with the inclusion of a panel of prototypic sequences that were retrieved from GenBank (13, 16) (see Fig. S1 in the supplemental material for GenBank accession numbers) representing each of the 67 HCV subtypes. Alignments of the prototypic sequences and the nucleotide sequences generated from the HITS-p cohort were performed using the Clustal W program in the MEGA5 software package (13, 36). To determine genotype, phylogenetic analysis was performed on three different genomic regions—the Core region, with amplicon lengths of 270 bp; the E1/HVR1 region, spanning 657 bp; or the 5′UTR region, spanning 175 bp. Best-fit substitution models were determined using the MEGA 5 model test. Trees were constructed from Core and 5′UTR sequences using a Kimura 2-parameter model with gamma distribution for all genotypes and from E1/HVR1 sequences using a Tamura-Nei model with gamma distribution. Evolutionary history was inferred using the maximum likelihood method (bootstrap test of 1,000 replications; 70% cutoff for clusters) (36). As 5′UTR subtyping of genotype 1 is problematic because of the highly conserved nature of this region, subtype 1a and 1b sequences were determined on nucleotide 243. This nucleotide is known to differ in the 1a and 1b sequences, with an A and G, respectively (25). Trees were visualized with FigTree (37).
Definitions.
“Multiple infection” was defined as the condition of either simultaneous or sequential infection of a subject with two or more strains of HCV. As previously described, multiple infection was further classified into “incident mixed infection,” where the subject was infected with two or more strains at the first viremic time point; “superinfection,” where the subject became infected with a second strain of HCV superimposed on a previous infection strain; and “reinfection,” where a subject was infected with one strain of virus, cleared that virus (with at least one aviremic time point), and then became infected with another, phylogenetically distinct viral strain (16). “Strain switch” was designated when a different strain of virus was detected in longitudinal follow-up but the presence or absence of viremia during the intervening period had not been established.
Statistical analysis.
Descriptive analyses of the demographic and risk behavior characteristics of the subject group were conducted using SPSS Statistics (Version 22.0; IBM Corp., Armonk, NY). The R statistical package was used to perform a two-tailed one-sample z test for equal proportions on genotype and multiple infection intrasubtype data to investigate possible homotypic immunity (38).
RESULTS
Subject and sample characteristics.
Of the 500 subjects enrolled in the HITS-p cohort, there were 182 subjects with documented seroconversion who were included in the incident case group. Of these 182 incident subjects, HCV RNA was detectable in 136 (75%). A further 13 viremic subjects were excluded from further analysis for a range of reasons, including the lack of a stored sample, a viral load of <15 IU/ml, and collection of samples in lithium heparin as the anticoagulant. There were 123 primary incident case subjects (90%) who had at least one viremic time point available and were suitable for subsequent genotyping and sequence analysis. Of these 123, 32 had only one viremic time point, while the remaining 91 had at least two viremic time points, making a total of 354 samples available for analysis. Three different regions of the HCV genome, 5′UTR, Core, and E1/HVR1, were targeted for amplification and sequencing. In total, 97% (n = 342) of the viremic samples were successfully amplified and sequenced for at least one region. Including all multiple infections, there were 518 sequences generated, comprising n = 32 (6%) 5′UTR, n = 307 (59%) Core, and n = 179 (35%) E1/HVR1 sequences.
The demographic characteristics of the 123 primary incident case subjects revealed that 79 (64%) were male, with an overall mean age of 27.6 years (standard deviation [SD], 6.7), and that 98 (80%) subjects had attained less than 10 years of formal education. The majority of subjects reported previous imprisonment (78%) and also a high lifetime frequency of sharing of injecting equipment (67%). Over half (53%) of the subjects reported injecting drugs since imprisonment.
Genotype characterization of primary incident HCV.
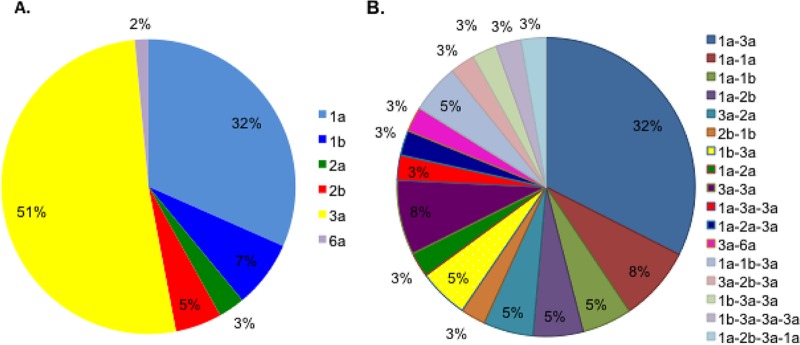
To determine the genotypes currently in circulation throughout New South Wales (NSW) prisons, the genotype(s) was determined at the first HCV RNA-positive time point for each of the 123 incident case subjects. There were 136 primary incident viruses, including 110 “monoinfections” (i.e., infections with one virus only) and 26 primary incident mixed infections in 13 subjects, 5 of whom were assigned to two or more of the multiple infection classification patterns described below. Of these 136 primary incident viruses, 39% (n = 53) were genotype 1, which included 32% (n = 43) with subtype 1a infection and 7% (n = 10) with subtype 1b infection (Fig. 1). The genotype 3 infections (n = 70) were uniformly subtype 3a infections and made up 51% of all primary incident viruses. Primary genotype 2 infections (n = 11) included subtypes 2a and 2b, comprising 3% (n = 4) and 5% (n = 7), respectively. Genotype 6a infections constituted 2% of primary incident infections (n = 2), whereas genotypes 4, 5, and 7 were not detected.
FIG 1.
Distribution of HCV subtypes and multiple-infection combinations. (A) Distribution of subtypes in the primary incident HCV infection samples in the cohort, with different subtypes represented by different colors as shown in the key. (B) A varied set of multiple-infection combinations were observed. Each multiple-infection combination is represented by a different color as shown in the key, with the percentage of each set as a proportion of the total also represented.
Characterization of multiple infections by subject.
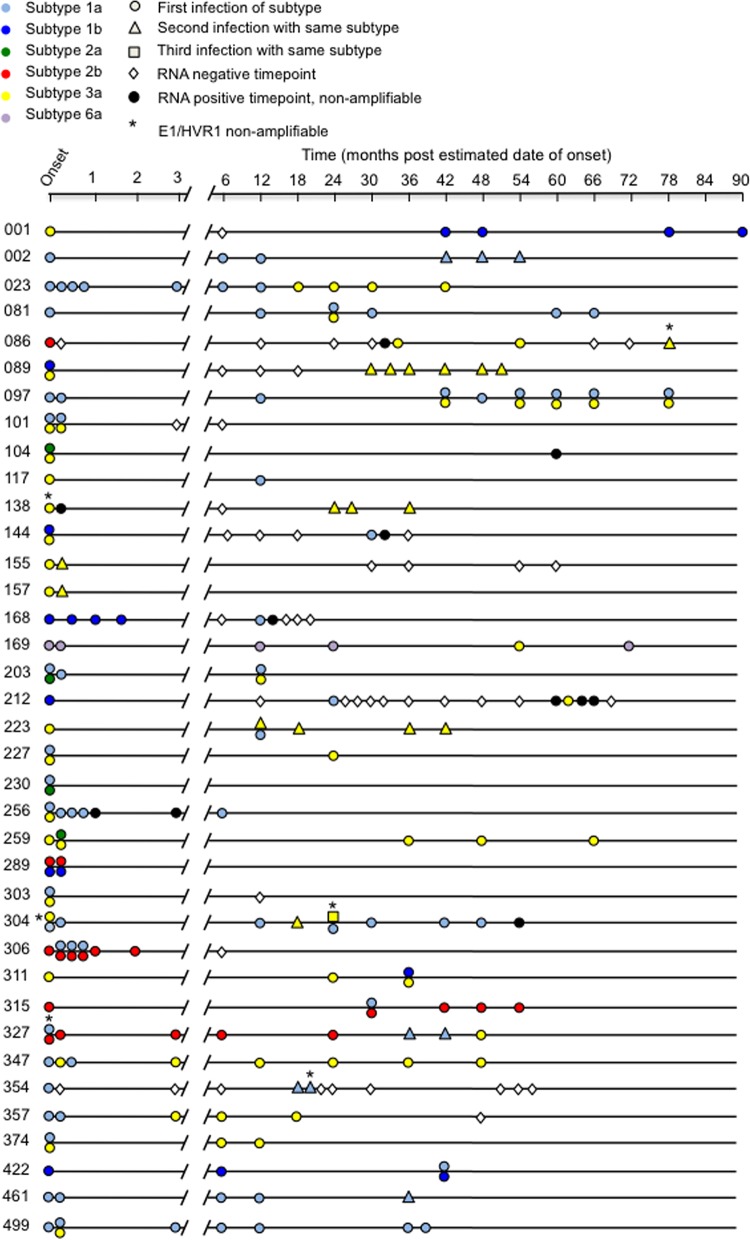
Of the 123 subjects whose viremic samples were genotyped using Core, E1/HVR1, and 5′UTR, 70% (n = 86) of subjects were found to be infected with one virus only, termed here “monoinfection,” and the remaining 30% (n = 37) were confirmed to have multiple infection (including incident mixed infection as described above). Of the 37 subjects with multiple infections, 49% (n = 18) were multiply infected with subtypes 1a and 3a—termed here “intergenotype multiple infection.” However, a wide range of combinations was evident (Fig. 1). Interestingly, 11 (30%) of the 37 subjects had multiple infection with the same subtype—termed here “intrasubtype multiple infection” (Fig. 1). Of these 11 subjects, seven were infected with two subtype 3a viruses (19% of the total multiple infection group) and four were infected with two 1a subtype viruses (11% of the total multiple infection group). It should be noted that, for four subjects (Fig. 2; subject identifiers 138, 304, 327, and 354), Core sequence clustering showed intrasubtype infection, but, because of superinfection with other genotypes or low viral loads at these time points, the E1/HVR1 region could not be amplified for these viruses. These subjects were included as intrasubtype infections (Fig. 2 [identified with asterisks]). For subject 086, only the 5′UTR from each infection was able to be amplified. This subject was included because there were two HCV RNA-negative time points seen over an 18-month period (Fig. 2 [identified with asterisks]) (28). Surprisingly, six of the subjects in the cohort were infected with three viruses (Fig. 2; subject identifiers 144, 212, 203, 086, 089, and 223) and another two subjects with four viruses (Fig. 2; subject identifiers 327 and 304).
FIG 2.
Multiple-infection subjects. Data are shown for 37 subjects identified as having multiple infection. The line represents a longitudinal time scale from incident infection to the last sampling point in months. The color symbol designates the subtype; first, second, and third infections with the same subtype are represented with circles, triangle, and squares, respectively. Time points representing subjects with viremia from whom a sequence was unobtainable are designated in black, time points representing subjects from whom E1/HVR1 was unable to be amplified are designated with an asterisk, and time points representing RNA-negative results are represented by an empty diamond with a black outline. Time points where two viral strains were present have two symbols indicated (see key).
The multiple-infection episodes for 30 of the 37 subjects followed four different patterns defined as follows: (i) eight subjects (22%) were classified as having primary incident mixed infection, as two distinct HCV strains were detected at the first HCV RNA-positive time point; (ii) 5 subjects (13%) were classified as having “reinfection,” as observed from longitudinal follow-up; (iii) 10 subjects (27%) were classified as having superinfection; and, finally, (iv) 7 subjects (19%) were designated strain switch subjects, as the incident HCV strain was replaced by a second strain with no intervening time points negative for infection. The remaining 7 of the 37 multiply infected subjects displayed a complex history of infection that encompassed two or more different pattern designations (Fig. 2; subject identifiers 086, 089, 144, 203, 223, 304, and 327).
Analysis of intrasubtype infections.
It was of interest to determine if the likelihood of infection with a second virus from the same subtype was lower than the likelihood of a second infection with a different subtype/genotype, thereby suggesting homotypic immunity. If it is assumed that no protection was conferred from the primary infection and that each infection was entirely independent, then the chance of a second infection with genotype 3a should have been approximately the same as that of a primary infection (i.e., 51%), with the potential caveat of differential clearance of one strain over another resulting in aviremia and no sample available for amplification. The expected probability of a subsequent infection being a genotype 3a infection, given that the initial infection was a genotype 3a infection, would be 26% (0.51 × 0.51); thus, 26% of the multiple-infection cohort should have had 3a-3a infections. This expected proportion of 3a-3a infections was compared with the observed proportion (7/34 = 21%; P = 0.6), indicating no statistically significant difference. A similar analysis performed for genotype 1a infections revealed that the expected rate of 10% of 1a intrasubtype infections (0.32 × 0.32) was closely concordant with the observed rate of 4/34 (12%) (P = 1.0).
Spontaneous clearance.
Of the 86 monoinfected subjects, longitudinal follow-up allowed assessment of disease outcome (clearance or chronicity) in 57 subjects. The remaining 29 subjects lacked longitudinal samples to determine clearance or chronicity and therefore were classified as having unresolved infections. At least 6 months of follow-up was required to define infection outcome. Of the 57 subjects with sufficient longitudinal follow-up, 19% (n = 11) cleared the virus and 81% (n = 46) progressed to chronic infection. This clearance rate is comparable to the clearance rate of monoinfected subjects seen in other studies (7, 39). In contrast, reinfection subjects showed a high rate of spontaneous clearance, with 5 of 8 (63%) subjects clearing two or more viruses. In 19 (80%) of the 24 subjects with superinfection and incident mixed infection, either two viruses were eventually cleared or one virus superseded another and persisted (Fig. 2). Only one (4%) subject (Fig. 2; subject identifier 097) developed infection with two viruses for a period greater than 6 months and did not clear either virus in follow-up. The remaining four (17%) of the 24 subjects did not have sufficient follow-up time points to determine the outcome of infection.
In the subjects with multiple infection, there was an apparent pattern of shortened duration of infection. In the eight subjects who developed reinfection, 50% had at least one reinfection that lasted no longer than 4 weeks from detection.
DISCUSSION
In this study, a sensitive nRT-PCR-based assay was used to describe the distribution of HCV genotypes and the frequency of multiple infections among incident infections in an Australian custodial setting. Previous prevalence surveys of chronic HCV infection in Australia between 1997 and 2000 resulted in reported ranges of 20% to 38% for genotype 3 and 52% to 65% for genotype 1 (18–24). In contrast to those studies, the findings reported here indicate an apparent increase in the transmission of genotype 3 (51% of incident infections).
This report of an increased frequency of genotype 3 infection is consistent with a comparable trend in prevalent genotype data comparing studies from several decades ago to more recent cross-sectional studies (40–42). One possible explanation for the emergence of genotype 3 infection is that this strain has been reported to have a reduced likelihood of spontaneous clearance in primary infection compared to genotype 1 and, accordingly, a higher rate in the establishment of chronic infection. Consequently, it is hypothesized that the increasing pool of genotype 3-infected donors is associated with an increased likelihood of genotype 3 transmissions. The increased prevalence of genotype 3 infection raises long-term clinical concerns, as chronic infection with genotype 3 has been associated with an increased risk of cirrhosis and hepatocellular carcinoma (HCC) compared to chronic infection with genotype 1 (7, 43). In addition, the current DAAs are less effective against genotype 3 (44, 45).
The frequency of multiple infections in this study (30%) was at the higher end of the scale but was still comparable to those calculated in other studies in high-risk cohorts, confirming that repeated infection is common in these populations and is of clinical concern (46, 47). It should also be noted that the data presented here were based on the use of a sensitive, subtype-specific assay system for detection of multiple infections which also incorporated both longitudinal time points and a relatively large sample size. This more comprehensive analysis may explain the higher rate of multiple infection seen in this study compared to others (19, 20, 22, 25, 48). It is also worth noting that this cohort was analyzed using samples collected in the custodial setting, which may impose risk factors that are different from rates of mixed infection that are higher than those seen with IDUs based in the community (16).
To date, there has been limited investigation of antiviral immunity in multiple-infection subjects. Clearance rates have been reported to improve from 25% to 59% in people with secondary infections (28). One recent study, examining adaptive immunity in reinfections, found a significant increase in the breadth of T cell responses. In the majority of reinfected IDUs, a heterologous neutralizing antibody (nAb) response was formed (49). While examination of the immune response was beyond the scope of this study, a trend toward more-transient infection, as well as a higher rate of spontaneous clearance in those with multiple infection, was observed and is consistent with other studies (28, 50, 51). Interestingly, the rates of intrasubtype 3a-3a and 1a-1a multiple infections were comparable in frequency to the primary infection rates. This suggests that very little sterilizing immunity against related subtypes is generated. These results differ from the results of a recently published paper that reported a decreased risk for acquisition of a secondary infection from the same subtype (52). The difference in intrasubtype infection results could be a consequence of the fact that this study implemented a highly sensitive genotyping assay designed to detect multiple infection in a single sample (16). In combination, these data suggest that the host response during an initial infection does not prevent subsequent infection but does facilitate better control upon reinfection. This implies that prophylactic vaccine design will need to focus more on facilitating rapid clearance of HCV infection rather than on inducing sterilizing immunity.
The limitations of the current study included a wide range in sampling frequencies (2 weeks to 6 months), which may have resulted in some infection episodes being undetected if they were cleared quickly (49, 53). This is likely to be relevant in the subjects with strain switch, where a lack of an intermediate time point with either superinfection or a negative RNA outcome might have better resolved the multiple infection category of these infections.
Summary.
This report indicates that the HCV epidemic in Australia is mirroring the global increase in genotype 3 infections and that multiple infection is common in high-risk populations. This study was the most intensive longitudinal analysis of multiple infection conducted to date, and the results indicate a high prevalence of multiple infection with complex patterns of natural history. For high-risk populations, pan-genotypic DAA treatment options and vaccination will likely be needed in combination, with a view to long-term elimination.
Supplementary Material
ACKNOWLEDGMENTS
The HITS-p investigators include Kate Dolan, Paul Haber, William Rawlinson, Carla Treloar, Greg Dore, Lisa Maher, Andrew Lloyd, and Fabio Luciani.
This work was supported by grants from National Health and Medical Research Council of Australia, including NSW Health, Justice Health, and Corrective Services NSW as partners (grant no. 222887 and 1016351), and by a National Health and Medical Research Council of Australia Practitioner Fellowship (no. 1043067 to A.R.L.). R.A.B. is supported by a NHMRC Career Development Fellowship (no. APP1084706).
Footnotes
Supplemental material for this article may be found at http://dx.doi.org/10.1128/JCM.00287-16.
REFERENCES
- 1.Hatzakis A, Chulanov V, Gadano AC, Bergin C, Ben-Ari Z, Mossong J, Schreter I, Baatarkhuu O, Acharya S, Aho I, Anand AC, Andersson MI, Arendt V, Arkkila P, Barclay K, Bessone F, Blach S, Blokhina N, Brunton CR, Choudhuri G, Cisneros L, Croes EA, Dahgwahdorj YA, Dalgard O, Daruich JR, Dashdorj NR, Davaadorj D, de Knegt RJ, de Vree M, Estes C, Flisiak R, Gane E, Gower E, Halota W, Henderson C, Hoffmann P, Hornell J, Houlihan D, Hrusovsky S, Jarcuska P, Kershenobich D, Kostrzewska K, Kristian P, Leshno M, Lurie Y, Mahomed A, Mamonova N, Mendez-Sanchez N, Norris S, et al. 2015. The present and future disease burden of hepatitis C virus (HCV) infections with today's treatment paradigm—volume 2. J Viral Hepat 22(Suppl 1):26–45. doi: 10.1111/jvh.12351. [DOI] [PubMed] [Google Scholar]
- 2.Hajarizadeh B, Grebely J, Dore GJ. 2013. Epidemiology and natural history of HCV infection. Nat Rev Gastroenterol Hepatol 10:553–562. doi: 10.1038/nrgastro.2013.107. [DOI] [PubMed] [Google Scholar]
- 3.Saraswat V, Norris S, de Knegt RJ, Sanchez Avila JF, Sonderup M, Zuckerman E, Arkkila P, Stedman C, Acharya S, Aho I, Anand AC, Andersson MI, Arendt V, Baatarkhuu O, Barclay K, Ben-Ari Z, Bergin C, Bessone F, Blach S, Blokhina N, Brunton CR, Choudhuri G, Chulanov V, Cisneros L, Croes EA, Dahgwahdorj YA, Dalgard O, Daruich JR, Dashdorj NR, Davaadorj D, de Vree M, Estes C, Flisiak R, Gadano AC, Gane E, Halota W, Hatzakis A, Henderson C, Hoffmann P, Hornell J, Houlihan D, Hrusovsky S, Jarcuska P, Kershenobich D, Kostrzewska K, Kristian P, Leshno M, Lurie Y, Mahomed A, Mamonova N, et al. 2015. Historical epidemiology of hepatitis C virus (HCV) in select countries—volume 2. J Viral Hepat 22(Suppl 1):6–25. doi: 10.1111/jvh.12350. [DOI] [PubMed] [Google Scholar]
- 4.Hepatitis C Virus Projections Working Group. 2006. Estimates and projections of the hepatitis C virus epidemic in Australia 2006. Hepatitis C Sub-Committee, Ministerial Advisory Committee on AIDS Sexual Health and Hepatitis, Canberra, Australia. [Google Scholar]
- 5.The Kirby Institute UNSW. 2014. HIV, viral hepatitis and sexually transmissible infections in Australia. Annual surveillance report. The Kirby Institute UNSW, Sydney, NSW, Australia. [Google Scholar]
- 6.Ascione A, Tartaglione T, Di Costanzo GG. 2007. Natural history of chronic hepatitis C virus infection. Dig Liver Dis 39(Suppl 1):S4–S7. doi: 10.1016/S1590-8658(07)80003-X. [DOI] [PubMed] [Google Scholar]
- 7.Grebely J, Page K, Sacks-Davis R, van der Loeff MS, Rice TM, Bruneau J, Morris MD, Hajarizadeh B, Amin J, Cox AL, Kim AY, McGovern BH, Schinkel J, George J, Shoukry NH, Lauer GM, Maher L, Lloyd AR, Hellard M, Dore GJ, Prins M; InC3 Study Group. 2014. The effects of female sex, viral genotype, and IL28B genotype on spontaneous clearance of acute hepatitis C virus infection. Hepatology 59:109–120. doi: 10.1002/hep.26639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grebely J, Grady B, Hajarizadeh B, Page K, Dore GJ; INC3 Study Group . 18 February 2013. Disease progression during advanced fibrosis: IL28B genotype or HCV RNA levels? Hepatology doi: 10.1002/hep.26675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seeff LB. 2002. Natural history of chronic hepatitis C. Hepatology 36(Suppl 1):S35–S46. doi: 10.1053/jhep.2002.36806. [DOI] [PubMed] [Google Scholar]
- 10.Bretaña NA, Boelen L, Bull R, Teutsch S, White PA, Lloyd AR, Luciani F; HITS-p investigators . 2015. Transmission of hepatitis C virus among prisoners, Australia, 2005–2012. Emerg Infect Dis 21:765–774. doi: 10.3201/eid2105.141832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Law MG, Dore GJ, Bath N, Thompson S, Crofts N, Dolan K, Giles W, Gow P, Kaldor J, Loveday S, Powell E, Spencer J, Wodak A. 2003. Modelling hepatitis C virus incidence, prevalence and long-term sequelae in Australia, 2001. Int J Epidemiol 32:717–724. doi: 10.1093/ije/dyg101. [DOI] [PubMed] [Google Scholar]
- 12.Sy T, Jamal MM. 2006. Epidemiology of hepatitis C virus (HCV) infection. Int J Med Sci 3:41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith DB, B J, Kuiken C, Muerhoff AS, Rice CM, Stapleton JT, Simmonds P. 20 December 2013. Expanded classification of hepatitis C virus into 7 genotypes and 67 subtypes: updated criteria and genotype assignment web resource. Hepatology doi: 10.1002/hep.26744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simmonds P, Bukh J, Combet C, Deleage G, Enomoto N, Feinstone S, Halfon P, Inchauspe G, Kuiken C, Maertens G, Mizokami M, Murphy DG, Okamoto H, Pawlotsky JM, Penin F, Sablon E, Shin IT, Stuyver LJ, Thiel HJ, Viazov S, Weiner AJ, Widell A. 2005. Consensus proposals for a unified system of nomenclature of hepatitis C virus genotypes. Hepatology 42:962–973. doi: 10.1002/hep.20819. [DOI] [PubMed] [Google Scholar]
- 15.Lamoury FM, Jacka B, Bartlett S, Bull RA, Wong A, Amin J, Schinkel J, Poon AF, Matthews GV, Grebely J, Dore GJ, Applegate TL. 2015. The influence of hepatitis C virus genetic region on phylogenetic clustering analysis. PLoS One 10:e0131437. doi: 10.1371/journal.pone.0131437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pham ST, Bull RA, Bennett JM, Rawlinson WD, Dore GJ, Lloyd AR, White PA. 2010. Frequent multiple hepatitis C virus infections among injection drug users in a prison setting. Hepatology 52:1564–1572. doi: 10.1002/hep.23885. [DOI] [PubMed] [Google Scholar]
- 17.Yusim K, Fischer W, Yoon H, Thurmond J, Fenimore PW, Lauer G, Korber B, Kuiken C. 2010. Genotype 1 and global hepatitis C T-cell vaccines designed to optimize coverage of genetic diversity. J Gen Virol 91:1194–1206. doi: 10.1099/vir.0.017491-0. [DOI] [PubMed] [Google Scholar]
- 18.Messina JP, Humphreys I, Flaxman A, Brown A, Cooke GS, Pybus OG, Barnes E. 2015. Global distribution and prevalence of hepatitis C virus genotypes. Hepatology 61:77–87. doi: 10.1002/hep.27259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaba S, Dutta U, Byth K, Crewe EB, Khan MH, Coverdale SA, Lin R, Liddle C, Farrell GC. 1998. Molecular epidemiology of hepatitis C in Australia. J Gastroenterol Hepatol 13:914–920. doi: 10.1111/j.1440-1746.1998.tb00761.x. [DOI] [PubMed] [Google Scholar]
- 20.McCaw R, Moaven L, Locarnini SA, Bowden DS. 1997. Hepatitis C virus genotypes in Australia. J Viral Hepat 4:351–357. doi: 10.1046/j.1365-2893.1997.00060.x. [DOI] [PubMed] [Google Scholar]
- 21.Mison LM, Young IF, O'Donoghue M, Cowley N, Thorlton N, Hyland CA. 27 February 2003. Prevalence of hepatitis C virus and genotype distribution in an Australian volunteer blood donor population. Transfusion doi: 10.1046/j.1537-2995.1997.37197176954.x. [DOI] [PubMed] [Google Scholar]
- 22.Chen J, McGuinness PH, Koorey DJ, Rickard K, Wylie B, McCaughan GW. 1997. Hepatitis C virus genotypes in a cohort of Australian blood donors and haemophiliac and liver transplant patients. J Gastroenterol Hepatol 12:182–187. doi: 10.1111/j.1440-1746.1997.tb00404.x. [DOI] [PubMed] [Google Scholar]
- 23.Baker RI, Smith J, Eikelboom J, Leahy B, Kay I, Lavis N, Palladino S, Cheng W, Price J, Mews C. 1996. Hepatitis C genotypes in Australian haemophilia patients. Aust N Z J Med 26:789–792. doi: 10.1111/j.1445-5994.1996.tb00626.x. [DOI] [PubMed] [Google Scholar]
- 24.Hollander A, Glaumann H, Weiland O. 2004. Histological findings, genotype distribution and percentage of patients fulfilling the treatment criteria among patients with chronic hepatitis C virus infection in a single Swedish centre. Scand J Gastroenterol 39:164–167. doi: 10.1080/00365520310008115. [DOI] [PubMed] [Google Scholar]
- 25.White PA, Zhai X, Carter I, Zhao Y, Rawlinson WD. 2000. Simplified hepatitis C virus genotyping by heteroduplex mobility analysis. J Clin Microbiol 38:477–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Freeman AJ, Zekry A, Whybin LR, Harvey CE, van Beek IA, de Kantzow SL, Rawlinson WD, Boughton CR, Robertson PW, Marinos G, Lloyd AR. 2000. Hepatitis C prevalence among Australian injecting drug users in the 1970s and profiles of virus genotypes in the 1970s and 1990s. Med J Aust 172:588–591. [DOI] [PubMed] [Google Scholar]
- 27.Grebely J, Pham ST, Matthews GV, Petoumenos K, Bull RA, Yeung B, Rawlinson W, Kaldor J, Lloyd A, Hellard M, Dore GJ, White PA; ATAHC Study Group . 2012. Hepatitis C virus reinfection and superinfection among treated and untreated participants with recent infection. Hepatology 55:1058–1069. doi: 10.1002/hep.24754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sacks-Davis R, Aitken CK, Higgs P, Spelman T, Pedrana AE, Bowden S, Bharadwaj M, Nivarthi UK, Suppiah V, George J, Grebely J, Drummer HE, Hellard M. 2013. High rates of hepatitis C virus reinfection and spontaneous clearance of reinfection in people who inject drugs: a prospective cohort study. PLoS One 8:e80216. doi: 10.1371/journal.pone.0080216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Poordad F, Dieterich D. 2012. Treating hepatitis C: current standard of care and emerging direct-acting antiviral agents. J Viral Hepat 19:449–464. doi: 10.1111/j.1365-2893.2012.01617.x. [DOI] [PubMed] [Google Scholar]
- 30.Jaroszewicz J, Flisiak R, Dusheiko G. 2014. A pill for HCV—myth or foreseeable future? Liver Int 34:6–11. doi: 10.1111/liv.12294. [DOI] [PubMed] [Google Scholar]
- 31.Teutsch S, Luciani F, Scheuer N, McCredie L, Hosseiny P, Rawlinson W, Kaldor J, Dore GJ, Dolan K, Ffrench R, Lloyd A, Haber P, Levy M. 2010. Incidence of primary hepatitis C infection and risk factors for transmission in an Australian prisoner cohort. BMC Public Health 10:633. doi: 10.1186/1471-2458-10-633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Luciani F, Bretaña NA, Teutsch S, Amin J, Topp L, Dore GJ, Maher L, Dolan K, Lloyd AR; HITS-p investigators . 2014. A prospective study of hepatitis C incidence in Australian prisoners. Addiction 109:1695–1706. doi: 10.1111/add.12643. [DOI] [PubMed] [Google Scholar]
- 33.Dolan K, Teutsch S, Scheuer N, Levy M, Rawlinson W, Kaldor J, Lloyd A, Haber P. 2010. Incidence and risk for acute hepatitis C infection during imprisonment in Australia. Eur J Epidemiol 25:143–148. doi: 10.1007/s10654-009-9421-0. [DOI] [PubMed] [Google Scholar]
- 34.Al Olaby RR, Azzazy HM. 2011. Hepatitis C virus RNA assays: current and emerging technologies and their clinical applications. Expert Rev Mol Diagn 11:53–64. doi: 10.1586/erm.10.101. [DOI] [PubMed] [Google Scholar]
- 35.Felsenstein J. 1985. Confidence limits on phylogenies with a molecular clock. Syst Zool 34:152–161. doi: 10.2307/2413323. [DOI] [Google Scholar]
- 36.Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. 2011. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol Biol Evol 28:2731–2739. doi: 10.1093/molbev/msr121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guindon S, Gascuel O. 2003. A simple, fast, and accurate algorithm to estimate large phylogenies by maximum likelihood. Syst Biol 52:696–704. doi: 10.1080/10635150390235520. [DOI] [PubMed] [Google Scholar]
- 38.R Development Core Team. 2010. A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.r-project.org/.
- 39.Micallef JM, Kaldor JM, Dore GJ. 2006. Spontaneous viral clearance following acute hepatitis C infection: a systematic review of longitudinal studies. J Viral Hepat 13:34–41. doi: 10.1111/j.1365-2893.2005.00651.x. [DOI] [PubMed] [Google Scholar]
- 40.Pawlotsky JM, Benchiki H, Pellet C, Duval J, Dhumeaux D, Revuz J, Bagot M. 1995. Lichen planus and hepatitis C virus (HCV)-related chronic hepatitis: evaluation of HCV genotypes. Br J Dermatol 133:666–667. doi: 10.1111/j.1365-2133.1995.tb02734.x. [DOI] [PubMed] [Google Scholar]
- 41.Berger A, Doerr HW, Scharrer I, Weber B. 1997. Follow-up of four HIV-infected individuals after administration of hepatitis C virus and GBV-C/hepatitis G virus contaminated intravenous immunoglobulin: evidence for HCV but not for GBV-C/HGV transmission. J Med Virol 53:25–30. [PubMed] [Google Scholar]
- 42.Martinot-Peignoux M, Roudot-Thoraval F, Mendel I, Coste J, Izopet J, Duverlie G, Payan C, Pawlotsky JM, Defer C, Bogard M, Gerolami V, Halfon P, Buisson Y, Fouqueray B, Loiseau P, Lamoril J, Lefrere JJ, Marcellin P. 1999. Hepatitis C virus genotypes in France: relationship with epidemiology, pathogenicity and response to interferon therapy. The GEMHEP. J Viral Hepat 6:435–443. doi: 10.1046/j.1365-2893.1999.00187.x. [DOI] [PubMed] [Google Scholar]
- 43.Kanwal F, Hoang T, Kramer JR, Asch SM, Goetz MB, Zeringue A, Richardson P, El-Serag HB. 2011. Increasing prevalence of HCC and cirrhosis in patients with chronic hepatitis C virus infection. Gastroenterology 140:1182–1188 e1181. doi: 10.1053/j.gastro.2010.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jacobson IM, Gordon SC, Kowdley KV, Yoshida EM, Rodriguez-Torres M, Sulkowski MS, Shiffman ML, Lawitz E, Everson G, Bennett M, Schiff E, Al-Assi MT, Subramanian GM, An D, Lin M, McNally J, Brainard D, Symonds WT, McHutchison JG, Patel K, Feld J, Pianko S, Nelson DR; POSITRON Study; FUSION Study . 2013. Sofosbuvir for hepatitis C genotype 2 or 3 in patients without treatment options. N Engl J Med 368:1867–1877. doi: 10.1056/NEJMoa1214854. [DOI] [PubMed] [Google Scholar]
- 45.Lawitz E, Mangia A, Wyles D, Rodriguez-Torres M, Hassanein T, Gordon SC, Schultz M, Davis MN, Kayali Z, Reddy KR, Jacobson IM, Kowdley KV, Nyberg L, Subramanian GM, Hyland RH, Arterburn S, Jiang D, McNally J, Brainard D, Symonds WT, McHutchison JG, Sheikh AM, Younossi Z, Gane EJ. 2013. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med 368:1878–1887. doi: 10.1056/NEJMoa1214853. [DOI] [PubMed] [Google Scholar]
- 46.van de Laar TJ, Molenkamp R, van den Berg C, Schinkel J, Beld MG, Prins M, Coutinho RA, Bruisten SM. 2009. Frequent HCV reinfection and superinfection in a cohort of injecting drug users in Amsterdam. J Hepatol 51:667–674. doi: 10.1016/j.jhep.2009.05.027. [DOI] [PubMed] [Google Scholar]
- 47.Aitken CK, Lewis J, Tracy SL, Spelman T, Bowden DS, Bharadwaj M, Drummer H, Hellard M. 2008. High incidence of hepatitis C virus reinfection in a cohort of injecting drug users. Hepatology 48:1746–1752. doi: 10.1002/hep.22534. [DOI] [PubMed] [Google Scholar]
- 48.Aitken C, McCaw R, Jardine D, Bowden S, Higgs P, Nguyen O, Crofts N, Hellard M. 2004. Change in hepatitis C virus genotype in injecting drug users. J Med Virol 74:543–545. doi: 10.1002/jmv.20212. [DOI] [PubMed] [Google Scholar]
- 49.Osburn WO, Fisher BE, Dowd KA, Urban G, Liu L, Ray SC, Thomas DL, Cox AL. 2010. Spontaneous control of primary hepatitis C virus infection and immunity against persistent reinfection. Gastroenterology 138:315–324. doi: 10.1053/j.gastro.2009.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Laskus T, Wang LF, Radkowski M, Vargas H, Nowicki M, Wilkinson J, Rakela J. 2001. Exposure of hepatitis C virus (HCV) RNA-positive recipients to HCV RNA-positive blood donors results in rapid predominance of a single donor strain and exclusion and/or suppression of the recipient strain. J Virol 75:2059–2066. doi: 10.1128/JVI.75.5.2059-2066.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schröter M, Feucht HH, Zöllner B, Schäfer P, Laufs R. 2003. Multiple infections with different HCV genotypes: prevalence and clinical impact. J Clin Virol 27:200–204. doi: 10.1016/S1386-6532(02)00264-0. [DOI] [PubMed] [Google Scholar]
- 52.Thomas XV, Grady BP, Van Der Meer JT, Ho CK, Vanhommerig JW, Rebers SP, De Jong MD, Van Der Valk M, Prins M, Molenkamp R, Schinkel J; MOSAIC (MSM Observational Study of Acute Infection with hepatitis C) study group . 2015. Genetic characterization of multiple hepatitis C virus infections following acute infection in HIV-infected men who have sex with men. AIDS 29:2287–2295. doi: 10.1097/QAD.0000000000000838. [DOI] [PubMed] [Google Scholar]
- 53.Vickerman P, Grebely J, Dore GJ, Sacks-Davis R, Page K, Thomas DL, Osburn WO, Cox AL, Aitken CK, Hickman M, Hellard M; International Collaboration of Incident HIV and Hepatitis C in Injecting Cohorts (InC3) . 2012. The more you look, the more you find: effects of hepatitis C virus testing interval on reinfection incidence and clearance and implications for future vaccine study design. J Infect Dis 205:1342–1350. doi: 10.1093/infdis/jis213. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.