Abstract
Streptococcus pneumoniae is both a commensal and a major pathogen that causes invasive disease in people of all ages. The introduction of serotype-specific pneumococcal vaccines has reduced the burden of disease but has also led to replacement with new strains; thus, serotyping remains important for vaccine-related disease surveillance. Conventional serotyping methods are laborious and expensive. We developed an easy-to-perform genotypic TaqMan array card (TAC) to identify S. pneumoniae strains, including lytA-based sequences, and 53 sequence-specific PCRs to identify 74 serotypes/serogroups covering all current vaccine types as well as prevalent nonvaccine types. The TAC method was evaluated on 146 clinical S. pneumoniae isolates and 13 nonpneumococcal species that naturally inhabit the upper respiratory tract and yielded 97% (142/146) sensitivity and 100% (13/13) specificity versus results of standard Quellung serotyping. The calculated limit of detection was 20 to 200 fg (∼8 to 84 genome equivalents) per reaction. On 23 blinded nasopharyngeal specimens that were pneumococcus culture positive, the TAC pan-pneumococcus lytA assay was positive in 21 (91% sensitivity versus culture). On TAC lytA-positive specimens, a serotype result was obtained on 86%, and the result was 95% accurate versus the subsequent culture's Quellung result. TAC also detected mixed serotypes in two specimens where Quellung detected only the predominant serotype. This TAC method yields fast and comprehensive serotyping compared to the standard method and may be useful on direct specimens.
INTRODUCTION
Streptococcus pneumoniae (the pneumococcus) is a leading invasive pathogen of children and older adults, principally causing pneumonia, otitis media, and meningitis. The precursor to invasive disease is upper airway colonization (1). Existing vaccines are based upon capsular polysaccharide and are highly effective only against vaccine types (2–5). Serotype replacement occurs with increased colonization and disease caused by nonvaccine strains (6, 7). With over 90 different capsular serotypes, there is a constant race to add more capsular types to further expand coverage to reduce disease burden amid a headwind of changing strain replacement.
In this context it is important to epidemiologically follow pneumococcal serotypes, both in invasive strains to detect emergence of virulent serotypes and also in the upper airway to monitor strain replacement (1, 8). However, serotyping of pneumococci with the Quellung method is technically difficult, requires expensive panels of polyclonal antisera and precise inocula (9), and may yield visually ambiguous reactions (10). Furthermore, a limited number of subcultured colonies are typed, limiting the ability to detect mixed infections, particularly from nasopharyngeal specimens (11, 12).
Molecular serotyping methods are therefore emerging. After elucidation of the capsular biosynthetic locus (13), PCR assays for the capsular polysaccharide synthesis gene clusters have been devised. Sequencing-based assays of the cps and wzh genes (14, 15) have been published, as have real-time PCR assays to detect 21 serotypes/serogroups (16, 17). Nanofluidic, microarray, and Luminex-based systems have also been developed (18–21). Recently, we optimized 53 singleplex reactions to discern most serotypes/serogroups, including all vaccine types (22). However, performing that many reactions per specimen is onerous and difficult to implement in field settings; therefore, in this work we further optimized and configured the reactions to a single TaqMan array card (TAC).
MATERIALS AND METHODS
Bacterial strains.
All bacterial strains utilized in this study were cultured at Emory University on blood agar plates and incubated at 37°C with 5% CO2 overnight (∼16 h) prior to DNA extraction. Strains from 70 S. pneumoniae included serotypes 1, 2, 3, 4, 5, 6A, 6B, 6C, 7A, 7B, 7F, 8, 9L, 9N, 9V, 10A, 10B, 10F, 11A, 11B, 11C, 11F, 12B, 12F, 13, 14, 15A, 15B, 16A, 16F, 17A, 17F, 18C, 19A, 19B, 19C, 19F, 19“F” (atypical), 20, 21, 22A, 22F, 23A, 23B, 23F, 24A, 24B, 25A, 27, 28A, 28F, 29, 31, 33A, 33B, 33D, 33F, 34, 35A, 35B, 35F, 36, 38, 39, 41A, 41F, 43, 45, 46, and 47A, as described previously (22). For specificity testing, we included 20 streptococci naturally found in the nasopharynx, including S. infantis, S. oralis, S. anginosus, S. intermedius, S. sobrinus, S. pseudopneumoniae, S. mitis, S. parasanguinis, S. australis, S. mutans, S. peroris, S. oligofermentans, S. intestinalis, S. vestibularis, S. cristatus, S. salivarius, S. gordonii, S. sanguinis, S. sinensis, Dolosigranulum pigrum, and three other bacterial species Neisseria meningitidis, Haemophilus influenzae, and Staphylococcus aureus.
Nasopharyngeal samples from children.
Nasopharyngeal (NP) samples (n = 28) belonged to our laboratory collection, and pneumococcal carriage had been analyzed in our previous studies (10, 23). NP samples were stored at −80°C in skim milk-tryptone-glucose-glycerin (STGG) transport medium prior to DNA extraction.
Quellung standard serotyping.
Quellung results were determined as described previously (22). Briefly, a fresh overnight bacterial culture in a blood agar plate was suspended in 1× phosphate-buffered saline (PBS) and then mixed with antiserum on a glass slide and read microscopically at a magnification of ×100. Pneumococcus Neufeld antiserum was obtained from the Statens Serum Institute (Copenhagen, Denmark).
DNA extraction from bacterial cultures and nasopharyngeal specimens.
A bacterial colony was suspended in 200 μl of lysis buffer (Tris-EDTA [TE] buffer containing 0.04g/ml lysozyme and 75 U/ml mutanolysin), or 200 μl of nasopharyngeal specimens (in STGG medium) was mixed with 100 μl of lysis buffer. Samples were incubated for 1 h at 37°C. DNA was then purified using a QIAamp DNA minikit (Qiagen, Valencia, CA, USA) according to the manufacturer's instructions and eluted in 100 μl. The quality and quantification of DNA preps obtained from bacterial cultures were further evaluated using a NanoDrop system (NanoDrop Technologies, Wilmington, DE).
Assay development on 384-well plates.
We adopted 53 serotype/serogroup-specific primers and probes from published sources (16, 22, 24–26) (Table 1) and, if needed, made modifications to accommodate the common cycling condition of the TaqMan array card (TAC) using Primer Express, version 3 (Applied Biosystems, Life Technologies Corp., Carlsbad, CA, USA). We also included one pan-pneumococcus assay (lytA) (26) and an assay for an internal control (27). Optimization of conditions and probe specificity testing were performed using the 384-well format of the ViiA7 platform (Applied Biosystems, Life Technologies Corp., Carlsbad, CA, USA). Each primer/probe set (0.09 μl of each forward and reverse primer, 0.025 μl of probe of a 50 μM stock) was amplified in singleplex in a total of 5 μl of PCR mixture containing 2.5 μl of 2× TaqMan universal master mix II with uracil-N glycosylase (UNG) (Applied Biosystems, Life Technologies Corp., Carlsbad, CA, USA), 1.295 μl of nuclease-free water, and 100 pg of genomic DNA. Cycling conditions included UNG activation at 50°C for 2 min and initial denaturation at 95°C for 10 min, followed by 40 cycles of denaturation at 95°C for 10 s and annealing/extension at 60°C for 1 min. We included 54 previously characterized serotypes in each run for specificity testing, and nuclease-free water was used for a nontemplate control.
TABLE 1.
Primer and probe sequences of the 53 PCRs corresponding to 74 serotypes
| Serotype or sample type | Target | Sequence (5′–3′)a | Reference(s) or source |
|---|---|---|---|
| 1 | wchD | F-CGTGCGGTAATTGAAGCTATGA | 24 |
| R-TGTGGCCCCAGCAACTCT | |||
| P-TGCTTGCCCTTGTATAGGGT | |||
| 2 | wzy | F-TTATGGACTGGCTGATGGTTCTC | 25 |
| R-AAATCCTGACCCAATAATAGCCTTT | |||
| P-AGGTCAACGTATTGGAACTCTTAGAAATTGGGAAA | |||
| 3 | tnp | F-GGTCAGCAGAAAGTATGCATTGG | 22, 24 |
| R-TCGTTTATCCAGGGTCTGATGA | |||
| P-TATTGGATGTGGTTTATCGTGAAGA | |||
| 4 | wzy | F-GCATCAGCGACGGTTGTTAT | This study |
| R-CACCACCATAGTAACCAAAGTTCC | 16 | ||
| P-TTACCTGTAGGCTCTTCTTTTG | 16 (modified) | ||
| 5 | wzy | F-CATGATTTATGCCCTCTTGCAA | 16 (modified) |
| R-GACAGTATAAGAAAAAGCAAGGGCTAA | |||
| P-CTTCTTCTCATCGTTTCCGCAT | |||
| 6ABCD | wciP | F-AAGTTTGCRCTAGAGTATGGGAAGGT | 22, 24 (modified) |
| R-ACATTATGTCCATGTCTTCGATACAAG | |||
| P-TGTTCTGCCCTGAGCAACTGG | |||
| 6CD | wciNbeta | F-CAATCAGGCAGTTCTTTTCTCG | 22 |
| R-ACCTGACTCACCATCAATAACC | |||
| P-AAATGGGAGGGCTTTGGATTGGC | |||
| 7AF | wcwH | F-ATGAAGGCTTTGGTTTGACAGG | 16 (modified) |
| R-ATTCTCGCCATCAATTGCATATTC | |||
| P-TGAGACTAACGCACAGCCA | |||
| 7BC-40 | wcxU | F-TCCAGATATAGTCATTCCCAATCAG | 22 (modified) |
| R-AAAGAAGGTAAATCCCATGATGAATT | |||
| P-TCCCTCATTATCGATTACTGACCCACCA | |||
| 8 | wzx | F-CCACTCATCAGTTTCCCATATGTTT | 22, 24 |
| R-TCAATAATTGAAGAAGCGAACGTT | |||
| P-TGATGGCAGATGGGTTGGGACGAG | |||
| 9AV | wzx | F-AGGTATCCTATATACTGCTTTAGG | 16 (modified) |
| R-CGAATCTGCCAATATCTGAAAG | |||
| P-ACACATTGACAACCGCTACA | |||
| 9LN | wzx | F-CGTGGAATTTTCTATACTGCAATAGG | 22 (modified) |
| R-CTACTGCTACGATACCATATTCTACAG | |||
| P-CAATTCTTAGCCGGATTCTCTC | |||
| 10A | wcrD | F-AGAGGCCCTAAGAAAAGATTCG | 22 (modified) |
| R-CCCAGTCATCCCCATCAATAAC | |||
| P-AGGTCATGGCTCAACAATT | |||
| 10B | wcrD | F-AAATATGAGATTGGTAAGGAATATTCTGG | 22 |
| R-GTCTTTTCACTTAAACGAATTCCATTC | |||
| P-AACGGATTCCAATGCACTCGGTAACT | |||
| 11AD | wchK | F-CGGCCCAGCTACATTTATGG | This study |
| R-TGATCATTCACATGCTCACCAA | |||
| P-AAATACCAATAGTTGTTCCGAGATTAAAGAAGT | |||
| 11F* | wchK | F-TGGTCCAGCTACTTTTATGGC | 22 |
| R-TGATCATTCACATGCTCCCC | |||
| P-ACTCCAATAGTTGTTCCGAGGCAAAAGA | |||
| 12ABF-44-46 | mnaB | F-GCACCCACGGGTAAATATTCTAC | 16 (modified) |
| R-CAACTAAGAACCAAGGATCCACAG | |||
| P-ATACAATGCCCACCAACACC | |||
| 12B | wzx | F-GGTTGCTGATCAAAAGGTCTATG | This study |
| R-AGGTTCAAAGTAAGATTTTTAGCAA | This study | ||
| P-AGATAAAAATCTTTCCAAATCATCAAAGTGA | 22 (modified) | ||
| 13 | wzy | F-AGACTACCATTTTTTGATCAGTTAGATT | 22 |
| R-CAGAAAACATATTTTGTTCATAAATCCATC | |||
| P-AAGCAGCACTTCCAAGTCGTAATCTACC | |||
| 14 | wchL | F-CGACTGAAATGTCACTAGGAGAAGAT | 22, 24 (modified) |
| R-AATACAGTCCATCAATTACTGCAATACTC | |||
| P-TCATTCGTTTGCCAATACTTGATGGTCTC | |||
| 15 | wzx | F-TTGAATCAGGTAGATTGATTTCTGCTA | 22, 24 |
| R-CTCTAGGAATCAAATACTGAGTCCTAATGA | |||
| P-CTCCGGCTTTTGTCTTCTCTGT | |||
| 16F | wzy | F-TAATGTTATGACCTTGGTAATCTTCCC | 16 (modified) |
| R-TCCCAAAGGATAATCAATAACTTTTAGAAG | |||
| P-TCTTCCAAATGCTTAACCGC | |||
| 17F | abp2 | F-GGAACTGTTGATCATCTTAGCGTA | This study |
| R-TTTTGATCCCGTACTCGGAAG | This study | ||
| P-TCTTCGTATGCTAGTTCTAAGAGAGCTACTGA | 25 (modified) | ||
| 18ABCF | wzy | F-TCGATGGCTAGAACAGATTTATGG | 16 (modified) |
| R-CCATTGTCCCTGTAAGACCATTG | |||
| P-TTGAATCAACCTATAATTTCGCCCC | |||
| 19A | wzy | F-GCTCATTGATATCCAATTCTGGAA | This study |
| R-CATGGCTAAGTGCAAGATTATGAATC | |||
| P-AGCTCTTACTATTATAGTTGACCTCATTATTCT | |||
| 19F | wzy | F-CGGGGTCAAATATTCAGTGG | This study |
| R-CACGAATGAGAACTCGAATAAAAG | 16 | ||
| P-TTCGCACTGTCAATTCACCT | 16 (modified) | ||
| 19“F”b | wzy | F-GTCCTTAGTTCTGGTTATTCGGG | 22 |
| R-GGATGAGGAACCGAATCGAAG | |||
| P-CCAGTTATGAAGGTGAGCTAACAGTGCG | |||
| 20 | wciL | F-AAAGATACTGGCTGAGGAGCTATCTATT | 22, 24 |
| R-AGTCAAAAGTACTCAACCATTCTGATATATTC | |||
| P-AGGATAAGGTCTACTTTGTGGGAGTTC | |||
| 21* | wzy | F-GGTTTAAATATCGCTCCGGGTAT | 25 |
| R-CAAAAAAAGGGCTTGTAGACGAA | |||
| P-TGTGAATTGGACACGTTATGGAGC | |||
| 22AF | wcwA | F-TCTCTGAAATGGTTGTTGAAGGAA | 22, 24 (modified) |
| R-TCGCATCCGATAGTTCTTGTGA | |||
| P-TGGCAATCCCAGGACAA | |||
| 23A | wzy | F-CTCCCCTCCATTACCCATTTGG | 16 (modified) |
| R-TGAAGAAAGTGCTGTTTGTGAACC | |||
| P-TCCCACACTCCCTACTCCCA | |||
| 23B | wzx | F-TTGAAGAAATTGCTCCAGAAACAT | 22, 25 |
| R-CCAAAAGACTAGCCTCAACCACTAA | |||
| P-TAGAGCTATTTATCTTTCGTGGTTTT | |||
| 23F | wzy | F-AAGTGATAGTGAACTTGGGATTGTCT | This study |
| R-GATTCTATTTGCAAACACGTTGAGA | |||
| P-TGTTAAAAATACACACAACATCAACA | |||
| 24A | wzx | F-CTTGGAGTTGCTAATTATGGGAAG | 22 (modified) |
| R-ATCTCTTACACGTGCACACTC | |||
| P-CACAGCATATCGTAAAATACCCGCA | |||
| 25AF* | wcyE | F-ATACCAACTAGAATCAGCAGGAC | 22 (modified) |
| R-AAATGGAATATCTTTTGATAATTTACTCGC | |||
| P-CCGCTGGACTTACTGCAATA | |||
| 27 | whaK | F-AGCGATTTAGCGACTGATATCC | 22 |
| R-TCTCAAAATCGATCTCGCGTG | |||
| P-TGTGGAAGGCGTTTGAAGGTGACT | |||
| 29* | wcrJ | F-TTCGAGTTGTGCCGTTTTTACA | 25 (modified) |
| R-GGCGTACCCACCTCTAAAATTTT | |||
| P-TGAATCCTAGTCTTTTCTCTGCG | |||
| 31 | wzy | F-GCAGAAGTTTTAAGTCACGGAC | 22 |
| R-AGCATTACAGATGTCACTAAGGG | |||
| P-CCCCCACGTAAAACCGCAAGG | |||
| 33AF-37 | wzy | F-GGAACTGGTTCAGCAACTATACG | 16 (modified) |
| R-GGTTCTAAGACCGTCTGAAATACC | |||
| P-TAGGACTTTTCTGCCATGCC | |||
| 33B | wciN | F-CCTGTTAGTGCACCTGTATTTAAC | 22 (modified) |
| R-GCATTCAAAACTCCTTCATCTCC | |||
| P-TTCGTTGTTCACGCCATTTA | |||
| 33D* | wciN | F-CGTATAGTCTTGCGACATTTCA | 22 (modified) |
| R-TTCCACATGCGTTACCTCAC | |||
| P-CACAACTAGTTTTTTATCAAAAAGACCTTGGC | |||
| 34 | wzy | F-CGGTGGAGTAGGTCAAGATG | 22 |
| R-GTCTGTTCTCCCCAATATACTGAG | |||
| P-ACGGAGCGCCAATGTACTTGAATAGTT | |||
| 35AC-42 | wcrK | F-TGTTTCAAGCTTCCCCTTTAGA | This study |
| R-AAATGAAATCAAAGTATCACGTATCG | 22 (modified) | ||
| P-TTCAAAATACCCAGGACACCCGTTCA | 22 | ||
| 35B | wcrJ | F-GCATGGAGGTGGAGCATACA | 22, 24 (modified) |
| R-TGTAAAGACTGCACAACTCGATATAAAA | |||
| P-AACAATATTAGTAAAGCGCAGGTC | |||
| 35F-47F | wzy | F-GTGGTCGTATATACTTGATGAATAAATCG | 22 (modified) |
| R-ACATACAAATTATCAACATACAGATAGGTC | |||
| P-TTCAACTGGTCGTCCGAATA | |||
| 36* | wzy | F-CTTGTCTATTCAGCCCTTCTGG | 22 (modified) |
| R-CGCGATTATATTGTAAATTGGGAACT | |||
| P-AGAATGCCCGCTACAATGAG | |||
| 38-25AF | wciI | F-GTCTTACGTAGAACCTCTCTGGATGA | 22, 24 |
| R-TGGTCCTACAAGCGACATGTG | |||
| P-TTGCCACAGATTTGGAATATTTTGGTCGG | |||
| 39* | wcrG | F-CAAAAAAATGAACTAACTCAAATAGTAACG | 22 |
| R-ATACTGTAATTTTCTTGTTTATTTGCGG | |||
| P-AAGTCAGGCGTATTCTTCACAAGGGAAA | |||
| 41A | wciB | F-GCAAATAGATGTATCCCAGTTAACAC | 22 (modified) |
| R-GGTAGCTCTTTTGGTTTAATGTCC | |||
| P-CGACCGAATAGTCTAGCTTCAAAGG | |||
| 41F | wzx | F-TTTTTGGGAGGAAGTGCTTTT | 22 |
| R-AACCGCTTTCTCATGATTCATAACT | This study | ||
| P-CTTCTGTGCTAACAGTGGAGAT | 22 (modified) | ||
| 43 | wzx | F-AGAGGCTACATCAAATAGTTGGC | 22 |
| R-GAATCACACCGTAACTTCCAAAG | |||
| P-TCCAATAGTACTCACCCCTACCGAGC | |||
| 45* | wzy | F-TCTAGCTACTTGACTAAAATATTTGAACTG | 22 (modified) |
| R-GACGAGTCGATTTCGCTGTAT | |||
| P-CTTTTAGTGACCTCGCTCCC | |||
| 47AF* | whaI | F-AGGAATTGGTAGAGAGTTTGTGG | 22 |
| R-GAAAGTTGAACCATCATCCGTC | |||
| P-CACTTGATGGAATGCCTGCTGCC | |||
| lytA | lytA | F-TCGTGCGTTTTAATTCCAGCT | 26 (modified) |
| R-ACGCAATCTAGCAGATGAAGCA | |||
| P-CTCCCTGTATCAAGCGTTTTCGGCA | |||
| PhHV | gB | F-GGGCGAATCACAGATTGAATC | 27 |
| R-GCGGTTCCAAACGTACCAA | |||
| P-TATGTGTCCGCCACCATCT |
F, forward primer; R, reverse primer; P, probe labeled with FAM (6-carboxyfluorescein) except for the probes for the serotypes marked with asterisks, which are labeled with VIC at the 5′ end. All are 3′ minor groove binder probes.
Atypical 19F.
Evaluation of the TaqMan array card.
Primer and probe oligonucleotides were synthesized and spotted onto the TaqMan array card by Applied Biosystems (Life Technologies Corp., Carlsbad, CA, USA) as laid out in Fig. 1. Twenty microliters of input DNA (1 ng/μl for isolates) was mixed with 50 μl of 2× TaqMan universal master mix II with UNG (Applied Biosystems, Life Technologies Corp., Carlsbad, CA, USA) and 30 μl of nuclease-free water to a 100-μl final volume. This was loaded into each port of the card, whereby each card included seven clinical samples and one synthetic positive-control plasmid (Genewiz, Inc., South Plainfield, NJ, USA) that we designed to contain the primer and probe region of all 55 assays (53 serotype-specific assays plus lytA and phocine herpesvirus [PhHV]). The loaded card was centrifuged twice at 1,200 rpm for 1 min and then sealed; the loading ports were excised, and the card was inserted into a ViiA7 instrument (Life Technologies Corp., Carlsbad, CA, USA) and run under the same cycling conditions as described above for 40 cycles.
FIG 1.
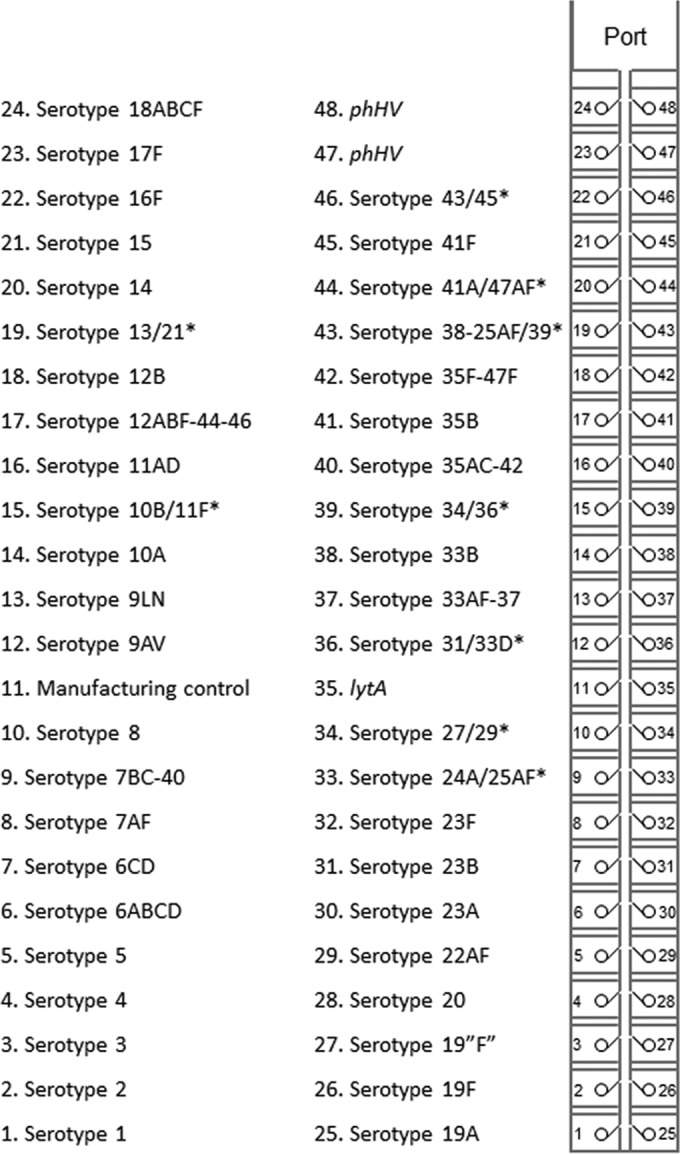
Streptococcus pneumoniae serotyping TaqMan array card layout. The TaqMan array card includes eight sample ports, whereby each sample is aliquoted into 48 PCRs. Serotypes in the form AB or A-B indicate a common assay that detects multiple serotypes/serogroups. Serotypes in the form A/B* indicate a duplex assay.
Statistical analysis.
Means or medians were compared using Student's t test or a Mann-Whitney test. Data are shown as means ± standard deviations unless otherwise stated. A standard curve of lytA was generated with known DNA concentrations and plotted against the threshold cycle (CT) to yield the copy number, calculated as 10(CT − 33.701)/−3.4262.
RESULTS
Analytical assay performance.
The 53 serotype/serogroup-specific singleplex PCR assays as well as the S. pneumoniae lytA assay were tested against 54 serotyped pneumococcal isolates as well as several nonpneumococcal species, and 100% specificity with no cross-reactivity was observed (see Fig. 1 in the supplemental material). The PCR performance of each primer/probe assay was determined on both 384-well plates and the TaqMan array card formats. DNA from both individual and pooled serotypes was tested in serial dilution. The overall linearity of the 53 serotype assay targets including lytA was 0.997 ± 0.01 and 0.986 ± 0.02, and the PCR efficiencies were 93% ± 4.9% and 97% ± 9.7% using the 384-well plates and TaqMan array card formats, respectively. The limit of detection on 384-well plates was 10 to 100 fg/reaction while that of TAC was 20 to 200 fg/reaction (Table 2).
TABLE 2.
PCR performance of each serotype/serogroup-specific assay
| Serotype or sample | 384-well plate |
TaqMan array card |
||
|---|---|---|---|---|
| Linearity (R2)a | LOD (fg)b | Linearity (R2) | LOD (fg) | |
| 1 | 0.953 (87.2) | 10 (4.2) | 0.994 (85.7) | 20 (8.4) |
| 2 | 0.998 (85.9) | 10 (4.2) | 0.940 (87.3) | 20 (8.4) |
| 3 | 0.999 (97.7) | 10 (4.2) | 0.998 (98.8) | 20 (8.4) |
| 4 | 0.998 (90.0) | 100 (42) | 0.998 (95.6) | 200 (84) |
| 5 | 0.997 (89.9) | 10 (4.2) | 1.000 (92.8) | 20 (8.4) |
| 6ABCD | 0.999 (92.4) | 10 (4.2) | 0.995 (98.9) | 20 (8.4) |
| 6CD | 0.999 (91) | 10 (4.2) | 0.998 (98.6) | 20 (8.4) |
| 7AF | 1.000 (92.9) | 10 (4.2) | 0.998 (89.5) | 20 (8.4) |
| 7BC-40 | 0.999 (91.1) | 10 (4.2) | 0.968 (80.4) | 20 (8.4) |
| 8 | 0.999 (100) | 10 (4.2) | 0.996 (99.0) | 20 (8.4) |
| 9AV | 0.992 (95.7) | 10 (4.2) | 0.993 (109.1) | 20 (8.4) |
| 9LN | 0.993 (90.6) | 10 (4.2) | 0.957 (87.4) | 20 (8.4) |
| 10A | 1.000 (97.0) | 10 (4.2) | 0.983 (102.6) | 20 (8.4) |
| 10B | 1.000 (94.4) | 10 (4.2) | 0.996 (108.1) | 20 (8.4) |
| 11AD | 1.000 (92.4) | 10 (4.2) | 0.965 (86.5) | 20 (8.4) |
| 11F | 0.994 (84.8) | 10 (4.2) | 0.943 (120.2) | 20 (8.4) |
| 12ABF-44-46 | 0.999 (99.2) | 10 (4.2) | 0.997 (102.3) | 20 (8.4) |
| 12B | 1.000 (91.5) | 100 (42) | 0.961 (76.1) | 200 (84) |
| 13 | 0.999 (90.9) | 100 (42) | 0.861 (94.8) | 200 (84) |
| 14 | 0.999 (95.7 | 10 (4.2) | 0.994 (95.7) | 20 (8.4) |
| 15 | 1.000 (93.7) | 10 (4.2) | 0.994 (102.6) | 20 (8.4) |
| 16F | 0.998 (86.9) | 100 (42) | 0.979 (92.5) | 200 (84) |
| 17F | 0.998 (88.5) | 10 (4.2) | 0.996 (103.3) | 20 (8.4) |
| 18ABCF | 0.999 (91.0) | 10 (4.2) | 0.998 (78.4) | 20 (8.4) |
| 19A | 1.000 (92.8) | 10 (4.2) | 0.994 (99.5) | 20 (8.4) |
| 19F | 0.999 (99.3) | 10 (4.2) | 0.998 (95.0) | 20 (8.4) |
| 19“F” | 1.000 (94.4) | 10 (4.2) | 0.993 (94.4) | 20 (8.4) |
| 20 | 0.998 (95.3) | 10 (4.2) | 0.996 (90.6) | 20 (8.4) |
| 21 | 0.999 (93.4) | 10 (4.2) | 0.993 (98.2) | 20 (8.4) |
| 22AF | 0.998 (100) | 10 (4.2) | 0.999 (103.5) | 20 (8.4) |
| 23A | 0.999 (89.3) | 10 (4.2) | 0.995 (92.8) | 20 (8.4) |
| 23B | 0.998 (103) | 10 (4.2) | 0.992 (103.7) | 20 (8.4) |
| 23F | 0.996 (88.5) | 10 (4.2) | 0.998 (93.6) | 20 (8.4) |
| 24A | 0.998 (100) | 10 (4.2) | 0.973 (82.8) | 20 (8.4) |
| 25AF | 0.997 (88.5) | 10 (4.2) | 0.997 (103.6) | 20 (8.4) |
| 27 | 0.998 (89.9) | 10 (4.2) | 0.996 (106.7) | 20 (8.4) |
| 29 | 0.992 (85.5) | 10 (4.2) | 0.997 (70.0) | 20 (8.4) |
| 31 | 0.999 (93.1) | 10 (4.2) | 0.996 (89.7) | 20 (8.4) |
| 33AF-37 | 1.000 (90.7) | 10 (4.2) | 0.998 (101.3) | 20 (8.4) |
| 33B | 0.993 (97.8) | 10 (4.2) | 0.996 (98.9) | 20 (8.4) |
| 33D | 1.000 (96.5) | 10 (4.2) | 0.985 (95.1) | 20 (8.4) |
| 34 | 0.996 (92.6) | 100 (42) | 1.000 (103.4) | 200 (84) |
| 35AC-42 | 0.997 (105) | 10 (4.2) | 0.996 (103.8) | 20 (8.4) |
| 35B | 0.998 (94.0) | 10 (4.2) | 0.979 (100.2) | 20 (8.4) |
| 35F-47F | 0.997 (90.1) | 10 (4.2) | 0.996 (94.3) | 20 (8.4) |
| 36 | 0.999 (88.7) | 10 (4.2) | 0.997 (103.1) | 20 (8.4) |
| 38-25AF | 0.999 (96.8) | 10 (4.2) | 1.000 (94.3) | 20 (8.4) |
| 39 | 0.999 (96.4) | 10 (4.2) | 0.986 (108.8) | 20 (8.4) |
| 41A | 1.000 (91.7) | 10 (4.2) | 0.994 (97.9) | 20 (8.4) |
| 41F | 1.000 (79.0) | 100 (42) | 0.997 (105.7) | 200 (84) |
| 43 | 0.998 (95.4) | 10 (4.2) | 0.929 (96.8) | 20 (8.4) |
| 45 | 1.000 (94.7) | 10 (4.2) | 0.998 (95.0) | 20 (8.4) |
| 47AF | 1.000 (93.4) | 100 (42) | 0.995 (104.3) | 200 (84) |
| lytA | 0.998 (94.8) | 10 (4.2) | 0.999 (97.9) | 20 (8.4) |
| PhHV | 0.994 (94.7) | 0.986 (114.9) | ||
Values in parentheses represent PCR efficiency (%).
LOD, limit of detection. Values in parentheses are the numbers of copies per reaction. The genome size of S. pneumoniae serotype 4 TIGR4 (2,160,842 bp) was used for calculations.
Evaluation of TaqMan array card serotyping on clinical isolates.
The performance of the TaqMan array card was evaluated on 54 S. pneumoniae serotypes (previously serotyped by Quellung reactions) and then on 92 blinded isolates, which included serotypes 1, 2, 3, 4, 5, 6A, 6B, 7F, 8, 9N, 9V, 10A, 10F, 11A, 11B, 11C, 12F, 14, 15B, 16A, 17A, 17F, 18C, 19A, 19B, 19C, 19F, 20, 22A, 22F, 23F, 24B, 28A, 28F, 33F, and 13 non-S. pneumoniae strains. TAC yielded 97% (155/159) agreement compared with the Quellung serotype result (Table 3). There was 100% specificity, and all four discordant samples were indicated as serotype 22F by Quellung (performed twice) but negative with the TAC 22AF assay. This was not due to 22AF assay failure since it was positive for three serotype 22A strains.
TABLE 3.
Performance of TaqMan array card serotyping on isolates versus the Quellung standard
| Isolate condition and Quellung serotype or sample type | No. of isolates tested | No. of concordant results | No. of discordant results | % Accuracy |
|---|---|---|---|---|
| Unblinded | ||||
| All serotypes from Table 2 | 54 | 54 | 0 | 100 |
| Blindeda | ||||
| 1 | 4 | 4 | 0 | 100 |
| 2 | 2 | 2 | 0 | 100 |
| 3 | 3 | 3 | 0 | 100 |
| 4 | 4 | 4 | 0 | 100 |
| 5 | 2 | 2 | 0 | 100 |
| 6A | 3 | 3 | 0 | 100 |
| 6B | 5 | 5 | 0 | 100 |
| 7F | 4 | 4 | 0 | 100 |
| 8 | 3 | 3 | 0 | 100 |
| 9N | 4 | 4 | 0 | 100 |
| 9V | 4 | 4 | 0 | 100 |
| 10A | 3 | 3 | 0 | 100 |
| 11A | 3 | 3 | 0 | 100 |
| 12F | 1 | 1 | 0 | 100 |
| 14 | 4 | 4 | 0 | 100 |
| 15B | 2 | 2 | 0 | 100 |
| 17F | 3 | 3 | 0 | 100 |
| 18C | 4 | 4 | 0 | 100 |
| 19A | 3 | 3 | 0 | 100 |
| 19F | 5 | 5 | 0 | 100 |
| 20 | 3 | 3 | 0 | 100 |
| 22A | 2 | 2 | 0 | 100 |
| 22F | 4 | 0 | 4b | 0 |
| 23F | 4 | 4 | 0 | 100 |
| 33F | 3 | 3 | 0 | 100 |
| Serotypes not included in Table 2 | 10 | 10b | 0 | 100 |
| Nonpneumococcal bacteria | 13 | 13c | 0 | 100 |
| Total | 159 | 155 | 4 | 97 |
Serotypes in bold are those included in PCV13.
Positive with lytA but negative with any serotype-specific probe on the TAC.
Negative with any probe on the TAC, including lytA.
TaqMan array card serotyping on direct specimens.
Twenty-eight nasopharyngeal specimens underwent DNA extraction and TAC testing, and the results were compared with the culture and Quellung results (22). In 23 of these nasopharyngeal specimens an S. pneumoniae strain had been isolated whereas five were culture negative. The TAC yielded a lytA-positive result in 21/23 culture-positive specimens and was positive in 1/5 culture-negative specimens (CT of 34), corresponding to a TAC lytA sensitivity of 91% and specificity of 80% versus culture (Table 4). The serotype assays were exclusively positive in lytA-positive specimens (TAC serotype assays, 100% specificity versus lytA). In the 22 lytA-positive specimens, a serotype result was obtained for 19 specimens (TAC serotype assays, 86% sensitivity versus lytA). The TAC serotype result matched the Quellung result in 18 specimens (95% accuracy), the exception being one pneumococcus specimen nontypeable by Quellung that was serotype 4 by TAC (with a somewhat late CT of 30 compared with the other serotype 4 strains). There were two culture-positive specimens undetectable by lytA on the TAC, one of which was lytA-positive when larger volumes of DNA were used (1 μl; CT of 37) in a plate format and one of which remained negative. Likewise, we retested the three lytA-positive/serotype-negative samples with the serotype assays with larger volumes of DNA, and one became positive (1 μl; CT of 36). We used the TAC lytA CT to extrapolate the pneumococcal concentration in the nasopharyngeal specimens, and the two discrepant results (e.g., lytA positive/serotype negative) were both at the lowest concentration of 3 × 103 to 4 × 103 CFU/ml.
TABLE 4.
Performance of TaqMan array card serotyping method on nasopharyngeal specimens
| Quellung serotype or culture resulta | TaqMan array card |
|||
|---|---|---|---|---|
| lytA CT | Serotype result(s) (CT) | DNA (copies/reaction) | Predicted bacterial load from lytA CT (CFU/ml) | |
| 4 | 27 | 4 (29), 23B (30) | 9.33E1 | 9.33E5 |
| 4 | 28 | 4 (28) | 4.70E1 | 4.70E5 |
| 6A | 27 | 6ABCD (29) | 6.77E1 | 6.77E5 |
| 6A | Negative | Negative | NAb | NA |
| 10A | 31 | 10A (33) | 6.49E0 | 6.49E4 |
| 11A | 23 | 11AD (23) | 4.96E2 | 4.96E6 |
| 11A | 28 | 11AD (28) | 5.94E1 | 5.94E5 |
| 11A | 32 | 11AD (35) | 4.16E0 | 4.16E4 |
| 11A | 34 | 11AD (34) | 8.59E−1 | 8.59E3 |
| 17F | 30 | 17F (30) | 1.32E1 | 1.32E5 |
| 17F | 33 | 17F (36) | 1.66E0 | 1.66E4 |
| 19A | 29 | 19A (31), 6CD (33) | 1.79E1 | 1.79E5 |
| 19A | 28 | 19A (30) | 3.71E1 | 3.71E5 |
| 19F | 29 | 19F (29) | 2.85E1 | 2.85E5 |
| 19F | 28 | 19“F” (30) | 4.20E1 | 4.20E5 |
| 19F | 30 | 19F (30) | 1.41E1 | 1.41E5 |
| 19F | 28 | 19F (28) | 5.04E1 | 5.04E5 |
| 19F | 35 | Negative | 3.86E−1 | 3.86E3 |
| 23F | 28 | 23F (31) | 3.63E1 | 3.63E5 |
| 23F | 27 | 23F (28) | 7.45E1 | 7.45E5 |
| 23F | Negative | Negative | NA | NA |
| 35F | 35 | Negative | 3.16E−1 | 3.16E3 |
| NT | 27 | 4 (30) | 3.08E1 | 3.08E5 |
| Pneumococcal culture negative | ||||
| With positive TAC result (n = 1) | 34 | Negative | 9.62E−1 | 9.62E3 |
| With negative TAC result (n = 4) | Negative | Negative | NA | NA |
The Quellung reaction was performed with pure culture colonies from the same nasopharyngeal samples. NT, not typeable.
NA, not applicable.
DISCUSSION
In this work we describe the development of a TaqMan array card that compartmentalizes 53 reactions to detect 74 pneumococcal serotypes and that can be used on isolates or nasopharyngeal specimens. Once developed, the TAC assay is as simple to perform as a single PCR. The TAC assays exhibited excellent linearity and limits of detection, albeit they were slightly less sensitive than the assays in a plate format, where more DNA template can be added. This slight sensitivity loss may not be clinically deleterious, and certainly the procedural advantage of the TAC versus setting up 54 singleplex PCRs is enormous.
For isolates where abundant DNA is available, performance remained excellent, with 97% accuracy versus the Quellung result. Indeed, the card had 100% accuracy on blinded isolates from a wide variety of 24 serotypes, including all of the PCV13 strains. Discrepancies were observed only with 22F strains. Curiously, wcwA sequences, according to GenBank accession numbers CR931681.1 and CR931682.1, are identical between 22A and 22F in the primer region, yet the 22F strains did not amplify, while 22A did, suggesting that there is a disconnect between the available 22F GenBank sequence and these four strains (see Fig. 2 in the supplemental material). Future iterations of the assays can attempt to understand and improve this. This caveat aside, the assay is clearly robust for use on cultured isolates from invasive sites and should provide an important tool to document whether serotype replacement is occurring in invasive strains (28).
The assay also worked well on direct nasopharyngeal specimens, with a 91% sensitivity versus culture and an 86% accuracy of the serotype result versus the Quellung reaction on lytA-positive specimens. A few samples had low levels of DNA at the lytA or serotype level that could be rescued with larger amounts of DNA. Thus, the serotype result was 100% accurate for any lytA result of a CT of 34 or below (corresponding to a nasopharyngeal density of 8 × 103 CFU/ml), which is how we would propose using the assay. This assay is suitable for monitoring pneumococcus density and mixed infections in nasopharyngeal specimens, which is of great interest in the effort to better document the phenomenon of serotype replacement in the nasopharynx after vaccination (6). Regarding mixed infections, there was one discrepant nasopharyngeal specimen which was nontypeable by Quellung but serotype 4 by TAC, which we hypothesize was mixed. It is also plausible that this specimen represents a weakly expressing strain. We think that applying TAC to nasopharyngeal colonization will be particularly useful to monitor vaccine effectiveness in communities over time, ensuring that vaccine types are being eliminated as expected. Nasopharyngeal materials are much easier to obtain than invasive isolates, particularly in children and in resource-limited settings where the burden is highest. It has been proposed that the absence of a vaccine type in nasopharyngeal specimens in children with pneumonia could be used as a surrogate for vaccine effectiveness (11).
Limitations of our study are that the number of direct specimens with culture- and serotype-confirmed results was small; thus, the sensitivity and specificity estimates of the TAC assay are approximate, and additional evaluation will be beneficial. Other investigators have found that nonpneumococcal streptococcal species can interfere with serotyping assays (29), so more direct specimen testing is needed. Although the limit of detection by TAC was within the range of other reported assays (26), it was 2-fold higher than that of the regular real-time PCR format (22). Some serotypes could not be identified individually by single assay sets. For example, to infer serotype 6AB we must detect serotypes 6ABCD in the absence of serotypes 6CD (Fig. 1). We certainly suspect that the serotype reactions may need to be modified over time to include alternate types.
We embarked on this project because we have demonstrated excellent performance and reproducibility of the TAC platform in multisite field studies in Africa and Asia (30), areas of high pneumococcal carriage, coinfection, and variable serotype distributions. While the real-time PCR instrument is costly (∼$75,000), it also performs routine real-time PCR. To our knowledge, the TAC platform exists in at least 13 countries across sub-Saharan Africa and South Asia. The TAC cards are stable at 4°C for at least 2 years and cost about $50 per specimen, or approximately $1 per reaction, which compares favorably with conventional Quellung testing, which can cost up to $100 per colony (12). In conclusion, the TaqMan array card is a fast, high-throughput, serotyping method for pneumococci that is suitable to field studies.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by NIH grant K24 AI102972 (to E.R.H.) and by the Murdoch Children's Research Institute (to J.V.) which received funds from the Bill and Melinda Gates Foundation (grant 52099). P.T. is funded by the Wellcome Trust as part of the Wellcome Trust-Mahidol University-Oxford Tropical Medicine Research Programme.
We thank Catherine Satzke for helpful discussions and Yiming Lin from Emory University for his assistance in some laboratory procedures. We also thank Lesley McGee and Bernard Beall from the CDC for providing most nonpneumococcal streptococci utilized in this study.
Footnotes
Supplemental material for this article may be found at http://dx.doi.org/10.1128/JCM.00613-16.
REFERENCES
- 1.Bogaert D, De Groot R, Hermans PW. 2004. Streptococcus pneumoniae colonisation: the key to pneumococcal disease. Lancet Infect Dis 4:144–154. doi: 10.1016/S1473-3099(04)00938-7. [DOI] [PubMed] [Google Scholar]
- 2.Klugman KP, Madhi SA, Huebner RE, Kohberger R, Mbelle N, Pierce N, Vaccine Trialists Group. 2003. A trial of a 9-valent pneumococcal conjugate vaccine in children with and those without HIV infection. N Engl J Med 349:1341–1348. doi: 10.1056/NEJMoa035060. [DOI] [PubMed] [Google Scholar]
- 3.Black SB, Shinefield HR, Ling S, Hansen J, Fireman B, Spring D, Noyes J, Lewis E, Ray P, Lee J, Hackell J. 2002. Effectiveness of heptavalent pneumococcal conjugate vaccine in children younger than five years of age for prevention of pneumonia. Pediatr Infect Dis J 21:810–815. doi: 10.1097/00006454-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Cutts FT, Zaman SM, Enwere G, Jaffar S, Levine OS, Okoko JB, Oluwalana C, Vaughan A, Obaro SK, Leach A, McAdam KP, Biney E, Saaka M, Onwuchekwa U, Yallop F, Pierce NF, Greenwood BM, Adegbola RA, Gambian Pneumococcal Vaccine Trial Group. 2005. Efficacy of nine-valent pneumococcal conjugate vaccine against pneumonia and invasive pneumococcal disease in The Gambia: randomised, double-blind, placebo-controlled trial. Lancet 365:1139–1146. doi: 10.1016/S0140-6736(05)71876-6. [DOI] [PubMed] [Google Scholar]
- 5.Olarte L, Barson WJ, Barson RM, Lin PL, Romero JR, Tan TQ, Givner LB, Bradley JS, Hoffman JA, Hulten KG, Mason EO, Kaplan SL. 2015. Impact of the 13-valent pneumococcal conjugate vaccine on pneumococcal meningitis in US children. Clin Infect Dis 61:767–775. doi: 10.1093/cid/civ368. [DOI] [PubMed] [Google Scholar]
- 6.Weinberger DM, Malley R, Lipsitch M. 2011. Serotype replacement in disease after pneumococcal vaccination. Lancet 378:1962–1973. doi: 10.1016/S0140-6736(10)62225-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gaviria-Agudelo CL, Jordan-Villegas A, Garcia C, McCracken GH Jr. 22 February 2016. The effect of 13-valent pneumococcal conjugate vaccine on the serotype distribution and antibiotic resistance profiles in children with invasive pneumococcal disease. J Pediatr Infect Dis Soc doi: 10.1093/jpids/piw005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weinberger DM, Bruden DT, Grant LR, Lipsitch M, O'Brien KL, Pelton SI, Sanders EA, Feikin DR. 2013. Using pneumococcal carriage data to monitor postvaccination changes in invasive disease. Am J Epidemiol 178:1488–1495. doi: 10.1093/aje/kwt156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Habib M, Porter BD, Satzke C. 2014. Capsular serotyping of Streptococcus pneumoniae using the Quellung reaction. J Vis Exp 84:e51208. doi: 10.3791/51208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hanke CR, Grijalva CG, Chochua S, Pletz MW, Hornberg C, Edwards KM, Griffin MR, Verastegui H, Gil AI, Lanata CF, Klugman KP, Vidal JE. 2016. Bacterial density, serotype distribution and antibiotic resistance of pneumococcal strains from the nasopharynx of Peruvian children before and after pneumococcal conjugate vaccine 7. Pediatr Infect Dis J 35:432–439. doi: 10.1097/INF.0000000000001030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Turner P, Hinds J, Turner C, Jankhot A, Gould K, Bentley SD, Nosten F, Goldblatt D. 2011. Improved detection of nasopharyngeal cocolonization by multiple pneumococcal serotypes by use of latex agglutination or molecular serotyping by microarray. J Clin Microbiol 49:1784–1789. doi: 10.1128/JCM.00157-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huebner RE, Dagan R, Porath N, Wasas AD, Klugman KP. 2000. Lack of utility of serotyping multiple colonies for detection of simultaneous nasopharyngeal carriage of different pneumococcal serotypes. Pediatr Infect Dis J 19:1017–1020. doi: 10.1097/00006454-200010000-00019. [DOI] [PubMed] [Google Scholar]
- 13.Bentley SD, Aanensen DM, Mavroidi A, Saunders D, Rabbinowitsch E, Collins M, Donohoe K, Harris D, Murphy L, Quail MA, Samuel G, Skovsted IC, Kaltoft MS, Barrell B, Reeves PR, Parkhill J, Spratt BG. 2006. Genetic analysis of the capsular biosynthetic locus from all 90 pneumococcal serotypes. PLoS Genet 2:e31. doi: 10.1371/journal.pgen.0020031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elberse KE, van de Pol I, Witteveen S, van der Heide HG, Schot CS, van Dijk A, van der Ende A, Schouls LM. 2011. Population structure of invasive Streptococcus pneumoniae in The Netherlands in the pre-vaccination era assessed by MLVA and capsular sequence typing. PLoS One 6:e20390. doi: 10.1371/journal.pone.0020390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leung MH, Bryson K, Freystatter K, Pichon B, Edwards G, Charalambous BM, Gillespie SH. 2012. Sequetyping: serotyping Streptococcus pneumoniae by a single PCR sequencing strategy. J Clin Microbiol 50:2419–2427. doi: 10.1128/JCM.06384-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pimenta FC, Roundtree A, Soysal A, Bakir M, du Plessis M, Wolter N, von Gottberg A, McGee L, Carvalho MDG, Beall B. 2013. Sequential triplex real-time PCR assay for detecting 21 pneumococcal capsular serotypes that account for a high global disease burden. J Clin Microbiol 51:647–652. doi: 10.1128/JCM.02927-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dube FS, van Mens SP, Robberts L, Wolter N, Nicol P, Mafofo J, Africa S, Zar HJ, Nicol MP. 2015. Comparison of a real-time multiplex PCR and sequetyping assay for pneumococcal serotyping. PLoS One 10:e0137349. doi: 10.1371/journal.pone.0137349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tomita Y., Okamoto A., Yamada K., Yagi T., Hasegawa Y., Ohta M. 2011. A new microarray system to detect Streptococcus pneumoniae serotypes. J Biomed Biotechnol 2011:352736. doi: 10.1155/2011/352736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Satzke C, Dunne EM, Porter BD, Klugman KP, Mulholland EK, PneuCarriage Project Group. 2015. The PneuCarriage Project: a multi-centre comparative study to identify the best serotyping methods for examining pneumococcal carriage in vaccine evaluation studies. PLoS Med 12:e1001903. doi: 10.1371/journal.pmed.1001903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dhoubhadel BG, Yasunami M, Yoshida LM, Thi HA, Thi TH, Thi TA, Watanabe K, Suzuki M, Morimoto K, Dang DA, Ariyoshi K. 2014. A novel high-throughput method for molecular serotyping and serotype-specific quantification of Streptococcus pneumoniae using a nanofluidic real-time PCR system. J Med Microbiol 63:528–539. doi: 10.1099/jmm.0.071464-0. [DOI] [PubMed] [Google Scholar]
- 21.Yu J, Lin J, Kim KH, Benjamin WH Jr, Nahm MH. 2011. Development of an automated and multiplexed serotyping assay for Streptococcus pneumoniae. Clin Vaccine Immunol 18:1900–1907. doi: 10.1128/CVI.05312-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sakai F, Chochua S, Satzke C, Dunne EM, Mulholland K, Klugman KP, Vidal JE. 2015. Single-plex quantitative assays for the detection and quantification of most pneumococcal serotypes. PLoS One 10:e0121064. doi: 10.1371/journal.pone.0121064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sakai F, Talekar SJ, Klugman KP, Vidal JE, for the Investigators G. 2013. Expression of virulence-related genes in the nasopharynx of healthy Children. PLoS One 8:e67147. doi: 10.1371/journal.pone.0067147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Azzari C, Moriondo M, Indolfi G, Cortimiglia M, Canessa C, Becciolini L, Lippi F, de Martino M, Resti M. 2010. Realtime PCR is more sensitive than multiplex PCR for diagnosis and serotyping in children with culture negative pneumococcal invasive disease. PLoS One 5:e9282. doi: 10.1371/journal.pone.0009282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Azzari C, Moriondo M, Cortimiglia M, Valleriani C, Canessa C, Indolfi G, Ricci S, Nieddu F, de Martino M, Resti M. 2012. Potential serotype coverage of three pneumococcal conjugate vaccines against invasive pneumococcal infection in Italian children. Vaccine 30:2701–2705. doi: 10.1016/j.vaccine.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 26.Carvalho Mda G, Tondella ML, McCaustland K, Weidlich L, McGee L, Mayer LW, Steigerwalt A, Whaley M, Facklam RR, Fields B, Carlone G, Ades EW, Dagan R, Sampson JS. 2007. Evaluation and improvement of real-time PCR assays targeting lytA, ply, and psaA genes for detection of pneumococcal DNA. J Clin Microbiol 45:2460–2466. doi: 10.1128/JCM.02498-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu J, Gratz J, Amour C, Kibiki G, Becker S, Janaki L, Verweij JJ, Taniuchi M, Sobuz SU, Haque R, Haverstick DM, Houpt ER. 2013. A laboratory-developed TaqMan Array Card for simultaneous detection of 19 enteropathogens. J Clin Microbiol 51:472–480. doi: 10.1128/JCM.02658-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feikin DR, Kagucia EW, Loo JD, Link-Gelles R, Puhan MA, Cherian T, Levine OS, Whitney CG, O'Brien KL, Moore MR. 2013. Serotype-specific changes in invasive pneumococcal disease after pneumococcal conjugate vaccine introduction: a pooled analysis of multiple surveillance sites. PLoS Med 10:e1001517. doi: 10.1371/journal.pmed.1001517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carvalho Mda G, Pimenta FC, Moura I, Roundtree A, Gertz RE Jr, Li Z, Jagero G, Bigogo G, Junghae M, Conklin L, Feikin DR, Breiman RF, Whitney CG, Beall BW. 2013. Non-pneumococcal mitis-group streptococci confound detection of pneumococcal capsular serotype-specific loci in upper respiratory tract. PeerJ 1:e97. doi: 10.7717/peerj.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu J, Kabir F, Manneh J, Lertsethtakarn P, Begum S, Gratz J, Becker SM, Operario DJ, Taniuchi M, Janaki L, Platts-Mills JA, Haverstick DM, Kabir M, Sobuz SU, Nakjarung K, Sakpaisal P, Silapong S, Bodhidatta L, Qureshi S, Kalam A, Saidi Q, Swai N, Mujaga B, Maro A, Kwambana B, Dione M, Antonio M, Kibiki G, Mason CJ, Haque R, Iqbal N, Zaidi AK, Houpt ER. 2014. Development and assessment of molecular diagnostic tests for 15 enteropathogens causing childhood diarrhoea: a multicentre study. Lancet Infect Dis 14:716–724. doi: 10.1016/S1473-3099(14)70808-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


