Abstract
Background:
Primary mucosal malignant melanoma is an extremely rare, aggressive neoplasm accounting for 0.5% of all oral malignancies. Any pigmented lesion in oral cavity should have an index of suspicion, which should be investigated to detect the disease at an early stage and managed appropriately. Melanomas tend to invade locally into the tissue or metastasize more commonly than other malignant tumors of the oral cavity.
Materials and Methods:
We report a retrospective case series of eight patients suffering from primary oral malignant melanoma treated in our department between 2012 and 2014. The details were recorded from the departmental computerized database and patients on follow-up.
Results:
There were six male and two female patients with a mean age of 46.8 years. Hard palate was the most common affected site in oral cavity. Pigmented lesion\ulcer was the most common presenting symptom. Majority of patients (5 patients) were diagnosed with Stage III (distant metastasis), two patients in Stage II, and one patient in Stage I. Three patients were treated with definitive surgery and five patients with palliative chemotherapy in view of distant disease. Following surgery, two of them required adjuvant chemoradiotherapy in view of nodal spread. Patients had a mean follow-up of 10.5 months (range: 8–26 months). Patients treated with definitive surgery had a mean survival rate of 16 months (range: 10–26 months), with local recurrence in one patient. Metastatic melanoma patients treated with palliative chemotherapy had a mean disease control rate of 5 months (range 5–9 months).
Conclusion:
Oral melanoma carries dismal prognosis with a 5-year survival rate of 5–20%. Early detection of the lesion, proper evaluation, and appropriate treatment are very important to cure the disease.
Keywords: Aggressive, malignant melanoma, oral mucosa, pigmented, tumor
INTRODUCTION
Malignant melanoma of oral cavity is an infrequent neoplasm originating from malignant transformation of melanocytes found in the basal layer of oral mucosal membrane. Melanocytes are neural crest-derived cells that migrate to the skin, mucosal membranes, and several other sites.[1] It represents 0.2–8% of the total cases of melanoma from the other locations of the body and 0.5% of all oral neoplasia.[2,3]
Exact etiology is not known. A definitive precursor lesion for mucosal melanoma has not been identified; however, atypical melanocytic hyperplasia may represent a proliferative phase before overt tumorigenesis occurs.[1] Mechanical trauma such as dental irritation, tobacco use, exposure to formaldehyde, and alcohol are the other possible predisposing factors.[4]
Majority of cases occur after 40 years of age, with a higher incidence in the sixth decade and slightly more male predilection. The common sites of occurrence are the palate and gingiva, with the maxillary arch being affected 80% of the time.[5] Clinical features include the presence of melanotic pigmentation (in 30% of cases before diagnosis), amelanotic lesions (up to 20%), pain, and bleeding.[6] The most common sites of metastasis are lymph nodes, lung, bone, liver, and brain.[7]
Surgical resection of the lesion with negative margins is the treatment of choice with the ill-defined role of chemo radiotherapy in the adjuvant setting. It has a poor prognosis with regard to delayed diagnosis, high rates of local relapse, and distant metastasis due to early hematogenous spread.[8]
The present article describes clinical and epidemiological features of 8 patients presented to our department and treatment modalities, as it adds to the natural history of the lesion.
MATERIALS AND METHODS
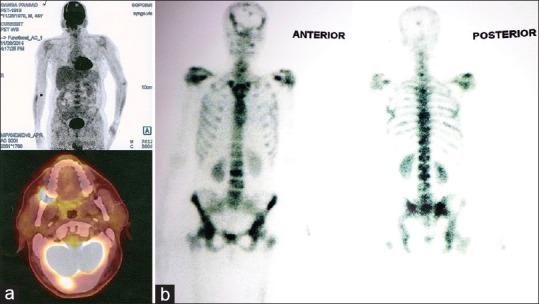
This is a retrospective study of eight cases of oral malignant melanoma that were treated at our institution during August 2012 to October 2014. All patients underwent a complete examination, chest X-ray, and computed tomography (CT) scan. Positron emission tomography (PET) scan was performed in two patients. Punch biopsy/incision biopsy was done in all patients to confirm diagnosis. The age, sex of patients, tumor location, symptoms, radiological features, final histopathology, treatment modalities, and outcome were recorded [Table 1].
Table 1.
Clinicoepidemiological features of malignant melanoma patients treated at our department
RESULTS
Age/gender
The mean age of patients was 46.8-year-old with a range of 35–65 years. Majority of patients were above 40 years with none below the age of 30 years. Peak incidence was in the fourth to sixth decade. There were six male and two female patients (sex ratio - 3:1).
Risk factors
Majority of patients had a history of tobacco chewing (87.5% cases [7 patients]) and smoking (62.5% cases [5 patients]) whereas none of them had a history of alcohol consumption or exposure to formaldehyde.
Clinical features
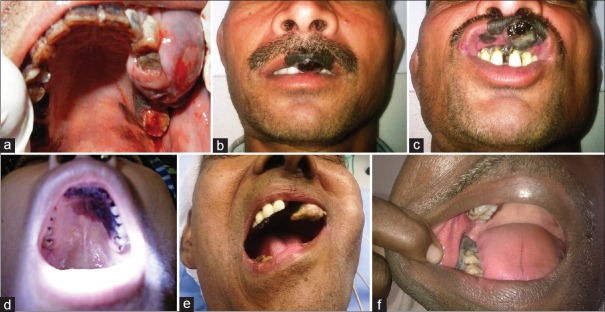
Most common presenting feature was pigmented lesion (87.5%), followed by ulcer, pain, and bleeding. Majority of the patients presented with duration of symptoms between 2 and 18 months (mean duration - 9.4 months). Most common site of involvement was hard palate (50% cases), followed by upper alveolus, lower alveolus, lip and floor of mouth (FOM) [Figure 1a–f].
Figure 1.
(a-f) Clinical photographs showing malignant melanoma of the oral cavity affecting various sites
Diagnosis, staging, and metastasis
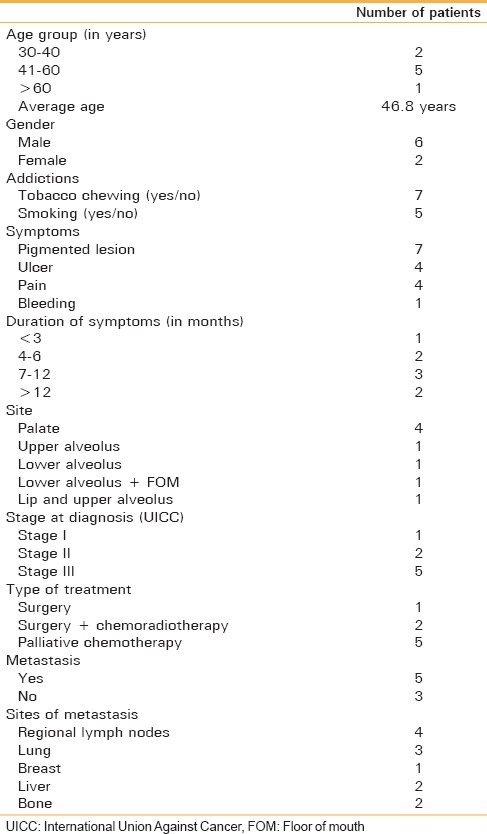
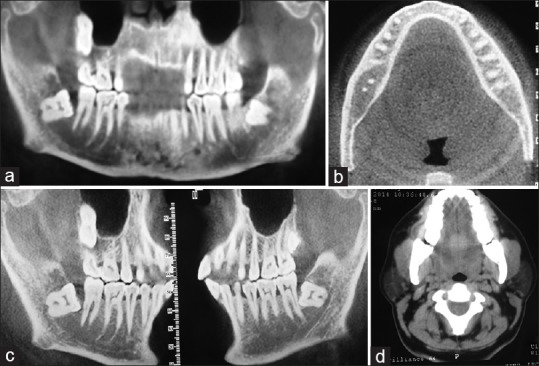
Orthopantomogram and CT scan were the imaging modalities used to know the site and extent of the tumor [Figure 2a–d]. PET scan was done in two patients as a part of staging purpose [Figure 3a and b]. Patients were staged as per International Union Against Cancer (UICC) staging. Majority of patients (5 patients [62.5%]) were diagnosed with Stage III (distant metastasis), two patients in Stage II, and one patient in Stage I. Most common site of metastasis was regional lymph nodes, lung, followed by bone and liver with breast being one of the rare sites. Diagnosis of all patients was confirmed with punch/incision biopsy [Figure 4].
Figure 2.
(a-d) Orthopantomogram and computed tomography scan showed cortical erosion of the mandibular bone (right side)
Figure 3.
(a) Positron emission tomography scan showing increased tracer activity in the right mandibular region. (b) Positron emission tomography scan showing extensive skeletal metastasis with increased tracer uptake in hard palate
Figure 4.
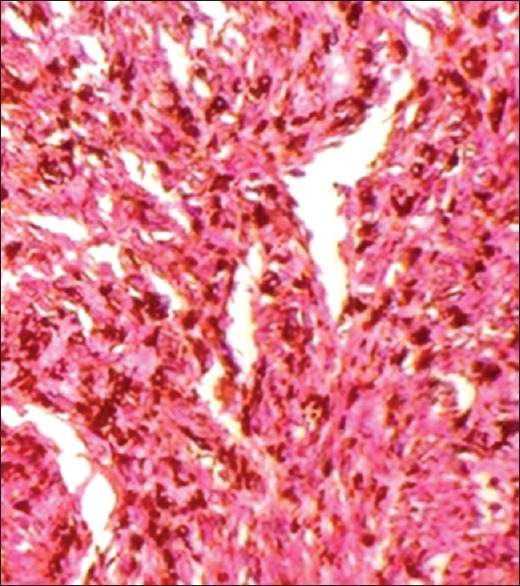
Photomicrograph showing a hypercellular tumor with spindle-shaped melanocytes suggestive of malignant melanoma
Treatment modalities
Three patients were treated with definitive surgery [Figure 5a and b] and five patients with palliative chemotherapy in view of distant disease. Following surgery, two of them required adjuvant chemoradiotherapy in view of node positivity [Table 2].
Figure 5.

(a) Intraoperative photograph showing exophytic pigmented growth arising from mandibular gingiva. (b) Surgical resection specimen showing a pigmented tumor arising from mandibular gingiva
Table 2.
Treatment modalities and outcome of 8 patients of oral malignant melanoma
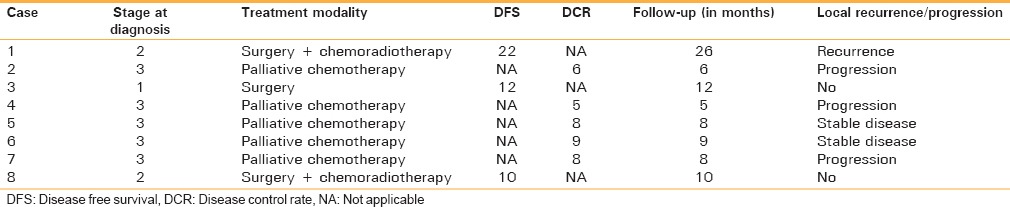
Outcome
Patients were followed up for 8 months to 26 months with a mean follow-up of 10.5 months. Patients treated with definitive surgery had a better survival (10–26 months, mean - 16 months), with local recurrence in one patient. Metastatic melanoma patients treated with palliative chemotherapy had a mean disease control rate of 5 months (range 5–9 months) [Table 2].
DISCUSSION
Most common site for head and neck melanoma is conjunctiva, followed by upper respiratory tract. Mucosal melanoma of the oral cavity is the unusual malignancy accounting for 0.2–8% of all the melanomas affecting the patients.[4] Jackson and Simpson have described that melanomas of the oral cavity account for <2% of all melanomas, while Reddy et al. have reported an incidence of 0.3–1.3%.[9,10] It has a poor prognosis due to several characteristics such as remaining asymptomatic for a long time, which leads to its late discovery.[4]
Oral melanomas may be primary or metastatic lesion from other sites. Greene et al. described the criteria for primary oral malignant melanoma which includes demonstration of clinical and microscopic evidence of melanoma in the oral mucosa, presence of junctional activity, and inability to demonstrate extraoral primary melanoma.[11] Exact etiopathogenesis is not well understood. Precursor lesion such as preexisting melanosis or atypical melanocytic hyperplasia may represent a proliferative phase before overt tumorigenesis occurs.[1] Mechanical trauma such as dental irritation, tobacco use, exposure to formaldehyde, and alcohol are the other possible etiological factors.[4]
The average age of the cases studied was 46.8 years, and 75% of patients were above the age of 40 years, which agrees with Doval et al. and Tanaka et al. Rapidis et al. reported that this disease is unusual before the age of 30 years supporting the above study.[12,13,14]
In the present study, there was a male preponderance (3:1 ratio), which agrees with a review of literature.[8] However, some studies such as studies by Lopez-Graniel et al. and Chidzonga's et al. have noted female preponderance.[15,16]
Majority of patients in the present study had a history of tobacco chewing (87.5% cases) and smoking (62.5%). However, no etiologic factors have been identified for oral melanomas. In comparison to cutaneous or other site melanomas which are believed to arise from a nevus, primary oral melanomas present as pigmented areas or de novo (30% cases).
Oral melanomas are usually asymptomatic and usually present late with symptoms resulting from ulceration, growth, or bleeding. Most of the patients had pigmented lesions/ulceration at presentation (7 out of 8 cases). Around 50% of cases had pain and one presented with bleeding from ulcerated lesion. Oral melanomas are highly aggressive in nature due to hematogenous spread early in the course of the disease.
The present study found hard palate as the most frequent site of disease (50% cases), finding relation with Meleti et al.[17] Other less common sites were upper alveolus, lower alveolus, and FOM as in the Lopez-Graneil et al.'s study, who noted 73% cases had disease in hard palate.[15]
In our study, most of the patients presented at advanced stage. Five cases had distant metastases; among them, lung was the most common site of distant metastasis followed by liver and bone. One patient had metastasis to breast. These results agrees with that of Temam et al., who reported lung metastasis in 53%, bone metastasis in 36%, liver metastasis in 20%, and brain metastasis in 20% cases.[18]
Patients were staged according to UICC Staging: Stage I confined to oral cavity, Stage II to positive cervical nodes, and Stage III to distant metastasis. One patient had Stage I disease and underwent surgery and two patients had Stage II disease at diagnosis and had undergone surgery plus chemoradiotherapy. Five patients presented with distant metastasis and started on palliative chemotherapy. Most important factors determining oral melanoma prognosis include tumor thickness, depth, and stage at presentation, which is related to poor outcome.
The mainstay of treatment of patients with head and neck mucosal melanomas is surgery, which entails complete resection of the primary tumor and any positive cervical lymph nodes.[19] Postoperative RT should be considered to reduce the likelihood of local–regional recurrence.[20]
CONCLUSION
Primary oral melanoma is a rare condition with poor prognosis. Any pigmented lesion in oral cavity should have an index of suspicion, which should be investigated to detect the disease at an early stage and managed appropriately. Tumor size and metastases are related to the prognosis of the disease. Oral melanomas usually present in advanced stage and carries worse prognosis as compared to cutaneous melanomas. The main treatment modality is surgical resection, which offers the best chance for long-term survival. The present study highlights that an early diagnosis and interventions are required to improve the prognosis of the patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Our sincere thanks to Prof. Ravikant, Vice Chancellor, King George Medical University, Lucknow, for guiding and permitting to publish this article.
REFERENCES
- 1.Hicks MJ, Flaitz CM. Oral mucosal melanoma: Epidemiology and pathobiology. Oral Oncol. 2000;36:152–69. doi: 10.1016/s1368-8375(99)00085-8. [DOI] [PubMed] [Google Scholar]
- 2.Aguas SC, Quarracino MC, Lence AN, Lanfranchi-Tizeira HE. Primary melanoma of the oral cavity: Ten cases and review of 177 cases from literature. Med Oral Patol Oral Cir Bucal. 2009;14:E265–71. [PubMed] [Google Scholar]
- 3.Rapini RP, Golitz LE, Greer RO, Jr, Krekorian EA, Poulson T. Primary malignant melanoma of the oral cavity. A review of 177 cases. Cancer. 1985;55:1543–51. doi: 10.1002/1097-0142(19850401)55:7<1543::aid-cncr2820550722>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 4.Guevara-Canales JO, Gutiérrez-Morales MM, Sacsaquispe-Contreras SJ, Sánchez-Lihón J, Morales-Vadillo R. Malignant melanoma of the oral cavity. Review of the literature and experience in a Peruvian population. Med Oral Patol Oral Cir Bucal. 2012;17:e206–11. doi: 10.4317/medoral.17477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ebenezer J. Malignant melanoma of the oral cavity. Indian J Dent Res. 2006;17:94–6. doi: 10.4103/0970-9290.29882. [DOI] [PubMed] [Google Scholar]
- 6.González-García R, Naval-Gías L, Martos PL, Nam-Cha SH, Rodríguez-Campo FJ, Muñoz-Guerra MF, et al. Melanoma of the oral mucosa. Clinical cases and review of the literature. Med Oral Patol Oral Cir Bucal. 2005;10:264–71. [PubMed] [Google Scholar]
- 7.Shah JP, Kraus DH, Dubner S, Sarkar S. Patterns of regional lymph node metastases from cutaneous melanomas of the head and neck. Am J Surg. 1991;162:320–3. doi: 10.1016/0002-9610(91)90140-9. [DOI] [PubMed] [Google Scholar]
- 8.McLean N, Tighiouart M, Muller S. Primary mucosal melanoma of the head and neck. Comparison of clinical presentation and histopathologic features of oral and sinonasal melanoma. Oral Oncol. 2008;44:1039–46. doi: 10.1016/j.oraloncology.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 9.Jackson D, Simpson HE. Primary malignant melanoma of the oral cavity. Oral Surg Oral Med Oral Pathol. 1975;39:553–9. doi: 10.1016/0030-4220(75)90194-2. [DOI] [PubMed] [Google Scholar]
- 10.Reddy CR, Rao TR, Ramulu C. Primary malignant melanoma of the hard palate. J Oral Surg. 1976;34:937–9. [PubMed] [Google Scholar]
- 11.Greene GW, Haynes JW, Dozier M, Blumberg JM, Bernier JL. Primary malignant melanoma of the oral mucosa. Oral Surg Oral Med Oral Pathol. 1953;6:1435–43. doi: 10.1016/0030-4220(53)90242-4. [DOI] [PubMed] [Google Scholar]
- 12.Doval DC, Rao CR, Saitha KS, Vigayakumar M, Misra S, Mani K, et al. Malignant melanoma of the oral cavity: Report of 14 cases from a regional cancer centre. Eur J Surg Oncol. 1996;22:245–9. doi: 10.1016/s0748-7983(96)80011-4. [DOI] [PubMed] [Google Scholar]
- 13.Tanaka N, Mimura M, Ogi K, Amagasa T. Primary malignant melanoma of the oral cavity: Assessment of outcome from the clinical records of 35 patients. Int J Oral Maxillofac Surg. 2004;33:761–5. doi: 10.1016/j.ijom.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Rapidis AD, Apostolidis C, Vilos G, Valsamis S. Primary malignant melanoma of the oral mucosa. J Oral Maxillofac Surg. 2003;61:1132–9. doi: 10.1016/s0278-2391(03)00670-0. [DOI] [PubMed] [Google Scholar]
- 15.Lopez-Graniel CM, Ochoa-Carrillo FJ, Meneses-García A. Malignant melanoma of the oral cavity: Diagnosis and treatment experience in a Mexican population. Oral Oncol. 1999;35:425–30. doi: 10.1016/s1368-8375(99)00017-2. [DOI] [PubMed] [Google Scholar]
- 16.Chidzonga MM, Mahomva L, Marimo C, Makunike-Mutasa R. Primary malignant melanoma of the oral mucosa. J Oral Maxillofac Surg. 2007;65:1117–20. doi: 10.1016/j.joms.2006.11.045. [DOI] [PubMed] [Google Scholar]
- 17.Meleti M, Mooi WJ, Casparie MK, van der Waal I. Melanocytic nevi of the oral mucosa – No evidence of increased risk for oral malignant melanoma: An analysis of 119 cases. Oral Oncol. 2007;43:976–81. doi: 10.1016/j.oraloncology.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 18.Temam S, Mamelle G, Marandas P, Wibault P, Avril MF, Janot F, et al. Postoperative radiotherapy for primary mucosal melanoma of the head and neck. Cancer. 2005;103:313–9. doi: 10.1002/cncr.20775. [DOI] [PubMed] [Google Scholar]
- 19.Lazarev S, Gupta V, Hu K, Harrison LB, Bakst R. Mucosal melanoma of the head and neck: A systematic review of the literature. Int J Radiat Oncol Biol Phys. 2014;90:1108–18. doi: 10.1016/j.ijrobp.2014.03.042. [DOI] [PubMed] [Google Scholar]
- 20.Mendenhall WM, Amdur RJ, Hinerman RW, Werning JW, Villaret DB, Mendenhall NP. Head and neck mucosal melanoma. Am J Clin Oncol. 2005;28:626–30. doi: 10.1097/01.coc.0000170805.14058.d3. [DOI] [PubMed] [Google Scholar]