Abstract
Eosinophilic ulcer of the oral mucosa is considered to be a benign, reactive, and self-limiting lesion, with unclear pathogenesis, manifesting as a rapidly developing solitary ulcer. We report a case of a 42-year-old man who presented with a chronic indurated ulcer of buccal mucosa adjacent to the right upper wisdom tooth. Histopathological examination showed polymorphic inflammatory infiltrate, rich in eosinophilis, involving the superficial mucosa, and the deeper muscle layer. Immunohistochemical analysis revealed single CD30+ cells scattered within an inflammatory infiltrate. The lesion was excised, and healing was uneventful with no recurrence in more than a year.
Keywords: Eosinophilic ulcer, non healing ulcer, traumatic ulcer
INTRODUCTION
Eosinophilic ulcer of the mucosa is an uncommon self-limited oral condition that clinically manifests as a solitary ulceration with elevated indurated borders affecting tongue, buccal mucosa, or lip with pathogenesis still unclear, however, it may resemble malignancies, traumatic ulcerations, and some infections such as deep fungal infections, tuberculosis, and primary syphilis. Histological findings are characteristic and consist of eosinophilic-rich mixed infiltrates accompanied by the population of large mononuclear cells whose origins have been a matter of a debate, mostly thought to be corresponding to histiocytes, myofibroblasts, or activated lymphoid cells.[1,2,3,4]
Eosinophilic ulcer also has been referred as traumatic ulcerative granuloma with stromal eosinophilia, traumatic eosinophilic granuloma, traumatic granuloma, and ulcerative eosinophilic granuloma.[4,5,6,7] In infants, usually on the ventral surface of the anterior tongue secondary to trauma from newly erupted primary teeth, the eosinophilic ulcer is referred as Riga–Fede disease.[8,9,10]
We present a patient with eosinophilic ulcer affecting the right cheek mucosa.
CASE REPORT
A 40-year-old male was referred to oral surgery speciality at HCF Dental Centre, Sydney for opinion and treatment of a chronic ulcer. The patient stated that the lesion had first occurred 6 months back which had increased in size and giving him more discomfort. He was apparently fit and well and not on any medications.
Clinical examination revealed a large ulcer in the right buccal mucosa adjacent to tooth number 18. The ulcer was about 4 and 5 cm with the grayish pink base and indurated margins [Figure 1]. Tooth number 18 was buccally inclined and difficult to clean. There were no palpebal lymph nodes. The patient did not recall any trauma to cheek in the past.
Figure 1.

Clinical photograph showing indurated ulcer on the right buccal mucosa
He visited a dentist initially about 6 months back with the symptom of pain and discomfort in that region to be looked at. The patient was diagnosed as temporomandibular joint pain on the right side and was advised symptomatic treatment. There was no mention of any ulcer which might have been missed during the first visit. Subsequently, the area did not get better and he visited again to be checked after 5 months. Then, he was diagnosed as a chronic ulcer and got referred to oral surgery.
Considering chronicity of the ulcer and its indurated margin it was decided to have an excisional/incisional biopsy and the removal of tooth number 18 which could have been a causative factor for trauma. The patient decided to seek the second opinion where he was advised the same line of treatment.
He decided to have a biopsy and removal of the tooth under general anesthetic. After removal of tooth number 18, the exposure of ulcer was good and an excisional biopsy was performed with safety margins. The area was sutured primarily. The postoperative period was uneventful and the wound healed within 3 weeks without any complications [Figure 2]. A follow-up of a year showed no recurrence or abnormalities.
Figure 2.

One-week postoperative photograph after excisional biopsy
Microscopic examination revealed the extent of ulceration, and all sections presented similar histologic features. The surrounding epithelium was intact and well differentiated though slightly hyperplasic. The cellular infiltrate within the submucosal tissue consisted predominantly of eosinophils with a few scattered lymphocytes, plasma cells, and lymphocytes [Figure 3].
Figure 3.
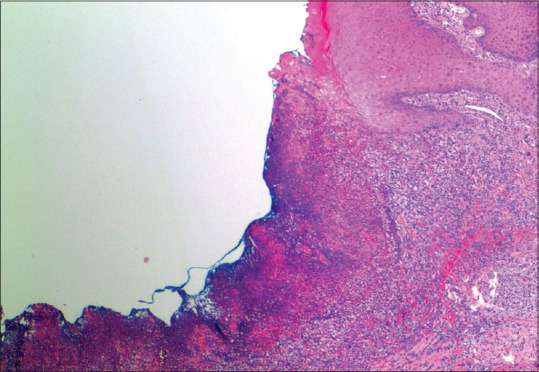
Histopathological features presence of fibroprulent membrane and dense lymphocytic infiltrate (H and E)
The inflammatory infiltrate included numerous mast cells, particularly in the corium adjacent to the hyperplastic epithelium. The infiltrated tissue was well vascularized. No atypical cells or signs of granulomatous infiltration were seen [Figure 4]. A follow-up of a year showed no recurrence or abnormalities [Figure 5].
Figure 4.
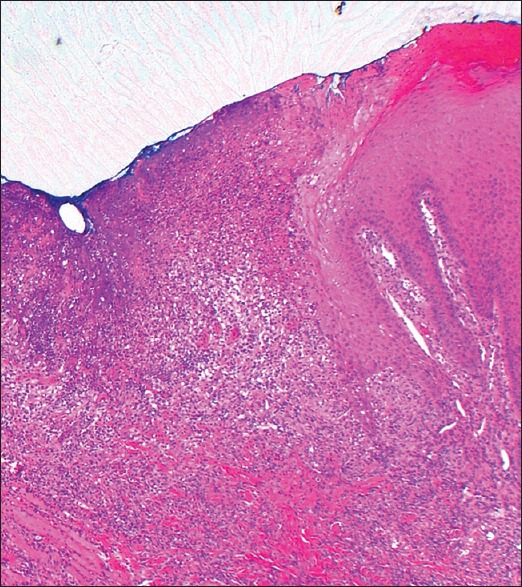
Histophotomicrograph showing no atypical cells or granulomatous infiltration
Figure 5.

Clinical photograph after 1 year
DISCUSSION
Eosinophilic ulcer of the oral mucosa is also known as traumatic ulcerative granuloma with stromal eosinophilia, oral traumatic granuloma, traumatic ulcer, or eosinophilic ulcer of the tongue. It usually affects older adults but may occur at any age, including children, and may or may not be painful. It often occurs on the lateral tongue but may also be seen in gingival and other areas of oral mucosa. It usually appears as a sharp, punched-out ulcer, often with a surrounding pale indurated rim that is, clinically suspicious for malignancy. There may be exuberant polypoidal pyogenic granuloma-like granulation tissue.[1,2,4,11]
It may be present for weeks and may or may not be painful. Multiple ulcers may occur, either simultaneously or recurrently. These ulcers are often self-healing but many may persist for weeks or longer.
The cause is usually unknown but there is often an association with trauma (hence the term “traumatic ulcer”), particularly in younger patients in relation to newly erupted teeth.
Microscopically there is usually (as in this case) a deep ulcer with associated dense acute and chronic inflammation extending into deep underlying tissue, sometimes involving voluntary muscle. The infiltrate includes numerous lymphocytes and eosinophils, together with some normal histiocytes. Large, atypical, CD30-positive mononuclear cells may be present in some patients, raising the possibility that these lesions may be part of an evolving CD30 + lymphoproliferative disorder.[2,10,12,13] Further investigations may then be indicated to exclude this possibility, depending on clinical evaluation, and any relevant history.
In some cases, as in the current patient, there is surrounding epithelial hyperplasia with atypia that may mimic malignancy, both clinically and histologically. However, especially in a longstanding ulcer, the atypia is more likely to be reactive in nature.[5,6]
Pathologically, the differential diagnoses include squamous carcinoma or lymphoma, as noted above. Viral infection, such as due to herpes or Epstein–Barr virus, may also cause oral ulceration. Other less likely differential diagnoses include the granulomas of mycobacterial, or deep mycotic infection, or tertiary syphilis. Smaller ulcers may be seen in autoimmune disease (e.g., Sjogren's syndrome), granulomatous cheilitis, and Crohn's disease.[3,13,14,15,16] The clinical and microscopic features together with special stains for micro-organisms and immunohistochemical markers should assist in distinguishing these conditions.
Most simple ulcers of the oral cavity do not contain significant numbers of eosinophils and the reason for their presence in this type of lesion is unknown. They may be due to released tissue toxins or other reactants.[14,15,16,17] Eosinophils may be present in a variety of cutaneous and gastrointestinal conditions, often related to allergic, parasitic or drug-related causes, or as part of a systemic eosinophilia. However, in the most cases of oral eosinophilic ulceration these conditions are not evident.
The ulcers often spontaneously heal after the biopsy. However, recurrence is common, particularly if there is persistent trauma. Where there is associated atypical epithelial hyperplasia, clinical follow-up is important to exclude the possibility of developing malignancy, as in this case.
Despite the similarity in terminology, the eosinophilic granuloma is clinically and microscopically a distinct condition, being related to or a subtype of histiocytosis-X or Langerhans cell histiocytosis. This type of lesion is unusual in oral mucosa but does have a predilection for the bones of the jaw, more often the mandible, where it may cause a localized ragged zone of destruction.[4,18,19,20] The disease may be localized to a single site (then called “eosinophilic granuloma”) or may manifest as a part of a systemic histiocytosis involving several different organs, such as bone (as above), skin, lymph nodes, spleen, lungs, gastrointestinal tract, and other areas. Histologically these lesions show diffuse interstitial infiltration by large atypical histiocytes with accompanying eosinophils.[11,21] The presence of an eosinophilic granuloma or a similar histiocytic lesion is, therefore, an indication for further investigation to exclude systemic disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Regezi JA, Zarbo RJ, Daniels TE, Greenspan JS. Oral traumatic granuloma. Characterization of the cellular infiltrate. Oral Surg Oral Med Oral Pathol. 1993;75:723–7. doi: 10.1016/0030-4220(93)90430-c. [DOI] [PubMed] [Google Scholar]
- 2.Lourenço SV, Silva MA, Nico MM. An ulcer on the lip. Clin Exp Dermatol. 2005;30:199–200. doi: 10.1111/j.1365-2230.2005.01724.x. [DOI] [PubMed] [Google Scholar]
- 3.Segura S, Romero D, Mascaró JM, Jr, Colomo L, Ferrando J, Estrach T. Eosinophilic ulcer of the oral mucosa: Another histological simulator of CD30 lymphoproliferative disorders. Br J Dermatol. 2006;155:460–3. doi: 10.1111/j.1365-2133.2006.07331.x. [DOI] [PubMed] [Google Scholar]
- 4.Hirshberg A, Amariglio N, Akrish S, Yahalom R, Rosenbaum H, Okon E, et al. Traumatic ulcerative granuloma with stromal eosinophilia: A reactive lesion of the oral mucosa. Am J Clin Pathol. 2006;126:522–9. doi: 10.1309/AFHA406GBT0N2Y64. [DOI] [PubMed] [Google Scholar]
- 5.Kumar SK, Dhyllon A, Sedghizadeh PP. Indurated tongue lesion. J Am Dent Assoc. 2008;139:159–61. doi: 10.14219/jada.archive.2008.0131. [DOI] [PubMed] [Google Scholar]
- 6.Boffano P, Gallesio C, Campisi P, Roccia F. Traumatic ulcerative granuloma with stromal eosinophilia of the retromolar region. J Craniofac Surg. 2009;20:2150–2. doi: 10.1097/SCS.0b013e3181bec6f0. [DOI] [PubMed] [Google Scholar]
- 7.Gagari E, Stathopoulos P, Katsambas A, Avgerinou G. Traumatic ulcerative granuloma with stromal eosinophilia: A lesion with alarming histopathologic presentation and benign clinical course. Am J Dermatopathol. 2011;33:192–4. doi: 10.1097/DAD.0b013e3181e26db0. [DOI] [PubMed] [Google Scholar]
- 8.el-Mofty SK, Swanson PE, Wick MR, Miller AS. Eosinophilic ulcer of the oral mucosa. Report of 38 new cases with immunohistochemical observations. Oral Surg Oral Med Oral Pathol. 1993;75:716–22. doi: 10.1016/0030-4220(93)90429-8. [DOI] [PubMed] [Google Scholar]
- 9.Riga A. Di una malattia della prima infanzia, Probabilmente non-trattata, di movimenti patologici. Napoli. 1881 [Google Scholar]
- 10.Fede F. Della produzione sottolinguale o malattia di Riga. Atto Congresso italiano di pediatria 1890. Napoli. 1891:251. [Google Scholar]
- 11.Segura S, Pujol RM. Eosinophilic ulcer of the oral mucosa: A distinct entity or a non-specific reactive pattern? Oral Dis. 2008;14:287–95. doi: 10.1111/j.1601-0825.2008.01444.x. [DOI] [PubMed] [Google Scholar]
- 12.Elzay RP. Traumatic ulcerative granuloma with stromal eosinophilia (Riga-Fede's disease and traumatic eosinophilic granuloma) Oral Surg Oral Med Oral Pathol. 1983;55:497–506. doi: 10.1016/0030-4220(83)90236-0. [DOI] [PubMed] [Google Scholar]
- 13.Pilolli GP, Lucchese A, Scivetti M, Maiorano E, Favia G. Traumatic ulcerative granuloma with stromal eosinophilia of the oral mucosa: Histological and immunohistochemical analysis of three cases. Minerva Stomatol. 2007;56:73–9. [PubMed] [Google Scholar]
- 14.Alobeid B, Pan LX, Milligan L, Budel L, Frizzera G. Eosinophil-rich CD30 lymphoproliferative disorder of the oral mucosa. A form of “traumatic eosinophilic granuloma”. Am J Clin Pathol. 2004;121:43–50. doi: 10.1309/JQFX-PND6-DBLF-6B9U. [DOI] [PubMed] [Google Scholar]
- 15.Woo SB. USA: Elsevier Saunders; 2012. In Oral Pathology, A Comprehensive Atlas and Text; pp. 140–1. [Google Scholar]
- 16.Fonseca FP, de Andrade BA, Coletta RD, Vargas PA, Lopes MA, de Almeida OP, et al. Clinicopathological and immunohistochemical analysis of 19 cases of oral eosinophilic ulcers. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:532–40. doi: 10.1016/j.oooo.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 17.Chatzistamou I, Doussis-Anagnostopoulou I, Georgiou G, Gkilas H, Prodromidis G, Andrikopoulou M, et al. Traumatic ulcerative granuloma with stromal eosinophilia: Report of a case and literature review. J Oral Maxillofac Surg. 2012;70:349–53. doi: 10.1016/j.joms.2011.03.026. [DOI] [PubMed] [Google Scholar]
- 18.Lombardi T, Küffer R, Samson J. Eosinophilic ulceration of the oral mucosa. A case report. Int J Oral Maxillofac Surg. 1993;22:366–7. doi: 10.1016/s0901-5027(05)80670-8. [DOI] [PubMed] [Google Scholar]
- 19.Bortoluzzi MC, Passador-Santos F, Capella DL, Manfro G, Nodari RJ, Jr, Presta AA. Eosinophilic ulcer of oral mucosa: A case report. Ann Stomatol (Roma) 2012;3:11–3. [PMC free article] [PubMed] [Google Scholar]
- 20.Damevska K, Gocev G, Nikolovska S. Eosinophilic ulcer of the oral mucosa: Report of a case with multiple synchronous lesions. Am J Dermatopathol. 2014;36:594–6. doi: 10.1097/DAD.0b013e31829ae478. [DOI] [PubMed] [Google Scholar]
- 21.Ficarra G, Prignano F, Romagnoli P. Traumatic eosinophilic granuloma of the oral mucosa: A CD30+ (Ki-1) lymphoproliferative disorder? Oral Oncol. 1997;33:375–9. doi: 10.1016/s1368-8375(97)00014-6. [DOI] [PubMed] [Google Scholar]


