Abstract
This qualitative study describes the temporal patterns of fatigue found as part of a larger study designed to elicit a description of the experience and self-management of fatigue for patients on hemodialysis. Two patterns of fatigue were identified. The first pattern, continuous fatigue, was characterized by participants who experienced fatigue at all times, which was their normal, baseline feeling. Within this group, two subgroups were identified. The second pattern of fatigue, post-dialysis fatigue only, was characterized by participants who experienced fatigue only after their hemodialysis session. This study is unique because it expands our knowledge about hemodialysis and fatigue by describing the patterns that fatigue follows over time from one hemodialysis session to the next. Insight into these phenomena could help ameliorate fatigue and allow nurses to tailor interventions for patients on hemodialysis.
Keywords: Hemodialysis, fatigue, temporal pattern
Fatigue is identified by patients on hemodialysis as a symptom they experience and with which they frequently struggle (Jablonski, 2007; Weisbord et al., 2005). Patients on hemodialysis around the world are impacted by its effects. Research indicates that patients on hemodialysis in Europe, Asia, and the Middle East felt the most fatigue immediately after hemodialysis, were not able to carry out daily activities, and experienced role limitations and a decrease in strength and physical ability due to their fatigue (Heiwe, Clyne, & Dahlgren, 2003; Kazemi, Nasrabadi, Hasanpour, Hassankhani, & Mills, 2011; Lee, Lin, Chaboyer, Chiang, & Hung, 2007). Further, they had trouble remembering and concentrating due to fatigue (Heiwe et al., 2003; Lee et al., 2007). Patients on hemodialysis in the United States described a similar physical and mental fatigue that affected their ability to carry out daily activities, remember, and concentrate, and they experienced their worst fatigue after their hemodialysis session (Horigan, Schneider, Docherty & Barroso, 2013). Clearly, fatigue affects the lives of patients on hemodialysis worldwide.
Of particular interest with regard to the experience of fatigue are the temporal patterns of the symptom, times when it is the most and least severe, and its duration and frequency. There has been little work in the area of identifying temporal patterns of fatigue in patients on hemodialysis. Post-dialysis fatigue is identified in the literature, but it is not adequately defined. What is known comes from the early work of Sklar and colleagues (Sklar, Riesenber, Silber, Ahmed, & Ali, 1996; Sklar et al, 1999). Post-dialysis fatigue is a frequent complaint of patients on hemodialysis, it occurs after dialysis sessions, and those who experience it require more sleep immediately after dialysis (Sklar et al., 1996). Patients who experience post-dialysis fatigue require almost five hours of sleep to recover after their sessions and had more depression, insomnia, and body aches than those who did not experience post-dialysis fatigue (Sklar et al., 1996). Further, patients with post-dialysis fatigue experienced limitations in their functional independence and participation in social activities on the day of dialysis (Rocco, Mercieri, & Yavuzer, 2006). Post-dialysis fatigue is debilitating on dialysis session days for those who experience it, but elucidating a definition of post-dialysis fatigue is complicated because there has been no further work done to specify the characteristics of the phenomenon. Limited research indicates there is no definitive cause of post-dialysis fatigue, but the lack of work in this area makes it difficult to draw conclusions.
The causes of post-dialysis fatigue largely remain a mystery. Post-dialysis fatigue is not predicted by clinical measures, such as nutritional status, lab results, the adequacy of dialysis, or activity level (Leinau, Murphy, Bradley, & Fried, 2009; Liu, 2006; Morsch, Goncalves, & Barros, 2006; Sklar et al.,1996). Research suggests that it may be part of a symptom complex or syndrome that includes symptoms of nausea, muscle cramps, and headache that may be due to the fluid shifts that occur during hemodialysis (Sklar et al., 1999). Further, post-dialysis fatigue seems to be ameliorated by rest and sleep (Sklar et al., 1996). While this information is important, it is the only research of its kind, and without additional research, it cannot be taken as proof that post-dialysis fatigue is part of a symptom complex or that it is not correlated with clinical measures. Further work in this area is warranted to help remedy these gaps in knowledge.
Two dialysis-related variables have been studied in relation to post-dialysis fatigue; however, these studies are few in number. Singh et al. (2003) studied post-dialysis fatigue in relation to dialysis membrane composition and cytokine production. They found that cytokine levels increased significantly with both types of dialyzer membranes but that levels of post dialysis fatigue did not vary between dialyzer membranes (Singh et al., 2003). Azar (2009) studied the effect of cooling the dialysate temperature on levels of post-dialysis fatigue and found that levels and the length of time post-dialysis fatigue lasted improved significantly when the dialysate was cooled. These studies point to areas that are in need of further research.
Post-dialysis fatigue has also been studied in relation to muscle function and exercise, but again, these studies are limited, and conceptually, the definition of post-dialysis fatigue is not well-delineated in this research. Delgado and Johansen (2012) studied barriers to exercise in patients on hemodialysis. They found that the most commonly reported barrier to exercise was fatigue, but it was not associated with decreased activity levels (Delgado & Johansen, 2012). In their abstract, the authors note that “post-dialysis fatigue was not associated with differences in activity level in multivariate analysis” (Delgado & Johansen, 2012, p. 1152). Yet in the body of the article, post-dialysis fatigue is not mentioned again; rather, the authors refer to fatigue. It seems, but is not clear, that the terms fatigue and post-dialysis fatigue were used interchangeably.
Lockhart et al. (2010) studied the effect of several mobility measures and post-dialysis fatigue on the incidence of falls in elderly patients on hemodialysis and found that post-dialysis fatigue increased susceptibility to falls when elderly patients returned home from hemodialysis. It is not clear what these authors used as their operational definition of post-dialysis fatigue because they reported measures of strength, post-uro locomotion tests, dynamic stability, and get up and go times. It is possible they used strength as a proxy for post-dialysis fatigue or a combination of all measures as an overall measure for post-dialysis fatigue. The lack of a clear conceptualization of fatigue in this work makes it difficult to make assumptions about the effect of post-dialysis fatigue on these variables and points to the need for a clear definition of post-dialysis fatigue.
Post-dialysis fatigue may be conceptually similar to the continuous fatigue that patients on hemodialysis experience, but it differs in severity and timing. It is important to clarify if and how post-dialysis fatigue differs from the continuous fatigue patients on hemodialysis experience to intervene effectively. Further, predictors may be responsible for phenomena amenable to intervention. Whether the phenomenon of post-dialysis fatigue progresses to a continuous state is unknown, and if so, at what point, to whom does this occur, and what factors may be associated with this change? Insight into these phenomena will expand our knowledge base, and identify areas for further research and ways to tailor interventions for fatigue as experienced by patients on hemodialysis. Therefore, the purpose of this article is to describe the temporal patterns of fatigue over a 36-hour period, from one hemodialysis session to the next.
Methods
This study is part of a larger study that was designed to investigate the experience and self-management of fatigue in patients on hemodialysis. Details about these findings have been reported previously (Horigan et al., 2013). The present results expand these findings by describing the temporal patterns of fatigue for patients on hemodialysis over a 36-hour period, from one hemodialysis session to the evening before the next session. The study setting and sample, procedures, data collection, and data analysis have been reported in detail (Horigan et al., 2013). Therefore, only abbreviated descriptions or aspects of the study method unique to the description of the temporal patterns of fatigue will be discussed here.
Design
A qualitative descriptive design (Neergaard, Olesen, Andersen & Sondergaard, 2009; Sandelowski, 2000) was used to investigate the temporal patterns of fatigue for patients on hemodialysis. This included in-depth interviews followed by the completion of a 36-hour fatigue diary. Follow-up interviews were conducted to clarify information gleaned from the initial interviews and fatigue diaries, and to conduct member checks.
Setting and Sample
Participants were recruited from a local hemodialysis center in a rural area in the Mid-Atlantic region. Interviews with participants took place wherever participants felt it was most convenient for them, most often in their homes on days when they did not have hemodialysis (n = 13). At times, it was more convenient for participants to be interviewed before their hemodialysis sessions. These interviews were conducted at the hemodialysis center in a private conference room. No interviews were conducted during hemodialysis sessions. Data from all 14 participants were used to investigate the temporal patterns of fatigue in this population.
Procedures
After Institutional Review Board approval was obtained, an employee from the hemodialysis center approached patients, gave a very brief description of the study, and asked if they would be interested in speaking with the first author (Horigan) about it. If patients were willing, the first author then spoke with them about what the study would entail. If patients agreed and met inclusion and exclusion criteria, the first author made an appointment to come to the place most convenient for the patient to review the consent form, obtain their informed consent, collect demographic data, and conduct the first interview.
Instruments
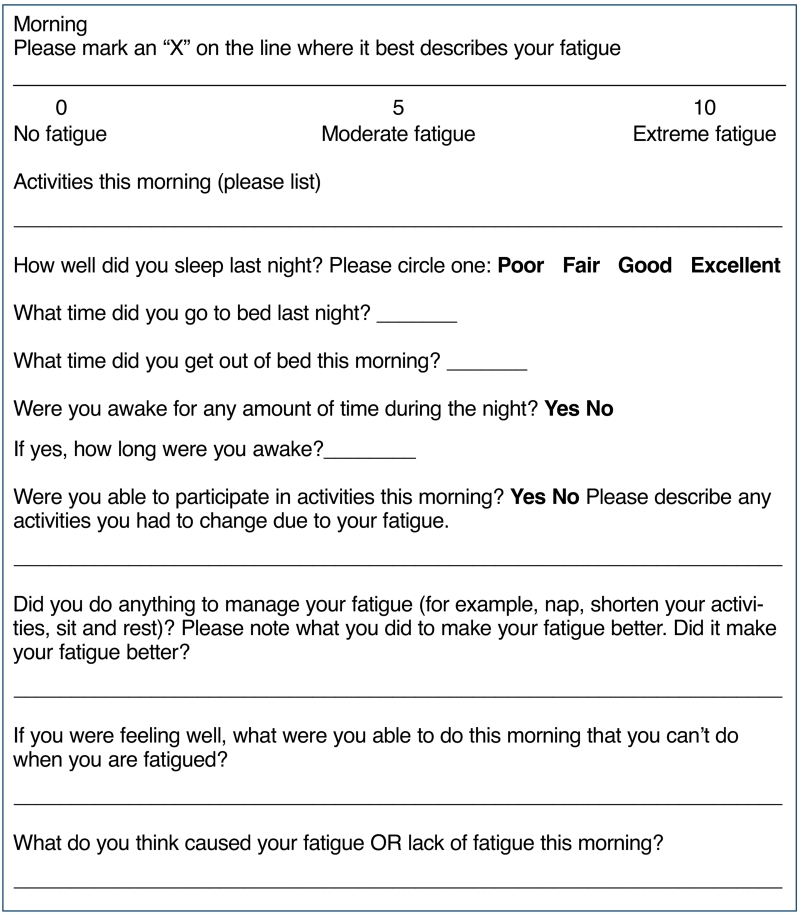
Participants were asked to fill out a 36-hour fatigue diary during the week. There were four entry points for each day contained in the diary: morning, afternoon, evening, and night. When instructions on how to complete the diary were reviewed with participants, the above timeframes were discussed. While the time for recording data in the fatigue diary was not prescriptive, in general, it was suggested that participants record the morning data around the time they ate breakfast, the afternoon data around the time they at lunch, the evening data around supper, and nighttime data near the time they went to bed. In the morning entry point, participants were asked to rate their sleep quality from the night before as poor, fair, good, or excellent. They were asked to record what time they went to bed the night before and what time they got up on the current day. They were also asked to note if they were awake at any point during the night, and if so, for how long. All diary entry points had a visual analogue scale on which participants were asked to mark their level of fatigue at that time with “0” indicating no fatigue and “10” indicating extreme fatigue; to list any activities they were able to participate in and any they had to change due to their fatigue; to note anything they did to manage their fatigue at that point and if it made their fatigue better; if they were feeling well, what were they able to do that they were not usually able to do when they were fatigued; and what they thought caused their fatigue or lack of fatigue. The afternoon (between lunch and dinner), evening, and night entry points also asked that participants compare their fatigue to the previous entry and note any changes in fatigue level and why they thought their fatigue had changed. See Figure 1 for a sample diary page.
Figure 1. Sample Diary.
Data collection
Individual, semi-structured interviews were conducted by the first author. These interviews are an appropriate data collection method when the researcher knows enough about the phenomenon to devise questions prior to the interview but not enough to anticipate subject’s answers (Richards, 2006). Further, because hemodialysis schedules are fairly complicated, requiring patients to attend sessions for three to four hours, three times weekly, individual interviews were the most pragmatic method of data collection for this study. Field notes were written immediately after each interview by the first author to capture the natural environment of the subject and to use in validation of the interview data.
When the interview was completed, participants were given a fatigue diary to complete. Symptom diaries are useful because they provide convergent evidence and the unique viewpoint of the participant (Broom & Tovey, 2008; Furness & Garrud, 2010). They have been used successfully in patients on hemodialysis in previous studies (Yngman-Uhlin & Edell-Gustafsson, 2006). Instructions on how to complete the diary were reviewed and any questions answered. Participants were asked to start the diary entry on the morning of a hemodialysis day and end 36 hours later, the evening of the following non-hemodialysis day. This could be started at any time during the week, as long as it was started on the morning of a day when the participant had hemodialysis. This allowed the capture of the phenomenon of fatigue as it changed over 36 hours, from one dialysis session to evening before the next hemodialysis session.
A second meeting was scheduled with each participant after the first interview, and the diaries were analyzed so participants could clarify or elaborate on their responses from either the first interview or the diary. At this second meeting, member checks were conducted (Cho & Trent, 2006; Milne & Oberle, 2005; Steinhauser & Barroso, 2009). Participants confirmed that the analyses of the first interviews and diaries were on target during the second interview. Any inconsistencies bet ween data from the diary and data from the first interview were clarified at this time. These checks helped make sure an accurate picture of participants’ fatigue as they experienced it was presented.
Data analysis
All taperecorded interviews were transcribed verbatim and proofread for accuracy. Rigor was ensured in several ways in this study (Milne & Oberle, 2005; Steinhauser & Barroso, 2009; Tuckett, 2005). Details on the data analysis have ben published previously (Horigan et al., 2013). The first author (Horigan) performed all of the data analysis, and the second author (Barroso) reviewed codes and coded approximately 80% of the transcripts, as well as reviewed themes found in the data.
Qualitative content analysis, in particular manifest and latent content analysis, was used to analyze all transcribed interviews (Graneheim & Lundman, 2004; Hseih & Shannon, 2005). Content analysis refers to the interpretation of text data and is appropriate when the aim of the research is to describe a phenomenon or experience. Data become the source of codes and categories developed. Therefore, the knowledge gained from this type of analysis is grounded in the data (Hseih & Shannon, 2005). Diaries were analyzed first as a separate source of data, and patterns within the data in the diaries were identified. Specifically, question-by-question analysis was done within each participant, comparing results across Day 1 and Day 2. Then, question-by-question analysis was done across subjects by day. This allowed for the identification of patterns within and across subjects. The diaries were then analyzed in conjunction with the initial interview and any new or clarified data from the second interview, looking for patterns across these data sources and among all sources across subjects (Ong & Jinks, 2006).
Results from the visual analogue scale were graphed to provide a visual perspective of the severity of fatigue over the 36-hour period. The following is an example of how a typical 36-hour diary was analyzed. When a 36-hour diary was received from a subject, the first author reviewed it to gain a sense of patterns that exist in fatigue occurrence, severity, and what was done to manage fatigue daily. Usually, participants rated their fatigue on a hemodialysis day prior to hemodialysis as minor to moderate in severity. After hemodialysis, fatigue was severe, with self-management consisting of sleeping or resting. The next day, participants often noted their fatigue was better and less severe, and they had to do little to manage it. Next, the first author compared diary data to that of the first interview to determine if the diary data supported data from the interview. It was expected that participants would state during their interview that their fatigue was the worst after hemodialysis requiring them to rest. If there were inconsistencies between the interview data and diary data, these were addressed in the second interview with the subject. New or clarified data were then analyzed in conjunction with the diary. The pattern of fatigue established in the data over 36 hours was then compared among participants to determine if there was an overall pattern in the diary data (Broom & Tovey, 2008; Ong & Jinks, 2006).
Results
This section will begin with a description of the two types of fatigue experienced by patients on hemodialysis. Following this, a comparison of the two fatigue experiences will be presented. Demographic characteristics of the sample are presented in Table 1. Of those who were approached to participate in this study, only two stated they did not have fatigue and were therefore not included in this work.
Table 1. Demographic Characteristics (n = 14).
| Demographic Measure | Number of Participants |
|
|---|---|---|
| Gender | Male | 7 |
| Female | 7 | |
| Race | Caucasian | 12 |
| African American | 2 | |
| Age range | Less than 50 | 2 |
| 50 to 59 | 3 | |
| 60 to 69 | 4 | |
| 70 to 79 | 3 | |
| 80 to 89 | 2 | |
| Number of years on hemodialysis |
Less than 1 year | 1 |
| 1 to 3 years | 7 | |
| 4 to 6 | 2 | |
| 7 to 9 | 2 | |
| 10 to 12 | 2 | |
| Socioeconomic status |
Receive disability | 8 |
| Average monthly income | $1442 | |
| Range of monthly income | $582 to $3772 | |
| Education | College graduates | 2 |
| High school graduates | 9 | |
| Did not complete high school | 3 | |
| Family | Children in the home | 3 |
| Patient is primary caregiver for another | 4 |
Patients with Continuous Fatigue
A larger group of patients (n = 9) described a continuous fatigue that is their usual, baseline energy/fatigue level. In general, the majority of participants in this group had been on hemodialysis more than four years and reported two or more co-morbidities when asked about their health problems. They had a dramatic increase in their fatigue level directly after hemodialysis from which they recovered slowly, over several hours, with recovery often extending into the evening or the next day. Fatigue for participants with continuous fatigue was never-ending, and just as they started to feel better, they had to go back to hemodialysis. One participant said: “I just start to get over that real tiredness, but then you turn around and start all over.”
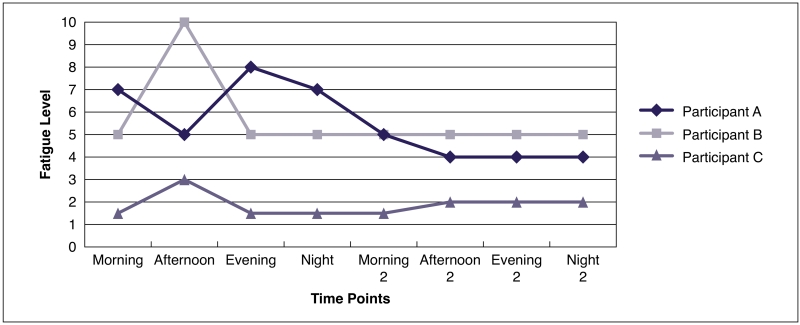
Within this group, there were two sub-groups of patients. The first subgroup of patients (n = 3) had a spike in their baseline fatigue that occurred directly after hemodialysis. In this group, the severity of fatigue was greater than 5 (0 to 10 scale) for two of the three participants and spiked to 8 to 10 during their time of the most severe fatigue. These patients required sleep and/or rest after their hemodialysis session, and after resting for several hours, they returned to their baseline level of fatigue.
One 68-year-old retired man on hemodialysis for eight years who lives at home with his wife, a cancer patient, stated: “That’s what I mean, I have to sit down for two hours, I go to sleep, then I wake up, and I’m not going to say normal, but I’m better.”
Another participant, a 74-year-old man on hemodialysis for three years, who lived independently with his wife after retiring as the manager of the department of public works, stated: “I get so tired, especially right after dialysis, I usually sleep till, if I lay down at 12:30, I sleep till about 3 o’clock.” When asked if he felt better when he woke up, he replied, “Yeah.”
Figure 2 depicts a graph of data from fatigue diaries that participants completed as part of the study. This graph demonstrates how from one hemodialysis day to the next, fatigue spikes after hemodialysis, and recovery occurs several hours after the hemodialysis session, returning participants to their baseline fatigue level. All three participants who described this pattern are depicted in this graph.
Figure 2. Continuous Fatigue with a Spike after Dialysis.
Note: This figure illustrates how participants have a continuous level of fatigue that spikes after dialysis and returns back to their baseline several hours after their dialysis session. Participant A had dialysis in the afternoon with a spike in fatigue in the evening. Participants B and C had dialysis in the morning with a spike in fatigue in the afternoon.
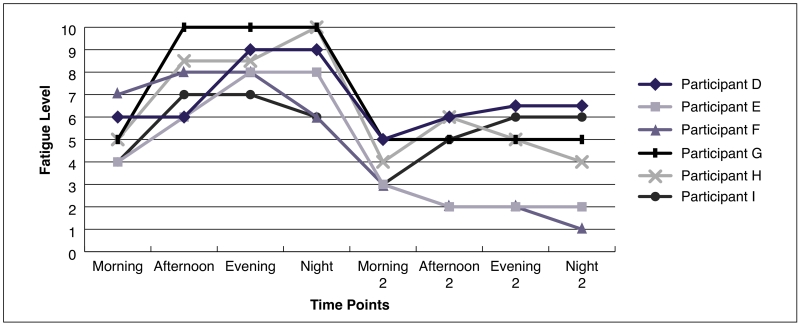
The second sub-group (n = 6) also experienced an acute, extreme fatigue after hemodialysis, but this fatigue plateaued after hemodialysis and took most, if not all, of the rest of the day to return to baseline. Half of these patients reported five to six co-morbidities, and 4 of 6 of these participants reported fatigue that plateaued anywhere from 7 to 10 in severity on a 0 to 10 scale and lasted for at least two time points at that intense level. These patients would often come home from hemodialysis, go to bed, rest or sleep for several hours, then get up for a short amount of time and return to bed in the early evening, only to return to their baseline fatigue the next morning. The following demonstrates the difference between the two groups. One participant, who was 70 years old and who used to work as a dietary assistant and cook, lived with her adult daughter and had been on hemodialysis for ten years. She stated that she naps when she comes home from hemodialysis. When asked if she felt better, she said: “For a little while…and then I have to go back; once I go to bed, have a good night’s rest, then I can get up the next day and do whatever.”
Another participant, a 56-year-old woman who previously worked as a store clerk and lived with her husband and multiple pets in a small apartment said:
Sometimes it [fatigue] continues on into the evening… I had taken my nap; I went out front to sit down [to watch a parade]… I just couldn’t even stay out there; I went to bed, and I stayed in bed till the next morning. I missed the parade and everything.
Figure 3 demonstrates how those in the second sub-group (n = 6) with continuous fatigue have a prolonged recovery, often lasting into the evening or next day. Participants with continuous fatigue attempted to manage their fatigue, but the efficacy of these management techniques was inconsistent. Participants always found it necessary to lie down and rest immediately after their hemodialysis sessions. One man said:
I don’t know, I get so tired, especially right after dialysis. Seems like as soon as they unhook, you could lay there and go to sleep, but then starting in the car, you start getting sleepy, and by the time I get home, I lay down and go to sleep.
Figure 3. Continuous Fatigue with a Plateau after Dialysis.
Note: This figure illustrates that those with continuous fatigue have a prolonged recovery that lasts until the next day. For participants D and E, dialysis was completed in the afternoon. For participants F, G, H and I, dialysis was in the morning.
Participants with continuous fatigue learned to adjust their routines and activities to accommodate their level of fatigue, often scheduling any necessary activities on non-dialysis days. One participant, a 45-year-old single parent and attorney, who had retired due to end stage renal disease (ESRD) and hemodialysis, stated: “I consider my dialysis days [to be] days where I get nothing done except for dialysis. They’re write-off days.”
Another participant, a 27-year-old woman trying to earn a college degree stated:
My school schedule, I made it for Tuesday and Thursday, and next semester, I will have a Wednesday class, but it’s in the evenings; that way, I’ll have time to get home and rest myself and then go to school.
Patients with Post-Dialysis Fatigue Only
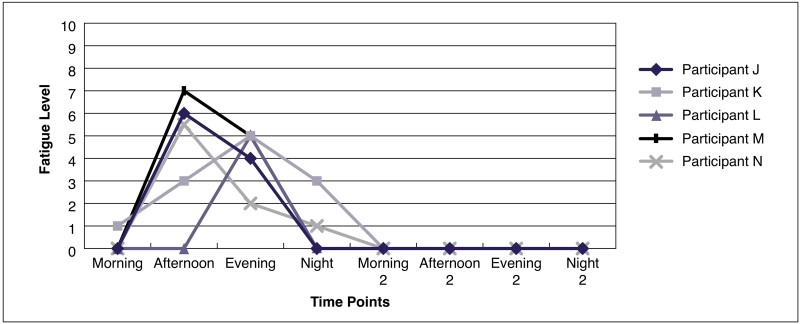
Five participants experienced post-dialysis fatigue only. Of these, none reported a fatigue severity of over 6 (0 to 10 scale) after hemodialysis. All in the post-dialysis fatigue-only group stated they came home from hemodialysis and needed to rest or sleep for several hours before they felt well enough to get up and carry on with any activity. They reported sleeping two to three hours after hemodialysis to recover from fatigue. These patients were able to push through the fatigue after hemodialysis if necessary, although this was not their preference. They found if they pushed through the fatigue, by the end of the day, they were completely worn out and usually retired early for the evening. Further, they did not feel fatigued on days that they did not have hemodialysis. In general, this group had been on hemodialysis for less than five years, and each reported only one co-morbidity when asked about other health problems.
One participant, a 59-year-old man with post-dialysis fatigue only who lived with his wife, received disability from his job as a dock worker, and continued to work part-time. He stated: “On the days I go to dialysis I’ll come home and I’ll sleep for two hours and then I get up…as long as I can lay down for a couple of hours, I don’t have no fatigue.”
Another participant, an 87-year-old retired professor who lived with his wife in an assisted living community, talked about when he got home from hemodialysis. He said: “I always sit down and usually like to have a cup of tea or something. It [the fatigue] just comes over you. I am usually doing ok by supper time.”
Another participant, a 52-year-old woman with grown children, who lived with her husband and continued to work part time in a doctor’s office, explained how she felt worn out immediately after hemodialysis. She said:
After I get off dialysis, I’m just so weak I don’t want to drive until I’m ready to…there’s been several occasions that he’s [husband] had to come and pick me up because I couldn’t drive, and later on that evening, we’d come back and get my car.
Figure 4 demonstrates how patients with post-dialysis fatigue only (n = 5) change from the day of a hemodialysis session to the next. Participants with post-dialysis fatigue only described an acute fatigue that occurred after their hemodialysis sessions only and was relieved by two to three hours of sleep or rest. While they experienced consequences of fatigue, these occurred only on hemodialysis days and were not as severe in nature as the consequences for those with continuous fatigue. They discussed that they lost time to their dialysis sessions and hemodialysis-related procedures. One 58-year-old man who received disability from his job as a dockworker but continued to work part-time at home doing clerical work said:
I find that it aggravates me to have to go to dialysis because it kills four hours of my time that I can’t do anything… I’m stuck over there with needles in my arm…you got another two hours you have to rest so there’s six hours. So there’s half a day gone.
Figure 4. Fatigue Levels over 36 Hours in Patients with Post-Dialysis Fatigue Only.
Note: This figure illustrates that patients with post-dialysis fatigue only have very low levels of fatigue that become acutely worse after dialysis and they recover from this by nighttime. Participants J and N completed dialysis in the late morning. Participants K, L, and M completed dialysis in the mid to late afternoon.
They also noted their fatigue could be insidious at times, causing them to sleep unexpectedly and wake wondering what had happened and how much time had passed. One participant, an 87-year-old retired professor who lived in an upscale assisted living facility with his wife, talked about dozing off during his hemodialysis session:
It just sort of comes over you. Sitting here, and I don’t even know when it is going to happen… I usually take something to read, but sometimes, I am sitting there, people watching, and I fall off to sleep. They come to check on something, and they wake me up… I did not even know I had fallen asleep. You just sort of feel like you lost time; you missed out.
Patients in this group did not have the same difficulty participating in activities as those with continuous fatigue experienced. Patients with post-dialysis fatigue only had trouble with activities on hemodialysis days. They scheduled work and exercise on non-hemodialysis days and that they reported doing either of these activities at all is different from those with continuous fatigue. One participant who continued to work part-time stated:
I go to work, I get up at 5:00 in the morning, I go to work, and I work from 8:00 until 5:00 or 5:30 those two days [nondialysis days]. I come home, I cook supper, I clean up the kitchen. I have no problem.
Participants with post-dialysis fatigue only also saw themselves as healthier and more fortunate than those with continuous fatigue. They observed on their own that there seemed to be people who suffered more from fatigue than they did and who were more limited in what they could do because of their fatigue. A 52-year-old woman who worked part-time added: “I’m okay, just like a normal day, I don’t have any problems. People tell me they don’t think there’s anything wrong with me,” Another participant, when talking about napping after hemodialysis, stated: “Yes, just a little nap. Some of them say they have to go to bed as soon as they get home.”
Discussion
The findings reported here are a portion of results gleaned from a larger study designed to investigate the experience and self-management of fatigue in patients on hemodialysis (Horigan et al., 2013). These results describe the temporal patterns of fatigue for patients on hemodialysis over a 36-hour period from one dialysis session to the following day. This work extends knowledge in the study of fatigue in patients on hemodialysis because it is the first to report findings of this kind. Limited information exists on how fatigue changes over time for patients on hemodialysis from one hemodialysis session to the next. It has been noted that patients on hemodialysis often experience a lasting fatigue that does not relent (Sklar et al., 1996), yet the relationship, if any, between this lasting fatigue and post-dialysis fatigue remains unknown.
Foundational work on post-dialysis fatigue was done by Sklar et al. (1996) and essentially explained the phenomenon of post-dialysis fatigue. The current study is unique because it further expands our knowledge about post-dialysis fatigue and continuous fatigue by describing the patterns that fatigue follows over time from one hemodialysis session throughout the next day. One group of patients in this study experienced post-dialysis fatigue only, an acute fatigue that occurred after their hemodialysis session and required several hours of sleep or rest to recover. After resting, they transitioned back to their normal energy level and were able to participate in daily activities. The other group of patients in this study experienced continuous fatigue, a fatigue that was always present and that worsened considerably after their hemodialysis session. All patients who experienced continuous fatigue required sleep or rest for several hours after their hemodialysis session. After resting or sleeping for several hours, some of these participants returned to their baseline level of fatigue, while others had a prolonged recovery that lasted late into the evening or into the next day.
In their work, Sklar et al. (1996) studied patients with and without post-dialysis fatigue and noted they did not address the common complaint of continuous fatigue in the study. They do not report any findings regarding continuous fatigue, which leaves questions regarding how many of their participants had underlying continuous fatigue and how this is related to post-dialysis fatigue. Findings from the current study are significant because they are the first to describe the two patterns of fatigue that patients on hemodialysis experience. While the findings do not clarify the relationship between post-dialysis fatigue and continuous fatigue, they offer a basis for future research. Further work focused on tracking patients with post-dialysis fatigue only over time would help establish whether or not this type of fatigue is stable or if it transitions to continuous fatigue.
It has been established that patients on hemodialysis experience fatigue that can be intense and impacts their quality of life. Karakan, Sezer, and Ozdemir (2011) found that 83.8% of their patients reported moderate to severe fatigue intensity, as measured with the Piper Fatigue Scale. Similarly, Bonner, Wellard, and Caltabiano (2007) found that patients on hemodialysis had high scores on the Fatigue Severity Scale, indicating a more severe level of fatigue. The current study expands these findings by measuring fatigue intensity over time and relating fatigue severity to the timing of hemodialysis sessions. Participants with post-dialysis fatigue only had less severe fatigue than those who experienced continuous fatigue. The severity of fatigue for patients with post-dialysis fatigue only did not reach higher than 6 on a 0 to 10 scale. However, those with continuous fatigue experienced fatigue severity 6 or more on a 0 to 10 scale often for extended periods of time. These findings are important to consider because future research could investigate the possible etiology of fatigue intensity and recovery time.
Past research in this area of inquiry identified post-dialysis fatigue as an often debilitating and incapacitating symptom, requiring several hours of sleep or rest to recover (Sklar et al., 1996). Similar to the findings of Sklar et al. (1996), this study found that patients on hemodialysis had a considerable increase in their fatigue after their hemodialysis sessions. However, contrary to their findings, participants in this study who experienced post-dialysis fatigue only did not require five hours of sleep to recover. Most participants in this group reported needing two to three hours of sleep after hemodialysis. Further, patients with post-dialysis fatigue only perceived that there were patients who seemed to feel worse than they did after hemodialysis. They thought of themselves and their lives as less impacted by fatigue than those they identified as feeling worse. They felt they were healthier because their fatigue did not last as long as some patients.
Similar to Rocco and colleagues (2006), the current research found that patients who experienced post-dialysis fatigue only describe functional limitations and decreased socialization on dialysis days only. They pointed out that they saved their activities for non-hemodialysis days when they feel good. This work extends these findings by comparing those with post-dialysis fatigue only to those with continuous fatigue, a condition where patients have an underlying level of fatigue at all times that is acutely exacerbated after their hemodialysis sessions, requiring varying amounts of time and sleep and rest for recovery. Those with post-dialysis fatigue only do not experience the severity of limitations in their socialization and activities that those with continuous fatigue experience. In fact, those with post-dialysis fatigue only are able to work and exercise on their non-hemodialysis days.
Limitations
There are limitations to this work. First, the study was conducted at a rural hemodialysis clinic in a Mid-Atlantic state in the South. This work may not have captured the struggles of post-dialysis fatigue for those who live in an urban setting. However, as is the case, this work provides a view of patients on hemodialysis who live in a rural area s in the U.S. that has not been presented in the literature. Another limitation is the way in which fatigue was operationally defined for inclusion in this study. By including patients who described a sensation of needing rest, it is possible that other aspects of fatigue were missed, such as cognitive fatigue. However, this did not seem to be the case because many participants reported other aspects of their fatigue (Horigan et al., 2013). The only participants who were excluded were those who reported they did not experience fatigue, and therefore, would not have provided information regarding the phenomenon. Fatigue itself may have played a role in limiting our work, though this was not found to be the case in this study. Participants were informed before the interview that if they felt too tired to continue at any time, the interview could be stopped. Further, the first author closely watched for signs of fatigue during the interview. At no time during our data collection were interviews stopped and rescheduled due to fatigue.
Implications for Research
Our research identified two groups of patients: those who experience post-dialysis fatigue only and those who have continuous fatigue. The identification of different patterns of fatigue has helped elucidate differences in the experience of fatigue, which need further research. Of particular interest is whether there are physiologic or clinical differences in patients who experience these patterns of fatigue. Additional research studies that employ a longitudinal design are warranted to help verify these patterns of fatigue and may point to additional patterns or clarify existing patterns. Further, studies of sleep and activity as they relate to fatigue patterns would be of value and provide areas of possible intervention.
Implications for Practice
Findings from this study may be helpful to nephrology nurses as they care for patients on hemodialysis. The knowledge that patients on hemodialysis do not experience fatigue in identical patterns has implications for nursing care and patient education. An in-depth nursing assessment of fatigue for patients on hemodialysis that includes severity and timing is essential to help improve patients’ quality of life. Helping patients identify a pattern in their fatigue experience may help them in scheduling activities and time with family and regulating sleep schedules. Further, continued assessment of fatigue will help identify changes in patterns and severity of fatigue for patients on hemodialysis that may require adjustment in their daily activities. Educating patients who are new to hemodialysis about fatigue will be helpful as they navigate the changes that kidney failure and dialysis schedules have on their lives. Explaining that they will likely need to rest after dialysis will help them anticipate and plan for this. Nurses are in a key position to help patients track their fatigue and suggest lifestyle changes and resources that will help patients ameliorate their fatigue as much as possible.
Conclusion
Fatigue is one of the most commonly occurring symptoms for patients on hemodialysis. Worldwide, patients report both physical and mental fatigue that impacts their daily lives and activities. However, there has been little investigation regarding the temporal pattern of fatigue for patients on hemodialysis. The research reported here, the first to illustrate temporal patterns of fatigue from one dialysis session throughout the next day, suggests there are two major patterns of fatigue: post-dialysis fatigue only and continuous fatigue. The identification of these patterns is important, particularly as a beginning point for future research to expand upon and further describe the temporal patterns of fatigue to ultimately improve the quality of life for patients on hemodialysis.
Acknowledgments
The authors would like to thank Diane Holditch-Davis, PhD, RN, FAAN; Susan Schneider, PhD, RN, AOCN, ACNS-BC, FAAN; and Sharron Docherty, PhD, MScN, CPNP-AC/PC, RN, for their contributions to this work.
Source of Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and or publication of this article: This work was supported by a grant from the American Nephrology Nurses’ Association and by grant number F31NR012342-01A1 from the National Institute of Nursing Research and the National Institutes of Health. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NINR/ NIH.
Biographies
Ann E. Horigan, PhD, RN, is an Assistant Clinical Professor, Emory University, Nell Hodgson Woodruff School of Nursing, Atlanta, GA. She may be contacted directly via ahoriga@emory.edu
Julie V. Barroso, PhD, RN, FAAN, is a Professor and Chair of the Department of Nursing in the College of Nursing, the Medical University of South Carolina, Charleston, SC.
Footnotes
Statement of Disclosure: The author reported no actual or potential conflict of interest in relation to this continuing nursing education activity.
Note: The Learning Outcome and additional statements of disclosure, and instructions for CNE evaluation can be found on page XXX.
References
- Azar AT. Effect of dialysate temperature on hemodynamic stability among hemodialysis patients. Saudi Journal of Kidney Disease and Transplant. 2009;20(4):596–603. [PubMed] [Google Scholar]
- Bonner A, Wellard S, Caltabiano M. Levels of fatigue in people with ESRD living in far North Queensland. Journal of Clinical Nursing. 2010;17(1):90–98. doi: 10.1111/j.1365-2702.2007.02042.x. [DOI] [PubMed] [Google Scholar]
- Broom A, Tovey P. Exploring the temporal dimension in cancer patients’ experiences of nonbiomedical therapeutics. Qualitative Health Research. 2008;18:1650–1661. doi: 10.1177/1049732308326511. [DOI] [PubMed] [Google Scholar]
- Cho J, Trent A. Validity in qualitative research revisited. Qualitative Research. 2006;6:319–340. [Google Scholar]
- Delgado C, Johansen KL. Barriers to exercise participation among dialysis patients. Dialysis, Nephrology and Transplantation. 2012;27(3):1152–1157. doi: 10.1093/ndt/gfr404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furness P, Garrud P. Adaptation after facial surgery: Using the diary as a research tool. Qualitative Health Research. 2010;20:262–272. doi: 10.1177/1049732309357571. [DOI] [PubMed] [Google Scholar]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nursing Education Today. 2004;24(2):105–112. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Heiwe S, Clyne N, Dahlgren MA. Living with chronic renal failure: patients’ experiences of their physical and functional capacity. Physiotherapy Research International. 2003;8(4):167–177. doi: 10.1002/pri.287. [DOI] [PubMed] [Google Scholar]
- Horigan AE, Schneider SM, Docherty S, Barroso J. The experience and self-management of fatigue in patients on hemodialysis. Nephrology Nursing Journal. 2013;40(2):113–122. PMID:23767335. [PMC free article] [PubMed] [Google Scholar]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Jablonski A. The multidimensional characteristics of symptoms reported by patients on hemodialysis. Nephrology Nursing Journal. 2007;34(1):29–37. quiz 38. [PubMed] [Google Scholar]
- Karakan S, Sezer S, Ozdemir F. Factors related to fatigue and subgroups of fatigue in patients with end-stage renal disease. Clinical Nephrology. 2011;76(5):358–364. doi: 10.5414/cn106960. [DOI] [PubMed] [Google Scholar]
- Kazemi M, Nasrabadi AN, Hasanpour M, Hassankhani H, Mills J. Experience of Iranian persons receiving hemodialysis: A descriptive, exploratory study. Nursing Health Science. 2011;13(1):88–93. doi: 10.1111/j.1442-2018.2011.00586.x. [DOI] [PubMed] [Google Scholar]
- Lee BO, Lin CC, Chaboyer W, Chiang CL, Hung CC. The fatigue experience of haemodialysis patients in Taiwan. Journal of Clinical Nursing. 2007;16(2):407–413. doi: 10.1111/j.1365-2702.2005.01409.x. [DOI] [PubMed] [Google Scholar]
- Leinau L, Murphy TE, Bradley E, Fried T. Relationship between conditions addressed by hemodialysis guidelines and non-ESRD-specific conditions affecting quality of life. Clinical Journal of the American Society of Nephrology. 2009;4:572–578. doi: 10.2215/CJN.03370708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu HE. Fatigue and associated factors in hemodialysis patients in Taiwan. Research in Nursing and Health. 2006;29:40–50. doi: 10.1002/nur.20109. [DOI] [PubMed] [Google Scholar]
- Lockhart TE, Barth AT, Zhang X, Songra R, Abdel-Rahman E, Lach J. Portable non-invasive fall risk assessment in end-stage renal disease patients on hemodialysis. ACM Transactions on Computer-Human Interaction. 2010:84–93. doi: 10.1145/1921081.1921092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milne J, Oberle K. Enhancing rigor in qualitative description. Journal of Wound, Ostomy and Continence Nursing. 2005;32(6):413–420. doi: 10.1097/00152192-200511000-00014. [DOI] [PubMed] [Google Scholar]
- Morsch CM, Goncalves LF, Barros E. Health-related quality of life among haemodialysis patients-relationship with clinical indicators, morbidity and mortality. Journal of Clinical Nursing. 2006;15:498–504. doi: 10.1111/j.1365-2702.2006.01349.x. [DOI] [PubMed] [Google Scholar]
- Neergaard M, Olesen F, Andersen R, Sondergaard J. Qualitative description – The poor cousin of health research? BMC Medical Research Methodology. 2009;9(52) doi: 10.1186/1471-2288-9-52. retrieved from http://www.biomedcentral.com/1471-2288/9/52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong B, Jinks C. “Walking like John Wayne”: Open format diaries of people with knee pain and disability. Chronic Illness. 2006;2(1):21–26. doi: 10.1177/17423953060020010901. [DOI] [PubMed] [Google Scholar]
- Richards L. Read me first: A user’s guide to qualitative methods. Sage; Thousand Oaks, CA: 2006. [Google Scholar]
- Rocco DG, Mercieri A, Yavuzer G. Multidimensional health-status assessment of chronic hemodialysis patients: The impact on quality of life. Europa Medicophysica. 2006;42(2):113–119. [PubMed] [Google Scholar]
- Sandelowski M. Whatever happened to qualitative description? Research in Nursing and Health. 2000;23(4):334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Singh NP, Bansal R, Thakur A, Kohli R, Bansal RC, Agarwal SK. Effect of membrane composition on cytokine production and clinical symptoms during hemodialysis: A crossover study. Renal Failure. 2003;25(3):419–430. doi: 10.1081/jdi-120021154. [DOI] [PubMed] [Google Scholar]
- Sklar A, Newman N, Scott R, Semenyuk L, Schultz J, Fiacco V. Identification of factors responsible for postdialysis fatigue. American Journal of Kidney Diseases. 1999;34(3):464–470. doi: 10.1016/s0272-6386(99)70073-9. [DOI] [PubMed] [Google Scholar]
- Sklar A, Riesenberg L, Silber A, Ahmed W, Ali A. Postdialysis fatigue. American Journal of Kidney Diseases. 1996;28(5):732–736. doi: 10.1016/s0272-6386(96)90256-5. [DOI] [PubMed] [Google Scholar]
- Steinhauser K, Barroso J. Using qualitative methods to explore key questions in palliative care. Journal of Palliative Medicine. 2009;12(8):725–730. doi: 10.1089/jpm.2009.9580. [DOI] [PubMed] [Google Scholar]
- Tuckett A. Rigour in qualitative research: Complexities and solutions. Nurse Researcher. 2005;13(1):29–42. doi: 10.7748/nr2005.07.13.1.29.c5998. [DOI] [PubMed] [Google Scholar]
- Weisbord SD, Fried LF, Arnold RM, Fine MJ, Levenson DJ, Peterson RA, Switzer GE. Prevalence, severity, and importance of physical and emotional symptoms in chronic hemodialysis patients. Journal of the American Society of Nephrology. 2005;16(8):2487–2494. doi: 10.1681/ASN.2005020157. [DOI] [PubMed] [Google Scholar]
- Yngman-Uhlin P, Edell-Gustafsson U. Self-reported subjective sleep quality and fatigue in patients with peritoneal dialysis treatment at home. International Journal of Nursing Practice. 2006;12(3):143–152. doi: 10.1111/j.1440-172X.2006.00566.x. [DOI] [PubMed] [Google Scholar]
Additional Reading
- Taylor SE, Buunk BP, Aspinwall L. Social comparison, stress and coping. Personality and Social Psychology Bulletin. 1990;16:74–89. [Google Scholar]