Abstract
Purpose
To determine whether a novel exoskeletal device (Pediatric Wilmington Robotic Exoskeleton, P-WREX) is feasible and effective for intervention to improve reaching and object interaction for an infant with arm movement impairments.
Methods
An 8-month old with arthrogryposis was followed every two weeks during a 1-month baseline, 3-month intervention, and 1-month post-intervention. At each visit, reaching and looking behaviors were assessed.
Results
Within sessions, the infant spent more time contacting objects across a larger space, contacting objects with both hands, and looking at objects when wearing the P-WREX. Throughout intervention, the infant increased time contacting objects both with and without the device and increased bilateral active shoulder flexion.
Conclusions
1) It may be feasible for families to use exoskeletons for daily intervention, 2) Exoskeletons facilitate immediate improvements in function for infants with impaired upper extremity mobility, and 3) Interventions using exoskeletons can improve independent upper extremity function across time.
Keywords: exoskeleton, assistive device, rehabilitative device, upper extremity, movement impairment, arthrogryposis
Introduction and Purpose
The ability to reach for and interact with objects is a skill that allows infants to explore, gather information, and learn about their environment.1, 2 Reaching emerges as poorly controlled swiping movements from 1 to 3 months of age, followed by more controlled, visually-guided reaching and grasping of objects from 4 to 5 months of age.3, 4 The ability to reach for objects has been shown to play a key role in advancing object exploration behaviors and learning in infancy.5, 6
Arthrogryposis is a non-progressive neuromuscular disorder emerging from limited mobility from 6 to 8 weeks gestational age. Infants are born with significant muscle contractures, fibrosis, and weakness limiting movement across multiple affected joints.7 They may have difficulty lifting their arms against gravity, which can impair reaching and object exploration. Rehabilitation devices have not been available to enhance movement, exploration, and learning for such young populations. Recently, a novel exoskeleton, the Wilmington Robotic Exoskeleton (WREX) became available to adolescents and adults with significant upper extremity weakness.8, 9, 10
The WREX used here is the Pediatric (P)-WREX. It consists of 3D-printed plastic supportive parts with elastic bands to provide torque about the shoulder and elbow joints to support flexion against gravity. The WREX is a passive exoskeleton that supports the arm in a new resting position based on the properties of the elastic bands. It does not allow for programming or feedback. It attaches to a custom trunk brace for use outside of a seating device. The WREX has been shown to improve upper extremity function within one session for older children with arthrogryposis, muscular dystrophy, or spinal muscular atrophy (SMA).8, 9, 10 For children with arthrogryposis between 6 and 14 years of age, it has been shown to improve fine motor performance, feeding, participation in school and hobbies, self-esteem, motivation, and social interaction.8, 9
This study is the first to evaluate the feasibility and effectiveness of the WREX device for an infant. The purpose of this study was to determine whether a pediatric version of the WREX (P-WREX; Figure 1) was feasible for use in daily intervention, and whether its use could improve reaching and object interaction behaviors for an infant with arthrogryposis. Our goal was to follow the participant longitudinally to characterize his behavioral changes across time. Based on previous studies, we hypothesized our participant would show improved reaching and object interaction abilities when wearing the P-WREX.8, 9, 10 Because arthrogryposis is not progressive and literature suggests postnatal muscle growth is possible in this population, we also hypothesized that intervention using the P-WREX would improve reaching and object interaction abilities for the infant across time even when he was not wearing the device.11, 12
Figure 1.

The infant with the P-WREX. Rubber bands attach to the device on the lateral side of the arms, stretching across the shoulder and elbow joints in a manner that provides torque aiming to assist with flexion at those joints.
Methods
Subject
An infant with amyoplasia, the most common type of arthrogryposis, and his family participated in this study. Parents provided informed consent. The infant was assessed every two weeks from 8 through 13 months of age. The infant had a history of muscle fibrosis, decreased muscle mass, and multiple joint contractures in more than one area of the body with the limbs affected in a symmetrical manner, patent ductus arteriosus, patent foramen ovale, bilateral Achilles tendon lengthening (age 4 months), and ear tube placement (age 12 months). The infant received physical therapy and occupational therapy each 1 hour per week since 3 months of age. These services continued throughout the study. At the initiation of the study, the infant had full functional passive range of motion at both shoulders and elbows. He sat independently without arm support and used a bilateral palmar grasp. No standardized assessment of cognition was performed for this study, but the child qualified for special education services based on his early intervention assessments.
Study Schedule
The participant’s object interaction abilities with and without the P-WREX were assessed using a single-subject ABA design once every two weeks throughout a: 1) 1-month baseline (P-WREX only used during assessments); 2) 3-month intervention; and 3) 1-month post-intervention phase.
Intervention
Parents were educated via a manual, discussion, and demonstration to perform intervention activities with the infant wearing the P-WREX 60 minutes daily. In addition, the P-WREX could be used as desired during unstructured free play, or typical daily activities. Parents were instructed to supervise the infant whenever the P-WREX was worn. Parents reported daily durations for intervention and free play wear.
Intervention consisted of activities in sitting to promote general arm movement, reaching, object exploration, and elbow flexion (please see Appendix or contact the corresponding author for details regarding intervention activities). The overall goal was for parents to provide opportunities for the infant to move and explore objects in a larger play space than was available to him without the P-WREX. To progressively challenge the infant, the level of assistance provided by the P-WREX was decreased every two weeks, while the intervention tasks and object placement remained stable. The assistance level was decreased by replacing the elastic bands across the shoulder with bands of lower stiffness so the resting shoulder flexion position changed from 90 degrees to 80 degrees and so forth across time.
Post-Intervention Phase
The family was instructed to discontinue the structured intervention but to continue use of the P-WREX for unstructured free play as desired. This phase provided us with information about intervention retention effects as well as how often the family might typically use the device outside of intervention. Parents reported duration of free play wear.
Procedures
Visits were performed at Nemours/A. I. duPont Hospital for Children, the University of Delaware, or the home depending on the family’s preference. Assessments were video recorded using two camcorders providing frontal and side views of the infant. Videos were synchronized and coded by two coders using OpenSHAPA software. Twenty percent of the files were re-coded for intra- and inter-rater agreement (both > 90% for all measures based on the equation [Agreed/(Agreed+Disagreed)] * 100). Blind coding of P-WREX ON and OFF conditions was not possible. Random inter-rater reliability coding aimed to minimize bias related to knowledge of device condition.
The Alberta Infant Motor Scale (AIMS), a reliable and validated norm-referenced comprehensive motor assessment tool, was administered at each visit to assesses posture, weight bearing, and movement in prone, supine, sitting, and standing.13, 14
Strength was assessed monthly by measuring the maximum active shoulder flexion range of motion bilaterally in side lying (gravity-eliminated), supine, and sitting, a common method for infants not yet able to follow instructions required for manual or mechanized muscle testing procedures.
To assess feasibility of the device, a perception questionnaire regarding ease of use, comfort, and appearance was provided to the parents.
At each visit, the infant was provided the Reaching Location Assessment and the Midline Reaching Assessment – both seated with and without the P-WREX. Condition order was alternated at each visit to avoid familiarity or fatigue effects. Trials began when the infant was in a positive behavioral state and looking at the assessment object.
The Reaching Location Assessment measured ability to contact an object presented across the reaching space. The infant was provided 30-second opportunities to interact with an object (2 × 2" block at all assessments) at eye, chest, and hip height. At each height, the object was presented at midline, right, and left, but for the current analyses, midline, right, and left data were combined within each height because no systematic differences were observed across these positions. We coded Toy Contacts based on the start and end video frames for periods when any part of either hand was in contact with the toy. Data were converted to percentages of time by dividing by total assessment time.
The Midline Reaching Assessment measured ability to contact an object (2 × 12" rod at all assessments) presented in midline at chest height for 3 consecutive minutes. We coded: 1) Right/Left Hand Toy Contact – when the left or right hand was in contact with the toy; 2) Mouth Reaching – when the infant opened his mouth and moved it toward the toy while looking at the toy, and 3) Visual Attention to the Toy – when the infant’s eyes were directed at the toy for more than 1 second. Data were converted to percentages of time, dividing by assessment time, and times of behavioral overlap were identified. This produced: Unimanual Toy Contact – when only either the left or right hand was in contact with the toy, Bimanual Toy Contact – when left and right hand toy contact periods overlapped, and Toy Contact While Looking – multimodal exploration when toy contact and visual attention periods overlapped. The types of behavioral analyses used in this study are well-established methods widely used in developmental research.15, 16, 17, 18
Data Analysis
To test for changes within sessions with and without the P-WREX, Wilcoxon signed-rank tests were used to analyze aggregated differences from all study visits because data were not normally distributed in some conditions due to the large number of zero values. Statistically significant differences between conditions occurred when p was ≤ .05 and trends occurred when p was ≤ .10.
To test for changes across time with or without the P-WREX, the 2-SD band method was applied.19, 20 Statistically significant change during the intervention phase occurred when at least 2 consecutive data points during intervention fell outside the mean ± 2SD band calculated from baseline.21
For all analyses, PASW (Predictive Analytics Software) Statistics version 18.0.3 (IBM Corporation, Somers, NY) was used.
Results
Developmental and Strength Assessments
The infant consistently scored below the fifth percentile on the AIMS, suggesting considerably delayed motor development.13 The infant’s active shoulder flexion range of motion (Table 1) did not change during baseline, but improved both against gravity (sitting and supine) and with gravity eliminated (side lying) throughout the intervention and post-intervention phases, more for the right arm than left.
Table 1.
Values for Active Flexion Range of Motion.
| Time of Testing | Sitting | Supine | Side lying | |||
|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Right | Left | |
| First Baseline Visit | 15° | 0° | 30° | 30° | 90° | 30° |
| Last Baseline Visit | 15° | 0° | 30° | 30° | 90° | 30° |
| One Month Into Intervention | 30° | 30° | 100° | 30° | 100° | 45° |
| Two Months Into Intervention | 45° | 30° | 145° | 30° | 145° | 80° |
| End of Intervention | 60° | 30° | 145° | 30° | * | * |
| End of Post-Intervention | 80° | 30° | 145° | 45° | * | * |
Testing was attempted but not completed in side lying at the end of the study because the infant had improved mobility and did not allow experimenters to maintain him in that position. Note that observed active range of motion improved in all three positions throughout the intervention and post-intervention phases. Improvements in strength were greater for the right arm than for the left.
Feasibility
During the intervention phase, intervention occurred 37.3 ± 11.9 minutes/day (general arm movement 2.5 ± 5.9, reaching 18.3 ± 4.7, object exploration 8.1 ± 4.0, elbow flexion 8.5 ± 3.6 minutes) and unstructured free play wear occurred 44.6 ± 32.8 minutes/day. During the post-intervention phase, free play wear occurred 61.4 ± 15.2 minutes/day.
Parents rated ease of donning as a 3 (1 = very difficult, through 5 = very easy) and ease of doffing as a 4. They rated the infant’s comfort as a 3 (1 = very uncomfortable, through 5 = very comfortable) after 1 hour of wear. They rated ease of use outside of the home as a 2 (1 = very difficult, through 5 = very easy), reporting it did not fit in the car seat or stroller, was “cumbersome” to carry alone, and was “difficult to carry (the infant) with it on.” They rated restrictiveness on daily activities as a 3 (1 = extremely restricted, through 5 = no restrictions), reporting it did not assist elbow flexion well and limited floor play. They rated restrictions on mobility as a 1 (1 = extremely restricted, through 5 = no restrictions) because it restricted floor mobility (transitions and rolling). They rated appearance as a 2 (1 = very unattractive, through 5 = very attractive), noting the unattractive elastic bands and device bulk.
Reaching Location Assessment
Within sessions, the P-WREX was most effective at improving reaching ability when the infant reached for objects at hip and chest level (Figure 2A). The infant contacted objects at hip level more with the P-WREX (Mdn = 34.78% of time) than without (Mdn = 17.86%), z = −1.960, p = .050, medium effect size r = −0.46. He contacted objects at chest level more with the P-WREX (Mdn = 35.42%) than without (Mdn = 0%), z = −2.521, p = .012, large effect size r = −0.59. The infant never contacted objects at eye level without the P-WREX (Mdn = 0%), and rarely contacted objects at eye level with it (Mdn = 0%), z = −1.604, p = .109, medium effect size r = −0.38. The infant had increased contact with objects at hip and chest levels when wearing the P-WREX at most visits during the baseline, intervention, and post-intervention phases (Figures 2B and 2C). He contacted objects at eye level at only a few visits during the baseline and intervention phases while wearing the P-WREX (Figure 2D).
Figure 2.




From the Reaching Location Assessment, differences in ability to interact with objects averaged across all visits for each reaching space (A; error bars represent standard error; * represents a significant difference, † represents a trend for significant difference) and at each visit within each reaching space – hip level (B), chest level (C), and eye level (D) – with and without the P-WREX (P-WREX ON and P-WREX OFF). Within sessions, the P-WREX improved the infant’s ability to contact objects across the play space, with the greatest improvements observed when reaching for objects at chest and hip level. Across time, reaching behavior generally increased during the intervention phase, but decreased during the post-intervention phase. This suggests that targeted interventions may be necessary in coordination with device use to advance behavioral performance across time.
Across time with the P-WREX on, the infant spent significantly more time contacting objects at hip (2SD band 0 to 56.8%) and chest (2SD band 0 to 29.9%) level during intervention than during baseline; whereas contact at eye level did not significantly change (2SD band 0 to 12.85%). Across time when not wearing the P-WREX, the infant spent significantly more time contacting objects at hip level (2SD band 0 to 25.5%), whereas change in contacts at chest (2SD band at 0%) and hip level (2SD band at 0%) was not significant.
Midline Reaching Assessment
Within sessions, the infant showed improved unimanual and bimanual contact with objects presented in midline at chest level when wearing the P-WREX (Figure 3A). The infant spent more time contacting objects unimanually with the P-WREX (Mdn = 25.49% of time) than without (Mdn = 1.67%), z = −2.547, p = .011, large effect size r = −0.58 (Figures 3A and 3B).
Figure 3.





From the Midline Reaching Assessment, differences in ability to contact objects unimanually and bimanually and to reach for objects with the mouth averaged across all visits (A; error bars represent standard error; * represents a significant difference) and at each individual visit (B–D) with and without the P-WREX. Note that unimanual and bimanual reaching increased while reaching for objects with the mouth decreased both within sessions when the P-WREX was donned and across time when the P-WREX was not donned. Across time, unimanual reaching with the P-WREX on generally increased during the intervention phase, but decreased during the post-intervention phase, again suggesting that targeted interventions in coordination with device wear may best facilitate improvements in some behaviors across time. Across time without the P-WREX, trajectories for contacting objects with the hand and attempting to reach for objects with the mouth (E) show that a decrease in the amount of mouth reaching coincided with the emergence and increase in object contacts with the hand.
Across time, there was a significant increase in unimanual contacts between the baseline and the intervention phases without the P-WREX (2SD band at 0%), but not with the P-WREX (2SD band 0 to 92.83%). Around 6 weeks into the intervention, the infant showed independent reaching for the first time and his percent time contacting objects unimanually while not wearing the P-WREX steadily increased from this point through the end of the study (Figure 3B). In contrast, while wearing the device, his unimanual contacts increased during intervention but decreased during the post-intervention phase.
Within sessions, the infant showed bimanual object contacts only when wearing the P-WREX (Figures 3A and 3C). While never observed without the P-WREX (Mdn = 0%), this challenging behavior was observed infrequently, but significantly more, while using the P-WREX (Mdn = 1.95%), z = −2.366, p = .018, large effect size r = −0.53.
Across time, the ability to contact objects bimanually emerged mid-way through the intervention phase and persisted thereafter. There were no significant differences in bimanual contacts between the baseline and the intervention phase with (2SD band 0 to 10.34%) or without (2SD band at 0%) the P-WREX.
Within sessions, the infant spent less time reaching for objects with his mouth with the P-WREX (Mdn = 0%) than without (Mdn = 2.15%), z = −2.100, p = .036, medium effect size r = −0.47 (Figures 3A and 3D).
Across time, mouth reaching without the P-WREX significantly decreased throughout the study (2SD band 4.82 to 32.35%) completely disappearing in the middle of intervention. Interestingly, this decrease in mouth reaching without the P-WREX coincided with the emergence and steady increase in hand reaching ability also observed without the device (Figure 3E). Thus, as the infant’s manual abilities improved across time, he decreased his attempts to reach for and explore objects using his mouth, a less adaptive strategy.
Within sessions, the infant showed improved visual attention for objects when wearing the P-WREX. The infant’s visual attention to presented objects was higher with the P-WREX (Mdn = 48.86%) than without (Mdn = 23.51%), z = −2.191, p = .028, medium effect size r = −0.49 (Figure 5A). Across time, there were no significant differences in visual attention from baseline through intervention with (2SD band 0 to 97.83%) or without (2SD band 0 to 79.94%) the P-WREX.
Within sessions, percent time looking at objects while contacting them, or multimodal exploration, was significantly greater with the P-WREX (Mdn =24.58%) than without (Mdn = 6.09%), z = −2.803, p = .005, large effect size r = −0.63 (Figures 4A and 4C). Across time, multimodal exploration did not significantly change with (2SD band 0 to 62.98%) or without (2SD band 0 to 32.87%) the P-WREX. Interestingly, both visual attention to objects and multimodal exploration seemed to increase during the intervention then decrease during the post-intervention phase of the study with the P-WREX on (Figures 4B and 4C).
Figure 4.



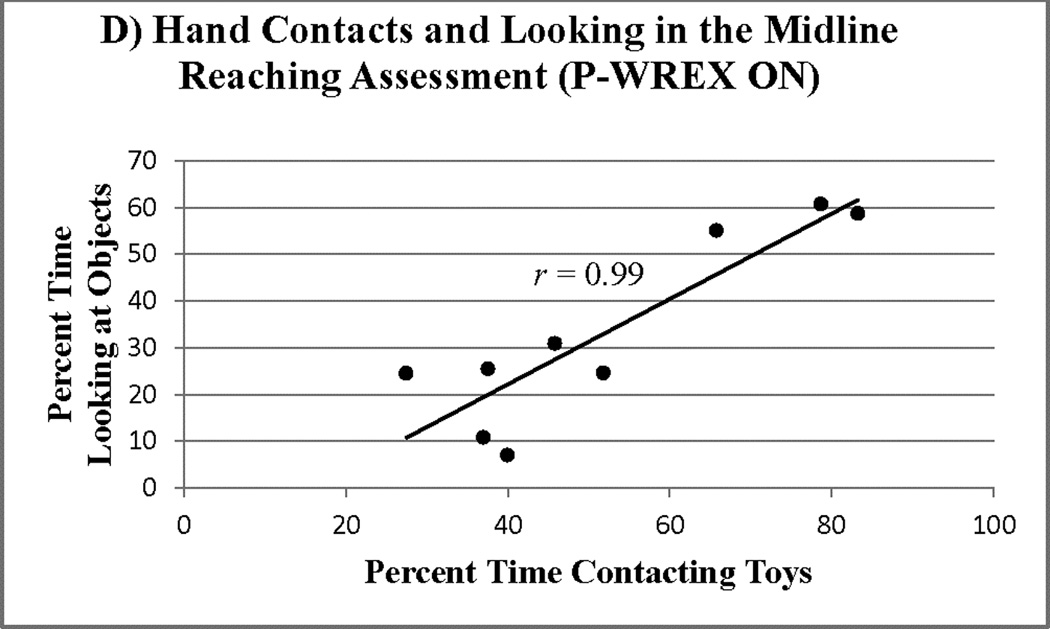

Differences in looking behavior and multimodal exploration (looking while contacting objects) within visits (A; error bars represent standard error; * represents a significant difference) and across time (B, C) with and without the P-WREX during the Midline Reaching Assessment. Within sessions, the infant directed more visual attention to objects while wearing the P-WREX despite the fact that the objects were presented at a location that was always easy to view, midline at chest height. Also, the infant was better able to contact objects while looking at them when wearing the P-WREX. Across time with the P-WREX on, both looking and contacts with looking increased throughout the intervention phase, but decreased during the post-intervention phase, again highlighting that use of the device in isolation without targeted intervention activities may not be enough to facilitate performance of a variety of key behaviors across time. Reaching behavior was positively correlated with visual attention while wearing the P-WREX (D); this relation, however, was not significant without the device (E). Thus, the P-WREX might facilitate hand-eye coordination that enables effective multimodal object exploration.
Moreover, Figures 4D and 4E suggest that time looking at objects was associated with time reaching for and contacting objects with either hand. This association was much stronger with the P-WREX than without (Pearson correlation, 2-tailed: r(7) = .99, p < .0001 with the P-WREX; r(8) = .004, p = .992 without the P-WREX). Thus, the P-WREX may have facilitated not only object contacts but also interest in objects.
Discussion
Exoskeletons May Be Feasible for Daily Intervention in the Natural Environment
This study suggests that exoskeletons like the P-WREX may be feasible for use in daily, home-based intervention with infants. Throughout the study, the P-WREX device was used daily for up to 1 hour. The device was reasonably comfortable and did not present significant difficulties for donning and doffing. However, parents reported concerns that it restricted floor mobility, poorly assisted elbow flexion, was unattractive, and bulky (difficult to carry and incompatible with devices like car seats and strollers).
Other key challenges relate to accessibility and affordability. Versions of the device can be purchased through JAECO Orthopedic, AI DuPont Hospital for Children, or Magic Arms for about $10,000 per pair. There is typically an extended waiting period to receive the device and young children require replacements regularly due to growth. There is a need to continue to improve existing exoskeletons and to develop more affordable, accessible exoskeletal devices that address the limitations identified in this study (recently developed alternatives are: Angel Arms open source 3D-printed exoskeleton, http://3dprint.com/tag/angel-arms/; Playskin Lift™ open source exoskeletal garment, http://www.ncbi.nlm.nih.gov/pubmed/26316534).
Exoskeletons May Be Effective Assistive Devices
The findings suggest that exoskeletons may serve as effective assistive devices to improve function when worn. Within a session, the P-WREX significantly improved reaching ability at hip and chest level, increased unimanual and bimanual object contact, decreased less adaptive mouth reaching, increased attention to objects, and increased multimodal exploration. Reaching and visual attention were significantly correlated only while wearing the P-WREX, further suggesting the P-WREX facilitated both object interaction and attention.
Tools like the P-WREX are important to assist movement and play in early development. The way children interact with and gather information about objects impacts their perceptual-motor, language, social, and cognitive development.22, 23, 24, 25 Children typically learn about objects by interacting with them a large amount of the time via a variety of behavioral combinations.17 The amount and variability of behavioral performance, and consequent information uptake and learning, is often diminished for children with disabilities.18, 26, 27, 28 Devices like the P-WREX may allow young children to explore, gather information, play, and learn when it is critical in early development despite their existing movement limitations.
Exoskeletons May Be Effective Rehabilitative Devices
The findings also suggest that exoskeletons like the P-WREX may serve as effective rehabilitative devices to improve function even when they are not donned. Across time, the infant’s active range of shoulder flexion improved during the intervention and post-intervention phases, but not during baseline, suggesting intervention with P-WREX increased muscle strength. While wearing the device, the infant spent more time contacting objects at hip and chest height during the intervention phase compared to baseline.
Without the device donned, the infant showed improved object interaction during the intervention phase, spending more time contacting objects at hip and chest height and less time mouth reaching compared to baseline. At the first visit, the infant was unable to contact objects at chest height despite the fact that he was 8 months old and reaching typically emerges by 5 months. This ability emerged for the infant without the device about 6 weeks into the intervention, a period long enough to allow for changes in muscle strength, and improved throughout the remainder of the study.
This steady increase in hand reaching ability without the P-WREX donned was temporally associated with a significant decrease in mouth reaching, which was no longer observed after the middle of the intervention. Individuals who cannot yet control their arm movement for reaching often employ mouth or feet reaching strategies. These strategies provide limited object exploration and manipulation possibilities and typically dissipate as manual abilities improve.
The limited number of baseline visits in this study likely reduced power to detect other effects. For future studies, more data points in baseline are recommended. Because the device cost was high and this was the first time a device like this has been used for an infant, only one participant was studied. Future studies would benefit from a larger participant pool. Also, because these devices are novel, we did not have subject-specific criteria for adjusting the level of assistance. Future research should evaluate criteria for determining optimal levels of assistance to promote skill development. Furthermore, the nature of this study did not allow us to separate the effects of the device and intervention from one another or potential maturational effects, especially considering that the course of early development has not been well documented for children with arthrogryposis. Studies with larger subject pools from a variety of populations must be conducted to verify these findings and rule out other potential causes of change, such as maturation, experience, and ongoing interventions.
Exoskeletons May Be Most Effective as Part of a Targeted Intervention Program
An important finding was that when wearing the device, the infant showed improved unimanual reaching ability, visual attention, and multimodal exploration across time only during periods when device wear was paired with targeted daily intervention. Performance of these behaviors while wearing the P-WREX increased during the intervention phase, but then decreased during the post-intervention phase when the family continued using the P-WREX about 1 hour/day for free play but ceased performing the targeted intervention activities. These results suggest that devices like the P-WREX may be most effective at maximizing function across time when combined with targeted interventions. Isolated use of such devices may not facilitate improvements in behavioral performance longitudinally.
Conclusions
Exoskeletons may serve as feasible and effective assistive devices for immediate improvements in infants’ reaching and visual attention abilities when they are worn. They may also have potential as rehabilitative devices to improve object interaction abilities across time, even when they are not donned. It is likely that exoskeletons need to be paired with targeted intervention activities for optimal rehabilitative benefits to be observed across time. Early intervention could be greatly enhanced by these innovative tools that allow children to learn to move, explore, and play in spaces otherwise unavailable to them. Future research incorporating measures of cognition and larger samples of children representing a wider spectrum of diagnoses is needed to further explore the effectiveness of novel exoskeletons like the P-WREX.
Supplementary Material
Acknowledgments
We would like to acknowledge the infant and his parents for their participation, time, and patience in making the current longitudinal study possible. Also, we would like to thank the research assistants who helped with the coding of data.
Grant support: This research was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (1R21HD076092-01A1; Lobo, PI).
Footnotes
Conflict of Interest statement: The authors declare no conflict of interest.
References
- 1.Gibson EJ, Spelke ES. The development of perception. In: Mussen PH, editor. Handbook of Child Psychology: Cognitive Development. Vol. 3. New York: Willey; 1983. pp. 1–76. [Google Scholar]
- 2.Gibson EJ. Exploratory behavior in the development of perceiving, acting, and the acquiring of knowledge. Annu Rev Psychol. 1988;39:1–41. [Google Scholar]
- 3.Lockman JJ, Ashmead DH, Bushnell EW. The development of anticipatory hand orientation during infancy. J Exp Child Psychol. 1984;37:176–186. doi: 10.1016/0022-0965(84)90065-1. [DOI] [PubMed] [Google Scholar]
- 4.Thelen E, Corbetta D, Kamm K, et al. The transition to reaching: Mapping intention and intrinsic dynamics. Child Dev. 1993;64:1058–1098. [PubMed] [Google Scholar]
- 5.Needham A, Barrett T, Peterman K. A pick-me-up for infants’ exploratory skills: Early simulated experiences reaching for objects using ‘sticky mittens’ enhances young infants’ object exploration skills. Infant Behav Dev. 2002;25:279–295. [Google Scholar]
- 6.Libertus K, Needham A. Teach to reach: The effects of active vs. passive reaching experiences on action and perception. Vision Res. 2010;50:2750–2757. doi: 10.1016/j.visres.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Staheli LT, Hall JG, Jaffe KM, et al. Arthrogryposis: A Text Atlas. New York, NY: Cambridge University Press; 1998. [Google Scholar]
- 8.Rahman T, Sample W, Jayakumar S, et al. Passive exoskeletons for assisting limb movement. J Rehabil Res Dev. 2006;43:583–589. doi: 10.1682/jrrd.2005.04.0070. [DOI] [PubMed] [Google Scholar]
- 9.Rahman T, Sample W, Seliktar R, et al. Design and testing of a functional arm orthosis in patients with neuromuscular diseases. IEEE T Neur Sys Reh. 2007;15(2):244–251. doi: 10.1109/TNSRE.2007.897026. [DOI] [PubMed] [Google Scholar]
- 10.Haumont T, Rahman T, Sample W, et al. Wilmington robotic exoskeleton: A novel device to maintain arm improvement in muscular disease. J Pediatr Orthoped. 2011;31(5):e44–e49. doi: 10.1097/BPO.0b013e31821f50b5. [DOI] [PubMed] [Google Scholar]
- 11.Bamshad M, Van Heest AE, Pleasure D. Arthrogryposis: A review and update. J Bone Joint Surg Am. 2009;91(4):40–46. doi: 10.2106/JBJS.I.00281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mercuri E, Manzur A, Main M, et al. Is there post-natal muscle growth in amyoplasia? A sequential MRI study. Neuromuscular Disord. 2009;19:444–445. doi: 10.1016/j.nmd.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 13.Piper MC, Darrah J. Motor Assessment of the Developing Infant. Saunders Company, PA: 1994. [Google Scholar]
- 14.Almeida KM, Dutra MVP, de Mello RR, et al. Concurrent validity and reliability of the Alberta Infant Motor Scale in premature infants. J Pediat. 2008;84:442–448. doi: 10.2223/JPED.1836. [DOI] [PubMed] [Google Scholar]
- 15.Needham A, Barrett T, Peterman K. A pick-me up for infants’ exploratory skills: Early simulated experiences reaching for objects using “sticky mittens” enhances young infants’ object exploration skills. Infant Behav Dev. 2002;25:279–295. [Google Scholar]
- 16.Corbetta D, Snapp-Childs W. Seeing and touching: The role of sensory-motor experience on the development of infants reaching. Infant Behav Dev. 2009;32:44–58. doi: 10.1016/j.infbeh.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Lobo MA, Kokkoni E, et al. Not just playing around: Infants’ behaviors with objects reflect ability, constraints, and object properties. Infant Behav Dev. 2014;37:334–351. doi: 10.1016/j.infbeh.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lobo MA, Kokkoni E, et al. Infants born preterm demonstrate impaired exploration behaviors throughout infancy and toddlerhood. Phys Ther. 2015;95:51–64. doi: 10.2522/ptj.20130584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bloom M, Fisher J. Evaluating Practice: Guidelines for the Accountable Professional. Englewood Cliffs, NJ: Prentice Hall; 1982. [Google Scholar]
- 20.Nourbakhsh MR, Ottenbacher KJ. The statistical analysis of single-subject data: a comprehensive examination. Phys Ther. 1994;74:768–776. doi: 10.1093/ptj/74.8.768. [DOI] [PubMed] [Google Scholar]
- 21.Gottman JM, Leiblum SR. How to Do Psychotherapy and How to Evaluate It. New York, NY: Holt, Rinehart and Winston; 1974. [Google Scholar]
- 22.Thelen E. Grounded in the world: Developmental origins of the embodied mind. Infancy. 2000;1:3–28. doi: 10.1207/S15327078IN0101_02. [DOI] [PubMed] [Google Scholar]
- 23.Iverson JM, Fagan MK. Infant vocal-motor coordination: Precursor to the gesture-speech system? Child Dev. 2004;75:1053–1066. doi: 10.1111/j.1467-8624.2004.00725.x. [DOI] [PubMed] [Google Scholar]
- 24.Smith LB. Cognition as a dynamic system: Principles from embodiment. Dev Rev. 2005;25:278–298. [Google Scholar]
- 25.Lobo MA, Harbourne RT, Dusing SC, McCoy SW. Grounding early intervention: Physical therapy cannot just be about motor skills anymore. Phys Ther. 2013;93(1):94–103. doi: 10.2522/ptj.20120158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ruff HA, McCarton C, Kurtzberg D, Vaughan HG., Jr Preterm infants’ manipulative exploration of objects. Child Dev. 1984;55:1166–1173. [PubMed] [Google Scholar]
- 27.Cohen SE, Parmelee AH, Beckwith L, Sigman MD. Cognitive development in preterm infants: Birth to 8 years. J Dev Behav Pediatr. 1986;7(2):102–110. doi: 10.1097/00004703-198604000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Lawson KR, Ruff HA. Early focused attention predicts outcome for children born prematurely. Dev Behav Pediatr. 2004;25:399–406. doi: 10.1097/00004703-200412000-00003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


