Abstract
Objective
Feasibility trials assess whether a behavior change program warrants a definite trial evaluation. This paper reports the feasibility of an intervention consisting of Self Determination Theory-informed text messages, pedometers, and goal prompts to increase adolescent physical activity.
Methods
A four-group randomized design with baseline and immediate post-study assessments was used. Groups (pedometer; pedometer + goal prompt; pedometer + goal prompt + theory-informed texts; no-treatment control) were systematically varied to assess the additive effect of intervention components on objectively-measured physical activity (ie, ActiGraph). The primary outcome of the 12-week intervention was program feasibility. Changes in average daily step counts and minutes of moderate-to-vigorous physical activity were also examined. Post-intervention research with a sub-set of participants examined program reactions.
Results
Participants (N = 160) were evenly split by sex, mostly 14-15 years old, and of diverse race/ethnicity. Feasibility criteria were met. Attrition rate was less than two percent. Modest increases in average daily step counts and moderate-to-vigorous physical activity were observed in all groups except the control group. Participants reported positive reactions to the intervention.
Conclusions
An intervention consisting of pedometers, theory-informed texts, and goal prompts, is a feasible and acceptable method for promoting physical activity to adolescents.
Keywords: text messages, Self Determination Theory, physical activity, pedometers, adolescents, feasibility
INTRODUCTION
Few adolescents in the United States engage in the recommended amounts of physical activity (PA).1 National data show that 72.9% of high school students reported not engaging in 60 or more minutes of PA each day.2 Inadequate PA increases the risk of obesity3 and related diseases, such as type 2 diabetes, cardiovascular disease, and certain cancers.4, 5 Adolescence appears to be a particularly vulnerable period.6 Substantial decreases in PA have been observed between early and late adolescence in both males and females,7,8 with continued decreases into adulthood.9 Thus, there is a public health urgency to identify effective methods to reverse this alarming trend.
Interventions to increase child and adolescent PA have had some success.10–13 When assessed with objective methods, however, increases were small, with little effect on overall PA.14 Thus, innovative methods are needed.
As PA tracks into adulthood,9,15 interventions should focus on promoting PA that can be maintained over time.16 Walking is an enjoyable and familiar form of moderate intensity PA17 when performed briskly.18 It is convenient, and does not require expensive equipment, travel to a specific location, or specialized skills,19–21 suggesting that walking can be sustained over time. Interventions to increase walking have been effective with children and adolescents;22 therefore, encouraging adolescents to increase daily steps may be an effective method for increasing PA in a manner that can be maintained.23
Self-monitoring with goal-setting or feedback is an effective behavior change technique for adults.24 Pedometers, augmented with a daily step goal, offer a convenient way to both self-monitor and obtain real-time feedback on goal progress.25 Pedometer-based studies have increased PA among adults,26 children,27 and adolescents;27 however, additional strategies may be needed to sustain PA over time.27
Motivation is likely an important aspect of sustained PA.16 Self Determination Theory (SDT),28 a theory of motivation, posits that three basic psychological needs (autonomy – having choice and control; competence - having the knowledge and skill to successfully perform a behaviour; and relatedness – connectedness to important others and self) influence motivation, which in turn influences behavior. Higher need satisfaction leads to greater integration of the behavior into one's sense of self (eg, “I am a person who is physically active.”), thus increasing self-determined (ie, autonomous) motivation. SDT has shown promising results with children and adolescents29–34 and may provide insight into ways to promote sustained PA. For example, interventions to enhance psychological need satisfaction have improved cardiovascular fitness in adolescents,29 and both autonomous motivation and PA in children.33 It has also explained changes in elementary children's motivation to participate in physical education class when they moved to middle school,32 and it successfully predicted step counts30 and intention to be physically active during leisure time.31
Interventions should use familiar, convenient, and appealing methods to reach the intended audience. Texting is popular among adolescents, with data suggesting they send and/or receive a median of 100 texts each day.35 Text message-based interventions can be delivered with high fidelity (ie, quality of intervention delivery36),37 a key consideration impacting intervention effectiveness.38
Texting has shown promise as a method for promoting health-enhancing behaviors to children and adolescents.39 Few studies, however, have investigated text messages as a method for promoting PA alone. For example, in a review of information and communication technologies promoting PA to children and adolescents, only three of the nine studies included texting as part of the intervention, and only one of these promoted only PA.40 Although studies have investigated text messages as a method for promoting PA alone,41–44 most have promoted PA along with other behaviors, such as improved diet;45–58 and/or reduced sedentary behavior.48,49,51,53,56,57 Of these, most were designed to promote diabetes41,46,47,50,54 or weight48,51–53,55,58 management. Further, while some studies have investigated text messages as the primary intervention mode,41,45,59 most have incorporated them into multi-component interventions that combined text messages with other intervention components such as in-person meetings, telephone calls, apps, and/or online programs.42,43,46–56
Although theory provides important insights into behavior and can be used to design more focused interventions,60 few studies using text messages alone or in combination with other intervention components reported a theoretical framework. Of those that did, Social Cognitive Theory61 was the most common. Only one published study using text messages to promote PA to children and adolescents could be located that incorporated SDT into its theoretical framework48 and that was a multi-component intervention for overweight/obese adolescents that incorporated text messages in the maintenance phase. No studies were located that investigated SDT-informed text messages emphasizing the basic psychological needs as the primary intervention method for increasing PA in adolescents. Because satisfaction of the basic psychological needs promotes autonomous motivation,28 and motivation is an essential component of behavior change,61 SDT-informed text messages represent a potentially cost effective method for increasing PA. Further, an SDT-grounded study with inactive adults enrolled in an exercise class found that need supportive text messages increased intrinsic (autonomous) motivation and self-reported moderate-to-vigorous PA (MVPA).62 This suggests that need-supportive text messages may be an effective method for increasing and sustaining both autonomous motivation and PA in adolescents. Thus, there is a need to investigate the feasibility and acceptability of this cost-effective, scalable, and easy to disseminate approach with adolescents.
An early step when developing a previously untested intervention is an assessment of feasibility.63 Feasibility studies identify needed changes in procedures and intervention components prior to an efficacy study.64, 65 The purpose of the research reported here was to assess the feasibility of promoting PA to adolescents using pedometers, self-set step goals, and SDT-grounded texts. To assess feasibility, recruitment, attrition, technical issues, data completeness, participant satisfaction, and internal consistency of self-report measures were examined.
METHODS
Study Design
This 12-week study assessed the feasibility of a text message-based intervention approach, using a four-group, randomized design with two data collection periods: baseline and immediate post intervention. After completing baseline data collection, adolescents were randomized using a random numbers table generated by the study biostatistician (YL) with Statistical Analysis Software (SAS) (version 9.4, SAS Institute Inc., Cary, NC, 2012). The four groups were defined as follows: control (no intervention); pedometer-only; pedometer + goal prompts (texts to set a daily step goal for the week); and pedometer + goal prompts + SDT-informed texts (texts promoting satisfaction of the basic psychological needs). After randomization to group, all adolescents except those in the control group received a pedometer (New-Lifestyle, Model AT-82), their average baseline step counts, extracted from the ActiGraph (model GT3X+; Pensacola, FL), age-appropriate pedometer recommendations, and tips for ways to increase steps. The control group received the items listed above after completing post data collection. Feasibility was evaluated overall and by group using a priori criteria.
Sample size
Feasibility studies are not expected to test statistical significance; rather, they address key issues, such as refinement of the research question, study design, procedures (eg, recruitment, data collection), and measurement tools.66–68 The literature is inconsistent regarding appropriate sample sizes for feasibility studies.69 In an audit of pilot and feasibility trials,69 the median sample size for feasibility studies was 36, with a range of 10–300. Therefore, a sample size of 160 (40/group) was selected based on this finding. The 14-17 year old age range was selected because adolescents this age commonly use text messaging for communication,35 and substantial decreases in PA are observed between early and late adolescence.7, 8
Recruitment
Inclusionary criteria were: 14-17 year olds; fluent in English; with cell phone and internet access, and an unlimited text message plan. Exclusionary criteria included having physical (eg, broken leg) or mental (eg, learning impairments) conditions that limited PA or participation in data collection. As this was a minimal risk intervention, participation was not restricted based on current body weight or health status (other than as specified above).
Adolescents were recruited from a large area in the southwestern United States from August 2012 through February 2013. Methods included standard techniques such as posting flyers in community locations likely to be frequented by adolescents and/or their parents, placing notices in electronic newsletters and recruitment websites, attendance at community events, and contacting eligible families in the USDA/ARS Children's Nutrition Research Center volunteer database. Both written parental consent and adolescent assent were obtained prior to participation. Approval was received from the Institutional Review Board of the Baylor College of Medicine, Houston, TX, USA (H-27537). The trial was registered with Clinicaltrials.gov (NCT01482234).
Intervention Components
The 12-week intervention was grounded in SDT. Using an iterative approach, 84 texts were developed in partnership with adolescents who did not participate in the feasibility study. These texts included 12 goal prompts (eg, “My daily step goal this week is…!”) and 72 texts promoting the basic psychological needs. The SDT-informed texts were equally divided between autonomy (eg, “You're in charge! Make the choice to meet your step goal today.”), competence (eg, “You can meet your step goal; just keep steppin'!”) and relatedness (eg, “Meeting your step goal shows you have what it takes to be successful!”). Participants in the pedometer + goal prompt and pedometer + goal prompt + SDT-informed text groups received one goal prompt each week; those in the pedometer + goal prompt + SDT-informed text group also received six weekly texts promoting the basic psychological needs. The distribution schedule was pre-determined. Based on earlier feedback with a different group of 14-17 year olds,70 texts were sent at 8am each day. The four-group design systematically varied intervention components in an effort to determine the ideal combination for a future efficacy trial. The intervention has been described in greater detail elsewhere.70
An Administrative Management System (AMS) automated the study and facilitates future cost-effective dissemination. The AMS was hosted on a password-protected server accessed by study staff. It consisted of a participant database, text message database, and an algorithm. Study staff entered participants into the database after random assignment to group. Each morning at 8am, the AMS algorithm queried the participant database to determine which participants were to receive texts that day; next, it queried the text message database to determine texts to be sent to eligible participants. The algorithm then communicated with the SMS Gateway (Clickatel®) to automatically send the messages. The AMS allowed two-way communication (ie, the adolescents could text the study staff, and the staff could respond via the SMS Gateway). Logs of texts sent and received and technical issues were maintained.70
Procedures
Texts began on the Sunday following entry into the AMS. Adolescents received no more than one automated goal prompt or SDT-informed text per day. Goal prompts to set a daily step goal for the week were sent only on Sundays; SDT-informed texts were sent Monday – Saturday. Each SDT-informed text was designed to promote only one basic psychological need.70 All participants in the pedometer + goal prompts + SDT text group were sent all of the goal prompts and SDT-informed texts during the course of the intervention.
Feasibility criteria
The following criteria were established to determine project feasibility: recruitment goals met (N = 160); attrition rate less than 10%; few technical issues limiting text message delivery; complete data (self-report questionnaires, objectively-measured PA) collected on at least 75% of participants; high participant satisfaction (score of at least 15 out of 20); and acceptable internal consistency of self-report measures (≥ 0.70).70
Measurement
Recruitment was monitored through logs maintained by project staff. Attrition rate was determined by number of participants completing both baseline and post assessment data collection. Project staff and the SMS gateway maintained logs of technical issues. Complete data was determined by identifying the number of participants with complete data at both data collection periods. Program satisfaction was assessed by self-report at post assessment.
Two types of data were collected: objectively-measured PA (step counts, MVPA) and self-report questionnaires assessing demographic characteristics, psychosocial variables, and program satisfaction. PA (step counts, intensity) was assessed with 7 days of accelerometry at baseline and post. The activity monitor was sent and returned by prepaid courier service. The package contained an activity monitor pre-attached to a belt and a graphic information sheet demonstrating how to attach and detach the monitor. Adolescents were also emailed a link to a video demonstrating how to attach and detach the monitor.71
Self-report data included standard demographic questions (baseline only), social desirability of response (baseline only),72,73 basic psychological needs (Basic Psychological Needs Satisfaction Questionnaire),74 and PA motivation (Behavioral Regulation in Exercise Questionnaire).75 Program satisfaction was assessed with a 10-item questionnaire developed for this study, scored on a 3-point Likert scale (yes, no, maybe); total score ranged 0–20 (post only). Sample items included “The time I spent participating in the program was worth it”; “I would recommend the program to others”.
Self-report questionnaires were completed online over a secure, password-protected website. Adolescents were emailed a link to the questionnaires at each data collection period. Staff communicated with adolescents through texts, email, and phone or voice mail as needed.
Post intervention surveys and interviews
Post-intervention surveys and interviews were conducted with 60 randomly selected adolescents who participated in the feasibility study (20 per treatment group). Adolescents completed an online survey, followed by a telephone interview to discuss survey responses. All were asked a core set of questions assessing their thoughts about the overall program and potential enhancements. Additional questions were specific to the intervention components they received.
Statistical Analysis
Feasibility analysis was mainly descriptive (frequencies, percentages). For the feasibility assessment, descriptive statistics were compared to the target goals overall and for each intervention group. The control group was excluded from the “technical issues” feasibility criterion since they did not receive text messages; they were included in the evaluation of all other feasibility criteria.
Accelerometer data were screened to identify periods of wear and non-wear time using the publicly available SAS macros developed by the National Cancer Institute.76 To count as a valid day, participants needed to wear the monitor for at least 10 hours between 6am and midnight. Data were collected in 10 second epochs; epochs were collapsed so that all values of PA were expressed in minutes. Non-wear was defined as 60 minutes or more of consecutive zero counts. Counts < 0 or ≥ 17,000/10 second epoch were interpreted as spurious. Total wear-time was calculated by subtracting non-wear time from the total observation time for the day, 6:00am to midnight (1080 minutes or 18 hours). Step counts were extracted from the accelerometer. Daily step counts were averaged across valid days. Intensity (eg, sedentary, light, moderate-to-vigorous) was assessed with the Evenson cutpoints.77 Participants met the feasibility criteria if they met the wear criteria on at least 4 days, including one weekend day.
Data completeness was assessed by comparing the number of adolescents with complete data at both baseline and post assessment with the number of adolescents enrolled in the study. Program satisfaction was calculated by summing the item scores for each participant, then calculating average program satisfaction score across all participants.
All statistical analyses were conducted using the Statistical Analysis Software (SAS) (version 9.4, SAS Institute Inc., Cary, NC, 2010). Descriptive statistics were calculated for each outcome variable among the entire sample and across four groups. Numerical (Skewness, Kurtosis, and Kolmogorov-Smirnov D) and graphical methods were also used to test normality of each variable.
To evaluate changes in PA (MVPA, step counts) and psychosocial needs and motivation from baseline to post, a repeated measures mixed-effects model with a four-level between-subject factor (group: control, pedometer only, pedometer + goal prompts, pedometer + goal prompts + SDT texts) and a two-level within-subject factor (time: baseline, post) was used, where subjects were treated as random effects, and group, time, and potential interactions between group and time, as fixed effects. Restricted maximum likelihood was applied to estimate variance components and weighted least squares for estimating fixed effects. The mixed-effects models for PA outcome were adjusted for child sex, race/ethnicity, and age, and the models for the psychosocial needs and motivation outcomes were adjusted for social desirability as an additional covariate. As this was a pilot study, it was not powered to detect group differences. As a result, we focused on the strength of evidence for each test and provided an indication of the effect for each test and an exact p-value.78 This approach enables the reader to draw his or her own conclusions about the findings.
Descriptive statistics were calculated for the post study survey data. Similar to the approach used in the HEALTHY Study,79 interviewers created a summary of key points that emerged during the interviews. The summaries were used to ensure comprehension of survey responses and to provide additional insight into participant reactions and suggestions.
RESULTS
Recruitment
On hundred and sixty adolescents were enrolled in the study. Although they reported hearing about the study from a variety of sources, the most common recruitment sources were the USDA/ARS Children's Nutrition Research Center (CNRC) volunteer participant database (N = 77) and the CNRC newsletter, Nutrition & Your Child (N = 44).80 The recruitment goal (N = 160) was attained in approximately six months (August 2012 – February 2013); therefore, recruitment procedures and methods met feasibility standards.
Sample
Adolescents in the recruited sample were fairly evenly split by sex, mostly 14-15 years old, and of diverse race/ethnicity (Table 1).70 Accelerometer-derived step counts and PA indicated adolescents obtained a daily average of 6,824 steps and 22.98 minutes of MVPA (Table 1).
Table 1.
Descriptive statistics for baseline demographic characteristics and physical activity variables (N = 160)
| Total | Control | Pedometer Only | Pedometer + Prompts | Pedometer + Prompts + SDT Texts | |
|---|---|---|---|---|---|
|
|
|||||
| Group, N | 160 | 40 | 40 | 40 | 40 |
| Gender (N (%)) | |||||
| Male | 77 (48.13) | 20 (50.00) | 19 (47.50) | 15 (37.50) | 23 (57.50) |
| Female | 83 (51.88) | 20 (50.00) | 21 (52.50) | 25 (62.50) | 17 (42.50) |
| Age (years) (N (%)) | |||||
| 14–15 | 97 (60.60) | 23 (57.50) | 28 (70.00) | 26 (65.00) | 20 (50.00) |
| 16–17 | 63 (39.40) | 17 (42.50) | 12 (30.00) | 14 (35.00) | 20 (50.00) |
| Ethnicity/Race (N (%)) | |||||
| Hispanic | 43 (26.88) | 9 (22.50) | 11 (27.50) | 12 (30.00) | 11 (27.50) |
| White | 50 (31.25) | 15 (37.50) | 9 (22.50) | 12 (30.00) | 14 (35.00) |
| African American | 57 (35.63) | 13 (32.50) | 16 (40.00) | 15 (37.50) | 13 (32.50) |
| Mixed/Other | 10 (6.25) | 3 (7.50) | 4 (10.00) | 1 (2.50) | 2 (5.00) |
|
| |||||
| Physical Activity, N | 154 | 37 | 39 | 38 | 40 |
|
| |||||
| Moderate-vigorous (mins/day), (mean(SD)) | 22.98 (21.20) | 20.99 (15.49) | 20.52 (17.34) | 26.25 (30.29) | 24.12 (18.88) |
| Steps /day, (mean(SD)) | 6824 (2317) | 6884 (2574) | 6473 (1965) | 6980 (1956) | 6964 (2718) |
Note: N (%) = frequency (percentage); mean(SD) = mean (standard deviation); SDT = Self Determination Theory
Attrition
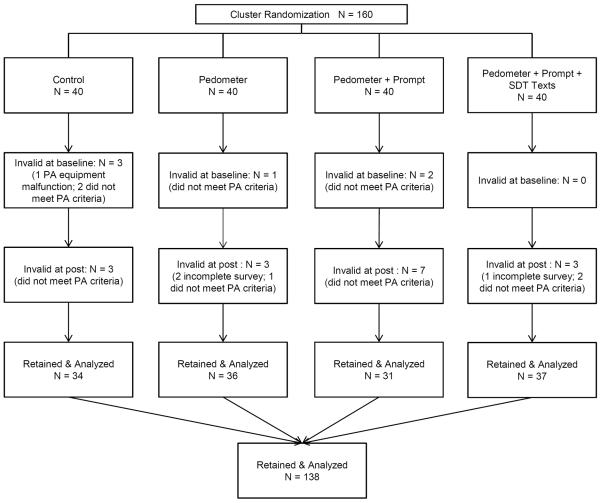
Attrition was low (Figure 1). Only 3 of the 160 adolescents (2%) chose not to participate in post assessment data collection. Attrition did not vary by group (data not shown). The attrition feasibility criterion (attrition < 10%) was met.
Figure 1.
Technical issues
Technical issues were defined as those occurring within the system itself (AMS databases, algorithm, SMS gateway). Only 1 technical issue affected text delivery (ie, the same text was sent multiple times to an adolescent), and it self-corrected. Therefore, the feasibility criterion (few technical issues limiting text message delivery) was met.
Complete data
Complete data (ie, baseline and post) were collected on 86% (N = 138) of participants (Figure 1). Reasons for incomplete data were not meeting PA minimum wear criteria (N = 18), not participating in post data collection, (N = 3), and activity monitor malfunction (N = 1). The feasibility criterion (complete data collected on ≥ 75% of participants) was met.
The retained sample was compared to those excluded to identify potential issues that need to be addressed prior to an efficacy study. The retained sample was similar to the recruited sample: 52.17% male, 14-15 years old (62.31%), and African American (33.33%). Differences in age (p = .006) and race/ethnicity (p = .005) were observed when comparing the retained sample (N = 138) to those excluded from the post analyses (N = 22). Those excluded were more likely to be 16 years old (31.82% vs. 21.74%) and African American (50.00% vs. 33.33%) (Table 2).
Table 2.
Comparison of retained (N = 138) and excluded (N = 22) participants by demographic characteristics
| Total | Retained | Excluded | p-value | |
|---|---|---|---|---|
|
|
||||
| Gender, (N (%)) | 0.850 | |||
| Male | 77 (48.13) | 72 (52.17) | 11 (50.00) | |
| Female | 83 (51.88) | 66 (47.83) | 11 (50.00) | |
| Age range, (N (%)) | 0.006 | |||
| 14 yrs | 49 (30.63) | 44 (31.88) | 5 (22.73) | |
| 15 yrs | 48 (30.00) | 42 (30.43) | 6 (27.27) | |
| 16 yrs | 37 (23.13) | 30 (21.74) | 7 (31.82) | |
| 17 yrs | 26 (16.25) | 22 (15.94) | 4 (18.18) | |
| Race/Ethnicity, (N (%)) | 0.005 | |||
| Hispanic | 43 (26.88) | 38 (27.54) | 5 (22.73) | |
| White | 50 (31.25) | 44 (31.88) | 6 (27.27) | |
| African American | 57 (35.63) | 46 (33.33) | 11 (50.00) | |
| Mixed/Other | 10 (6.25) | 10 (7.25) | 0 (0.00) | |
Note: N (%) = frequency (percentage)
Program satisfaction
Average program satisfaction was 17.47 points out of 20.0 possible points; there was evidence of group differences (p = .068). Program satisfaction was highest among the group that received all intervention components (18.18 points), followed by groups that received a pedometer + goal prompt (18.05 points), pedometer only (17.05 points), and the control group (16.60 points). Therefore, the feasibility criterion (program satisfaction score of ≥ 15 out of 20 points) was met.
Internal consistency
Internal consistency of all self-report measures exceeded the feasibility criterion (≥ 0.70) at both baseline and post assessment. The lowest alpha value was for social desirability (0.74); internal consistency for all other scales exceeded 0.80 (data not shown). Therefore, the measures were deemed appropriate for a future efficacy study.
PA trends
Descriptive trends in accelerometer-derived step counts and MVPA in all intervention groups were in the expected directions. Adolescents in the group receiving all intervention components had the greatest increases in steps (+317.8 steps/day) and MVPA (+1.73 minutes/day) when compared to other groups (Table 3). There was no evidence of interactions or group or time main effects.
Table 3.
Parameter estimates from repeated measures of mixed models, stratified by group and time.
| Physical Activity Intensity (activity monitors)2 | Baseline | Follow-up | Change from Baseline | Group × Time | Time | Group | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| N | Mean (SE)1 | N | Mean (SE) | Changes | P (t) | F(3,144) | P | F(1,144) | P | F(3,147) | P | |
|
|
||||||||||||
| Moderate-vigorous (mins/day) | 0.32 | 0.815 | 0.09 | 0.764 | 1.42 | 0.240 | ||||||
| Control | 37 | 21.00 (3.32) | 37 | 19.44 (3.32) | −1.56 | 0.555 | ||||||
| pedometer only | 39 | 21.61 (3.32) | 39 | 22.87 (3.37) | 1.26 | 0.626 | ||||||
| pedometer + prompts | 38 | 28.40 (3.45) | 33 | 28.51 (3.56) | 0.11 | 0.969 | ||||||
| pedometer + prompts + SDT texts | 40 | 23.30 (3.31) | 37 | 25.02 (3.37) | 1.73 | 0.498 | ||||||
| Steps /day | 0.25 | 0.862 | 0.51 | 0.475 | 0.48 | 0.696 | ||||||
| Control | 37 | 6783 (386.35) | 37 | 6708 (386.65) | −74.7 | 0.846 | ||||||
| pedometer only | 39 | 6461 (382.80) | 39 | 6745 (391.78) | 283.8 | 0.452 | ||||||
| pedometer + prompts | 38 | 7013 (397.88) | 33 | 7068 (416.05) | 54.7 | 0.890 | ||||||
| pedometer + prompts + SDT texts | 40 | 6730 (380.90) | 37 | 7048 (390.98) | 317.8 | 0.394 | ||||||
Note:
Adjusted mean (Standard error);
The models were controlled for age, gender, and ethnicity; P(t) = p value from t-test; F = F statistics; P = p-value from F test; SDT = Self Determination Theory
Basic Psychological Needs
Minimal changes occurred in the basic psychological needs, regardless of group. There was no evidence of interactions or group or time main effects (data not shown).
PA motivation
There was no evidence of interaction, group, or time effects occurred in autonomous or controlled motivation (data not shown).
Adolescent Suggestions
Adolescents who received all intervention components (N = 20) thought taking more steps each day was a good way to help them be more physically active (85%) and that the pedometer helped them keep track of their daily steps (80%). However, 75% thought other types of PA should be promoted in addition to walking. When asked to identify a realistic amount of steps to increase each day, adolescents were unsure, with responses ranging from “I don't know” (10%) to 1,000 (10%); the most common response was 200 steps per day (50%). Thus, it is not surprising that 75% of the adolescents would have liked the study to set a step goal for them each week. Further, although 55% would have liked to text their step goal to the study, 45% were unsure. There was also variation with regard to texting goal attainment status to the study: 55% reported they would have liked to do this, while 35% were unsure. Almost all (90%) said they would have liked the study to provide suggestions on ways to increase their daily steps. Eighty percent of the adolescents liked receiving daily texts for 12 weeks; 85% read them daily; 75% said they were helpful; and 55% said they were motivational. Suggestions for improvement included adding variety and making texts less repetitive and a little more interesting. Most (95%) would have liked some of the texts to include tips on how to meet their step goal. While the texts were sent at 8am each day, 55% said 3–6pm would be the best time to receive PA texts; noon was the next most popular response (20%).
Additional insights on adolescent reactions to the program were obtained from the interviews. Regardless of the intervention component received, most thought that taking more steps each day was a good way to help adolescents be more physically active because it is easy to do, does not require a lot of effort, and nothing else is needed (eg, equipment, special attire). They also saw it as the first step towards becoming more physically active. Most thought other types of PA should also be promoted, such as jumping jacks, running, jogging, and sports. However, adolescents cautioned the additional PA should not require much equipment and should include activities they can do on their own. Adolescents thought 12 weeks was an acceptable intervention length because it was not too short or long and was enough time for them to change their habits and maintain them. “It's hard to get yourself to exercise, especially if it's just a month long. In a couple of days you don't get very into it. But in 3 months you have the opportunity to really build on your goals and incorporate more types of exercise” (Female, pedometer + goal prompt group).
Discussion
Feasibility is an important first step in the development of a previously untested intervention.63–65 The primary purpose of this study was to examine the feasibility of promoting PA to adolescents using pedometers, goal prompts, and SDT-grounded text messages. All feasibility criteria were met; therefore, recruitment, retention, data collection, and intervention procedures and measures were deemed appropriate for use in a future efficacy study.
Program satisfaction was high, particularly in the group receiving all intervention components, indicating adolescents found the intervention approach acceptable. Thus, the present study makes an important contribution by demonstrating the feasibility and acceptability of SDT-informed texts, augmented with a pedometer and goal prompts, to increase adolescent PA. This is an important finding, given that this intervention approach is a scalable, potentially cost-effective, and broadly disseminable method for encouraging adolescents to be more physically active.
Another important finding was the low attrition rate. A possible explanation for this is that the text messages were developed in partnership with adolescents, which may have increased their acceptability.70 Hingle et al45 included adolescents in the development of texts promoting diet and PA45, and found that both the texts and the intervention mode (texting) were acceptable. Further, open-ended text messages guided by motivational interviewing were also found to be personally relevant and appealing to adolescents in an obesity treatment intervention.81 Alternatively, in a brief study investigating social support and PA, adolescent girls were encouraged to construct and send self-generated supportive texts to others in the study;43 however, they appeared unsure how to construct such texts. Further, other research found that overweight and obese adolescents were inconsistent in their views of what types of texts would support maintenance of behavior change.82 Because it is critical that text messages in an intervention of this type appeal to adolescents, these results suggest that text messages promoting behavior change should be jointly developed by researchers and adolescents using an iterative process,83 such as that used in the present study.70 Future research is needed to identify the best method for achieving this.
There were modest increases in accelerometer-derived average daily step counts and minutes of MVPA in the group that received all intervention components. Similar results were observed for basic psychological needs and motivation. Caution should be applied when interpreting these results, however. The study was not adequately powered to detect an effect on a primary outcome and therefore, it is possible that different results would have been obtained with an adequately-powered sample.66 Future intervention research should investigate short- and longer-term changes in steps and MVPA, basic psychological needs, intrinsic motivation with a larger group of adolescents. Future research should also examine the ideal intervention length and structure to sustain PA.
Theory is an important component of intervention design and evaluation,60 and there have been calls to carefully operationalize theory in behavioral interventions.84 The current study designed text messages tightly connected to the basic psychological needs, ie, autonomy, competence, and relatedness, which are key components of SDT.28 SDT has successfully guided research to understand and promote PA in children and adolescents.29–34 However, SDT-informed text messages targeting the basic psychological needs may not be powerful enough to enhance need satisfaction, autonomous motivation, and PA in adolescents. A multi-theoretical framework may be needed or perhaps the text messages need to be more targeted. For example, Kinnafick et al62 found that need-supportive text messages focused on environmental support enhanced the basic psychological needs, intrinsic motivation, and self-reported MVPA in adults. Thus, future research should investigate other methods for developing need-supportive text messages for adolescents and their effect on the basic psychological needs, intrinsic motivation, and PA.
Goal setting is an often-used behavior change technique.24 Since autonomy is a key construct in SDT and providing adolescents with study-determined goals seemed counter-intuitive to promoting choice and control, adolescents were asked to self-set a personal step goal each week.70 The post-study revealed that they would have liked to receive a weekly step goal set by the study. This suggests that adolescents may not have the skill to set optimal behavior change goals (ie, goals that are not too easy or difficult28) and would have benefitted from guidance in how to achieve this. Previous research supports that children and adolescents have difficulty setting goals.85–88 The literature provides guidance on how to address this issue. For example, SDT and goal setting theory were combined in a diet and PA behavior change intervention for overweight adolescents by focusing on intrinsic goals.89 Further, action plans were found to be effective at increasing fruit and vegetable intake with elementary aged children.90 Therefore, structured goal setting, an emphasis on intrinsic goals, and the inclusion of action plans may help adolescents attain their daily step goals within a SDT-guided intervention, particularly when the plan includes choice, emphasizes relatedness, and builds competence. The post-study suggested that adolescents were unsure of what a realistic step goal increase would be, which may partially explain the small increases observed in steps and MVPA. Therefore, structured goal setting that offers adolescents choice among realistic step increases may help them increase PA in a manner that increases PA and enhances both competence and autonomy.
Adolescents also stated they would have liked to report goal attainment. This was not originally included in the feasibility study because of concerns it would have a deleterious effect on autonomy (ie, sense of personal control). However, incorporating goal reporting into the intervention would provide an opportunity to provide need-supportive feedback encouraging persistence, acknowledging successes, and emphasizing feelings.28 Future research should identify the most effective ways to incorporate goal reporting and need-supportive feedback into a text message based intervention encouraging adolescents to be more physically active.
Strengths of this research included a design that facilitated a systematic examination of the incremental effect of each program component (pedometers alone, pedometers + goal prompts, pedometers + goal prompts + SDT-informed text messages) on steps and MVPA and an assessment of the feasibility of this intervention approach. It also had a firm grounding in theory (SDT), and post-study research was conducted to identify reactions. The study used an objective assessment of PA and provided a pedometer, a broadly available device with which adolescents are familiar. Limitations included conducting the study in one geographic area; recruiting adolescents from the CNRC volunteer database and newsletter which decreased generalizability; short study duration (12 weeks); no assessment of maintenance (ie, sustainability); and not comparing texting to other technology-based ways in which adolescents communicate (eg, SnapChat, Vine, Facebook Messenger).
CONCLUSIONS
SDT-grounded texts, augmented with pedometers and goal prompts, is a feasible method for promoting PA to adolescents. Post study surveys and interviews with adolescents provided important suggestions for enhancements that should be tested in a future, fully powered randomized controlled trial.
Acknowledgements
This project was supported by the National Institutes of Health, National Institute of Child Health & Human Development grant #R21HD066305 (to Dr. Thompson). This work is also a publication of the United States Department of Agriculture/Agricultural Research Center (USDA/ARS), Children's Nutrition Research Center, Department of Pediatrics, Baylor College of Medicine, Houston, Texas, and funded in part with federal funds from the USDA/ARS under Cooperative Agreement No. 58-6250-0-008. The contents of this publication do not necessarily reflect the views or policies of the USDA, nor does mention of trade names, commercial products, or organizations imply endorsement from the U.S. government. We would like to thank the adolescents who participated in this research. We would also like to extend our thanks to Archimage, Inc. of Houston, TX for its design services and would especially like to acknowledge Richard Buday, FAIA, its President, and Ramsey Tapia.
Human Subjects Statement Human subjects approval was received from the Institutional Review Board of the Baylor College of Medicine, Houston, TX, USA (H-27537).
Footnotes
Conflict of Interests Statement The authors have no conflicts of interest.
References
- 1.US Department of Health and Human Services - Physical Activity Guidelines Advisory Committee [Accessed February 5, 2016];Physical Activity Guidelines for Americans. 2008 Available at: http://www.health.gov/paguidelines/guidelines/default.aspx.
- 2.Kann L, Kinchen S, Shanklin SL, et al. Youth risk behavior surveillance - United States, 2013. MMWR Surveill Summ. 2014;63(Suppl 4):1–168. [PubMed] [Google Scholar]
- 3.Salbe AD, Weyer C, Harper I, et al. Assessing risk factors for obesity between childhood and adolescence: II. Energy metabolism and physical activity. Pediatrics. 2002;110(2 Pt 1):307–314. doi: 10.1542/peds.110.2.307. [DOI] [PubMed] [Google Scholar]
- 4.Alwan A, Armstrong T, Bettcher D, et al. Global Status Report on Noncommunicable Diseases 2010. World Health Organization; Geneva, Switzerland: 2011. Available from: http://www.who.int/nmh/publications/ncd_report2010/en/ [Google Scholar]
- 5.World Cancer Research Fund & American Institute for Cancer Research [Accessed February 5, 2016];Food, nutrition, physical activity, and the prevention of cancer: A global perspective. Available at: http://www.dietandcancerreport.org/cancer_resource_center/downloads/summary/english.pdf.
- 6.Dumith SC, Gigante DP, Domingues MR, et al. Physical activity change during adolescence: a systematic review and a pooled analysis. Int J Epidemiol. 2011;40(3):685–698. doi: 10.1093/ije/dyq272. [DOI] [PubMed] [Google Scholar]
- 7.Nelson MC, Neumark-Stzainer D, Hannan PJ, et al. Longitudinal and secular trends in physical activity and sedentary behavior during adolescence. Pediatrics. 2006;118(6):e1627–1634. doi: 10.1542/peds.2006-0926. [DOI] [PubMed] [Google Scholar]
- 8.Nader PR, Bradley RH, Houts RM, et al. Moderate-to-vigorous physical activity from ages 9 to 15 years. JAMA. 2008;300(3):295–305. doi: 10.1001/jama.300.3.295. [DOI] [PubMed] [Google Scholar]
- 9.Telama R, Yang X, Viikari J, et al. Physical activity from childhood to adulthood: a 21-year tracking study. Am J Prev Med. 2005;28(3):267–273. doi: 10.1016/j.amepre.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 10.Salmon J, Booth ML, Phongsavan P, et al. Promoting physical activity participation among children and adolescents. Epidemiol Rev. 2007;29:144–159. doi: 10.1093/epirev/mxm010. [DOI] [PubMed] [Google Scholar]
- 11.van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. Br J Sports Med. 2008;42(8):653–657. [PubMed] [Google Scholar]
- 12.Kriemler S, Meyer U, Martin E, et al. Effect of school-based interventions on physical activity and fitness in children and adolescents: a review of reviews and systematic update. Br J Sports Med. 2011;45(11):923–930. doi: 10.1136/bjsports-2011-090186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lonsdale C, Rosenkranz RR, Peralta LR, et al. A systematic review and meta-analysis of interventions designed to increase moderate-to-vigorous physical activity in school physical education lessons. Prev Med. 2013;56(2):152–161. doi: 10.1016/j.ypmed.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 14.Metcalf B, Henley W, Wilkin T. Effectiveness of intervention on physical activity of children: Systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54) BMJ. 2012;345:e5888. doi: 10.1136/bmj.e5888. [DOI] [PubMed] [Google Scholar]
- 15.Craigie AM, Lake AA, Kelly SA, et al. Tracking of obesity-related behaviours from childhood to adulthood: a systematic review. Maturitas. 2011;70(3):266–284. doi: 10.1016/j.maturitas.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 16.Teixeira PJ, Carraca EV, Markland D, et al. Exercise, physical activity, and self-determination theory: a systematic review. Int J Behav Nutr Phys Act. 2012;9:78. doi: 10.1186/1479-5868-9-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simpson ME, Serdula M, Galuska DA, et al. Walking trends among U.S. adults: the Behavioral Risk Factor Surveillance System, 1987–2000. Am J Prev Med. 2003;25(2):95–100. doi: 10.1016/s0749-3797(03)00112-0. [DOI] [PubMed] [Google Scholar]
- 18.Ridley K, Ainsworth BE, Olds TS. Development of a compendium of energy expenditures for youth. Int J Behav Nutr Phys Act. 2008;5:45. doi: 10.1186/1479-5868-5-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ogilvie D, Foster CE, Rothnie H, et al. Interventions to promote walking: systematic review. BMJ. 2007;334(7605):1204. doi: 10.1136/bmj.39198.722720.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee IM, Buchner DM. The importance of walking to public health. Med Sci Sports Exerc. 2008;40(7 Suppl):S512–518. doi: 10.1249/MSS.0b013e31817c65d0. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention Vital signs: Walking among adults--United States, 2005 and 2010. MMWR Morb Mortal Wkly Rep. 2012;61(31):595–601. [PubMed] [Google Scholar]
- 22.Carlin A, Murphy MH, Gallagher AM. Do interventions to increase walking work? A systematic review of interventions in children and adolescents. Sports Med. 2016;46(4):515–530. doi: 10.1007/s40279-015-0432-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hillsdon M, Thorogood M. A systematic review of physical activity promotion strategies. Br J Sports Med. 1996;30(2):84–89. doi: 10.1136/bjsm.30.2.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Michie S, Abraham C, Whittington C, et al. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28(6):690–701. doi: 10.1037/a0016136. [DOI] [PubMed] [Google Scholar]
- 25.Tudor-Locke C. [Accessed February 5, 2016];Taking steps toward increased physical activity: using pedometers to measure and motivate. Available at: http://files.eric.ed.gov/fulltext/ED470689.pdf.
- 26.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298(19):2296–2304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- 27.Lubans DR, Morgan PJ, Tudor-Locke C. A systematic review of studies using pedometers to promote physical activity among youth. Prev Med. 2009;48(4):307–315. doi: 10.1016/j.ypmed.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 28.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well being. Am Psychol. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 29.Springer JB. “I am very, very proud of myself”: improving youth activity levels using self-determination theory in program development. Front Public Health. 2013;1:46. doi: 10.3389/fpubh.2013.00046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Standage M, Gillison FB, Ntoumanis N, et al. Predicting students' physical activity and health-related well-being: a prospective cross-domain investigation of motivation across school physical education and exercise settings. J Sport Exerc Psychol. 2012;34(1):37–60. doi: 10.1123/jsep.34.1.37. [DOI] [PubMed] [Google Scholar]
- 31.Standage M, Duda JL, Ntoumanis N. A model of contextual motivation in physical education: using constructs from self-determination and achievement goal theories to predict physical activity intentions. J Educ Psychol. 2003;95(1):97–110. [Google Scholar]
- 32.Ullrich-French S, Cox AE. Normative and intraindividual changes in physical education motivation across the transition to middle school: A multilevel growth analysis. Sport Exerc Perform Psychol. 2014;3(2):132–147. [Google Scholar]
- 33.Sebire SJ, Jago R, Fox KR, et al. Testing a self-determination theory model of children's physical activity motivation: a cross-sectional study. Int J Behav Nutr Phys Act. 2013;10:111. doi: 10.1186/1479-5868-10-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Owen KB, Smith J, Lubans DR, et al. Self-determined motivation and physical activity in children and adolescents: a systematic review and meta-analysis. Prev Med. 2014;67:270–279. doi: 10.1016/j.ypmed.2014.07.033. [DOI] [PubMed] [Google Scholar]
- 35.Lenhart A. [Accessed February 5, 2016];Teens, smartphones & texting. Available at: http://www.pewinternet.org/2012/03/19/teens-smartphones-texting/
- 36.Linnan L, Steckler A. Process evaluation for public health interventions and research: an overview. In: Linnan L, Steckler A, editors. Process Evaluation for Public Health Interventions and Research. Jossey-Bass; San Francisco, CA: 2002. pp. 1–23. [Google Scholar]
- 37.Mason M, Ola B, Zaharakis N, et al. Text messaging interventions for adolescent and young adult substance use: a meta-analysis. Prev Sci. 2015;16(2):181–188. doi: 10.1007/s11121-014-0498-7. [DOI] [PubMed] [Google Scholar]
- 38.Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol. 2008;41(3–4):327–350. doi: 10.1007/s10464-008-9165-0. [DOI] [PubMed] [Google Scholar]
- 39.Militello LK, Kelly SA, Melnyk BM. Systematic review of text-messaging interventions to promote healthy behaviors in pediatric and adolescent populations: implications for clinical practice and research. Worldviews Evid Based Nurs. 2012;9(2):66–77. doi: 10.1111/j.1741-6787.2011.00239.x. [DOI] [PubMed] [Google Scholar]
- 40.Lau PW, Lau EY, Wong del P, et al. A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents. J Med Internet Res. 2011;13(3):e48. doi: 10.2196/jmir.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Newton KH, Wiltshire EJ, Elley CR. Pedometers and text messaging to increase physical activity: randomized controlled trial of adolescents with type 1 diabetes. Diabetes Care. 2009;32(5):813–815. doi: 10.2337/dc08-1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Newton RL, Jr., Marker AM, Allen HR, et al. Parent-targeted mobile phone intervention to increase physical activity in sedentary children: randomized pilot trial. JMIR Mhealth Uhealth. 2014;2(4):e48. doi: 10.2196/mhealth.3420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Toscos T, Faber A, Connelly K, et al. Encouraging physical activity in teens: can technology help reduce barriers to physical activity in adolescent girls?. Proceedings of the 2nd International Conference on Pervasive Computing Technologies for Healthcare.2008. pp. 218–221. [Google Scholar]
- 44.Lau EY, Lau PW, Cai B, et al. The effects of text message content on the use of an internet-based physical activity intervention in Hong Kong Chinese adolescents. J Health Commun. 2015;20(9):1041–1051. doi: 10.1080/10810730.2015.1018580. [DOI] [PubMed] [Google Scholar]
- 45.Hingle M, Nichter M, Medeiros M, et al. Texting for health: the use of participatory methods to develop healthy lifestyle messages for teens. J Nutr Educ Behav. 2013;45(1):12–19. doi: 10.1016/j.jneb.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 46.Patrick K, Norman GJ, Davila EP, et al. Outcomes of a 12-month technology-based intervention to promote weight loss in adolescents at risk for type 2 diabetes. J Diabetes Sci Technol. 2013;7(3):759–770. doi: 10.1177/193229681300700322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Markowitz JT, Cousineau T, Franko DL, et al. Text messaging intervention for teens and young adults with diabetes. J Diabetes Sci Technol. 2014;8(5):1029–1034. doi: 10.1177/1932296814540130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Straker LM, Howie EK, Smith KL, et al. The impact of Curtin University's Activity, Food and Attitudes Program on physical activity, sedentary time and fruit, vegetable and junk food consumption among overweight and obese adolescents: A waitlist controlled trial. PLoS One. 2014;9(11):e111954. doi: 10.1371/journal.pone.0111954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Silva C, Fassnacht DB, Ali K, et al. Promoting health behaviour in Portuguese children via Short Message Service: the efficacy of a text-messaging programme. J Health Psychol. 2015;20(6):806–815. doi: 10.1177/1359105315577301. [DOI] [PubMed] [Google Scholar]
- 50.Froisland DH, Arsand E, Skarderud F. Improving diabetes care for young people with type 1 diabetes through visual learning on mobile phones: mixed-methods study. J Med Internet Res. 2012;14(4):e111. doi: 10.2196/jmir.2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Price S, Ferisin S, Sharifi M, et al. Development and implementation of an interactive text messaging campaign to support behavior change in a childhood obesity randomized controlled trial. J Health Commun. 2015;20(7):843–850. doi: 10.1080/10810730.2015.1018582. [DOI] [PubMed] [Google Scholar]
- 52.Militello L, Melnyk BM, Hekler EB, et al. Automated behavioral text messaging and face-to-face intervention for parents of overweight or obese preschool children: results from a pilot study. JMIR Mhealth Uhealth. 2016;4(1):e21. doi: 10.2196/mhealth.4398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Huang JS, Dillon L, Terrones L, et al. Fit4Life: A weight loss intervention for children who have survived childhood leukemia. Pediatr Blood Cancer. 2014;61(5):894–900. doi: 10.1002/pbc.24937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Franklin VL, Waller A, Pagliari C, et al. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med. 2006;23(12):1332–1338. doi: 10.1111/j.1464-5491.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- 55.de Niet J, Timman R, Bauer S, et al. The effect of a short message service maintenance treatment on body mass index and psychological well-being in overweight and obese children: a randomized controlled trial. Pediatr Obes. 2012;7(3):205–219. doi: 10.1111/j.2047-6310.2012.00048.x. [DOI] [PubMed] [Google Scholar]
- 56.Shapiro JR, Bauer S, Hamer RM, et al. Use of text messaging for monitoring sugar-sweetened beverages, physical activity, and screen time in children: a pilot study. J Nutr Educ Behav. 2008;40(6):385–391. doi: 10.1016/j.jneb.2007.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fassnacht DB, Ali K, Silva C, et al. Use of text messaging services to promote health behaviors in children. J Nutr Educ Behav. 2015;47(1):75–80. doi: 10.1016/j.jneb.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 58.Shrewsbury VA, O'Connor J, Steinbeck KS, et al. A randomised controlled trial of a community-based healthy lifestyle program for overweight and obese adolescents: the Loozit study protocol. BMC Public Health. 2009;9:119. doi: 10.1186/1471-2458-9-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sirriyeh R, Lawton R, Ward J. Physical activity and adolescents: an exploratory randomized controlled trial investigating the influence of affective and instrumental text messages. Br J Health Psychol. 2010;15(Pt 4):825–840. doi: 10.1348/135910710X486889. [DOI] [PubMed] [Google Scholar]
- 60.Baranowski T, Anderson C, Carmack C. Mediating variable framework in physical activity interventions. How are we doing? How might we do better? Am J Prev Med. 1998;15(4):266–297. doi: 10.1016/s0749-3797(98)00080-4. [DOI] [PubMed] [Google Scholar]
- 61.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 62.Kinnafick FE, Thogersen-Ntoumani C, Duda J. The effect of need supportive text messages on motivation and physical activity behaviour. J Behav Med. 2016 doi: 10.1007/s10865-016-9722-1. doi: 10.1007/s10865-016-9722-1. [Epub aphead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med. 2009;36(5):452–457. doi: 10.1016/j.amepre.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stevens J, Taber DR, Murray DM, et al. Advances and controversies in the design of obesity prevention trials. Obesity (Silver Spring) 2007;15(9):2163–2170. doi: 10.1038/oby.2007.257. [DOI] [PubMed] [Google Scholar]
- 65.Jago R, Sebire SJ. Publishing pilot and feasibility evaluations of behavioural interventions: Implications for preventive medicine. Prev Med. 2012;55(6):548–549. doi: 10.1016/j.ypmed.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 66.Kraemer HC, Mintz J, Noda A, et al. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63(5):484–489. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- 67.Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45(5):626–629. doi: 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Thabane L, Ma J, Chu R, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10:1. doi: 10.1186/1471-2288-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Billingham SA, Whitehead AL, Julious SA. An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom Clinical Research Network database. BMC Med Res Methodol. 2013;13:104. doi: 10.1186/1471-2288-13-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Thompson D, Cantu D, Bhatt R, et al. Texting to increase physical activity among teens (TXT Me!): rationale, design, and methods. JMIR Res Protoc. 2014;3(1):e14. doi: 10.2196/resprot.3074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Thompson DI, Abdelsamad D, Cantu DA, et al. Instructional physical activity monitor video in English and Spanish. Am J Prev Med. 2012;42(3):e29–30. doi: 10.1016/j.amepre.2011.10.024. [DOI] [PubMed] [Google Scholar]
- 72.Reynolds CR, Paget KD. National normative and reliability data for the Revised Children's Manifest Anxiety Scale. School Psych Rev. 1983;12(3):324–336. [Google Scholar]
- 73.Dadds MR, Perrin S, Yule W. Social desirability and self-reported anxiety in children: an analysis of the RCMAS lie scale. J Abnorm Child Psychol. 1998;26(4):311–317. doi: 10.1023/a:1022610702439. [DOI] [PubMed] [Google Scholar]
- 74.Wilson PM, Rogers WT, Rodgers WM, et al. The Psychological Need Satisfaction in Exercise Scale. J Sport Exerc Psychol. 2006;28(3):231–251. [Google Scholar]
- 75.Wilson PM, Rodgers WM, Loitz CC, et al. “It's Who I Am…Really!” The importance of integrated regulation in exercise contexts. J Appl Biobehav Res. 2006;11:79–104. [Google Scholar]
- 76.National Cancer Institute [Accessed February 5, 2016];SAS programs for analyzing NHANES 2003–2004 accelerometer data. Available at: http://appliedresearch.cancer.gov/nhanes_pam/
- 77.Trost SG, Loprinzi PD, Moore R, et al. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc. 2011;43(7):1360–1368. doi: 10.1249/MSS.0b013e318206476e. [DOI] [PubMed] [Google Scholar]
- 78.Sterne JA, Davey Smith G. Sifting the evidence-what's wrong with significance tests? BMJ. 2001;322(7280):226–231. doi: 10.1136/bmj.322.7280.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Schneider M, Hall WJ, Hernandez AE, et al. Rationale, design and methods for process evaluation in the HEALTHY study. Int J Obes (Lond) 2009;33(Suppl 4):S60–67. doi: 10.1038/ijo.2009.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.USDA/ARS Children's Nutrition Research Center, Baylor College of Medicine [Accessed February 5, 2016];Newsletter - Nutrition and Your Child. Available at: https://www.bcm.edu/departments/pediatrics/sections-divisions-centers/childrens-nutrition-research-center/news/cnrc-newsleters.
- 81.Woolford SJ, Clark SJ, Strecher VJ, et al. Tailored mobile phone text messages as an adjunct to obesity treatment for adolescents. J Telemed Telecare. 2010;16(8):458–461. doi: 10.1258/jtt.2010.100207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Smith KL, Kerr DA, Fenner AA, et al. Adolescents just do not know what they want: a qualitative study to describe obese adolescents' experiences of text messaging to support behavior change maintenance post intervention. J Med Internet Res. 2014;16(4):e103. doi: 10.2196/jmir.3113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Thompson D. Talk to me, please! The importance of qualitative research to games for health. Games Health J. 2014;3(3):117–118. doi: 10.1089/g4h.2014.0023. [DOI] [PubMed] [Google Scholar]
- 84.Michie S, Johnston J. Theories and techniques of behaviour change: developing a cumulative science of behaviour change. Health Psychol Rev. 2012;6(1):1–6. [Google Scholar]
- 85.Cullen KW, Baranowski T, Baranowski J, et al. “5 A Day” achievement badge for urban Boy Scouts: formative evaluation results. J Cancer Educ. 1998;13(3):162–168. doi: 10.1080/08858199809528538. [DOI] [PubMed] [Google Scholar]
- 86.Thompson D, Cullen KW, Boushey C, et al. Design of a website on nutrition and physical activity for adolescents: results from formative research. J Med Internet Res. 2012;14(2):e59. doi: 10.2196/jmir.1889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Thompson D, Baranowski T, Buday R, et al. In pursuit of change: youth response to intensive goal setting embedded in a serious videogame. J Diabetes Sci Technol. 2007;1(6):907–917. doi: 10.1177/193229680700100617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cullen KW, Thompson D, Boushey C, et al. Evaluation of a web-based program promoting healthy eating and physical activity for adolescents: Teen Choice: Food and Fitness. Health Educ Res. 2013;28(4):704–714. doi: 10.1093/her/cyt059. [DOI] [PubMed] [Google Scholar]
- 89.Fenner AA, Straker LM, Davis MC, et al. Theoretical underpinnings of a need-supportive intervention to address sustained healthy lifestyle changes in overweight and obese adolescents. Psychol Sport Exerc. 2013;14(6):819–829. [Google Scholar]
- 90.Thompson D, Bhatt R, Vazquez I, et al. Creating action plans in a serious video game increases and maintains child fruit-vegetable intake: a randomized controlled trial. Int J Behav Nutr Phys Act. 2015;12:39. doi: 10.1186/s12966-015-0199-z. [DOI] [PMC free article] [PubMed] [Google Scholar]