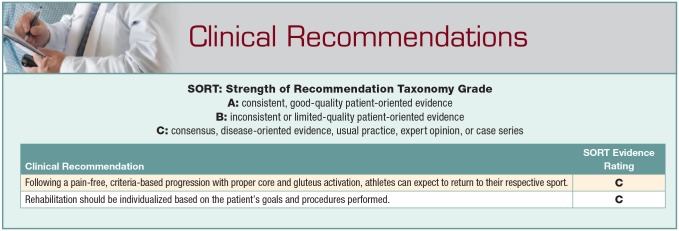
Abstract
Context:
Femoroacetabular impingement (FAI) was first described by Ganz in 2003 and is a significant cause of decreased function and mobility. Femoroacetabular impingement must be treated in an individualized, goal-oriented, stepwise fashion. This protocol was developed with biomechanical considerations of soft tissue and bony structures surrounding the hip joint.
Evidence Acquisition:
The PubMed database was searched for scientific and review articles from the years 2000 to 2015 utilizing the search terms: hip rehabilitation, femoroacetabular impingement, and arthroscopy.
Study Design:
Clinical review.
Level of Evidence:
Level 5.
Results:
Five hundred ninety-five of 738 patients were available for follow-up showing improvement from preoperative to 2-year follow-up of 61.29 to 82.02 for modified Harris Hip Score (mHHS), 62.79 to 83.04 for Hip Outcome Score–Activities of Daily Living (HOS-ADL), 40.96 to 70.07 for Hip Outcome Score–Sport-Specific Subscale (HOS-SSS), and 57.97 to 80.41 for Non-Arthritic Hip Score (NAHS); visual analog scale (VAS) scores decreased from 5.86 preoperatively to 2.94 postoperatively.
Conclusion:
Following a structured, criteria-based program, appropriate patients undergoing hip arthroscopy may achieve excellent outcomes and return to full independent activities of daily living as well as sport.
Keywords: femoroacetabular impingement (FAI), hip rehabilitation, impingement
Ganz et al7 were the first to describe femoroacetabular impingement (FAI) in 2003, showing that early surgical intervention to alleviate the femoral abutment against the acetabular rim may slow the degenerative process for young patients with hip pathology. Over the past decade, the diagnosis and treatment of FAI has evolved. As arthroscopic hip procedures continue to advance and the population of patients undergoing surgery expands, the need for quality and comprehensive rehabilitation is essential to maximize outcomes of this patient group.
Few publications have described physical therapy guidelines after hip arthroscopy since 2003.3,5,13,15-18 There has been limited discussion of outcomes using any of these rehabilitation protocols and limited evidence-based research behind treatment principles. In this postoperative period, it is important to follow general guidelines while individualizing the progression to align with the patient’s goals and expectations. This should be coupled with effective communication between the rehabilitation and surgical teams as to the specifics of the procedure performed, the patient’s preoperative status, any underlying comorbidities, and finally, the surgeon’s expectations for the patient.
Methods
Surgical Technique
The indications for surgery were predominantly labral tears with mechanical symptoms and failure of nonoperative treatment. Patient demographics can be found in Table 1.
Table 1.
Patient demographics
| Demographic | Mean | Range |
|---|---|---|
| Age, y | 38 | 13.1-76.3 |
| Sex, n (%) | ||
| Male | 228 (38.30) | |
| Female | 367 (61.70) | |
| Height, in | 67.5 | |
| Weight, lb | 166.86 | 100-350 |
| Body mass index, kg/m2 | 25.53 | 16.3-48.7 |
| Surgical side, n (%) | ||
| Right | 318 (54.45) | |
| Left | 277 (46.55) | |
| Procedure, % | ||
| Acetabuloplasty | 69.99 | |
| Femoroplasty | 65.9 | |
| Labral repair | 59.2 |
Bony lesions were corrected under fluoroscopic guidance. An acetabuloplasty was performed for pincer impingement and a femoral neck osteoplasty was performed for cam impingement. Each case with a crossover sign of 50% or greater was evaluated in the context of global over- or undercoverage and cam-type deformity. Performance of an acetabuloplasty was conducted on a case-by-case basis, taking into account acetabular and femoral structure, intra-articular damage, and ligamentous laxity. Labral tears were repaired when possible; otherwise, they were selectively debrided until a stable labrum was achieved while preserving as much labrum as possible. If the labrum was unrepairable, labral reconstruction was performed using either an autograft or an allograft gracilis hamstring tendon. Full-thickness cartilage damage was treated with debridement to create stable borders. Microfracture was performed in cases where bone was present after the bony decompression.17 Iliopsoas fractional lengthening was performed when patients had painful internal snapping and corresponding iliopsoas impingement lesion on the labrum. For trochanteric bursitis, lateral compartment endoscopy was performed with bursectomy and repair of gluteus medius tears, if necessary. Iliotibial band release was performed for those patients with painful external snapping documented on history and physical examination. Capsule closure or plication was performed unless contraindicated in cases such as preoperative decreased range of motion (ROM).8 Patients attended physical therapy starting postoperative day 1.
Principles of Rehabilitation Protocol
A preoperative program was initiated 1 month prior to the patients’ surgery. Patients were fitted with a hip brace that limits flexion beyond 90° and hip abduction beyond neutral, protecting the labral refixation, as well as neutral extension, which protects the capsular closure. Patents were instructed in proper gait mechanics and restrictions along with safe transfer techniques. Femoral and acetabular bony resection have the potential for disruption of the labral repair, making postoperative weightbearing restrictions essential. Patients were instructed to use 20 pounds of flat-foot weightbearing for 2 weeks after surgery to avoid stressing the femur or acetabulum postosteoplasty and to avoid stress to the repaired acetabular labrum. These weightbearing restrictions were used to avoid irritating the anterior hip by developing contractures of the hip flexor musculature and surgically repaired capsule. The 20-pound weight distribution was confirmed by the physical therapist. It was essential that the patient be compliant with flat-foot weightbearing in the early postoperative stage. Compliance with a home exercise program (HEP) was critical. On postoperative day 1, patients performed isometric contractions, including gluteus sets, quad sets, and transverse abdominis isometrics with diaphragmatic breathing (Figure 1). A specific, structured exercise progression was followed closely and reviewed at subsequent visits by the treating therapist (Table 2).
Figure 1.

Transverse abdominis isometrics.
Table 2.
Labral repair exercise progression
| Week | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | >12 | |
| Phase 1: Immediate rehabilitation (1-3 weeks) | |||||||||||||
| Short crank stationary bike: no resistance | × | × | × | × | |||||||||
| Quad sets | × | × | × | ||||||||||
| Gluteus sets | × | × | × | ||||||||||
| TA isometrics with diaphragmatic breathing | × | × | × | ||||||||||
| Prone lying | × | × | × | ||||||||||
| Prone glute squeeze with knee flexion | × | × | × | ||||||||||
| Supine heel slides | × | × | × | ||||||||||
| Quad rocking | × | × | |||||||||||
| Hooklying pelvic clock | × | × | × | × | |||||||||
| Hooklying with bent knee fall outs | × | × | × | × | |||||||||
| Hooklying marching | × | × | × | × | |||||||||
| Hooklying with hip abduction and adduction, isometric | × | × | × | × | |||||||||
| Passive circumduction | × | × | × | × | × | × | |||||||
| Passive IR log rolling | × | × | × | × | × | ||||||||
| Hip joint mobilizations Gr I, II caudal glides | × | × | |||||||||||
| Soft tissue mobilization- LS, glutes, HS, quad, hip flexor, adductors | × | × | × | × | × | × | × | × | × | × | × | × | |
| Phase 2: Intermediate rehabilitation (4-8 weeks) | |||||||||||||
| Supine double-leg bridge | × | × | × | ||||||||||
| Supine single-leg bridge | × | × | × | ||||||||||
| Prone IR/ER AROM | × | × | × | × | × | ||||||||
| Side-lying clams | × | × | × | × | × | × | |||||||
| ½ kneeling with shoulder flexion/rotation | × | × | × | × | |||||||||
| ½ kneeling with pelvic tilts | × | × | × | × | |||||||||
| Straight-leg raise hip abduction, extension | × | × | × | × | × | ||||||||
| Double-leg standing trunk rotation against band | × | × | × | × | × | × | × | ||||||
| Forward step-ups | × | × | × | × | × | × | |||||||
| Forward step-downs | × | × | × | × | × | × | × | ||||||
| Double-leg squat | × | × | × | × | × | × | |||||||
| Bike with resistance | × | × | × | × | × | × | × | × | |||||
| Double-leg balance board | × | × | × | × | |||||||||
| Hip joint mobilizations Gr III, IV, posterior, inferior | × | × | × | × | × | ||||||||
| Single-leg balance progression | × | × | × | × | × | ||||||||
| Single-leg squat | × | × | × | × | |||||||||
| Double → single-leg press | × | × | × | × | × | × | |||||||
| Elliptical | × | × | × | × | × | × | × | ||||||
| Phase 3: Advanced rehabilitation (9-12 weeks) | |||||||||||||
| 4-point alternate arm and leg extension | × | × | × | × | |||||||||
| Lunges all directions | × | × | × | × | |||||||||
| Lateral elastic band walk | × | × | × | × | |||||||||
| Monster walks with elastic band | × | × | × | × | |||||||||
| Single-leg squat on unstable surface | × | × | × | × | |||||||||
| Front and side plank progression | × | × | × | × | × | ||||||||
| Single-leg stance with rotation against band resistance | × | × | × | × | |||||||||
| Phase 4: Sport-specific training (>12 weeks) | |||||||||||||
| Return to run protocol | × | × | |||||||||||
| Cariocas | × | ||||||||||||
| Ladder drills (lateral, anterior, Z cuts) | × | ||||||||||||
| Return-to-play video testing | × | ||||||||||||
AROM, active range of motion; ER, external rotation; Gr, grade; HS, hamstring; IR, internal rotation; LS, lumbar spine; TA, transversus abdominus.
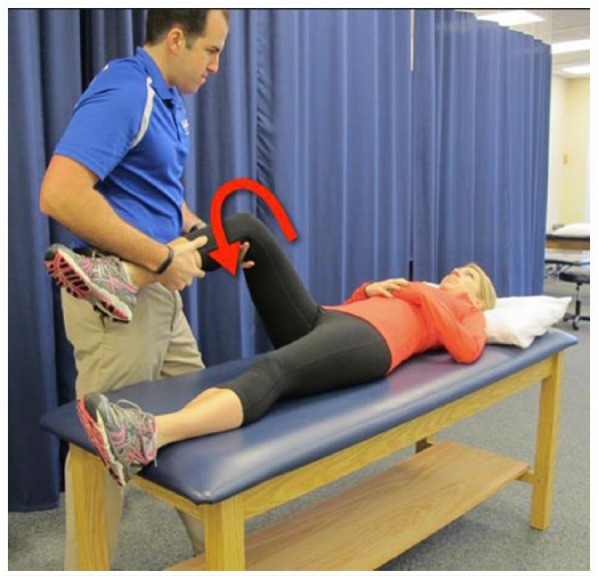
Phase 1
Postoperative care was initiated immediately on day 1 after surgery. Phase 1 lasts for 3 weeks. The goals of phase 1 are to diminish pain, protect the repaired tissues, and prevent muscle inhibition as well as the development of anterior hip contractures. The postoperative brace and crutches were used for 2 weeks immediately after surgery. After 2 weeks, the patient progressed to weightbearing as tolerated. Muscle weakness is expected during this stage; moderate quadriceps and gluteus muscle activation allows for successful transition to full weightbearing. Isometric exercises are continued in this phase (Figure 2), and passive range of motion (PROM) including circumduction (Figure 3) should be performed within restrictions (outlined below).
Figure 2.

Isometric with abduction ring.
Figure 3.
Circumduction.
PROM restrictions for weeks 1 through 3 are as follows:
Flexion 90°
Extension 0°
Abduction 25° to 30°
Internal rotation (IR) at 90° of hip flexion 0°
IR in prone limited by comfort
External rotation (ER) at 90° of hip flexion 30°
ER in prone position 20°
After 3 weeks, ROM progression is permitted within a pain-free range. Prior to the patients’ progression to phase II, full, nonpainful weightbearing must be achieved.
Phase 2
Phase 2 spans from week 4 through 8, with goals of continued protection of the repaired tissue, restoration of full hip ROM and normal gait patterns, and strengthening of the hip, pelvis, and both lower extremities with emphasis on the gluteus medius. Strengthening activities evolve from partial to full weightbearing positions, including leg press, double- followed by single-leg squats (Figure 4), and step-ups/downs. Double-leg standing with trunk rotation against elastic band resistance and standing shoulder extension against band resistance both help address core strength and stability. Patients progress to triplanar stepping, and balance progression begins with double- followed by single-leg stance activities. Elliptical trainer exercise can be initiated between 6 and 8 weeks postoperative for up to 10 minutes for cardiovascular endurance. To advance to phase 3 of the postoperative program, patients must demonstrate
Figure 4.
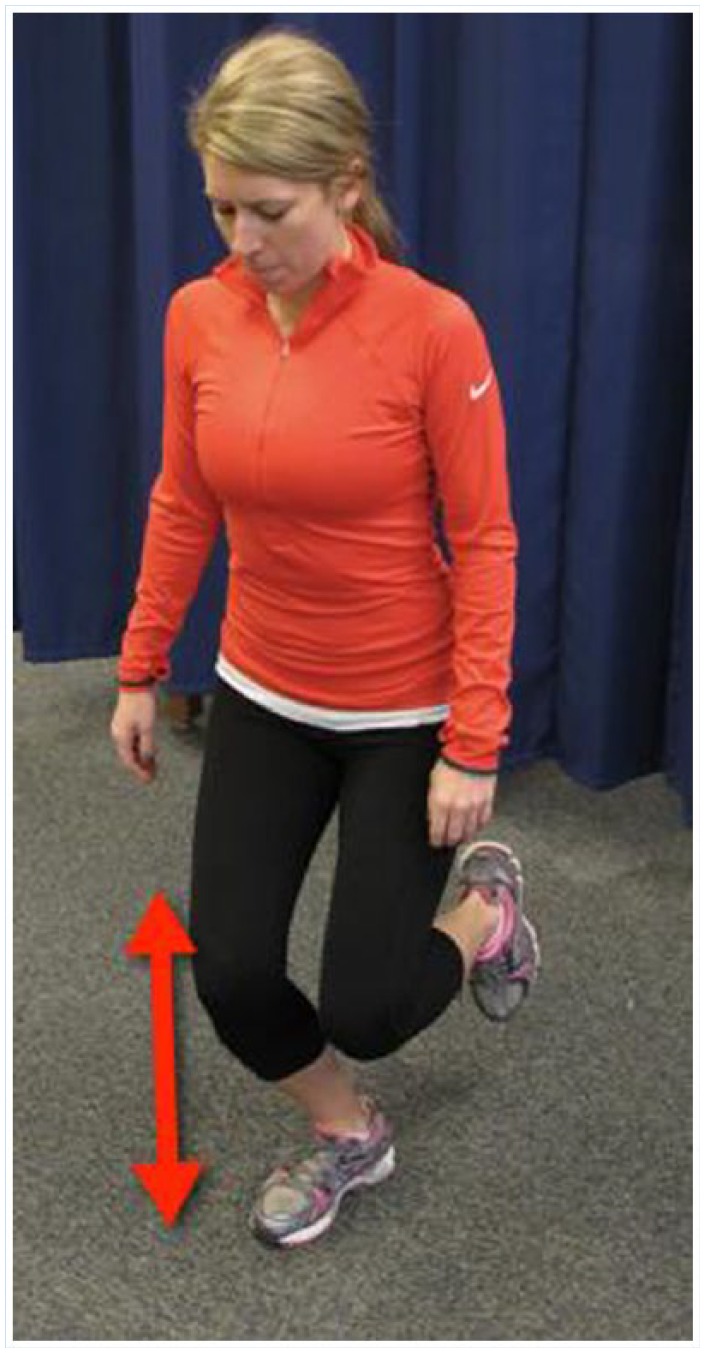
Single-leg squat.
Full and pain-free hip active range of motion (AROM) in all planes
Pain-free normalized gait
Hip flexor strength of 4− (of 5) on manual muscle testing
Hip abduction, adduction, extension, and IR/ER strength of 4 (of 5) on manual muscle testing
Phase 3 (Weeks 9-12)
The goals of phase 3 are the restoration of hip flexor muscle strength to 4 and 4+ (of 5) for all other hip motions, as well as improving balance, proprioception, and cardiovascular endurance. Precautions include avoidance of contact activities, aggressive hip flexor strengthening,4 as well as forced or aggressive stretching that elicits pain. Criteria for progression to sport-specific training includes hip flexor muscle strength of 4+ and 5 (of 5) in all other lower extremity musculature.
Phase 4 (>12 Weeks)
During phase 4, the athlete can begin a jogging progression program (Table 3) along with hopping and agility drills that are customized to the patient’s sport and/or work activities. Before return to play (RTP) is considered, full ROM to all planes of the hip and cardiovascular endurance consistent with sport and/or work demands must be demonstrated. Normal strength and flexibility throughout the core and lower extremities are needed to pass RTP testing. RTP testing uses slow-motion video analysis of biomechanical performance. During the Y-balance test, the athletes must achieve anterior reach within 4 cm in limb-to-limb comparison, and within a 6-cm limb-to-limb comparison on posteromedial and posterolateral reach tests. The athlete also must perform a single hop for distance, triple hop for distance, and triple crossover hop for distance with at least 90% limb symmetry. Stage 2 of RTP testing is a video analysis of a double-leg squat followed by single-leg squat off of an 18-inch box. In the double-leg squat, the athlete must not exhibit any lateral deviation of the hip/lower extremity away from the operative side. Passing the single-leg squat test requires no evidence of hip internal rotation or valgus, and the ipsilateral patella does not cross the plane of the great toe at the full depth of the squat. The final phase of RTP testing is a depth jump off of an 18-inch box, landing in a squat, and jumping straight up in 1 fluid motion finishing in a squat position and 15-foot lateral cone shuffles. Passing requires good hip and knee alignment at takeoff or landing and demonstration of good control during cone shuffles without hip internal rotation or valgus on the plant leg.
Table 3.
Jogging progression (initiated week 12 starting at stage 1)
| Stage | Walk, min | Jog, min | Repetitions | Total Time, min |
|---|---|---|---|---|
| 1 | 4 | 1 | 6 | 30 |
| 2 | 3 | 2 | 6 | 30 |
| 3 | 2 | 3 | 6 | 30 |
| 4 | 1 | 4 | 6 | 30 |
| 5 | 0 | 5 | 6 | 30 |
Results
Four patient-reported hip outcome scores were used to track progress during subsequent 2-year follow-up visits (Figure 5). Overall patient-reported satisfaction with surgery was 7.86, with a maximum score of 10 (Figure 6).
Figure 5.
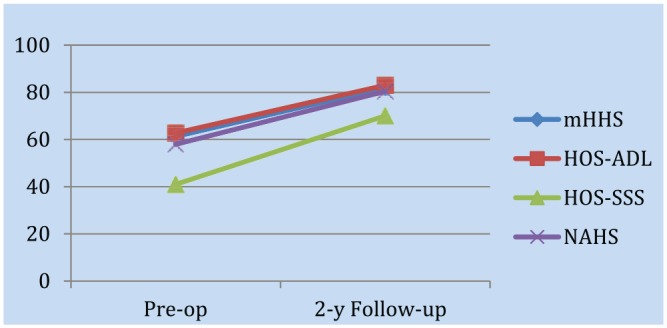
Outcome scores. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SSS, Hip Outcome Score–Sport-Specific Subscale; mHHS, modified Harris Hip score; NAHS, Non-Arthritic Hip Score.
Figure 6.
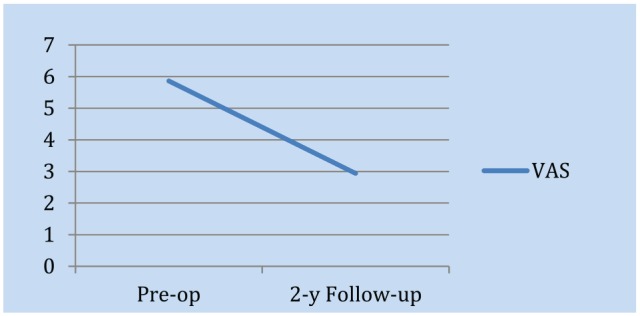
Pain visual analog scale (VAS).
Discussion
During the initial healing process, stress is minimized on both the labrum and the capsular repair. Strain on the anterior labrum can occur during provocative maneuvers of the normal hip, and anterior subluxation and anterior labral strain were observed when abduction and external rotation were combined in either moderate hip flexion or extension. A key consideration for safe progression of phase 1 (“immediate phase”) relates to the iliofemoral ligament and the impact of the anterior capsulotomy of the hip during the surgical procedure. Anterior capsulotomy increases visualization during surgery and is later closed with the iliofemoral ligament. The iliofemoral ligament resists hip extension and external rotation as well as prevents anterior translation of the femoral head when the hip is in neutral to extended positions.14 Labral lesions can occur during repetitive activities with hip flexion positions between 90° and 100°.1,7 In phase 1, ROM restrictions promote healing by avoiding excessive stress on the repaired labrum and capsule.
In phase 2, it is essential to reestablish a normal gait pattern as quickly as possible. Negative neuromuscular patterns or asymmetries developed from brace limitations and early ROM restrictions should be addressed immediately. Restoration of normal gait is directly related to reduction of pain and increased activity level.6 Gluteus medius strengthening, emphasized in phase 2, is essential as this muscle stabilizes the hip in both the frontal and transverse planes. If the hip lacks stability during single-leg weightbearing activities, the femur may adduct and internally rotate.10 This position can place excessive stress on the repaired soft tissue, and early activation of the gluteus medius is stressed to avoid this unsafe position. The exercises presented in phase 2 result in gluteus medius activation with low iliopsoas activation making them safe and effective in this stage of rehabilitation.14 Weightbearing exercises demonstrate significantly greater electromyographic activity than nonweightbearing hip abduction exercises.9 Excessive stretching and painful ROM will have the negative effects of irritating the repaired tissues and will ultimately slow the patients’ progression. Mild hip adductor soreness and hyperactivity is common due to hip abductor weakness, causing spasm and pain. This adductor muscle group has secondary joint actions of hip rotation and either flexion or extension depending on the position of the joint.11 In addition to facilitating these movements, the hip adductors play a role in stabilizing the hip and controlling alignment of the lower extremities.9
The postoperative rehabilitation protocol follows the guiding principle that range of motion and proximal muscular control must be established prior to progressing to distal dynamic strengthening. Early strengthening of the deep external rotators, including the quadratus femoris; obturator internus, externus, and gemelli; as well as the prime internal rotator, the gluteus minimus, is needed.15
If painful barriers or events do not resolve independently, immediate communication with the surgeon is necessary to avoid complications.
Single-leg squat exercises on an unstable surface elicit a high level of gluteus medius electromyographic activity.2 Only focusing on sagittal plane strengthening will limit the patient’s progression, especially when the patient’s goal is to return to sports that require lateral and rotational movements (eg, football, baseball, basketball, volleyball, lacrosse). After 12 weeks, the patient should be fully prepared to advance to sport-specific training. Return to play without restrictions can take between 6 and 9 months.12 Increased valgus knee motion is associated with decreased joint control in the coronal plane and may lead to increased risk of knee injury.6 It may be close to 1 year until the patient achieves maximum benefit and is able to play without any limitations.
Conclusion
Following a structured, criteria-based pre- and postoperative rehabilitation program that includes extensive collaboration and communication between the surgeon and rehabilitation team, patients undergoing hip arthroscopy can achieve excellent outcomes and return to full independent activities of daily living as well as sport.
Footnotes
The following author(s) declared potential conflicts of interest: Benjamin G. Domb, MD, is a paid consultant for MAKO Surgical, Arthrex, and Pacira; he has grants/grants pending from Arthrex, ATI, Breg, American Hip Institute, Pacira, and MAKO Surgical; holds patents for Hip Brace, LBR technique and kit; receives royalties from Orthomerica and DJO Global; and has stock/stock options from Stryker.
References
- 1. Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;(418):67-73. [PubMed] [Google Scholar]
- 2. Boren K, Conrey C, Le Coquic J, Paprocki L, Voight M, Robinson TK. Electromyographic analysis of gluteus medius and gluteus maximus during rehabilitation exercises. Int J Sports Phys Ther. 2011;6:206-223. [PMC free article] [PubMed] [Google Scholar]
- 3. Byrd JW. Femoroacetabular impingement in athletes: current concepts. Am J Sports Med. 2014;42:737-751. [DOI] [PubMed] [Google Scholar]
- 4. Dy CJ, Thompson MT, Crawford MJ, Alexander JW, McCarthy JC, Noble PC. Tensile strain in the anterior part of the acetabular labrum during provocative maneuvering of the normal hip. J Bone Joint Surg Am. 2008;90:1464-1472. [DOI] [PubMed] [Google Scholar]
- 5. Enseki KR, Martin RL, Draovitch P, Kelly BT, Philippon MJ, Schenker ML. The hip joint: arthroscopic procedures and postoperative rehabilitation. J Orthop Sports Phys Ther. 2006;36:516-525. [DOI] [PubMed] [Google Scholar]
- 6. Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35:1745-1750. [DOI] [PubMed] [Google Scholar]
- 7. Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112-120. [DOI] [PubMed] [Google Scholar]
- 8. Gupta A, Redmond JM, Stake CE, Dunne KF, Domb BG. Does primary hip arthroscopy result in improved clinical outcomes? 2-year clinical follow-up on a mixed group of 738 consecutive primary hip arthroscopies performed at a high-volume referral center. Am J Sports Med. 2016;44:74-82. [DOI] [PubMed] [Google Scholar]
- 9. Hrysomallis C. Hip adductors’ strength, flexibility, and injury risk. J Strength Cond Res. 2009;23:1514-1517. [DOI] [PubMed] [Google Scholar]
- 10. Krause DA, Jacobs PS, Pilger KE, Sather BR, Sibunka SP, Hollman JH. Electromyographic analysis of the gluteus medius in five weight-bearing exercises. J Strength Cond Res. 2009;23:2689-2694. [DOI] [PubMed] [Google Scholar]
- 11. Leighton RD. A functional model to describe the action of the adductor muscles at the hip in the transverse plane. Physiother Theory Pract. 2006;22:251-262. [DOI] [PubMed] [Google Scholar]
- 12. Lynch TS, Terra MA, Bedi A, Kelly BT. Hip arthroscopic surgery: patient evaluation, current indications, and outcomes. Am J Sports Med. 2013;41:1174-1189. [DOI] [PubMed] [Google Scholar]
- 13. Malloy P, Malloy M, Draovitch P. Guidelines and pitfalls for the rehabilitation following hip arthroscopy. Curr Rev Musculoskelet Med. 2013;6:235-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Martin HD, Savage A, Braly BA, Palmer IJ, Beall DP, Kelly B. The function of the hip capsular ligaments: a quantitative report. Arthroscopy. 2008;24:188-195. [DOI] [PubMed] [Google Scholar]
- 15. Spencer-Gardner L, Eischen JJ, Levy BA, Sierra RJ, Engasser WM, Krych AJ. A comprehensive five-phase rehabilitation programme after hip arthroscopy for femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2014;22:848-859. [DOI] [PubMed] [Google Scholar]
- 16. Stalzer S, Wahoff M, Scanlan M. Rehabilitation following hip arthroscopy. Clin Sports Med. 2006;25:337-357. [DOI] [PubMed] [Google Scholar]
- 17. Voight ML, Robinson K, Gill L, Griffin K. Postoperative rehabilitation guidelines for hip arthroscopy in an active population. Sports Health. 2010;2:222-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wahoff M, Ryan M. Rehabilitation after hip femoroacetabular impingement arthroscopy. Clin Sports Med. 2011;30:463-482. [DOI] [PubMed] [Google Scholar]