Abstract
Background:
Tennis elbow is commonly encountered by physicians, yet little is known about the cost of treating this condition.
Hypothesis:
The largest cost associated with treating tennis elbow is procedural intervention.
Study Design:
Descriptive epidemiology study.
Level of Evidence:
Level 4.
Methods:
This retrospective population-based study reviewed patients who were treated for new-onset tennis elbow between January 1, 2003 and December 31, 2012. All patients were followed up through their medical and administrative records to identify health care encounters and interventions for tennis elbow. Unit costs for each health service/procedure were adjusted to nationally representative unit costs in 2013 inflation-adjusted dollars.
Results:
In a cohort of 931 patients who had 2 or more clinical encounters for new-onset lateral epicondylosis during a 12-month period after initial diagnosis, 62% received a median of 3 physical therapy sessions (cost, $100/session) and 40% received a median of 1 steroid injection (cost, $82/injection). Only 4% of patients received surgical intervention with mean costs of $4000. The mean (median) total direct medical cost of services related to lateral epicondylosis for the entire cohort was $660 ($402) per patient over the 1-year period after diagnosis. Patients who continued to be treated conservatively between 6 and 12 months after diagnosis incurred relatively low median costs of $168 per patient.
Conclusion:
In this cohort, a second encounter with a physician for tennis elbow was a strong predictor of increased treatment cost due to a higher likelihood of specialist referral, use of physical therapy, or treatment with steroid injection.
Clinical Relevance:
The majority of direct medical spending on tennis elbow occurs within the first 6 months of treatment, and relatively little expense occurs between 6 and 12 months after diagnosis unless a patient undergoes surgical intervention.
Keywords: lateral epicondylitis, lateral elbow tendinosis, tennis elbow, cost
Lateral epicondylosis (epicondylitis), commonly referred to as tennis elbow, is a frequently encountered condition among primary care and specialty physicians with an incidence of 3.4 per 1000 individuals.4 A variety of therapeutic interventions have been described, including bracing, physical therapy, steroid injections, ultrasound treatment, and surgical debridement. Despite a significant number of publications addressing the diagnostic and treatment aspects of this condition, little is known regarding health care utilization and treatment costs. In a randomized trial of 180 patients, Struijs et al8 compared the cost effectiveness of bracing and physical therapy alone with using these 2 modalities in conjunction. Physical therapy alone appeared to have the least overall cost primarily due to lower indirect costs (eg, lost wages) in this group. The total cost difference was driven by higher indirect costs in the bracing group. In contrast, another trial comparing observation alone, physical therapy, and steroid injection showed no difference in total cost over 12 months of follow-up.1
However, the treatment of lateral epicondylosis is more complex and should account for other associated services not included in these studies, such as radiologic and procedural interventions. Patients with symptoms lasting longer than 6 months experience a prolonged disease course and may benefit from earlier procedural intervention,4 which could potentially lead to reduced direct or indirect costs. Therefore, the goals of this study were to describe health care utilization and direct medical costs of selected services associated with the management of lateral epicondylosis during the 1-year period after disease onset.
Methods
This was a population-based study conducted in Olmsted County, Minnesota, which has a population of 144,260 according to the 2010 census. As described previously,4 the Rochester Epidemiology Project (REP) resources were used to identify a cohort of all Olmsted County residents first diagnosed with lateral epicondylosis between January 1, 2003 and December 31, 2012. The utility of the REP for population-based epidemiologic and cost studies has been previously described.3,5-7
A total of 3166 residents of Olmsted County were identified who had International Classification of Diseases–Ninth Revision (ICD-9) diagnosis codes consistent with lateral epicondylosis between January 1, 2003 and December 31, 2012. Selected procedures of interest for the entire cohort of patients were identified using the ICD-9 procedure codes and Current Procedural Terminology (CPT) billing codes within 1 year of diagnosis.
Health care utilization and cost data during the 12-month time window after diagnosis of lateral epicondylosis were obtained from an institutional research database called the Olmsted County Healthcare Expenditure and Utilization Database (OCHEUD). Recognizing the discrepancies between billed charges and true resource use, widely accepted bottom-up microcosting valuation techniques were employed to generate standardized inflation-adjusted estimates of the costs of each service or procedure in constant dollars.2 In this population, patients could access a specialist provider without first being evaluated by a primary care provider. However, information on type of provider (primary care vs specialist) was available for visits at Mayo Clinic, and this information was used in subsequent analyses.
Lateral epicondylosis–related services were identified using the ICD-9 diagnosis code (726.32). The services identified included: physician office visits, steroid injections (including the cost of the medications and the surgical trays), physical therapy, radiographs, magnetic resonance imaging (MRI), and surgical treatment. The appendix (available at http://sph.sagepub.com/content/by/supplemental-data) provides a full list of ICD and CPT codes used for identification of services provided. The medical records of all subjects who underwent surgery were reviewed manually to verify the accuracy of the codes and whether the procedure was open or arthroscopic debridement. Descriptive statistics were used to summarize demographics, utilization of selected services, and costs.
For simplicity, this study will estimate the cost of a hypothetical cohort of 100 patients with at least 2 physician encounters for tennis elbow. The cost per service and mean number of services used per patient will be based on the utilization data from all patients in Olmsted County with at least 2 physician encounters. This study was conducted after institutional review board approval was obtained from Mayo Clinic (13-006875) and Olmsted Medical Center (042-OMC-13).
Results
The study population consisted of 3166 patients with a mean age of 47 ± 11 years, and 58% were female. The vast majority of patients had only 1 encounter for lateral epicondylosis (n = 2235, 71%), whereas 931 (29%) patients had 2 or more encounters. A total of 33 patients underwent surgery within the first year of their diagnosis.
Health care utilization and unit costs (ie, costs per encounter) were analyzed separately for the entire population of 3166 patients and the subset of 931 patients with 2 or more health care encounters for tennis elbow (Table 1). Most patients were treated with an open surgical technique. Fourteen patients had surgery within 6 months of diagnosis, and 19 patients had surgery between 6 and 12 months after diagnosis. The direct medical costs of open and arthroscopic surgery were similar.
Table 1.
Utilization and costs of selected services by lateral epicondylosis patients during the 12-month period after disease onset
| Utilization Category | Patients With at Least 1 Encounter |
Patients With 2 or More Encounters |
||||
|---|---|---|---|---|---|---|
| n (%) (n = 3166) | Median (Min, Max) Number During 12 Months | Mean/Median Cost per Unit Encounter, $ | n (%) (n = 931) | Median (Min, Max) Number During 12 Months | Mean/Median Cost per Unit Encounter, $ | |
| Office visit | 3166 (100) | 1 (1, 24) | 85/73 | 931 (100) | 3 (2, 24) | 86/81 |
| Specialist visit | 776 (36) a | 1 (1,18) | 100/98 | 439 (71) a | 2 (1,18) | 96/90 |
| Physical therapy | 698 (33) a | 2 (1, 32) | 103/94 | 385 (62) a | 3 (1, 32) | 100/83 |
| Steroid injection (without E&M) | 538 (17) | 1 (1, 5) | 78/68 | 374 (40) | 1 (1, 5) | 82/71 |
| Radiograph | 258 (8) | 1 (1, 4) | 34/34 | 151 (16) | 1 (1, 4) | 33/33 |
| MRI | 46 (1.5) | 1 (1, 2) | 572/582 | 35 (4%) | 1 (1, 2) | 572/582 |
| Surgical procedure | 33 (1) | — | 3553/3875 b | 33 (4) | — | 3553/3875 b |
| Open | 18/33 (55) | — | 4143/3787 | 18/33 (55) | — | 4143/3787 |
| Arthroscopic | 10/33 (30) | — | 3961/3938 | 10/33 (30) | — | 3961/3938 |
| Percutaneous tenotomy | 5/33 (15) | — | 611/665 | 5/33 (15) | — | 611/665 |
E&M, evaluation and management; max, maximum; min, minimum; MRI, magnetic resonance imaging.
Information on specialist and physical therapy visits are limited to those that occurred at 1 institution (Mayo Clinic). Therefore, percentages are calculated based on 2146 patients who had at least 1 Mayo Clinic encounter and 615 patients who had 2 or more encounters at the Mayo Clinic (both primary care and specialty visits).
Mean/median costs on the day of surgery.
We also examined the health care utilization and costs of 258 patients with symptom duration of at least 6 months (Table 2). In this group, 7% of patients underwent a procedural intervention (surgical debridement or percutaneous tenotomy) during the 6- to 12-month period after diagnosis. The median total cost per patient during the entire 6- to 12-month period was $168 for patients treated conservatively and $1536 for patients treated procedurally (surgery or percutaneous tenotomy).
Table 2.
Median direct medical cost (interquartile range) of 258 lateral epicondylosis patients with symptom duration beyond 6 months a
| Conservative Management (n = 239), $ | Procedural Management (Surgery or Percutaneous Tenotomy) (n = 19), $ | |
|---|---|---|
| Total costs per patient during 6- to 12-month period | 168 (103, 429) | 1536 (598, 2194) |
| Office visits and physical therapy | 115 (64, 294) | 228 (80, 923) |
| Steroid injections | 68 (63, 107) | 77 (60, 106) |
Costs are limited to the 6- to 12-month period.
The relative proportion of direct medical costs associated with treating tennis elbow is estimated in a hypothetical cohort of 100 patients based on the utilization patterns (Figure 1, Table 1) and is representative of patients with 2 or more physician visits for tennis elbow. The estimated annual direct medical cost of treating this cohort would be $80,144. In this cohort, only 4 patients would be treated surgically but would account for 20% of medical spending ($16,000). However, the largest expense would be office visits ($25,800) and specialty visits ($13,632), as nearly three-quarters of all patients would have seen a specialist twice. Physical therapy would account for 23% of spending ($18,600), as nearly two-thirds of patients would be seen 3 times by a therapist. Radiographic ($2832) and injection ($3280) costs would account for a much smaller portion of direct medical spending.
Figure 1.
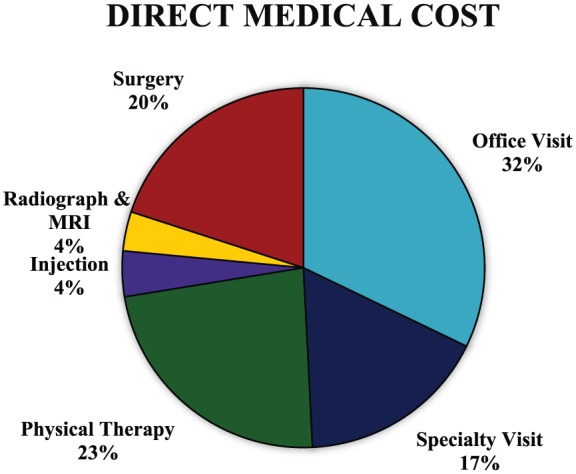
Percentage of annual direct medical costs of treating tennis elbow in a hypothetical cohort of 100 patients with at least 2 clinical encounters by service provided. MRI, magnetic resonance imaging.
Discussion
In this cohort, physical therapy was used more often than steroid injections and represented a substantially higher portion of the direct medical costs. Perhaps this trend reflects the recognition of lateral epicondylosis as a disease of chronic tendinopathy rather than an acute inflammatory process for which physical therapy and eccentric exercise might be the more effective intervention. While enhanced imaging of this condition can increase individual costs, at our institution, radiographic costs represent a small portion of spending on tennis elbow given the few patients who use this modality.
When evaluating patients with symptom duration between 6 and 12 months, 7% of patients were treated procedurally and constituted the vast majority of the direct medical costs. Patients treated conservatively between 6 and 12 months of the disease course accrued relatively little medical cost, and only 25% of their direct medical expenses occurred during this period. The lower costs may reflect symptom resolution or fewer clinical encounters as patients transitioned to home-based physical therapy regimens. Previously, symptom duration persisting beyond 6 months of diagnosis was associated with a prolonged disease course.4 However, current data indicate that for the majority of patients, this does not result in substantially higher direct medical cost within 1 year of diagnosis. This might indicate that using 6 months of symptom duration as a timeline to offer procedural intervention may not provide a direct medical cost savings benefit within the first year of diagnosis.
These findings should be interpreted in light of some limitations. First, these data reflect clinically recognized diagnoses and do not take into account self-diagnosed/treated patients who did not seek medical attention. In addition, the majority of data presented in this study are based on diagnostic and procedural codes and were not confirmed with chart review, thus making it susceptible to measurement error. Additionally, different treatment patterns of tennis elbow (such as timing of introducing physical therapy or injections) could not be accounted for and likely introduce treatment bias. Additionally, treatment with home therapy programs could result in substantial cost differences and was not accounted for. This study did not capture the costs of other treatment modalities such as braces, anti-inflammatory medications, or platelet-rich plasma injections. Similarly, this study did not evaluate percutaneous treatment options that can be used in the outpatient clinical setting and can thus dramatically influence cost of treatment. Additionally, the data presented in this study reflect the true cost of treating tennis elbow by providers in Olmsted County, Minnesota, and not the charges billed directly to patients or insurance companies and may not be representative of costs in all regions of the United States as indications and treatment protocols are not standardized within the profession. This is especially noted in the relatively limited use of MRI and cortisone injections in our patient cohort.
The indirect costs (missed work, loss of productivity, etc) of treating tennis elbow can add significantly to the societal burden of treating this condition. Sixteen percent of patients with tennis elbow reported work restrictions, and 4% reported missing at least 1 week of work.4 Using the human capital approach, this would correspond to about $800 lost per week for a worker with an annual salary of $40,000 (40 hours × $20) or significantly greater for employees with a higher annual salary. Therefore, the indirect costs of tennis elbow can add significantly to the societal financial burden of treating this condition and could potentially prompt earlier surgical intervention in an attempt to restore a patient’s ability to work.
Conclusion
Lateral epicondylosis remains a commonly encountered condition, and the majority of direct medical spending occurs within the first 6 months of diagnosis. Among patients seen 2 or more times by a provider, surgical intervention is used in only 4% of patients but represents 20% of spending. Although a 6-month timeline for procedural intervention can shorten the disease course for some patients and restore patient productivity, relatively little additional direct medical spending occurs beyond 6 months of diagnosis unless the patient undergoes surgical intervention.
Supplementary Material
Footnotes
The following author declared potential conflicts of interest: Bernard F. Morrey, MD, is a paid consultant for Tenex Health. This study was made possible by the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under award number R01AG034676. The findings and conclusions of this report are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
References
- 1. Korthals-de Bos I, Smidt N, van Tulder M, et al. Cost effectiveness of interventions for lateral epicondylitis: results from a randomised controlled trial in primary care. Pharmacoeconomics. 2004;22:185-195. [DOI] [PubMed] [Google Scholar]
- 2. Maradit Kremers H, Visscher S, Moriarty J, et al. Determinants of direct medical costs in primary and revision total knee arthroplasty. Clin Orthop Relat Res. 2013;471:206-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rocca W, Yawn B, St Sauver J, Grossardt B, Melton L. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87:1202-1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sanders T, Maradit Kremers H, Bryan A, Ransom J, Smith J, Morrey B. The epidemiology and healthcare burden of tennis elbow: a population based study. Am J Sports Med. 2015;43:1066-1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. St Sauver J, Grossardt B, Leibson C, Yawn B, Melton L, Rocca W. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87:151-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. St Sauver J, Grossardt B, Yawn B, et al. Data resource profile: The Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012;41:1614-1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. St Sauver J, Grossardt B, Yawn B, Melton L, Rocca W. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester Epidemiology Project. Am J Epidemiol. 2011;173:1059-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Struijs P, Korthals-de Bos I, van Tulder M, van Dijk C, Bouter L, Assendelft W. Cost effectiveness of brace, physiotherapy, or both for treatment of tennis elbow. Br J Sports Med. 2006;40:637-643. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


