Abstract
Context:
Shoulder dislocations are common in contact sports, yet guidelines regarding the best treatment strategy and time to return to play have not been clearly defined.
Evidence Acquisition:
Electronic databases, including PubMed, MEDLINE, and Embase, were reviewed for the years 1980 through 2015.
Study Design:
Clinical review.
Level of Evidence:
Level 4.
Results:
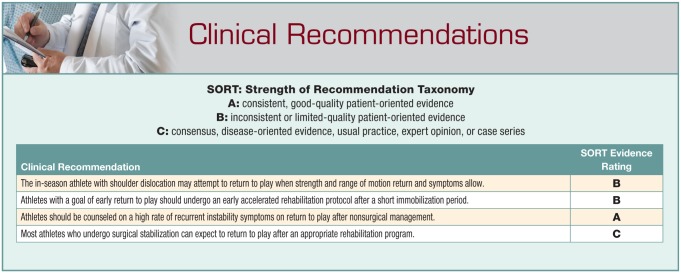
Much has been published about return to play after anterior shoulder dislocation, but almost all is derived from expert opinion and clinical experience rather than from well-designed studies. Recommendations vary and differ depending on age, sex, type of sport, position of the athlete, time in the sport’s season, and associated pathology. Despite a lack of consensus and specific recommendations, there is agreement that before being allowed to return to sport, athletes should be pain free and demonstrate symmetric shoulder and bilateral scapular strength, with functional range of motion that allows sport-specific participation. Return to play usually occurs 2 to 3 weeks from the time of injury. Athletes with in-season shoulder instability returning to sport have demonstrated recurrence rates ranging from 37% to 90%. Increased bone loss, recurrent instability, and injury occurring near the end of season are all indications that may push surgeons and athletes toward earlier surgical intervention.
Conclusion:
Most athletes are able to return to play within 2 to 3 weeks but there is a high risk of recurrent instability.
Keywords: return to play, shoulder instability, sports
Glenohumeral instability is a common injury in young athletes.20 This diagnosis ranges from microinstability to frank dislocation requiring manual reduction. A recent review of the National Collegiate Athletic Association (NCAA) Injury Surveillance system for years 1989 to 2004 reported 4080 glenohumeral instability events across various sports, equating to an injury rate of 0.12 per 1000 athlete-exposures.20 Not surprisingly, the greatest rates occurred in contact sports (football, hockey, wrestling).20 The vast majority of injuries were caused by contact with another player resulting in anterior instability.22 Typically, the arm is abducted and externally rotated and the excessive forceful rotation causes the humeral head to dislocate anteriorly and inferiorly, avulsing the labrum, inferior glenohumeral ligament (IGHL), and capsular complex from the glenoid.23,31 In addition to labral and capsular injury, impaction fractures of the anterior glenoid rim and posterolateral humeral head (Hill-Sachs lesions) also can occur, which further compromise shoulder joint stability. In-season athletes miss a variable amount of competition time after a shoulder dislocation. No consensus exists on the ideal in-season treatment of this injury or timing of return to play. This review provides a summary of the current evidence and highlights areas for future studies to guide the practitioner in caring for the in-season athlete with anterior shoulder instability.
Evaluation
The initial evaluation after shoulder dislocation should begin with a thorough history and physical examination. The athlete may describe a specific episode and mechanism of injury (contact or noncontact) or report feelings of recurrent looseness, shifting, or frank instability. Acute presentation of an anterior shoulder dislocation generally reveals the arm held in a position of adduction and internal rotation, a palpable prominence of the humeral head anterior and inferior, with a visible and palpable defect or sulcus over the posterior shoulder. After reduction, active and passive range of motion should be assessed along with a detailed neurovascular examination, especially evaluating the function of the axillary nerve. Radiographic workup requires at least an anteroposterior and axillary (or West Point) view to document concentric reduction as well as rule out fracture or significant bony involvement. A computed tomography (CT) scan may be indicated in recurrent dislocations or to evaluate the amount of bone loss in the first-time dislocator with a bony Bankart. Magnetic resonance imaging performed acutely can be useful to diagnose a Bankart lesion or humeral avulsion of the glenohumeral ligaments (HAGL) as hemarthrosis improves the visualization of those ligamentous and labral structures. Magnetic resonance imaging, however, is not always necessary in patients with a classic history and physical examination findings. Taylor and Arciero31 found a 97% incidence of Bankart lesions and 90% incidence of Hill-Sachs lesions in young athletes with a first-time dislocation.
Initial Treatment
There is insufficient evidence to reach consensus on nonoperative management after an anterior dislocation in terms of immobilization position, duration, and therapy.11 Recommendations range from no immobilization to sling immobilization in internal versus external rotation for 1 to 6 weeks.14,15,18,32 Marans et al18 revealed a 100% recurrent dislocation rate in adolescents treated with sling immobilization for up to 6 weeks. In contrast, Buss et al6 showed an 86% return-to-sport rate with no sling immobilization after the initial dislocation in a group of competitive high school and collegiate athletes. Although the duration of immobilization remains controversial, most treatment regimens aimed at rapid return to competition recommend a short period (3-10 days) of immobilization in a simple sling.21 A phased physical therapy protocol can be effective. This protocol progresses through cryotherapy and regaining painless motion, strengthening of the rotator cuff and periscapular muscles, shoulder stabilization drills, and then sport-specific drills.3,5,8 The first few days postinjury consist of simple sling use, gentle range of motion exercises, and cryotherapy. Week 2 involves strengthening the dynamic stabilizers, including the rotator cuff, as well as periscapular strengthening exercises. When range of motion and strength are similar to the contralateral side, sport-specific drills are initiated and return to play with a brace is considered.21 Typically, the time frame for return to play is approximately 3 weeks, but this can be accelerated based on individual circumstances.5
Recurrence
Multiple studies have demonstrated that shoulder instability recurrence depends primarily on the patient’s age and activity level. Young male athletes are at greatest risk of sustaining an initial glenohumeral instability injury35 and of developing recurrent instability.13,29 Sachs et al30 demonstrated that young age (<25 years) was a risk factor for recurrent shoulder dislocation, and this is supported by a study of athletes from the United States Military Academy that documented a 92% recurrence rate in young athletes.33 Hovelius et al13 reported a recurrence rate of 27% in patients older than 30 years but a 72% recurrence rate in those younger than 23 years, which makes up the large majority of the athletic population that a sports medicine team will encounter. More recently, Dickens et al9 reported recurrent instability in 64% of NCAA athletes who returned to sport in-season.
While there is a large volume of published data reporting the rates of recurrent instability in contact, collision, and overhead athletes after surgical stabilization, there is less available on those treated without surgery. Using data published in tables 1 and 3 of the NCAA injury database study by Owens et al,20 the incidence rates of recurrent instability in the reported sports were calculated. Male contact/collision sports (football, hockey, lacrosse, wrestling) had recurrent instability incidence rates of 0.05 to 0.18 per 1000 athlete-exposures (AEs), which were higher than the rates for basketball, baseball, and soccer (each at 0.03/1000 AEs). Women’s contact, overhead, and other sports all had incidence rates of 0.01 to 0.06 per 1000 AEs for recurrent instability.20 Unfortunately, in these data, it is not possible to identify how many of these instability recurrences occurred in athletes who had undergone surgical stabilization prior to their recurrent event. In the study of nonsurgically managed patients by Sachs et al,30 the rate of recurrent instability was higher for both contact sport participants (55% contact, 38% no contact) and those who “used the arm at or above chest level in their occupation” (51% above chest level, 28% not above chest level). The use of the label “occupation” suggests this was not a purely athletic group. Neither of these differences, however, were significant in the multivariate logistic regression analysis. On the basis of these 2 studies, there is a suggestion that contact and overhead sports may be related to an increased risk of recurrent shoulder instability, but further research is required to clarify these relationships before any definitive conclusions can be made.
The physician and sports medicine team should counsel the athlete that the risk of recurrent instability is high, although shoulder dislocation does not necessarily prevent the athlete from returning to play during the season. With recurrence, an increasing number of dislocations are associated not only with an increasing amount of glenoid bone loss but also the odds of having a critical level of bone loss (>20%).19 The long-term prevalence of instability-related arthropathy depends on the length of follow-up but has been noted to be from 28% to 67% after Bankart repair. Age at initial dislocation has been identified as a risk factor, while there is a lack of consensus regarding the effect of the number of presurgery dislocations on the development of OA in these patients.25-27
Return to Play
Very few clinical studies have been conducted to evaluate return to play for athletes with anterior shoulder instability. With exception to the data provided by Wheeler et al,33 Buss et al,6 and Dickens et al,9 most recommendations are based on expert opinion and anecdotal experience. There is no consensus on treatment or timing to return to play. Buss et al6 found that athletes undergoing nonoperative treatment for shoulder instability episodes missed an average of 10.2 days (range, 0-30 days) of sports participation, with 27 of 30 athletes returning to play within 2 to 3 weeks. Thirty-seven percent of these athletes experienced at least 1 instability episode during return to competition that season, but only 1 was unable to complete the season.
In a recent prospective study, Dickens et al9 found that 73% of NCAA athletes were able to return to sport after an instability episode and did so at a median of 5 days after injury. Of those who returned, 36% did not have a recurrence, 30% had a recurrence but could complete the season, and 33% had a recurrence and were not able to complete the season. They found that athletes who initially sustained a subluxation were 5.3 times more likely to return to sport than those with a dislocation. Those with recurrent subluxations returned to play sooner (median, 3 days) than those with dislocations (median, 7 days), but there was much greater variability in the time to return to play for recurrent dislocations. The Simple Shoulder Test score at the time of injury was linearly related to the time to return to play.9
There is no consensus on the criteria that should allow an athlete to return to sport. As a general practice, concurrent with most studies, athletes are allowed to return to play when they can demonstrate symmetric range of motion and strength and perform sport-specific exercises without pain and limitations.6,9,33 It is common practice, especially in contact and nonoverhead throwing athletes, to return to play wearing a shoulder stabilization brace to limit overhead motion and extreme abduction and external rotation.5,6,9 Buss et al6 reported that the athletes in their series who wore a brace on return to sport “reported an improved sense of stability compared to playing without a supplemental device.” Although bracing is common practice and associated with subjective improvement in stability, the only study to evaluate the effectiveness of bracing in preventing a recurrence found no difference in recurrent instability events in competitive, contact athletes with and without a brace.9 The study neither delineated the specific sport of each athlete, nor did it state whether they were first-time dislocators or repeat dislocators. Further studies modeled to evaluate the effectiveness of bracing are needed to help determine the value of bracing.
Surgical Treatment
The decision to proceed with surgical stabilization in the athlete depends on many factors and is typically undertaken after a failed course of nonsurgical management. Timing to surgical procedure has great variability depending on the extent of the injury, recurrences, age of the athlete, mechanisms, point in the season, and the athlete’s symptoms, sport, position, and future plans. Burkhead and Rockwood4 reported that only 16% of young patients with traumatic anterior instability had a good or excellent outcome after nonoperative treatment. The recurrence rate in athletes younger than 30 years who do elect nonsurgical management is 3 times higher than the rate in those having surgical repair.16,17 Nonsurgical management results in significantly lower overall shoulder-specific quality of life and significantly greater difficulty participating and performing in their sport of choice.16 Recurrent instability events, especially with lower energy mechanisms, and inability to perform sport-specific activities are indications for early surgical management. The relative and absolute indications for early surgery have been previously summarized (Table 1).21 In 1 of the few studies to report on in-season return to play, Buss et al6 reported 46% of the athletes who returned to sport underwent surgical stabilization at the conclusion of their season. There is a limited amount of evidence available to draw a conclusion on timing of surgery and whether return to play during the season affects outcomes.
Table 1.
Absolute and relative indications for early surgery a
| Absolute Associated injury >50% rotator cuff tear Glenoid osseous defect >25% Humeral head articular surface osseous defect >25% Proximal humerus fracture requiring surgery Irreducible dislocation Interposed tissue or nonconcentric reduction Failed trial of rehabilitation Inability to tolerate shoulder restrictions Inability to perform sport-specific drills without instability |
| Relative >2 shoulder dislocations during the season Overhead or throwing athletes Contact sport athletes Injury near the end of the season Age <20 years |
Reprinted with permission from Owens et al.21
There is currently no consensus on the superiority of arthroscopic versus open surgical intervention. Arthroscopic techniques for the treatment of anterior shoulder instability have improved substantially due to the development of new implants and instrumentation, greater surgeon experience, and increased comfort with arthroscopy. Arthroscopic techniques that preserve the subscapularis and are associated with less loss of external rotation have become more popular in recent years, despite historical recurrence rates being more favorable with open procedures (5%-9% vs arthroscopic 5%-33%).10,21 A 2013 meta-analysis found no significant difference in clinical outcomes or instability between arthroscopic and open procedures (11% vs 8%).12 Balg and Boileau1 reported on 131 patients in whom 14.5% had recurrent instability at a mean 17 months after arthroscopic Bankart repair. They identified the following as risk factors for recurrence: age less than 20 years at the time of surgery, involvement in competitive/contact sports or those involving forced overhead activity, shoulder hyperlaxity, Hill-Sachs lesion present on an anteroposterior radiograph of the shoulder in external rotation, and/or loss of the sclerotic inferior glenoid contour. The decision to proceed with an open or arthroscopic surgery depends on associated risk factors, the extent of bony involvement, and surgeon preference.21 The superiority of the open versus arthroscopic approach will continue to be a topic of discussion among orthopaedic surgeons and is beyond the scope of this review.
Return to Play after Surgery
Myriad protocols and guidelines have evolved to allow a timely return to sport after the various types of shoulder stabilization surgeries. Despite differences in surgical techniques, there are some general principles to consider in the rehabilitation process. Many of the principles used to guide return to sports after nonoperative treatment also apply to athletes attempting to return to their sport after surgical stabilization. Typically, the time range for return to play after surgery is 4 to 6 months,2,24 but it may be longer in some cases.
While the specifics of the rehabilitation protocol may vary among surgeons, athletes will generally follow a progressive, multiphase supervised physical therapy rehabilitation program.2,7,24,34 The first phase consists of sling immobilization in internal rotation for at least 4 weeks, Codman exercises,34 and isometric muscle contractions. The next phase, lasting approximately 4 weeks, consists of progressive passive range of motion followed by active-assisted range of motion exercises without resistance (limited to 45° external rotation). The third, approximately 4-week phase focuses on restoration of full active range of motion with progressively greater resistance exercises (deltoid, periscapular muscles, and rotator cuff). After this, plyometric exercises are added and the remaining rehabilitation aims to restore terminal external rotation, proprioceptive feedback, and sport-specific motion. Return to full activity sports is restricted until at least 4 months and after abduction and external rotation strength are symmetrical on manual muscle testing.2,24 In a study of 58 high school, collegiate, and professional American football players treated with open shoulder stabilization, Pagnani and Dome24 found that 89.7% were able to return to playing football for at least 1 year. Recently, Plath et al28 reported on return to sport of athletes across a variety of sports after arthroscopic Bankart repair for chronic glenohumeral instability. All 57 patients were able to return to at least 1 sporting or recreational activity after surgery, with 66% stating that the repair had strongly (33%) improved their sporting and recreational “proficiency” compared with preoperatively.28
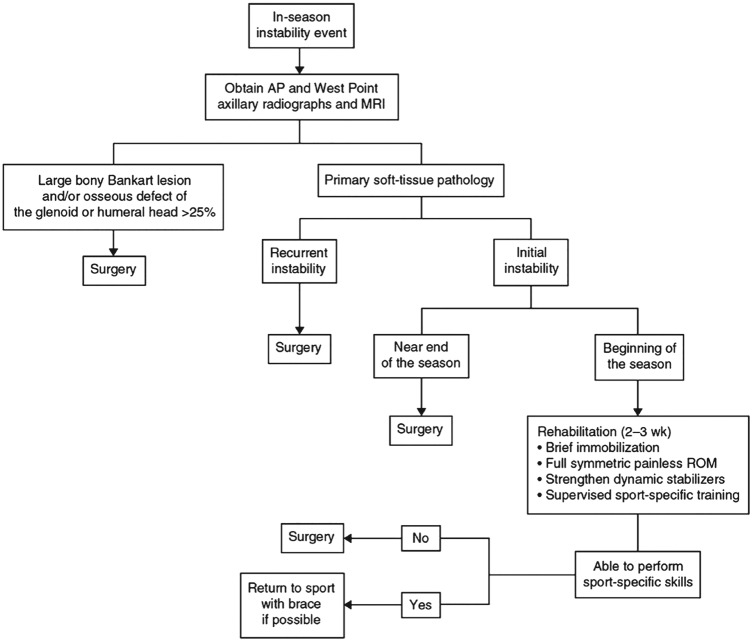
Treatment Algorithm
Owens et al21 described a treatment algorithm for the in-season athlete with instability (Figure 1). As with all algorithms, each patient should be approached individually. Timing of return to play or timing to surgery may differ based on the athlete’s symptoms, personal goals, and specific injury. Athletes with large bony defects, recurrent instability, or injuries near the end of the season should be considered for early surgical stabilization. Other athletes can initially be treated with rehabilitation, and their ability to return to play will determine the need for, and timing of, surgery. Balg and Boileau1 published their “Instability Severity Index Score” as a systematic algorithm to predict which patients are at greatest risk for developing recurrent instability after arthroscopic Bankart repair. They reported that if patients had more than 3 or 4 of the previously listed risk factors (see “Surgical Treatment” section), the risk of recurrence after an arthroscopic Bankart repair was 70%. We are not aware of reports of the application of this scoring system to the nonoperative management of the in-season athlete, but the same risk factors are likely predictive in high-risk athletes. Furthermore, this scoring system may assist the physician in determining the correct stabilization procedure when indicated. Overall, each athlete should be counseled on the high risk of recurrence and almost always undergo an initial course of nonoperative management as described above.
Figure 1.
Treatment algorithm for the in-season athlete with instability. AP, anteroposterior; MRI, magnetic resonance imaging; ROM, range of motion. Reprinted with permission from Owens et al.21
Conclusion
Glenohumeral instability in the athlete remains a common entity that presents a challenge for the athlete as well as the sports medicine team, especially when the injury occurs early to mid-season. The majority of athletes are able to return to sport usually within 2 weeks, although the time to return is variable depending on the extent of the injury and the recurrence rate is high. Further research is needed to evaluate the effectiveness of brace wear on preventing instability symptoms and recurrent dislocations. While the majority of cases eventually result in surgical stabilization, the timing to surgery and the use of open versus arthroscopic techniques remain controversial. Athletes can be expected to return to play around 6 months after surgical stabilization.
Acknowledgments
The authors would like to thank Tom Cichonski for his editorial assistance with this manuscript.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007;89:1470-1477. [DOI] [PubMed] [Google Scholar]
- 2. Bottoni CR, Wilckens JH, DeBerardino TM, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30:576-580. [DOI] [PubMed] [Google Scholar]
- 3. Brumitt J, Sproul A, Lentz P, McIntosh L, Rutt R. In-season rehabilitation of a Division III female wrestler after a glenohumeral dislocation. Phys Ther Sport. 2009;10:112-117. [DOI] [PubMed] [Google Scholar]
- 4. Burkhead WZ, Jr, Rockwood CA., Jr. Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg Am. 1992;74:890-896. [PubMed] [Google Scholar]
- 5. Burns TC, Owens BD. Management of shoulder instability in in-season athletes. Phys Sportsmed. 2010;38(3):55-60. [DOI] [PubMed] [Google Scholar]
- 6. Buss DD, Lynch GP, Meyer CP, Huber SM, Freehill MQ. Nonoperative management for in-season athletes with anterior shoulder instability. Am J Sports Med. 2004;32:1430-1433. [DOI] [PubMed] [Google Scholar]
- 7. Cohen BS, Romeo AA, Bach BR. Shoulder injuries. In: Brotzman SB, Wilk KE, eds. Clinical Orthopaedic Rehabilitation. Vol 2 Philadelphia, PA: Mosby; 2003:125-250. [Google Scholar]
- 8. Crockett HC, Gross LB, Wilk KE, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30:20-26. [DOI] [PubMed] [Google Scholar]
- 9. Dickens JF, Owens BD, Cameron KL, et al. Return to play and recurrent instability after in-season anterior shoulder instability: a prospective multicenter study. Am J Sports Med. 2014;42:2842-2850. [DOI] [PubMed] [Google Scholar]
- 10. Gill TJ, Micheli LJ, Gebhard F, Binder C. Bankart repair for anterior instability of the shoulder. Long-term outcome. J Bone Joint Surg Am. 1997;79:850-857. [DOI] [PubMed] [Google Scholar]
- 11. Handoll HH, Hanchard NC, Goodchild L, Feary J. Conservative management following closed reduction of traumatic anterior dislocation of the shoulder. Cochrane Database Syst Rev. 2006;(1):CD004962. [DOI] [PubMed] [Google Scholar]
- 12. Harris JD, Gupta AK, Mall NA, et al. Long-term outcomes after Bankart shoulder stabilization. Arthroscopy. 2013;29:920-933. [DOI] [PubMed] [Google Scholar]
- 13. Hovelius L, Eriksson K, Fredin H, et al. Recurrences after initial dislocation of the shoulder. Results of a prospective study of treatment. J Bone Joint Surg Am. 1983;65:343-349. [PubMed] [Google Scholar]
- 14. Itoi E, Hatakeyama Y, Sato T, et al. Immobilization in external rotation after shoulder dislocation reduces the risk of recurrence. A randomized controlled trial. J Bone Joint Surg Am. 2007;89:2124-2131. [DOI] [PubMed] [Google Scholar]
- 15. Jakobsen BW, Johannsen HV, Suder P, Sojbjerg JO. Primary repair versus conservative treatment of first-time traumatic anterior dislocation of the shoulder: a randomized study with 10-year follow-up. Arthroscopy. 2007;23:118-123. [DOI] [PubMed] [Google Scholar]
- 16. Kirkley A, Griffin S, Richards C, Miniaci A, Mohtadi N. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder. Arthroscopy. 1999;15:507-514. [DOI] [PubMed] [Google Scholar]
- 17. Kirkley A, Werstine R, Ratjek A, Griffin S. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation. Arthroscopy. 2005;21:55-63. [DOI] [PubMed] [Google Scholar]
- 18. Marans HJ, Angel KR, Schemitsch EH, Wedge JH. The fate of traumatic anterior dislocation of the shoulder in children. J Bone Joint Surg Am. 1992;74:1242-1244. [PubMed] [Google Scholar]
- 19. Milano G, Grasso A, Russo A, et al. Analysis of risk factors for glenoid bone defect in anterior shoulder instability. Am J Sports Med. 2011;39:1870-1876. [DOI] [PubMed] [Google Scholar]
- 20. Owens BD, Agel J, Mountcastle SB, Cameron KL, Nelson BJ. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med. 2009;37:1750-1754. [DOI] [PubMed] [Google Scholar]
- 21. Owens BD, Dickens JF, Kilcoyne KG, Rue JP. Management of mid-season traumatic anterior shoulder instability in athletes. J Am Acad Orthop Surg. 2012;20:518-526. [DOI] [PubMed] [Google Scholar]
- 22. Owens BD, Duffey ML, Nelson BJ, DeBerardino TM, Taylor DC, Mountcastle SB. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med. 2007;35:1168-1173. [DOI] [PubMed] [Google Scholar]
- 23. Owens BD, Nelson BJ, Duffey ML, et al. Pathoanatomy of first-time, traumatic, anterior glenohumeral subluxation events. J Bone Joint Surg Am. 2010;92:1605-1611. [DOI] [PubMed] [Google Scholar]
- 24. Pagnani MJ, Dome DC. Surgical treatment of traumatic anterior shoulder instability in American football players. J Bone Joint Surg Am. 2002;84-A:711-715. [DOI] [PubMed] [Google Scholar]
- 25. Papalia R, Osti L, Del Buono A, Denaro V, Maffulli N. Glenohumeral arthropathy following stabilization for recurrent instability. Br Med Bull. 2010;96:75-92. [DOI] [PubMed] [Google Scholar]
- 26. Pelet S, Jolles BM, Farron A. Bankart repair for recurrent anterior glenohumeral instability: results at twenty-nine years’ follow-up. J Shoulder Elbow Surg. 2006;15:203-207. [DOI] [PubMed] [Google Scholar]
- 27. Plath JE, Aboalata M, Seppel G, et al. Prevalence of and risk factors for dislocation arthropathy: radiological long-term outcome of arthroscopic Bankart repair in 100 shoulders at an average 13-year follow-up. Am J Sports Med. 2015;43:1084-1090. [DOI] [PubMed] [Google Scholar]
- 28. Plath JE, Feucht MJ, Saier T, et al. Sporting activity after arthroscopic Bankart repair for chronic glenohumeral instability. Arthroscopy. 2015;31:1996-2003. [DOI] [PubMed] [Google Scholar]
- 29. Robinson CM, Howes J, Murdoch H, Will E, Graham C. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Joint Surg Am. 2006;88:2326-2336. [DOI] [PubMed] [Google Scholar]
- 30. Sachs RA, Lin D, Stone ML, Paxton E, Kuney M. Can the need for future surgery for acute traumatic anterior shoulder dislocation be predicted? J Bone Joint Surg Am. 2007;89:1665-1674. [DOI] [PubMed] [Google Scholar]
- 31. Taylor DC, Arciero RA. Pathologic changes associated with shoulder dislocations. Arthroscopic and physical examination findings in first-time, traumatic anterior dislocations. Am J Sports Med. 1997;25:306-311. [DOI] [PubMed] [Google Scholar]
- 32. Taylor DC, Krasinski KL. Adolescent shoulder injuries: consensus and controversies. J Bone Joint Surg Am. 2009;91:462-473. [PubMed] [Google Scholar]
- 33. Wheeler JH, Ryan JB, Arciero RA, Molinari RN. Arthroscopic versus nonoperative treatment of acute shoulder dislocations in young athletes. Arthroscopy. 1989;5:213-217. [DOI] [PubMed] [Google Scholar]
- 34. Wilk KE, Reinold MM, Andrews JR. The Athlete’s Shoulder. 2nd ed. Philadelphia, PA: Churchill Livingstone; 2009. [Google Scholar]
- 35. Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am. 2010;92:542-549. [DOI] [PubMed] [Google Scholar]