Abstract
Context:
Groin pain is a common entity in athletes involved in sports that require acute cutting, pivoting, or kicking such as soccer and ice hockey. Athletic pubalgia is increasingly recognized as a common cause of chronic groin and adductor pain in athletes. It is considered an overuse injury predisposing to disruption of the rectus tendon insertion to the pubis and weakness of the posterior inguinal wall without a clinically detectable hernia. These patients often require surgical therapy after failure of nonoperative measures. A variety of surgical options have been used, and most patients improve and return to high-level competition.
Evidence Acquisition:
PubMed databases were searched to identify relevant scientific and review articles from January 1920 to January 2015 using the search terms groin pain, sports hernia, athletic pubalgia, adductor strain, osteitis pubis, stress fractures, femoroacetabular impingement, and labral tears.
Study Design:
Clinical review.
Level of Evidence:
Level 4.
Results and Conclusion:
Athletic pubalgia is an overuse injury involving a weakness in the rectus abdominis insertion or posterior inguinal wall of the lower abdomen caused by acute or repetitive injury of the structure. A variety of surgical options have been reported with successful outcomes, with high rates of return to the sport in the majority of cases.
Keywords: groin, pain, hip, athletic pubalgia (AP), differential diagnosis, surgical treatment, return to sports
Groin pain is a common entity in athletes, particularly those engaged in sports that require specific use (or overuse) of lower abdominal muscles and the proximal musculature of the thigh (eg, soccer, ice hockey, Australian Rules football).69 Despite the high prevalence of groin pain in athletes, the cause of groin pain can be difficult to elucidate because of the complex local anatomy and the broad differential diagnosis.15
An increasingly recognized cause of chronic groin pain in athletes is athletic pubalgia (AP). Gilmore initially described “Gilmore’s groin” in the early 1990s.25 Over the years, many different names have been associated with this injury, such as athletic pubalgia, sports hernia, pubic inguinal pain syndrome, sports-men’s groin, footballers groin injury complex, hockey player’s syndrome, athletic hernia, and inguinal disruption.34,55,56,73,74
AP is one of the more difficult diagnoses to make when evaluating a patient with groin pain. This condition is redundant, not well defined, and difficult to evaluate by physical examination and imaging modalities. There is also increasing awareness of an association between range of motion–limiting hip disorders (femoroacetabular impingement [FAI]) and AP in a subset of athletes.28,43 This has contributed to an increased level of complexity in the decision-making process regarding treatment. Still, it is possible to outline a diagnostic and therapeutic approach that can be used for patients with AP.
Anatomic and Biomechanical Considerations
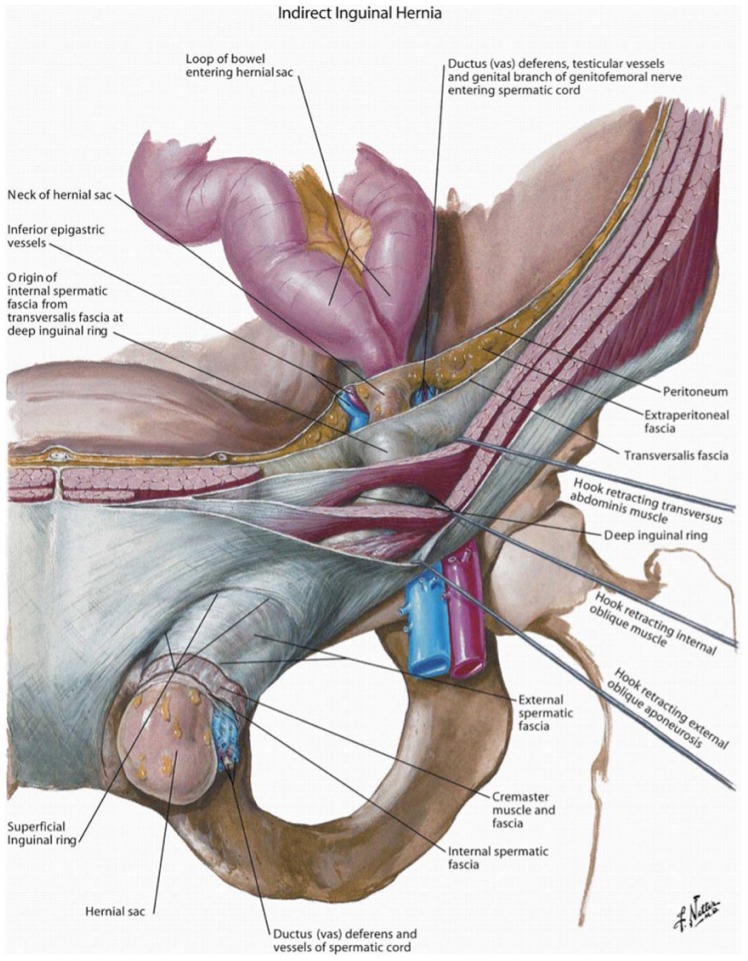
The anatomy of the groin region is complex and involves a confluence of structures (Figure 1). Typically, abdominal wall composition is described in tissue layers from superficial to deep as follows: skin, fascia, external oblique muscle and fascia, internal oblique muscle and fascia, transversus abdominis muscle and fascia, and transversalis fascia with the peritoneum posterior to the transversalis fascia. Before inserting at the midline, the superior fibers of the internal oblique aponeurosis split around the rectus abdominis (with the external oblique fully anterior and the transversus abdominis fully posterior), while the more inferior fibers of the internal oblique aponeurosis and transversus abdominis insert only anterior to the rectus, providing a potentially vulnerable area in the lower fourth of the abdomen where the transversalis fascia is the only structure present posterior to the rectus. The aponeuroses of the internal oblique and transversus abdominis fuse medially to form the conjoint tendon before insertion onto the pubic tubercle. The conjoint tendon inserts anterior to the rectus abdominis on the pubis.57,78
Figure 1.
The anatomic layers of the groin and the path of the indirect inguinal hernia. The rectus abdominis can be seen medially. Reprinted with permission from Swan and Wolcott.78
The inguinal canal passes obliquely inferiorly through the abdominal wall, just superior and parallel to the inguinal ligament. It contains the spermatic cord in men and the round ligament in women. The canal extends from the deep inguinal ring in the transversalis fascia and the superficial inguinal ring in the aponeurosis of the external oblique muscle, just superior and lateral to the pubic tubercle.57,78
The pubic aponeurosis complex is formed by a confluence of fibers from the rectus abdominus, conjoint tendon, and external oblique. The pubic aponeurosis is in continuity with the origin of the adductor muscles and gracilis and is referred to as the rectus abdominus/adductor aponeurosis. The pubic symphysis acts as the fulcrum for forces generated at the anterior pelvis. The structures involved in the pathogenesis of AP are all associated with this fulcrum.41
Pathogenesis
Despite consensus that AP results from injury to muscular and/or fascial attachments to the anterior pubis,1,44,78,79 there is considerable debate in the literature about the pathogenesis and the exact anatomical areas of disruption. The close proximity of numerous anatomical structures in the region in which AP develops results in the strong likelihood of coexisting conditions. Tears associated with AP may involve the transversalis fascia at the posterior inguinal wall, the insertion of the distal rectus abdominis, the conjoint tendon at its distal attachment to the anterior-superior pubis, and/or the external oblique aponeurosis.2,39,44 Although some believe that AP involves isolated rectus abdominis tearing near its distal insertion,2 only 6% to 8% of patients undergoing repair for AP were found to have an isolated tear to the rectus abdominis.1,52 Operative exploration often reveals multiple injury sites in the aforementioned structures, with subsequent subtle weakness to the posterior inguinal wall.48,50,82
Gilmore24 described an extensive injury primarily in soccer players with chronic groin pain. The injury that he coined “Gilmore’s groin” consists of a torn external oblique aponeurosis and conjoint tendon, with avulsion of the conjoint tendon from the pubic tubercle, dehiscence between the conjoint tendon and inguinal ligament, and the absence of a hernia.24 Williams and Foster86 disputed Gilmore’s description of the injury as overly complex. They described isolated tears of the external oblique aponeurosis on surgical exploration in their case series of 6 athletes. There was no evidence of conjoined tendon tear, posterior wall deficiency, or hernia. They concluded that primary suturing of the torn edges of the external oblique aponeurosis may provide immediate relief with rapid recovery.86
Meyers at al52 suggested the mechanism of insult to be a complex injury to the flexion/adduction apparatus of the lower abdomen and hip. Therefore, their surgical approach focuses on the rectus abdominis insertion on the pubis and the adductor longus origin.52
The most widely accepted theory of the pathogenesis is a disrupted rectus tendon attachment to the pubis and a weakened posterior inguinal wall.1,22,27,32,38,67,75-77 This develops as a result of an imbalance between the comparatively strong hip adductor muscles and the comparatively weaker lower abdominal muscles.3 The strong pull of the adductors, particularly against a fixed lower extremity, in the presence of relatively underconditioned abdominal muscles creates a shearing force across the hemipelvis, resulting in relative muscular overload with subsequent attenuation or tearing of the transversalis fascia and/or overlying musculature.3,8,27
Epidemiology
Chronic lower abdomen and groin pain is more prevalent in athletes involved in activities in which there are running, kicking, cutting movements, explosive turns and changes in direction, and rapid acceleration/deceleration.12,73,85 Soccer, ice hockey, and American football players tend to be most commonly affected in the United States.34,52,56 Other commonly involved sports include rugby, Australian Rules football, cricket, martial arts, basketball, baseball, field hockey, tennis, swimming, and long-distance running.12,21,34
AP is more common in men. The lower prevalence of AP in women is probably explained, in part, by differences in pelvic anatomy, lower extremity alignment, and muscle activation.9
Clinical Presentation
History
The classic presentation is an athlete complaining of an insidious onset of unilateral gradually increasing lower abdominal, deep groin, and proximal adductor pain.39 The athlete usually presents for evaluation after the pain has been present for several months, and in some cases, years.1,22,38,46,67,76,77
The pain is activity related and generally resolves with rest. Taking time off from offending activities can lead to resolution of symptoms, but the hallmark is recurrence of the pain with resumption of sports.17 An acute presentation is much less common but has been reported with a trunk hyperextension, hip hyperabduction mechanism that can lead to partial or complete ruptures of the distal rectus abdominus/adductor aponeurosis.52-54
The pain may radiate into the adductor region, perineum, rectus muscles, inguinal ligament, and testicular area. The lower abdomen and groin pain is often aggravated by sudden acceleration, twisting and turning, cutting or kicking movements, sit-ups, coughing, or sneezing.27,44,46,52,67,76
In 1 series of athletes with lower abdominal pain, 43% developed bilateral symptoms, and two-thirds subsequently developed proximal adductor–related pain.52 Deep anterior and lateral pain with prolonged sitting, flexion, abduction, and torsional activities can be secondary to intra-articular hip pathology. Intra-articular hip and pubalgia symptoms may coexist.28,43
Physical Examination
AP may be subtle, and in many cases, no significant examination findings are present. The physical examination for AP begins with palpation of the potential sites of injury. Lower abdominal, adductor, and symphyseal pain to palpation is common in athletes; therefore, it is critical to determine whether the pain correlates with their symptoms. The abdominal obliques, transverses abdominis, and conjoined tendon/rectus abdominus should be palpated for tenderness.41 There may be localized tenderness at or just above the pubic tubercle on the affected side; tenderness at or near the rectus insertion, lateral edge of the rectus, or the conjoined tendon/rectus abdominis interface on the affected side or both sides (if the disease is bilateral); and a tender or dilated superficial inguinal ring and tender posterior wall of the inguinal canal.1,15,27,32,42,47,48,69,79,81 To elicit the pain of AP, the patient performs a resisted sit-up, with legs extended and with feet flexed, while the examiner palpates the rectus abdominis insertion to re-create the symptoms.30 Occasionally symptoms can be reproduced by Valsalva maneuvers such as coughing and sneezing.12,79 The proximal adductor musculature (adductor longus, gracilis, pectineus) should also be palpated; resisted adduction in flexion and extension can be performed to elicit discomfort. Adductor tenderness has been reported in 36% of athletes with AP.12,79 This positive finding may indicate that the adductor longus origin needs to be addressed either by an injection or surgically. A diagnostic injection of local anesthetic may assist with this treatment decision. With AP there is no detectable true inguinal hernia.1,27 Sensory disturbances in the lower abdominal, inguinal, anteromedial thigh, and genital regions can occasionally be present with occasional entrapment of branches of the iliohypogastric, ilioinguinal, and genitofemoral nerves.41
With reports of associated intra- and extra-articular hip pathology in athletes, thorough evaluation of the hip joint is imperative.28,43 Limited hip range of motion, particularly internal rotation, flexion, and abduction, may indicate underlying FAI. Various provocative tests such as anterior impingement (pain with hip flexion, adduction, and internal rotation) are also indicative of concomitant hip joint pathology.29
The Consensus meeting74 suggested criteria for diagnosis of AP if at least 3 of the 5 following clinical signs are detectable: (1) pinpoint tenderness over the pubic tubercle at the point of insertion of the conjoint tendon, (2) palpable tenderness over the deep inguinal ring, (3) pain and/or dilation of the external ring with no obvious hernia evident, (4) pain at the origin of the adductor longus tendon, and (5) dull, diffuse pain in the groin, often radiating to the perineum and inner thigh or across the midline.
Imaging
Plain radiographs should include an anteroposterior pelvis and a lateral view of the proximal femur, which may demonstrate osteitis pubis, pelvic avulsion fractures/apophyseal injuries, stress fractures, degenerative hip disease, underlying FAI and dysplasia, and pelvic neoplasms.41 Bone scans can evaluate stress fractures, osteitis pubis, osteonecrosis, and tenoperiosteal lesions.19
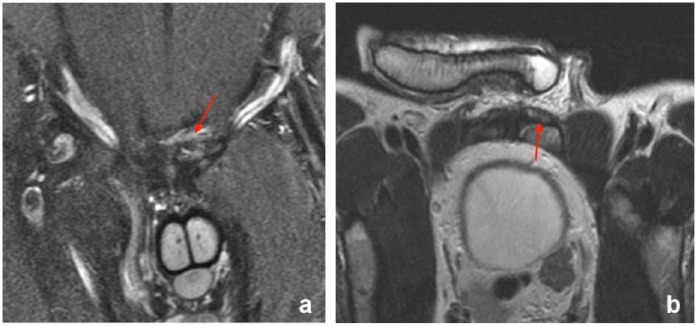
Magnetic resonance imaging (MRI) can demonstrate partial or complete tear of the rectus muscle (Figure 2) or conjoint tendon fibers and bone marrow edema at the pubis. MRI may also reveal adductor strains, labral tears, osteitis pubis, iliopsoas bursitis, avascular necrosis, and occult stress fractures.13,42 Albers et al2 obtained MRI scans on 32 athletes with AP confirmed during surgical exploration. The most common MRI findings included (1) increased signal in T2-weighted images in 1 or both pubic bones, (2) attenuation of the abdominal wall musculofascial layers, (3) bulging of the abdominal wall, and (4) increased signal within 1 or more of the groin muscles. However, such MRI findings lack specificity, and many patients with sports hernia have no pathologic findings on MRI.2 Another study reported that MRI is 68% sensitive and 100% specific for rectus abdominus pathology compared with findings at surgery and 86% sensitive and 89% specific for adductor pathology.88
Figure 2.
(a) Coronal short tau inversion recovery (STIR) and (b) oblique axial T2-weighted magnetic resonance images of a pelvis demonstrating tear of the left rectus tendon (arrow).
Dynamic ultrasonography may be a useful noninvasive diagnostic tool for evaluating AP where posterior inguinal wall deficiency is visible when it is displaced anteriorly rather than becoming taut as the patient strains during the procedure.37,61 However, these features are subtle, and this test is highly operator-dependent and with variable reproducibility.4,37,74
Despite numerous reports in the European literature regarding the safety and efficacy of herniography, this study is invasive, has high rate of complications, and lacks specificity. It is not recommended in the diagnostic work-up of the patient with suspected AP.46
Diagnostic Injections
The symptoms and physical examination findings of FAI, AP, osteitis pubis, and adductor strain can overlap. Diagnostic anesthetic injections are particularly beneficial to determine the primary source of groin pain. A positive response to fluoroscopic or ultrasound-guided intra-articular anesthetic injection suggests an intra-articular source of pain. Persistent pain in the lower abdominal and proximal adductor regions after intra-articular injections is consistent with coexistent athletic AP and adductor pathology.43 Flouroscopic or ultrasound-guided injections into the symphysis can be diagnostic for osteitis pubis. Adductor- and psoas-related pain can be identified with pubic cleft and psoas bursal injections, respectively.1 The sacroiliac joint, trochanteric bursa, iliopsoas tendon sheath, symphysis pubis, lumbar spine, and peripheral nerves are all potentially amenable to diagnostic injection, which also can be therapeutic.
Differential Diagnosis
A broad differential diagnosis must be considered during the evaluation of a patient with groin pain (Table 1). The possible etiologies for groin pain are vast, cover a wide range of physiologic systems and medical subspecialties, and require a thorough history, physical, and imaging studies. Several clinical entities that revolve around the pubic bone and hip joint can be confused with AP.
Table 1.
Differential diagnosis of groin pain
| Orthopaedic causes |
| Bone/joint Femoroacetabular impingement (FAI) Acetabular labral tears Osteitis pubis Stress fractures: Pubic ramus/femoral neck Degenerative hip joint disease Avascular necrosis of the femoral head Slipped capital femoral epiphysis Avulsion fracture: Anterior superior iliac spine/ anterior inferior iliac spine/ischium |
| Muscle Athletic pubalgia Hockey player’s syndrome Rectus femoris strain/tear Adductor strain/tendonitis Iliopsoas strain/tear Rectus abdominis strain/tear: Muscle contusion Gracilis syndrome Snapping hip syndrome |
| Neurologic Nerve entrapment: Ilioinguinal/obturator neuropathy Lumbar radiculopathy |
| Other orthopaedic Bursitis Bone/soft tissue neoplasm of hip/pelvis neoplasms: Bone/soft tissue Herniated nucleus pulposus Seronegative spondyloarthropathy |
| Nonorthopaedic causes |
| Hernia: Inguinal/femoral |
| Urologic Prostatitis/epididymitis/urethritis/urinary tract infection Testicular neoplasm Ureteral colic Hydrocele/varicocele |
| Gynecologic Endometriosis Pelvic inflammatory disease Ovarian cyst |
| Gastrointestinal Rectal/colon neoplasm Inflammatory bowel disease Diverticulitis |
Adductor Strains
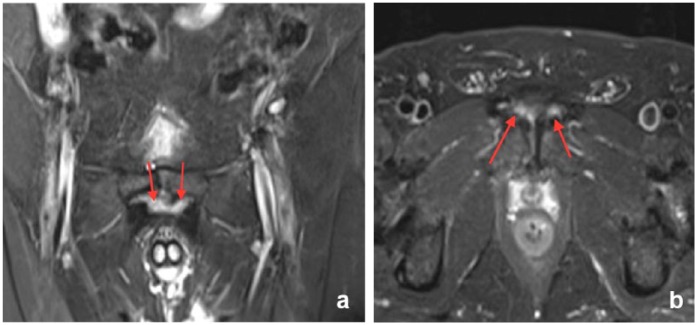
Adductor strains represent one of the most common groin injuries among athletes. Adductor strains accounted for 10% of all injuries in soccer players.84 Injuries usually occur at the musculotendinous junction but may also occur at the bone-tendon junction (enthesopathy), producing tenderness on deep palpation of the involved muscle and pain on resisted adduction.85
Although the diagnosis of these injuries is usually made clinically, ultrasound and MRI may be used in the acute setting (Figure 3). It is particularly useful in chronic injuries unresponsive to conservative treatment modalities to establish a definitive diagnosis and also to rule out other causes for groin pain.51
Figure 3.
(a) Coronal and (b) axial short tau inversion recovery (STIR) magnetic resonance images of a pelvis demonstrating bilateral adductor tear (arrow).
Treatment
Acute adductor strains are often initially treated conservatively with rest and nonsteroidal anti-inflammatory drugs (NSAIDs). Further management is dictated by the location of the strain. If the insult is near the bone-tendon junction (enthesopathy), physical therapy should be delayed until acute symptoms have improved. Because these areas are less vascular, some healing is needed before rehabilitation. Gentle stretching and strengthening should then follow over a period of weeks. If the tear is close to the musculotendinous junction or in the muscle belly, which are highly vascular zones, early and aggressive rehabilitation can be instituted.60 Physical therapy focuses on improving range of motion, strength, flexibility, decreasing the swelling, and institution of a core and contralateral lower extremity strengthening program. Return to sports after acute strains is generally recommended when athletes regain 70% of strength and a painless range of motion, usually by 4 to 8 weeks, while for chronic strains, the recovery period and return to sports may be as long as 6 months.31
Decreased range of motion and adductor strength are risk factors for adductor strains.80 Hence, the primary focus of an adductor injury prevention program is improving range of motion and strength of the adductor tendons.80
The role of steroid injection in adductor strains remains controversial. Schliders et al71 evaluated injection at the bone-tendon junction in competitive athletes and evaluated patients 1 year after the intervention. They concluded that athletes with MRI-documented enthesopathy and long duration of symptoms (mean, 25 weeks) were unlikely to benefit from injection while those with short duration (mean, 6 weeks) of symptoms improved.71 There is currently not enough good evidence for the use of steroid injections in adductor enthesopathy.
Acute complete adductor tears in athletes generally require surgical repair. However, for chronic recalcitrant adductor tears with failed conservative treatment for a minimum of 6 months, surgical treatment with tenotomy may improve the pain. In 1 recent study, 70 patients underwent tenotomy (1 cm from the adductor origin) for chronic adductor injuries. Seventy-three percent were satisfied with the outcome, but only 54% of athletes were able to return to their previous sport.5
Osteitis Pubis
Osteitis pubis (OP) is an isolated or repetitive insult to the pubic symphysis and surrounding structures, usually involving the adductor muscles or gracilis.7 It is usually seen in athletes with high-stress forces transferred through the pelvis and the pubic symphysis during kicking, rapid acceleration, deceleration, or sudden directional changes. These forces can cause stress reactions and a lytic response in the bone.7,83
The classic clinical presentation is pain in the pubic symphysis. There may be also pain in the proximal adductor, the lower abdominal muscles, perineal pain, and testicular or scrotal pain.49 Concomitant pathology must be ruled out such as adductor pathology, AP, FAI, and labral tears.
A typical physical examination finding is localized tenderness on direct palpation over the pubic symphysis.18 The diagnosis of OP is almost always made clinically, and radiographs are rarely helpful. Plain radiographs may show evidence of osteolysis with irregularity, sclerosis, and widening at the pubic symphysis, but these finding are nonspecific and were also found in up to 76% of asymptomatic soccer players.60 Bone scan may reveal increased uptake around the pubic symphysis and can confirm the diagnosis.18
MRI use has been increasing, but reports of sensitivity and specificity have yet to be documented in the literature.84 MRI findings include bone marrow edema and signs of stress reaction. MRI is commonly used to rule out associated pathology such labral tears.
Treatment
Management of OP can be difficult. Conservative treatment remains the first option, including relative rest, ice, NSAIDs, and aggressive physical therapy to strengthen the hip rotators, flexors, and adductors. Daily stretching should be encouraged, with avoidance of kicking and running. However, there is still no standard conservative treatment protocol.33 In spite of treatment, OP tends to have a protracted course and may take up to 6 months or more to return to a preinjury level of functioning.
Steroid injections were used in recalcitrant cases after failed initial conservative treatment of 16 high-level athletes with a positive MRI or bone scan; 14 had immediate relief of symptoms and returned to sports activities within 48 hours. At 6-month follow-up, 7 of 16 athletes remained symptom free; 1 patient had 2 more injections, 7 had persistent pain, and 1 was referred to surgery for painful joint disruption. All patients reported some improvement of their pain level but steroid injections remain controversial.60
Surgery
Surgery is rarely indicated in OP with failure of all conservative treatment modalities. One study recommends observation, physiotherapy, NSAIDs, and up to 3 steroid injections over at least 9 months before suggesting surgery.49 Twenty-three patients with OP (mean duration of symptoms, 13.32 months) who failed all conservative treatment measures were treated by curettage. They had a diagnostic corticosteroid/anesthetic injection into the pubic symphysis prior to surgery and experienced immediate pain relief. Of the 23 patients, 9 were much better, 9 were better, 3 had symptoms similar to before the procedure, and 2 had worsened symptoms at a mean of 24.31 months (range, 12.5-59.6 months). Seven patients were unable to return to full activity. Of those who did return fully, the mean time to recovery was 5.63 months.68
Another surgical option is wedge resection of the symphysis pubis with or without a plate arthrodesis. Ten patients had wedge resection after 10 months of failed conservative treatment. At 92-month follow-up, 7 patients were pain free, 1 had recurrence of pain, 1 had sacroiliac joint pain, and 1 had instability and was treated by arthrodesis.26 Fusion of the pubic symphysis with compression plating and bone grafting may be a viable treatment option for chronic OP,87 with mesh reinforcement of the pubic symphysis.63
Stress Fractures
Stress fractures in the pubic rami and the femoral neck are a fairly common cause of groin pain in athletes, especially long-distance runners, with the inferior pubic ramus being the most common.40,44 The classic presentation is a gradual onset of activity-related groin and thigh pain that improves with rest. The pain worsens during running, and stress fracture should be highly suspected in athletes with a sudden change in their training regimens. Tenderness to deep palpation is present over the pubic ramus, and athletes are unable to stand and support their full weight on the affected sitde.58
Plain radiographs are usually negative early in the course of the disease process, but bone scans can be positive as early as 4 to 8 days after the onset of symptoms.6 Computed tomography (CT) or MRI can confirm the diagnosis of stress fracture if the bone scan is negative. In cases where the pain is out of proportion to the physical findings and with failed conservative treatment modalities for a minimum of 6 to 8 weeks, MRI is particularly helpful to rule out other possible causes of groin pain in athletes.39
The treatment of pubic stress fracture is conservative, with rest for 4 to 6 weeks and avoidance of pain-associated activity. With noncompliance, delayed or nonunion often occurs.65 Stress fractures of the femoral neck may occur on the superior (tension) side of the femoral neck and may be treated conservatively with rest and nonweightbearing. However, if the fracture is on the inferior (compression) side, these stress fractures may progress to complete fracture, and surgery (prophylactic fixation) is the treatment of choice in most cases.40,44
Femoroacetabular Impingement
FAI syndrome can be caused by anatomic abnormalities of the femoral head/neck (cam lesion) and/or the acetabulum (pincer lesions). Impingement of the labrum against the femoral neck can occur with extremes of movement, particularly repeated hip flexion during sports, and this can occur even with normal hip morphology and may predispose to early arthritis of both the femoral head and acetabular surfaces.20 Cam lesions are more common in athletes while pincer lesions are mostly seen in women. Radiographic findings of FAI are frequently seen in asymptomatic athletes. Further studies are needed to determine which athletes with radiographic changes of FAI will develop the clinical symptoms of the syndrome.23
Diagnosis
The classic presentation is activity-related pain, which may be localized to the groin (up to 85%) or to the groin and affected hip (14%).35 The onset may be insidious or triggered by minor trauma. Mechanical symptoms, pain, stiffness, and decreased range of motion of the hip, particularly hip flexion and internal rotation, are common in athletes.14
Physical examination is the key because imaging alone is not sufficient. The anterior impingement test (decreased range of motion and painful limitation in flexion, internal rotation, and adduction of the hip) is the provocative test of choice, with a sensitivity of 75% and specificity of 43%.16
Imaging
Plain radiographs should include an anteroposterior view of the pelvis as well as a cross-table lateral view of the hip. The anteroposterior view can show overcoverage of the femoral head and femoral head deformities including a flattened head-neck junction and a pistol-grip deformity. The cross-table lateral view is used to measure the head-neck offset and the alpha angle. Normal values are a head-neck offset of greater than 7 mm and an alpha angle of less than 55°.59
Magnetic resonance arthrography is the best modality to evaluate associated lesion of the labrum and articular cartilage. A triad of abnormal head-neck morphology, anterosuperior cartilage abnormality, and anterosuperior labral disorders were found on magnetic resonance arthrography in 88% of patients with FAI.36
Treatment
Conservative treatment (restricted range of motion of the hip, physical therapy, NSAIDs) is almost always the first line of treatment. Thirty-seven patients with FAI were treated conservatively with NSAIDs and physical therapy to improve internal rotation/abduction, avoiding excessive physical activity.16 Thirty-three patients had significantly improved symptoms and Harris Hip Scores after 6 months. At 2-year follow-up, 27 patients maintained the improvement.16 Although this approach may benefit less active patients, it is not a practical solution for the athletic population.
Surgical correction of mechanical impingement and bony deformity of cam and/or pincer combined with labral repair is indicated for a symptomatic patient who has failed conservative management.10 In a recent review, arthroscopic outcomes were equal to or better than open methods, with lower rates of major complications.50
Treatment of Athletic Pubalgia
Groin pain from abdominal wall injury is common and often is self-limited and heals. In some cases, the injury becomes chronic and this subgroup of patients often requires surgery.
Factors affecting treatment strategies include: timing, sports season length, prior conservative treatment, activity level, and degree of limitation in upcoming athletic events.
Nonsurgical Treatment
A trial of conservative therapy is almost always the first treatment option for the in-season athlete (NSAIDs, heat or ice, and massage),3 with 6 to 8 weeks of rest followed by focused progressive resistance hip adductor strengthening and stretching exercises, sports-specific functional tasks, and gradual return to full activities.44 The primary focus of rehabilitation programs should be core strength, endurance, coordination and extensibility deficiencies, imbalances at the hip and abdominal muscles, and dynamically stabilizing the pelvic ring.3,12,80
The following is a 4-phase rehabilitation protocol for athletes with chronic groin pain: Phase 1 (weeks 1 and 2) focuses on massage and stretching. Phase 2 (weeks 3 and 4) emphasizes abdominal muscle strengthening. In phase 3 (week 5), functional activities, including running, are initiated. In phase 4 (week 6), the athlete returns to sport-specific activities. At approximately 10 to 12 weeks and when the athlete is pain free, return to sports competition is generally attempted.42
Ultrasound-guided steroid injection into the rectus abdominis insertion site, conjoined tendon, or adductor tendon might be helpful. However, there is not enough evidence regarding the short- and long-term efficacy of these injections.11
A prospective, randomized study of 30 athletes with chronic groin pain/AP with symptoms for at least 3 to 6 months compared nonoperative management with laparoscopic mesh repair. Seven athletes in the nonsurgical group failed all conservative treatment modalities, including steroid injections, and at 6 months elected for operative treatment; only 50% returned to sport at 1-year follow-up. In the surgical group, 29 of 30 athletes returned to full sports and were pain free at 1-year follow-up. Pain and patient satisfaction scores were better in the operative group at all points up to 1 year out from surgery.62
In summary, evidence of successful conservative treatment for AP is lacking.12,17,56,78
Because of the wide range of potential disorders and the potential overlap, a multidisciplinary team approach to assess all patients with possible AP includes an orthopaedic sports medicine specialist and a general surgeon with a special interest in abdominal wall disorders.
For the in-season athlete, a 4-week trial of rest, selective steroid or platelet-rich plasma injections to the rectus abdominus insertion and/or the adductor longus origin, or a short steroid burst with taper are treatment options. Closed-chain lower extremity workouts should be allowed during the rest period.
The in-season rehabilitation protocol (with or without corticosteroid injection) at our institution emphasizes strengthening (hip, core, lower abdominal, and low back muscles), restoration of normal lumbar and hip range of motion (soft tissue/joint mobilization), dynamic stability exercises, and cardiovascular training (see Supplemental Table 2 in the Appendix, available at http://sph.sagepub.com/content/by/supplemental-data). At the completion of the rest period and the rehabilitation program, a functional return to sport assessment is performed to see whether the athlete is capable of returning to the season. If despite all the conservative treatment measures the in-season athlete is unable to compete with persistent pain, we leave it up to the athlete to choose whether to return to the season. Surgery can be considered during the season. Based on the timing and season length, in-season surgery may or may not be season-ending.34
Surgical Treatment
A variety of surgical procedures have been described for the treatment of AP, including open repair of the rectus abdominus, external oblique, transversus abdominus, or transversalis fascia; repairs with mesh reinforcement; laparoscopic repairs; mini-open repairs; and broad pelvic floor repairs with or without adductor releases. All of these repairs represent variations of the standard hernia repair that is well described in the general surgical literature.
Open Repairs
Open repair can involve plication of the transversalis fascia, reapproximation of the conjoint tendon to the inguinal ligament, and approximation of the external oblique aponeurosis. Return-to-sport rate with open repair was 97% within 10 to 12 weeks.25 With surgical repair of the posterior inguinal wall, 14 of 15 athletes (87%) returned to full sports activities.27
Open repair of a posterior wall deficiency has produced excellent results, with 89% and 93%, respectively, able to return to play at the same level of competition.48,67 “Pelvic floor repair” with or without adductor longus release in a prospective study of 157 athletes with long-standing groin pain reattached the inferolateral edge of the rectus abdominis muscle to the pubic bone. A 95% success rate was reported, with 88% and 96% performing at or above their preinjury level by 3 and 6 months’ time, respectively.52 Forty-one male athletes underwent an open Bassini hernial repair and percutaneous adductor longus tenotomy.81 At final follow-up, all patients had resumed their sports activities.81 A “minimal repair” technique, involving a tension-free suture repair of the posterior inguinal wall deficiency and a decompression of the genital branch of the genitofemoral nerve, was used in 128 patients; 84% returned to sport at 4 weeks postoperatively.55 Twelve athletes underwent open internal oblique flap repair, 9 of which were reinforced with mesh. Eighty-three percent of the repairs were excellent and 17% satisfactory. At final follow-up, all 12 patients had resumed their sporting activities.1
Laparoscopic Repairs
The theoretical advantages of laparoscopic repairs include a more rapid recovery and return to sport, improved visualization, and the ability to perform bilateral repairs through the same incision(s).72 A laparoscopic mesh repair for posterior wall deficiencies in 35 professional soccer players resulted in 97% returning to play at 10 days.77 A laparoscopic repair in 131 professional athletes with a mean follow-up of 5 years had 97% resuming full sporting activities by 2 to 3 weeks.22 Fifty-four athletes treated by laparoscopic extraperitoneal inguinal hernia repair with synthetic mesh combined with ipsilateral adductor longus tenotomy returned to full sports-related activity in 24 days (range, 21-28 days).70
Surgical Technique, Including Postoperative Protocol
We prefer to perform an open procedure that is a McVay/Bassini variant using suture repair.45 The principles of our surgical technique are (1) reattachment and retensioning of the rectus abdominis to the pubis and broadening of its insertion, (2) stabilization of the conjoined tendon/rectus abdominis interface, and (3) reinforcement of the posterior wall of the inguinal canal. This repair is a modification of the McVay repair and the Bassini repair; these repairs are considered the “gold standard” repairs for conventional inguinal hernias.64,66 If the adductor longus is involved it can either be injected with steroid or platelet-rich plasma at the time of surgery or a release and lengthening can be performed. All visualized nerves including the femoral branch of the genitofemoral nerve are routinely preserved. Nerve release or division are rarely necessary if there is evidence of nerve entrapment.45
If patients have the typical symptom complex of AP but have a clear-cut conventional groin hernia, especially in the older patient group, then a laparoscopic transabdominal preperitoneal (TAPP) procedure is performed. Similarly, if the surgeon has already opened the groin and finds a clear-cut groin hernia in a patient with the typical AP symptom complex, then the approach is to broaden the rectus insertion with 1 or 2 sutures but still perform an open mesh repair for the hernia.45
The operation is performed as an outpatient surgical procedure. Local anesthesia is used preemptively in the incision and ilioinguinal nerve blocks performed with 1 mg hydromorphone subcutaneously in the postanesthesia care unit and oxycodone as needed for postoperative pain control. Weightbearing is allowed as tolerated with relative rest for the first 10 days.
The postoperative protocol involves 3 phases. Phase 1 (day 1 through week 2) focuses on wound care, pain control, edema reduction, improving soft tissue flexibility, and restoring hip normal passive range of motion (Table 3). Phase 2 (weeks 3-4) targets increasing hip range of motion, core strengthening, and improving biomechanics (Table 4). Phase 3 (weeks 5-8) involves returning to sports and plyometric exercises (Table 5) (see supplemental tables in the Appendix, available at http://sph.sagepub.com/content/by/supplemental-data).
Treatment of Associated AP and FAI
The commonly encountered overlap of AP with other hip and groin disorders, particularly in the young athletic population, further complicates the diagnosis and successful management of AP.27 There is a high incidence of symptom overlap between AP and FAI: 32% of patients who had previously undergone AP surgery subsequently required hip arthroscopy for FAI.28
In 37 hips of primarily Division I and professional athletes who presented with AP and FAI and received pubalgia surgery alone, 25% returned to sports. When only arthroscopic FAI correction was performed, 50% returned to sports. When both conditions were surgically managed in a staged manner or at the same setting, 89% returned to sports without limitations.57
Addressing both disorders surgically, in a staged or concurrent fashion, will allow for a more predictable return to sports with less time lost from athletics.
Conclusion
AP is a distinct syndrome of lower abdomen and groin pain that is found predominantly in high-performance athletes. It can lead to significant disability and time lost from athletics. A careful history, physical examination, and imaging are needed for an accurate diagnosis. Patients typically present with an insidious onset of unilateral deep groin pain, but physical examination reveals no detectable inguinal hernia. Most imaging studies will be normal. These patients often require surgical therapy after failure of nonoperative measures. A variety of surgical options have been used, and most patients improve and return to high-level competition. The principles of surgical treatment are reattachment and retensioning of the rectus abdominis and reinforcement of the posterior wall of the inguinal canal. Both open and laparoscopic techniques lead to excellent results in most reported studies. There is a subset of athletes who present with both symptomatic FAI and AP. Management of both may be necessary to improve outcomes.
Supplementary Material
Footnotes
The following author declared potential conflicts of interest: Brian Busconi, MD, is a paid consultant, lecturer/speaker, and has provided expert testimony for Mitek and Arthrex.
References
- 1. Ahumada LA, Ashruf S, Espinosa-de-los-Monteros A, et al. Athletic pubalgia: definition and surgical treatment. Ann Plast Surg. 2005;55:393-396. [DOI] [PubMed] [Google Scholar]
- 2. Albers SL, Spritzer CE, Garrett WE, Jr, Meyers WC. MR findings in athletes with pubalgia. Skeletal Radiol. 2001;30:270-277. [DOI] [PubMed] [Google Scholar]
- 3. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29:521-533. [DOI] [PubMed] [Google Scholar]
- 4. Armfield DR, Kim DH, Towers JD, Bradley JP, Robertson DD. Sports-related muscle injury in the lower extremity. Clin Sports Med. 2006;25:803-842. [DOI] [PubMed] [Google Scholar]
- 5. Atkinson HD, Johal P, Falworth MS, Ranawat VS, Dala-Ali B, Martin DK. Adductor tenotomy: its role in the management of sports-related chronic groin pain. Arch Orthop Trauma Surg. 2010;130:965-970. [DOI] [PubMed] [Google Scholar]
- 6. Barry NN, McGuire JL. Acute injuries and specific problems in adult athletes. Rheum Dis Clin North Am. 1996;22:531-549. [DOI] [PubMed] [Google Scholar]
- 7. Beatty T. Osteitis pubis in athletes. Curr Sports Med Rep. 2012;11:96-98. [DOI] [PubMed] [Google Scholar]
- 8. Biedert RM, Warnke K, Meyer S. Symphysis syndrome in athletes: surgical treatment for chronic lower abdominal, groin and adductor pain in athletes. Clin J Sport Med. 2003;13:278-284. [DOI] [PubMed] [Google Scholar]
- 9. Brophy RH, Backus S, Kraszewski AP, et al. Differences between sexes in lower extremity alignment and muscle activation during soccer kick. J Bone Joint Surg Am. 2010;92:2050-2058. [DOI] [PubMed] [Google Scholar]
- 10. Byrd JW, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:739-746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Campbell KJ, Boykin RE, Wijdicks CA, Giphart EJ, LaPrade RF, Philippon MJ. Treatment of a hip capsular injury in a professional soccer player with platelet-rich plasma and bone marrow aspirate concentrate therapy. Knee Surg Sports Traumatol Arthrosc. 2013;21:1684-1688. [DOI] [PubMed] [Google Scholar]
- 12. Caudill P, Nyland J, Smith C, Yerasimides J, Lach J. Sports hernias: a systematic literature review. Br J Sports Med. 2008;42:954-964. [DOI] [PubMed] [Google Scholar]
- 13. De Paulis F, Cacchio A, Michelini O, Damiani A, Saggini R. Sports injuries in the pelvis and hip: diagnostic imaging. Eur J Radiol. 1998;27(suppl 1):S49-S59. [DOI] [PubMed] [Google Scholar]
- 14. Ejnisman L, Philippon M, Lertwanich P. Femoroacetabular impingement: the femoral side. Clin Sports Med. 2011;30:369-377. [DOI] [PubMed] [Google Scholar]
- 15. Ekberg O, Persson NH, Abrahamsson PA, Westlin NE, Lilja B. Longstanding groin pain in athletes: a multidisciplinary approach. Sports Med. 1988;6:56-61. [DOI] [PubMed] [Google Scholar]
- 16. Emara K, Samir W, Motasem el H, Ghafar KA. Conservative treatment for mild femoroacetabular impingement. J Orthop Surg (Hong Kong). 2011;19:41-45. [DOI] [PubMed] [Google Scholar]
- 17. Farber AJ, Wilckens JH. Sports hernia: diagnosis and therapeutic approach. J Am Acad Orthop Surg. 2007;15:507-514. [DOI] [PubMed] [Google Scholar]
- 18. Fricker PA, Taunton JE, Ammann W. Osteitis pubis in athletes. Infection, inflammation or injury? Sports Med. 1991;12:266-279. [DOI] [PubMed] [Google Scholar]
- 19. Fricker PA. Management of groin pain in athletes. Br J Sports Med. 1997;31:97-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112-120. [DOI] [PubMed] [Google Scholar]
- 21. Garvey JF, Read JW, Turner A. Sportsman hernia: what can we do? Hernia. 2010;14:17-25. [DOI] [PubMed] [Google Scholar]
- 22. Genitsaris M, Goulimaris I, Sikas N. Laparoscopic repair of groin pain in athletes. Am J Sports Med. 2004;32:1238-1242. [DOI] [PubMed] [Google Scholar]
- 23. Gerhardt MB, Romero AA, Silvers HJ, Harris DJ, Watanabe D, Mandelbaum BR. The prevalence of radiographic hip abnormalities in elite soccer players. Am J Sports Med. 2012;40:584-588. [DOI] [PubMed] [Google Scholar]
- 24. Gilmore J. Groin pain in the soccer athlete: fact, fiction, and treatment. Clin Sports Med. 1998;17:787-793. [DOI] [PubMed] [Google Scholar]
- 25. Gilmore OJ. Gilmore’s groin: ten years experience of groin disruption-a previously unsolved problem in sportsmen. Sports Med Soft Tissue Trauma. 1991;1(3):12-14. [Google Scholar]
- 26. Grace JN, Sim FH, Shives TC, Coventry MB. Wedge resection of the symphysis pubis for the treatment of osteitis pubis. J Bone Joint Surg Am. 1989;71:358-364. [PubMed] [Google Scholar]
- 27. Hackney RG. The sports hernia: a cause of chronic groin pain. Br J Sports Med. 1993;27:58-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hammoud S, Bedi A, Magennis E, Meyers WC, Kelly BT. High incidence of athletic pubalgia symptoms in professional athletes with symptomatic femoroacetabular impingement. Arthroscopy. 2012;28:1388-1395. [DOI] [PubMed] [Google Scholar]
- 29. Hananouchi T, Yasui Y, Yamamoto K, Toritsuka Y, Ohzono K. Anterior impingement test for labral lesions has high positive predictive value. Clin Orthop Relat Res. 2012;470:3524-3529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hawkins RD, Hulse MA, Wilkinson C, Hodson A, Gibson M. The association football medical research programme: an audit of injuries in professional football. Br J Sports Med. 2001;35:43-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Holmich P, Uhrskou P, Ulnits L, et al. Effectiveness of active physical training as treatment for long-standing adductor-related groin pain in athletes: randomised trial. Lancet. 1999;353:439-443. [DOI] [PubMed] [Google Scholar]
- 32. Ingoldby C. Laparoscopic and conventional repair of groin disruption in sportsmen. Br J Surg. 1997;84:213-215. [DOI] [PubMed] [Google Scholar]
- 33. Jarosz BS. Individualized multi-modal management of osteitis pubis in an Australian Rules footballer. J Chiropr Med. 2011;10:105-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kachingwe AF, Grech S. Proposed algorithm for the management of athletes with athletic pubalgia (sports hernia): a case series. J Orthop Sports Phys Ther. 2008;38:768-781. [DOI] [PubMed] [Google Scholar]
- 35. Kaplan K, Shah M, Youm T. Femoroacetabular impingement: diagnosis and treatment. Bull NYU Hosp Jt Dis. 2010;68:70-75. [PubMed] [Google Scholar]
- 36. Kassarjian A. Hip MR arthrography and femoroacetabular impingement. Semin Musculoskelet Radiol. 2006;10:208-219. [DOI] [PubMed] [Google Scholar]
- 37. Kavanagh EC, Koulouris G, Ford S, McMahon P, Johnson C, Eustace SJ. MR imaging of groin pain in the athlete. Semin Musculoskel Radiol. 2006;10:197-207. [DOI] [PubMed] [Google Scholar]
- 38. Kluin J, den Hoed PT, van Linschoten R, Ijzerman JC, van Steensel CJ. Endoscopic evaluation and treatment of groin pain in the athlete. Am J Sports Med. 2004;32:944-949. [DOI] [PubMed] [Google Scholar]
- 39. Kumar A, Doran J, Batt ME, Nguyen-Van-Tam JS, Beckingham IJ. Results of inguinal canal repair in athletes with sports hernia. J R Coll Surg Edinb. 2002;47:561-565. [PubMed] [Google Scholar]
- 40. Fon LJ, Spence RA. Sportsman’s hernia. Br J Surg. 2000;87:545-552. [DOI] [PubMed] [Google Scholar]
- 41. Larson CM. Sports hernia/athletic pubalgia: evaluation and management. Sports Health. 2014;6:139-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Larson CM, Lohnes JH. Surgical management of athletic pubalgia. Oper Tech Sports Med. 2002;10:228-232. [Google Scholar]
- 43. Larson CM, Pierce BR, Giveans MR. Treatment of athletes with symptomatic intra-articular hip pathology and athletic pubalgia/sports hernia: a case series. Arthroscopy. 2011;27:768-775. [DOI] [PubMed] [Google Scholar]
- 44. LeBlanc KE, LeBlanc KA. Groin pain in athletes. Hernia. 2003;7:68-71. [DOI] [PubMed] [Google Scholar]
- 45. Litwin DE, Sneider EB, McEnaney PM, Busconi BD. Athletic pubalgia (sports hernia). Clin Sports Med. 2011;30:417-434. [DOI] [PubMed] [Google Scholar]
- 46. Lovell G. The diagnosis of chronic groin pain in athletes: a review of 189 cases. Aust J Sci Med Sport. 1995;27:76-79. [PubMed] [Google Scholar]
- 47. Lynch SA, Renström PA. Groin injuries in sport: treatment strategies. Sports Med. 1999;28:137-144. [DOI] [PubMed] [Google Scholar]
- 48. Malycha P, Lovell G. Inguinal surgery in athletes with chronic groin pain: the ‘sportsman’s’ hernia. Aust N Z J Surg. 1992;62:123-125. [DOI] [PubMed] [Google Scholar]
- 49. Mandelbaum B, Mora SA. Osteitis pubis. Oper Tech Sports Med. 2005;13:62-67. [Google Scholar]
- 50. Matsuda DK, Carlisle JC, Arthurs SC, Wierks CH, Philippon MJ. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy. 2011;27:252-269. [DOI] [PubMed] [Google Scholar]
- 51. Megliola A, Eutropi F, Scorzelli A, et al. Ultrasound and magnetic resonance imaging in sports-related muscle injuries. Radiol Med. 2006;111:836-845. [DOI] [PubMed] [Google Scholar]
- 52. Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BR. Management of severe lower abdominal or inguinal pain in high-performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med. 2000;28:2-8. [DOI] [PubMed] [Google Scholar]
- 53. Meyers WC, McKechnie A, Philippon MJ, Horner MA, Zoga AC, Devon ON. Experience with “sports hernia” spanning two decades. Ann Surg. 2008;248:656-665. [DOI] [PubMed] [Google Scholar]
- 54. Minnich JM, Hanks JB, Muschaweck U, Brunt LM, Diduch DR. Sports hernia: diagnosis and treatment highlighting a minimal repair surgical technique. Am J Sports Med. 2011;39:1341-1349. [DOI] [PubMed] [Google Scholar]
- 55. Muschaweck U, Berger L. Minimal repair technique of sportsmen’s groin: an innovative open-suture repair to treat chronic inguinal pain. Hernia. 2010;14:27-33. [DOI] [PubMed] [Google Scholar]
- 56. Nam A, Brody F. Management and therapy for sports hernia. J Am Coll Surg. 2008;206:154-164. [DOI] [PubMed] [Google Scholar]
- 57. Netter FH. The CIBA Collection of Medical Illustrations: The Digestive System I. New York, NY: RR Donnelley and Sons; 1975. [Google Scholar]
- 58. Noakes TD, Smith JA, Lindberg G, Wills CE. Pelvic stress fractures in long distance runners. Am J Sports Med. 1985;13:120-123. [DOI] [PubMed] [Google Scholar]
- 59. Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556-560. [DOI] [PubMed] [Google Scholar]
- 60. O’Connell MJ, Powell T, McCaffrey NM, O’Connell D, Eustace SJ. Symphyseal cleft injection in the diagnosis and treatment of osteitis pubis in athletes. AJR Am J Roentgenol. 2002;179:955-959. [DOI] [PubMed] [Google Scholar]
- 61. Orchard JW, Read JW, Neophyton J, Garlick D. Groin pain associated with ultrasound finding of inguinal canal posterior wall deficiency in Australian Rules footballers. Br J Sports Med. 1998;32:134-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Paajanen H, Brinck T, Hermunen H, Airo I. Laparoscopic surgery for chronic groin pain in athletes is more effective than nonoperative treatment: a randomized clinical trial with magnetic resonance imaging of 60 patients with sportsman’s hernia (athletic pubalgia). Surgery. 2011;150:99-107. [DOI] [PubMed] [Google Scholar]
- 63. Paajanen H, Heikkinen J, Hermunen H, Airo I. Successful treatment of osteitis pubis by using totally extraperitoneal endoscopic technique. Int J Sports Med. 2005;26:303-306. [DOI] [PubMed] [Google Scholar]
- 64. Panos RG, Beck DE, Maresh JE, Harford FJ. Preliminary results of a prospective randomized study of Cooper’s ligament versus Shouldice herniorrhaphy technique. Surg Gynecol Obstet. 1992;175:315-319. [PubMed] [Google Scholar]
- 65. Pavlov M, Nelson TL, Warren RF, Torg JS, Burnstein AH. Stress fractures of the pubic ramus. A report of twelve cases. J Bone Joint Surg Am. 1982;64:1020-1025. [PubMed] [Google Scholar]
- 66. Pokorny H, Klingler A, Schmid T, et al. Recurrence and complications after laparoscopic versus open inguinal hernia repair: results of a prospective randomized multicenter trial. Hernia. 2008;12:385-389. [DOI] [PubMed] [Google Scholar]
- 67. Polglase AL, Frydman GM, Farmer KC. Inguinal surgery for debilitating chronic groin pain in athletes. Med J Aust. 1991;155:674-677. [PubMed] [Google Scholar]
- 68. Radic R, Annear P. Use of pubic symphysis curettage for treatment-resistant osteitis pubis in athletes. Am J Sports Med. 2008;36:122-128. [DOI] [PubMed] [Google Scholar]
- 69. Renström P, Peterson L. Groin injuries in athletes. Br J Sports Med. 1980;14:30-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Rossidis G, Perry A, Abbas H, et al. Laparoscopic hernia repair with adductor tenotomy for athletic pubalgia: an established procedure for an obscure entity. Surg Endosc. 2015;29:381-386. [DOI] [PubMed] [Google Scholar]
- 71. Schilders E, Bismil Q, Robinson P, O’Connor PJ, Gibbon WW, Talbot JC. Adductor-related groin pain in competitive athletes. Role of adductor enthesis, magnetic resonance imaging, and entheseal pubic cleft injections. J Bone Joint Surg Am. 2007;89:2173-2178. [DOI] [PubMed] [Google Scholar]
- 72. Schurict A, Haut E, Wetzler M. Surgical options in the treatment of sports hernia. Oper Tech Sports Med. 2002;10:224-227. [Google Scholar]
- 73. Sheen AJ, Iqbal Z. Contemporary management of ‘inguinal disruption’ in the sportsman’s groin. BMC Sports Sci Med Rehabil. 2014;6:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Sheen AJ, Stephenson BM, Lloyd DM, et al. ‘Treatment of the sportsman’s groin’: British Hernia Society’s 2014 position statement based on the Manchester Consensus Conference. Br J Sports Med. 2014;48:1079-1087. [DOI] [PubMed] [Google Scholar]
- 75. Srinivasan A, Schuricht A. Long-term follow-up of laparoscopic preperitoneal hernia repair in professional athletes. J Laparoendosc Adv Surg Tech A. 2002;12:101-106. [DOI] [PubMed] [Google Scholar]
- 76. Steele P, Annear P, Grove JR. Surgery for posterior wall inguinal deficiency in athletes. J Sci Med Sport. 2004;7:415-421. [DOI] [PubMed] [Google Scholar]
- 77. Susmallian S, Ezri T, Elis M, Warters R, Charuzi I, Muggia-Sullam M. Laparoscopic repair of ‘sportsman’s hernia’ in soccer players as treatment of chronic inguinal pain. Med Sci Monit. 2004;10:52-54. [PubMed] [Google Scholar]
- 78. Swan KG, Jr, Wolcott M. The athletic hernia: a systematic review. Clin Orthop Relat Res. 2007;455:78-87. [DOI] [PubMed] [Google Scholar]
- 79. Taylor DC, Meyers WC, Moylan JA, Lohnes JH, Bassett FH, Garrett WE. Abdominal musculature abnormalities as a cause of groin pain in athletes. Am J Sports Med. 1991;19:239-242. [DOI] [PubMed] [Google Scholar]
- 80. Tyler TF, Nicholas SJ, Campbell RJ, Donellan S, McHugh MP. The effectiveness of a preseason exercise program to prevent adductor muscle strains in professional ice hockey players. Am J Sports Med. 2002;30:680-683. [DOI] [PubMed] [Google Scholar]
- 81. Van Der Donckt K, Steenbrugge F, Van Den Abbeele K, Verdonk R, Verhelst M. Bassini’s hernial repair and adductor longus tenotomy in the treatment of chronic groin pain in athletes. Acta Orthop Belg. 2003;69:35-41. [PubMed] [Google Scholar]
- 82. van Veen RN, de Baat P, Heijboer MP, et al. Successful endoscopic treatment of chronic groin pain in athletes. Surg Endosc. 2007;21:189-193. [DOI] [PubMed] [Google Scholar]
- 83. Verrall GM, Henry L, Fazzalari NL, Slavotinek JP, Oakeshott RD. Bone biopsy of the parasymphyseal pubic bone region in athletes with chronic groin injury demonstrates new woven bone formation consistent with a diagnosis of pubic bone stress injury. Am J Sports Med. 2008;36:2425-2431. [DOI] [PubMed] [Google Scholar]
- 84. Verrall GM, Slavotinek JP, Fon GT. Incidence of pubic bone marrow oedema in Australian Rules football players: relation to groin pain. Br J Sports Med. 2001;35:28-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Werner J, Hägglund M, Waldén M, Ekstrand J. UEFA injury study: a prospective study of hip and groin injuries in professional football over seven consecutive seasons. Br J Sports Med. 2009;43:1036-1040. [DOI] [PubMed] [Google Scholar]
- 86. Williams P, Foster ME. ‘Gilmore’s groin’—or is it? Br J Sports Med. 1995;29:206-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Williams PR, Thomas DP, Downes EM. Osteitis pubis and instability of the pubic symphysis. When nonoperative measures fail. Am J Sports Med. 2000;28:350-355. [DOI] [PubMed] [Google Scholar]
- 88. Zoga AC, Kavanagh EC, Omar IM, et al. Athletic pubalgia and the “sports hernia”: MR imaging findings. Radiology. 2008;247:797-807. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.