Abstract
Objective
The presence of deleterious mutations in breast cancer (BRCA)-1 or BRCA-2 gene has a decisive influence on the development of various types of neoplasms, such as breast, ovarian, tubal, and peritoneal cancers. Primary peritoneal cancer is an aggressive malignancy which, due to the absence of a specific screening test, cannot be diagnosed in its early stages. As a risk-reducing option, prophylactic bilateral salpingo-oophorectomy and mastectomy are often proposed in BRCA gene carriers. The effectiveness of a preventive surgical treatment is, however, unclear in the development of peritoneal cancer.
Material and Methods
An extensive electronic search was performed in PubMed, Scopus, and Cochrane databases.
Results
The total number of patients who underwent prophylactic bilateral salpingo-oophorectomy was 1,830, of whom 28 presented with peritoneal cancer (1.53%). The age of the included patients ranged from 48 to 61 years. BRCA-1 was present in 9 out of 28 patients and BRCA-2 in 2 patients, while the type of BRCA was unclear in 17 patients. Salpingo-oophorectomy was performed in 23 out of 28 patients, while oophorectomy was carried out in 5 patients. The interval from initial risk-reducing surgical treatment to the presentation of peritoneal cancer ranged from 12 to 84 months.
Conclusion
Modification of the follow-up guidelines and increase in healthcare providers’ awareness may reduce the risk of peritoneal cancer.
Keywords: BRCA gene, peritoneal carcinoma, management, prophylaxis, etiology
Introduction
Mutations in breast cancer (BRCA) genes are correlated with an increase in the risk of breast, ovarian, tubal, and peritoneal cancers. Premalignant dysplasias within the fallopian tubes have also been linked to BRCA gene mutations. The prevalence of BRCA mutations in the general population ranges between 0.07 and 0.24% for BRCA-1 and 0.14 and 0.22% for BRCA-2 (1). Genetic counseling and risk-reducing surgery, including prophylactic bilateral salpingo-oophorectomy and mastectomy, are often recommended in BRCA carriers. The median recommended age for prophylactic salpingo-oophorectomy in BRCA carriers is before the age of 40 years (in USA, before 35 years, while in Europe, before 40 years) or certainly after completion of family (2, 3).
Primary peritoneal cancer is an aggressive malignancy that cannot as yet be diagnosed early with screening tests. At present, the median age of peritoneal cancer diagnosis is 63 years, ranging from 44 to 74 years (4). The median survival rates vary from 11.3 to 17.8 months (5). Prophylactic salpingo-oophorectomy is used for cancer risk reduction in BRCA gene carriers and leads to decrease of ovarian/tubal/peritoneal cancer risk to 3.5–4.3% and breast cancer risk to 30–40% (1, 6). In a more optimistic study, prophylactic salpingo-oophorectomy was shown to be more effective in preventing ovarian, tubal, and breast cancers, with low surgical morbidity and complications including hematomas, cardiac arrhythmias, and injury of adjacent organs such as the bladder, ureters, and intestines (4). More specifically, in the above study, 3.4% of patients developed breast cancer and 0.8% developed peritoneal cancer. However, the follow-up period of that study was small (22 months) (4).
The aim of this report is to present a review of cases with peritoneal cancer after prophylactic bilateral salpingo-oophorectomy and to discuss the possible etiology of this rare entity as well as the possible changes in the management of such patients.
Material and Methods
We retrieved the included studies in our narrative review after performing an extensive electronic search in the PubMed (09/26/2015), Scopus (09/26/2015), and Cochrane (09/26/2015) databases. The search strategy adopted included the combination of the key words “BRCA” AND “peritoneal” AND (“carcinoma” OR “cancer” OR “neoplasm”). The reference list was also hand-searched for additional studies. Studies written only in the English language were included. The reporting data on primary peritoneal cancer in BRCA carriers after prophylactic bilateral salpingo-oophorectomy of the retrieved studies were regarded as includable for this review. Abstracts, commentaries, review articles, conference papers, animal studies, and editorials were not included in this review.
Results
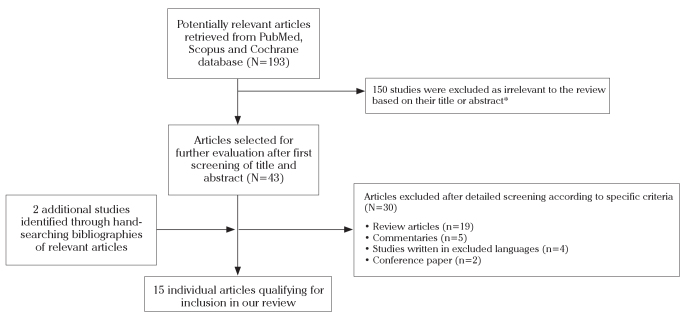
A total of 93 and 100 studies located in the PubMed and Scopus searches were retrieved, respectively, of which 13 studies met the inclusion criteria of our review (2, 4, 7–17). No further studies were retrieved from the Cochrane database. Two additional studies were found through hand-searching of references (18, 19). The search strategy followed is depicted in Figure 1 (flow diagram).
Figure 1.
The greater part of studies was retrieved in both databases
The major characteristics of the studies included in our review (demographics, publication type, histological type, type of BRCA gene, type of prophylactic surgical treatment, interval from initial prophylactic surgical treatment, and interval from initial prophylactic surgical treatment to detection of peritoneal cancer [in months]) are presented in Table 1.
Table 1.
Published cases of primary peritoneal cancer in BRCA carriers after prophylactic surgical treatment
| First author, (ref) country | Publication type | No. of patients (%) | Age of patients (in years) | Type of BRCA genes | Type of prophylactic surgical treatment | Interval from initial prophylactic surgical treatment to detection of peritoneal cancer (in months) | Histological type |
|---|---|---|---|---|---|---|---|
| Bacha et al. (4) Brazil | Retrospective study | 1/119 (0.8) | NR | BRCA-1/2 | Salpingo-oophorectomy | NR | NR |
| Reitsma et al. (2) Netherlands | Prospective study | 1/303 (0.3) | NR | BRCA-1 | Salpingo-oophorectomy | 50.4 | NR |
| Rhiem et al. (8) Germany | Retrospective study | 1/175 (0.6) | 59 | BRCA-1 | Salpingo-oophorectomy | 26 | NR |
| Powell et al. (7) USA | Prospective study | 2/111 (1.8) | NR | BRCA-1/2 | Salpingo-oophorectomy | 12 and 84 | Ovarian origin |
| Rabban et al. (9) USA | Retrospective study | 2/89 (2.2) | NR | BRCA-1/2 | Salpingo-oophorectomy | 22 and 62 | Serous carcinoma |
| Carison et al. (11) USA | Prospective study | 5/19 (26.3) | NR | BRCA-1/2 | Salpingo-oophorectomy | NR | NR |
| Kauff et al. (12) USA | Prospective study | 3/325 (0.9) | NR | BRCA-1 | Salpingo-oophorectomy | Median: 16 | NR |
| Maehle et al. (10) Norway | Prospective study | 3/49 (6.1) | NR | BRCA-1/2 | Salpingo-oophorectomy | NR | Serous carcinoma |
| Hill et al. (13) Canada | Case report | 1 | 56 | BRCA-1 | Oophorectomy, hysterectomy | 60 | Serous papillary adenocarcinoma |
| Meeuwissen et al. (18) Netherlands | Retrospective study | 1/152 (0.6) | 61 | BRCA-1 | Salpingo-oophorectomy | 14 | Papillary serous carcinoma |
| Powell et al. (14) USA | Retrospective study | 2/67 (2.9) | NR | BRCA-2 | Salpingo-oophorectomy | 60 | NR |
| Kauff et al. (15) USA | Prospective study | 1/98 (1) | NR | BRCA-1/2 | Salpingo-oophorectomy | 16.3 | NR |
| Scheuer et al. (16) USA | Prospective study | 1/233 (0.4) | 48 | BRCA-1 | Salpingo-oophorectomy | NR | NR |
| Colgan et al. (17) Canada | Prospective study | 1/60 (1.6) | NR | BRCA-1 | Oophorectomy | NR | NR |
| Tobacman et al. (19) USA | Prospective study | 3/29 (10.3) | NR | BRCA-1/2 | Oophorectomy | NR | NR |
Ref: reference; USA: United States of America; No.: number; NR: not referred; BRCA: breast cancer
Nine prospective studies, five retrospective studies, and one case report were included in the study. The total number of patients who underwent prophylactic bilateral salpingo-oophorectomy was 1830, of whom 28 had peritoneal cancer (1.53%). The age of the included patients ranged from 48 to 61 years. BRCA-1 was present in 9 out of 28 patients and BRCA-2 in 2 patients, while the type of BRCA was unclear in 17 patients. Salpingo-oophorectomy was performed in 23 out of 28 patients, while oophorectomy was carried out in 5 patients. The interval from initial risk-reducing surgical treatment to the presentation of peritoneal cancer ranged from 12 to 84 months. Regarding the histological type, this was mentioned in only 5 studies, but serous type was mentioned for all patients.
Discussion
For many years, it was believed that the ovarian and peritoneal epithelia share a common embryonal (mesonephric) origin. However, ovarian and primary peritoneal cancers are histologically similar to the Mullerian epithelium. For this reason, another peritoneal cancer etiology theory suggested that primary ovarian epithelial, tubal, and primary peritoneal cancers are all Mullerian in origin, and they are now considered to be a single disease entity. The majority of these cancers originate from the fimbriated end of the fallopian tube, but some of them derive from components of the secondary Mullerian system (20). It is thus believed that the etiology of such a rare cancer could be found in the fallopian tube remnants after prophylactic salpingo-oophorectomy. Compared to ovarian cancer, primary peritoneal cancer is characterized by loss of heterozygosity at chromosomal loci as well as overexpression of the human epidermal growth factor receptor 2 (HER2) oncogene on immunohistochemical analysis (21).
Primary peritoneal cancer is a rare malignancy mimicking ovarian cancer. In BRCA carriers, the lifetime risk of presenting with primary peritoneal cancer has been estimated to be 1.3%, and this risk should be explained when counseling patients for prophylactic salpingo-oophorectomy (22). This was also found in the present review, which demonstrated that the risk is around 1.53%. It has been shown that BRCA carriers are diagnosed at a younger mean age than patients without a mutation (60 versus 70 years), but the overall median survival is in favor of the BRCA carriers (148 versus 41 months) (22). Primary peritoneal cancer can be found many years after prophylactic salpingo-oophorectomy, and it usually presents at advanced stages (6). In the present review, the interval from initial surgery to presentation of peritoneal cancer ranged from 12 to 84 months. For this reason, long-term follow-up is required in such patients; and although it is very unlikely to be diagnosed early, our hospitals guidelines recommend that gynecologic examination, transvaginal ultrasound, and serum cancer antigen 125 (CA-125) be carried out on an annual basis. However, as was recently pointed out, there is a lack of follow-up protocols in the current literature (23). More specifically, although dual-energy X-ray absorptiometry testing, annual serum CA-125, and pelvic examination have been suggested, a recent cohort questionnaire-based study reported that some women do not have access to follow-up or have no support for their menopausal symptoms by health providers who either did not recommend follow-up testing or advised against hormone replacement therapy (HRT) use in younger patients with no other contraindication to the use of HRT (23, 24). Regarding possible future changes in the management of such patients, a recent review proposed that the source of primary peritoneal cancer in BRCA carriers after prophylactic salpingo-oophorectomy could be the appendix (25). It is therefore suggested by a research group that prophylactic appendectomy should also be considered in BRCA carriers to eliminate the risk of primary peritoneal cancer (25).
The possible mechanisms that could explain the origin of peritoneal cancer after prophylactic salpingo-oophorectomy include the presence of the precancerous lesion serous tubal intraepithelial carcinomas (STIC) during salpingectomy and the possibility that STIC would have metastasized to the peritoneum before the prophylactic procedure (26). Moreover, the second hypothesis could suggest that the salpingo-oophorectomy was incomplete, meaning that there might be an ovarian or tubal remnant postoperatively. Furthermore, the third hypothesis could include the primary origin of the peritoneal cancer. Although, the appendix hypothesis is also presented in the current literature by one research group, we do not believe that this hypothesis could explain the pathogenetic mechanism (25).
This current report has several limitations. First, the number of studies and of patients included is small, which underlines the rarity of cancer represented after risk-reducing surgical treatment in BRCA gene carriers. Concerning our selected search strategy, it could be considered limited due to the exclusion of abstracts, commentaries, review articles, conference papers, animal studies, as well as editorials. Restriction to only English language literature could also have limited the range of our search.
In conclusion, the role of prophylactic salpingo-oophorectomy in BRCA carriers is crucial for the prevention of breast/ovarian cancer. Peritoneal cytology at the time of prophylactic adnexectomy, is also advised in order to assist in the diagnosis of peritoneal carcinomatosis. However, there is still a risk of peritoneal cancer for such patients that they should be aware of. Changes and better organization in the follow-up guidelines and increase in healthcare providers’ awareness should be considered to reduce the risk of peritoneal cancer.
Footnotes
Ethics Committee Approval: N/A.
Informed Consent: N/A.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - C.I., N.V.; Design - C.I., I.D.G.; Supervision - N.V.; Materials - C.I., I.D.G.; Data Collection and/or Processing - C.I., I.D.G.; Analysis and/or Interpretation - C.I., I.D.G..; Literature Review - C.I., I.D.G.; Writer - C.I., I.D.G.; Critical Review - C.I., N.V.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Finch A, Beiner M, Lubinski J, Lynch HT, Moller P, Rosen B, et al. Salpingo-oophorectomy and the risk of ovarian, fallopian tube, and peritoneal cancers in women with a BRCA1 or BRCA2 Mutation. JAMA. 2006;296:185–92. doi: 10.1001/jama.296.2.185. http://dx.doi.org/10.1001/jama.296.2.185. [DOI] [PubMed] [Google Scholar]
- 2.Reitsma W, de Bock GH, Oosterwijk JC, Bart J, Hollema H, Mourits MJ. Support of the ‘fallopian tube hypothesis’ in a prospective series of risk-reducing salpingo-oophorectomy specimens. Eur J Cancer. 2013;49:132–41. doi: 10.1016/j.ejca.2012.07.021. http://dx.doi.org/10.1016/j.ejca.2012.07.021. [DOI] [PubMed] [Google Scholar]
- 3.Pölcher M, Hauptmann S, Fotopoulou C, Schmalfeldt B, Meinhold-Heerlein I, Mustea A, et al. Opportunistic salpingectomies for the prevention of a high-grade serous carcinoma: a statement by the Kommission Ovar of the AGO. Arch Gynecol Obstet. 2015;292:231–4. doi: 10.1007/s00404-015-3697-y. http://dx.doi.org/10.1007/s00404-015-3697-y. [DOI] [PubMed] [Google Scholar]
- 4.Bacha OM, Gregoire J, Grondin K, Edelweiss MI, Laframboise R, Simard J, et al. Effectiveness of risk-reducing salpingo-oophorectomy in preventing ovarian cancer in a high-risk French Canadian population. Int J Gynecol Cancer. 2012;22:974–8. doi: 10.1097/IGC.0b013e318257b936. http://dx.doi.org/10.1097/IGC.0b013e318257b936. [DOI] [PubMed] [Google Scholar]
- 5.Iavazzo C, Vorgias G, Katsoulis M, Kalinoglou N, Dertimas V, Akrivos T. Primary peritoneal serous papillary carcinoma: clinical and laboratory characteristics. Arch Gynecol Obstet. 2008;278:53–6. doi: 10.1007/s00404-008-0678-4. http://dx.doi.org/10.1007/s00404-008-0678-4. [DOI] [PubMed] [Google Scholar]
- 6.Laki F, Kirova YM, This P, Plancher C, Asselain B, Sastre X, et al. Prophylactic salpingo-oophorectomy in a series of 89 women carrying a BRCA1 or a BRCA2 mutation. Cancer. 2007;109:1784–90. doi: 10.1002/cncr.22603. http://dx.doi.org/10.1002/cncr.22603. [DOI] [PubMed] [Google Scholar]
- 7.Powell CB, Chen LM, McLennan J, Crawford B, Zaloudek C, Rabban JT, et al. Risk-reducing salpingo-oophorectomy (RRSO) in BRCA mutation carriers: experience with a consecutive series of 111 patients using a standardized surgical-pathological protocol. Int J Gynecol Cancer. 2011;21:846–51. doi: 10.1097/IGC.0b013e31821bc7e3. http://dx.doi.org/10.1097/IGC.0b013e31821bc7e3. [DOI] [PubMed] [Google Scholar]
- 8.Rhiem K, Foth D, Wappenschmidt B, Gevensleben H, Büttner R, Ulrich U, et al. Risk-reducing salpingo-oophorectomy in BRCA1 and BRCA2 mutation carriers. Arch Gynecol Obstet. 2011;283:623–7. doi: 10.1007/s00404-010-1476-3. http://dx.doi.org/10.1007/s00404-010-1476-3. [DOI] [PubMed] [Google Scholar]
- 9.Rabban JT, Krasik E, Chen LM, Powell CB, Crawford B, Zaloudek CJ. Multistep level sections to detect occult fallopian tube carcinoma in risk-reducing salpingo-oophorectomies from women with BRCA mutations: implications for defining an optimal specimen dissection protocol. Am J Surg Pathol. 2009;33:1878–85. doi: 10.1097/PAS.0b013e3181bc6059. http://dx.doi.org/10.1097/PAS.0b013e3181bc6059. [DOI] [PubMed] [Google Scholar]
- 10.Maehle L, Apold J, Paulsen T, Hagen B, Løvslett K, Fiane B, et al. High risk for ovarian cancer in a prospective series is restricted to BRCA1/2 mutation carriers. Clin Cancer Res. 2008;14:7569–73. doi: 10.1158/1078-0432.CCR-08-0112. http://dx.doi.org/10.1158/1078-0432.CCR-08-0112. [DOI] [PubMed] [Google Scholar]
- 11.Carlson JW, Miron A, Jarboe EA, Parast MM, Hirsch MS, Lee Y, et al. Serous tubal intraepithelial carcinoma: its potential role in primary peritoneal serous carcinoma and serous cancer prevention. J Clin Oncol. 2008;26:4160–5. doi: 10.1200/JCO.2008.16.4814. http://dx.doi.org/10.1200/JCO.2008.16.4814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kauff ND, Domchek SM, Friebel TM, Robson ME, Lee J, Garber JE, et al. Risk-reducing salpingo-oophorectomy for the prevention of BRCA1- and BRCA2-associated breast and gynecologic cancer: a multicenter, prospective study. J Clin Oncol. 2008;26:1331–7. doi: 10.1200/JCO.2007.13.9626. http://dx.doi.org/10.1200/JCO.2007.13.9626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hill KA, Rosen B, Shaw P, Causer PA, Warner E. Incidental MRI detection of BRCA1-related solitary peritoneal carcinoma during breast screening--A case report. Gynecol Oncol. 2007;107:136–9. doi: 10.1016/j.ygyno.2007.05.037. http://dx.doi.org/10.1016/j.ygyno.2007.05.037. [DOI] [PubMed] [Google Scholar]
- 14.Powell CB, Kenley E, Chen LM, Crawford B, McLennan J, Zaloudek C, et al. Risk-reducing salpingo-oophorectomy in BRCA mutation carriers: role of serial sectioning in the detection of occult malignancy. J Clin Oncol. 2005;23:127–32. doi: 10.1200/JCO.2005.04.109. http://dx.doi.org/10.1200/JCO.2005.04.109. [DOI] [PubMed] [Google Scholar]
- 15.Kauff ND, Satagopan JM, Robson ME, Scheuer L, Hensley M, Hudis CA, et al. Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med. 2002;346:1609–15. doi: 10.1056/NEJMoa020119. http://dx.doi.org/10.1056/NEJMoa020119. [DOI] [PubMed] [Google Scholar]
- 16.Scheuer L, Kauff N, Robson M, Kelly B, Barakat R, Satagopan J, et al. Outcome of preventive surgery and screening for breast and ovarian cancer in BRCA mutation carriers. J Clin Oncol. 2002;20:1260–8. doi: 10.1200/JCO.2002.20.5.1260. http://dx.doi.org/10.1200/JCO.20.5.1260. [DOI] [PubMed] [Google Scholar]
- 17.Colgan TJ, Murphy J, Cole DE, Narod S, Rosen B. Occult carcinoma in prophylactic oophorectomy specimens: prevalence and association with BRCA germline mutation status. Am J Surg Pathol. 2001;25:1283–9. doi: 10.1097/00000478-200110000-00009. http://dx.doi.org/10.1097/00000478-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Meeuwissen PA, Seynaeve C, Brekelmans CT, Meijers-Heijboer HJ, Klijn JG, Burger CW. Outcome of surveillance and prophylactic salpingo-oophorectomy in asymptomatic women at high risk for ovarian cancer. Gynecol Oncol. 2005;97:476–82. doi: 10.1016/j.ygyno.2005.01.024. http://dx.doi.org/10.1016/j.ygyno.2005.01.024. [DOI] [PubMed] [Google Scholar]
- 19.Tobacman JK, Greene MH, Tucker MA, Costa J, Kase R, Fraumeni JF., Jr Intra-abdominal carcinomatosis after prophylactic oophorectomy in ovarian-cancer-prone families. Lancet. 1982;2:795–7. doi: 10.1016/s0140-6736(82)92681-2. http://dx.doi.org/10.1016/S0140-6736(82)92681-2. [DOI] [PubMed] [Google Scholar]
- 20.Dubeau L. The cell of origin of ovarian epithelial tumours. Lancet Oncol. 2008;9:1191–7. doi: 10.1016/S1470-2045(08)70308-5. http://dx.doi.org/10.1016/S1470-2045(08)70308-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pentheroudakis G, Pavlidis N. Serous papillary peritoneal carcinoma: unknown primary tumour, ovarian cancer counterpart or a distinct entity? A systematic review. Crit Rev Oncol Hematol. 2010;75:27–42. doi: 10.1016/j.critrevonc.2009.10.003. http://dx.doi.org/10.1016/j.critrevonc.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 22.Levine DA, Argenta PA, Yee CJ, Marshall DS, Olvera N, Bogomolniy F, et al. Fallopian tube and primary peritoneal carcinomas associated with BRCA mutations. J Clin Oncol. 2003;21:4222–7. doi: 10.1200/JCO.2003.04.131. http://dx.doi.org/10.1200/JCO.2003.04.131. [DOI] [PubMed] [Google Scholar]
- 23.Chapman JS, Powell CB, McLennan J, Crawford B, Mak J, Stewart N, et al. Surveillance of survivors: follow-up after risk-reducing salpingo-oophorectomy in BRCA 1/2 mutation carriers. Gynecol Oncol. 2011;122:339–43. doi: 10.1016/j.ygyno.2011.04.004. http://dx.doi.org/10.1016/j.ygyno.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 24.Iavazzo C, Gkegkes ID, Vrachnis N. Early recurrence of early stage endometrioid endometrial carcinoma: possible etiologic pathways and management options. Maturitas. 2014;78:155–9. doi: 10.1016/j.maturitas.2014.04.009. http://dx.doi.org/10.1016/j.maturitas.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 25.Sitzmann JV, Wiebke EA. Risk-Reducing Appendectomy and the Elimination of BRCA1 -Associated Intraperitoneal Cancer. JAMA Surg. 2013;148:285–91. doi: 10.1001/jamasurg.2013.1006. http://dx.doi.org/10.1001/jamasurg.2013.1006. [DOI] [PubMed] [Google Scholar]
- 26.Chene G, Dauplat J, Radosevic-Robin N, Cayre A, Penault-Llorca F. Tu-be or not tu-be: that is the question… about serous ovarian carcinogenesis. Crit Rev Oncol Hematol. 2013;88:134–43. doi: 10.1016/j.critrevonc.2013.03.004. http://dx.doi.org/10.1016/j.critrevonc.2013.03.004. [DOI] [PubMed] [Google Scholar]