Introduction
Intracranial lipomas are considered to be choristomas rather than neoplasms or even hamartomas, as they are histologically composed of fat cells but anatomically misplaced. Intracranial lipomas are located in the midline in 90% of cases and supratentorial in 80%, with the dorsal pericallosal region being the most common site [1]. More than half of intracranial lipomas are associated with congenital malformations such as agenesis/dysgenesis of the corpus callosum [2]. Most intracranial lipomas are asymptomatic and are detected incidentally, however some cases present with headache and seizures [3].
Case Report
A 22 year old male patient, presented with features suggestive of complex partial seizures. Neurological examination was unremarkable and the patient was subjected to an magnetic resonance imaging (MRI) of the brain. The MR examination revealed a curvilinear shaped area of altered signal intensity surrounding the splenium of corpus callosum which appeared hyperintense on both T1 and T2 weighted images. There was a thin rim of signal loss around this lesion on all sequences, consistent with calcification (Fig. 1, Fig. 2). This appearance on MR was consistent with Lipoma of the Corpus Callosum. The diagnosis was confirmed on fat suppressed T1 weighted image (Fig 3) in which the lesion showed signal loss confirming the diagnosis.
Fig. 1.

T1 weighted mid sagittal MR of the brain showing a curvilinear bright hyperintense area around splenium of the corpus callosum suggestive of a lipoma, there is a thin area of signal loss around it, which represents calcification
Fig. 2.
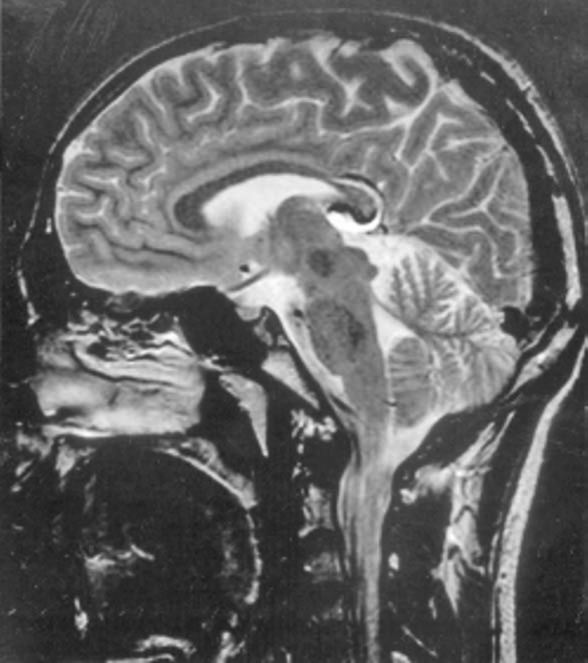
T2 weighted mid sagittal MR of the brain showing a curvilinear hyperintense area around the splenium of the corpus callosum suggestive of a lipoma, there is a thin area of signal loss around it which represents calcification
Fig. 3.

T1 weighted fat suppressed mid sagittal MR of the brain showing suppression of signals from the curvilinear area around the splenium of the corpus callosum which appeared hyperintense on T1 & T2 weighted images, confirming the presence of fat in the lesion.
Discussion
Intracranial lipomas are not true neoplasms, but congenital malformations which represent persistence of menix primitiva, a mesenchymal neural crest derivative [4]. Approximately 30% of intracranial lipomas are found in the region of corpus callosum and half of these are associated with various degrees of callosal dysgenesis [1]. Other sites of intracranial lipomas are optic chiasma and the basal cisterns, mainly involving the circurnesencephalic, interpeduncular and cerebello-pontine cisterns. Infratentorial lipomas are seen in the CP angle cisterns. Pericallosal lipomas have an incidence of 1: 1700 and are classified into two types the anteriorly located bulky tubulo-nodular, which have a mean diameter of more than 20 mm and the posteriorly located ribbon like curvilinear with mean diameter of more than 10 mm [3].
The first type is frequently associated with forebrain and rostral callosal abnormalities while the second type is associated with a normal corpus callosum [4]. Curvilinear type of pericallosal lipomas can be associated with fronto-nasal dyplasias [5] and Goldenhar syndrome [6]. In 50% of cases there is no clinical expression and patients are asymptomatic. In rest of the cases, presentation is usually in the form of headache, seizures and behavioural disturbances which are usually due to associated anomalies of the corpus callosum. Infratentorial lipomas can encompass the VII and VIII nerves, producing deafness and vertigo.
Imaging is the main stay in the diagnosis of intracranial lipomas. Plain radiographs of the skull may show curvilinear calcification especially in the tubulonodular variety. On CT scan the mass appears smoothly demarcated and hypodense with density of 50 to 100 negative HU. It is often marginated by nodular or curvilinear calcification. On MRI, lipomas appear homogenously hyperintense on both T1 and T2 weighted images, with areas of low signal intensity due to peripheral calcification. The diagnosis is often confirmed on fat suppressed images which show signal loss due to suppression of fat. Sometimes central flow voids representing pericallosal arteries coursing through the substance of tumour are seen.
Treatment of intracranial lipomas is surgical but often difficult, as many nerves and vessels traverse it and it has little or no effect on seizures.
Conflicts of Interest
None identified
References
- 1.Hagga John R, Lanzieri Charles F, Gilkeson Robert C. CT and MR imaging of the whole body. In: Kieffer Stephen A, Chang Ja-Kwei., editors. Intracranial neoplasms. 4th ed. Mosby; St Louis: 2003. pp. 171–173. [Google Scholar]
- 2.Osborne Annie G. Disorders of Neural tube closure. 1st ed. Mosby; St Louis: 1994. Diagnostic Neuroradiology. [Google Scholar]
- 3.Gomez Gosalvez FA. Intracranial lipomas in paediatrics: a retrospective study of 20 cases. Revista De Neurologia. 2003;16:515–521. [PubMed] [Google Scholar]
- 4.Kim Tate Hoon, joh Joon Hee, Miyoung Kim, Minkim Yan, Han Kwang Soo. Foetal pericallosal lipoma: US and MR findings. Korean Journal of Radiology. 2002;3:140–143. doi: 10.3348/kjr.2002.3.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alzouma Mohammad A., Ibrahim A, Alorainya Muneera Al, Husainb, Ruhaimic Khalid AL. Multiple Pericallosal Lipomas in two siblings with Frontonasal Dysplasia. American Journal of Neuroradiology. 2002;23:730–731. [PMC free article] [PubMed] [Google Scholar]
- 6.Thommem L, Bubl R, Fliegel CP. Lipoma of the corpus callosum as a constituent of Goldenhar syndrome. Monatsschr Kiderheilkd. 1986;134:541–543. [PubMed] [Google Scholar]


