Introduction
Meningococcal infection has been recognized as a serious problem for almost 200 years. Vieusseux gave the first description of meningococcal meningitis in 1805 when an outbreak swept through Geneva [1]. The causative agent, Neisseria meningitidis was identified in 1887 [2]. In general population, approximately 10% carry meningococcal bacteria in throat and nose without any ill effects [3]. In rare instances meningococci can overcome body's natural defense mechanisms and cause serious disease. It causes two life threatening diseases: meningococcal meningitis and fulminant meningococcemia which often occur together. Despite effective antibiotics and partially effective vaccines, Neisseria meningitides is still a leading cause of meningitis and fatal sepsis.
Definition
Meningitis is defined as an inflammatory response to bacterial infection of leptomeninges (pia-arachnoid) and the sub-arachnoid space. Although several bacteria can cause meningitis (Table 1) [5], Neisseria meningitidis is the most important because of its potential to cause epidemics.
Table 1.
Bacterial meningitis – Age dependent etiologic agents (in percent)
| Organism | Neonates (≤ 1mth) | Children (1 mth −15 yrs) | Adults (15-60 yrs) | Adults (>60 yrs) |
|---|---|---|---|---|
| Haemophilus influenzae | 4 | 52 | 5 | 20 |
| Neisseria meningitides | 1 | 27 | 30 | 12 |
| Streptococcus pneumoniae | 3 | 15 | 40 | 10 |
| Gram-negative bacilli | 50 | 2 | 5 | 20 |
| Gp B Streptococci | 35 | 2 | 5 | 9 |
| Staphylococci | 5 | 1 | 10 | 4 |
| Listeria monocytogenes | 2 | 1 | 5 | 25 |
Meningococcemia is meningococcal septicemia when the bacteria circulate and multiply in blood and involve multiple organs. It can cause multi-organ failure and severe disability or death in up to 50% of cases.
Epidemiology
Meningococcal disease can occur as a sporadic case, institution based focal outbreak, or an large epidemic. It has seasonal variation with majority of cases occurring during winter and early spring [6]. Serogroup A, B, and C are responsible for most cases of meningococcal meningitis world wide with serogroups A and C being predominant in Asia and Africa [7]. Serogroup A strain has caused large epidemics of meningococcal meningitis in the first half of the twentieth century and are now associated with recurring epidemics in sub Saharan Africa and the developing world. Serogroups B and C cause most cases of meningococcal meningitis in Europe and Americas. In recent years the number of cases due to serogroup Y and W-135 have been increasing in the western world.
Prevalence and incidence
Internationally, 5 lac cases of meningococcal meningitis occur each year with 50,000 deaths excluding periodic epidemics [8]. The highest burden is in sub-Saharan Africa, where it occurs in a cyclic mode. The proportion of cases among adolescents and young adults has increased in the recent years with 28% of affected persons being in the age group of 12-29 years in one of the studies [6]. In India, Meningococcal disease is endemic in Delhi and sporadic cases occurred in Haryana, Uttar Pradesh, Rajasthan, Sikkim, Gujarat, West Bengal and Orissa. The latest epidemic from 29 Mar 2005 in Delhi accounted for 214 cases including 16 deaths [9].
Relevance to Armed Forces
Meningococcal meningitis has special relevance in the Armed Forces due to overcrowded living in regimental centers and during wars. New military recruits have higher risk of meningococcal meningitis than general population or other military personnel [10]. Only sporadic cases 15,16 & 30 have been reported from Armed Forces in 2001, 2002 and 2003.
Etiologic Agent
Meningococci are gram–negative aerobic diplococci. Meningococci are classified by serologic typing on the basis of structural differences in capsule (serogroup), major outer-membrane protein (OMP), porins (serotype); opacity associated proteins or OMPs (serosubtype), lipooligosaccharide or LOS, (immunotype), and enzyme electrophoretic pattern (electrophoretic type, ETs). Identification of strain is done by pulsed field gel electrophoresis and identification of bacterial genomic sequence by polymerase chain reaction (PCR).
The serogroup classification of meningococci is done depending on the antigenicity of capsular polysaccharides [11]. At least 13 subtypes of N. meningitidis have been described: A, B, C, D, E, H, I, K, L, W-135, X, Y and Z. Of these, five serogroups (N. meningitides A, B, C, Y and W-135) are recognized to cause epidemics and are responsible for >90% of cases [8]. There are several factors, which determine the virulence of the bacteria including [11], Capsular polysaccharide, Outer-membrane proteins, Lipooligosaccharide (LOS), Bacterial pili, Opacity associated proteins (Opa, Opc proteins), Amount of blebbing or vesiculation of outer membrane, Specific nutrient acquisition factors (e.g. iron acquiring mechanism) [12].
Host Factors:
Meningococcal meningitis commonly affects children >3 years and young adults. It rarely affects people older than 50 years. Individuals with congenital deficiencies in complement components C5 to C9 cannot assemble the membrane-attack complex (MAC) needed to kill Neisseria and are predisposed to infection. Deficiency of properdin (a component of alternative complement pathway), functional or anatomical asplenia, and HIV infection also make individuals susceptible. Immunocompetent individuals can be affected by a virulent strain or when there is disruption of integrity of respiratory mucosa due to viral infections or tobacco smoking.
Environmental Factors:
Important environmental factors include overcrowding as in nursery schools, college campuses and military installations, urban residence, exposure to tobacco smoke and residence in the same household with a person who has meningococcal disease or is a carrier.
Pathogenesis
Spread is by direct contact or droplet infection. The incubation period averages 3-4 days (range 1-10 days) during which the person is infective. Meningococci colonize the upper respiratory tract and nonciliated mucosal cells internalize them. They traverse the mucosal cells, enter the submucosa and in approximately 10-20% cases make their way to the bloodstream. In the vascular compartment, they may be killed by the bactericidal antibodies, complement and phagocytic cells or may multiply and initiate bacteremic phase. The bacteria may seed local sites such as the meninges, joints or the pericardium or multiply in the bloodstream, causing meningococcemia with petechiae.
Upto one third of patients present with meningitis without signs of sepsis. Meningococcal pili may bind CD46, a complement regulatory protein that is expressed by the choroid plexus and meningeal epithelia and a vigorous inflammatory response ensues generally confined to the subarachnoid space and contiguous structures. Release of local inflammatory cytokines and nitric oxide causes breakdown of blood brain barrier, edema, induction of cellular apoptosis, coagulation, blockage of vessels and ischemia. Microscopically there is intense infiltration of meninges, blood vessels, Virchow Robin spaces and perivascular parenchyma with polymorphonuclear and mononuclear inflammatory cells. The resultant thickening of blood vessels leads to thrombosis, occlusion, cerebral infarction and focal deficits. Purulent exudates accumulate at the base of the brain and over the convexicity of the cerebral cortex. Increased intracranial pressure occurs due to blockage of CSF pathways by exudates.
Fulminant meningococcemia differs from other forms of septic shock by the prominence of hemorrhagic skin lesions (petechiae, purpura) and development of DIC. The dominant pro-inflammatory molecule in the meningococcal cell wall is the endotoxin or LOS (lipooligosaccharide) which stimulates monocytes, neutrophils, endothelial cells and promotes release of pro-inflammatory cytokines (tumor necrosis factor, IL-1, IL-8, interferon gamma). In addition, meningococci can invade the vascular endothelium which produces molecules with procoagulant and adhesive properties for leukocytes. Both platelets and leukocytes contribute to formation of microthrombi and vascular injury. Thrombosis of small to midsized arteries produces peripheral necrosis and gangrene necessitating limb or digit amputation.
Clinical Manifestations
Invasive meningococcal infection can present as pyogenic meningitis, meningitis with meningococcemia or meningococcemia without meningitis. Rash is probably the most important clue to the diagnosis of meningococcal meningitis.
During early prodromal stage, a patient may present with a non-specific febrile illness. Acute onset is characterized by severe headache, fever, nausea, vomiting, photophobia, and neck stiffness. Cerebral dysfunction is very early and is manifested by confusion, delirium, declining level of consciousness that ranges from lethargy to coma. Many manifest a diffuse eythematous maculopapular rash. As it evolves, petechiae and purpura appear primarily on the trunk and lower extremities (Fig. 1). Infants have a slower onset with non-specific signs and without stiffness of neck. Irritability and projectile vomiting are a common presenting feature. In children and adults, the classical signs of meningeal irritation are nuchal rigidity, Kernig's and Brudzinski's sign.
Fig. 1.

Meningococcal skin rash on lower limb. Some of the petechiae have coalesced to form ecchymotic patches. There is impending gangrene of digits. (Photograph from personal collection of Lt Col AS Kashyap)
Neurological complications include generalized and focal seizures in up to 40% cases. Generalized seizures occur early and are due to fever, metabolic derangement or toxic factors. Focal seizures are more common after 4 to 10 days and are caused by arterial thrombosis, cortical vein thrombosis or abscess formation. Cranial nerve palsies specially III, VI, VII and VIII occur due to purulent exudates in arachnoids and sheaths of these nerves. The complications of meningococcal meningitis are summarized in Table 2.
Table 2.
Complications of Meningococcal meningitis. High mortality rate in meningococcal meningitis is due to numerous potential complications.
| Meningococcal meningitis | Fulminant meningococcemia |
|---|---|
| Early:- | |
| Seizures | Loss of skin, digits due |
| Raised intracranial pressure | to ischemic necrosis and |
| Hydrocephalus | infection |
| Cerebral venous thrombosis | Shock |
| Cerebral edema | Multiorgan failure |
| Hemiparesis | |
| Late:- | |
| Communicating hydrocephalus | |
| Subdural effusions in children | |
| Deafness | |
| Cranial nerve palsies | |
| Mental retardation | |
Meningococcemia is characterized by an abrupt onset of fever, chills, nausea, vomiting, myalgias and petechial or purpuric rash. Prostration is common. It is often associated with rapid onset of hypotension, acute adrenal hemorrhage (Waterhouse- Friderichsen Syndrome) [13] and multiorgan failure. The most distinctive feature is rash (Fig 1). The petechiae may coalesce into hemorrhagic bullae or may ulcerate. Patients with severe coagulopathy may develop ischemic extremities or digits. Approximately 10 to 30% of patients with meningococcal disease have meningococcemia without meningitis. In most patients with fulminant meningococcemia CSF may be normal and CSF culture negative. Absence of meningitic signs in a patient with meningococcemia is a poor prognostic sign. It suggests that the bacteria have multiplied so rapidly in the blood that meningeal seeding and inflammation could not occur. Most of these patients also lack evidence of an acute-phase response i.e. they have normal erythrocyte sedimentation rates and the C-reactive protein concentration in blood is low. The clinical spectrum of severe meningococcal disease is summarized in Fig. 2.
Fig. 2.

The Spectrum of Severe Meningococcal disease. The two major syndromes are meningitis and meningococcemia. Both usually coexist. The typical features of meningitis are absent in neonates and infants.
Chronic meningococcemia is a rare syndrome of prolonged, intermittent fever, rash, arthralgias and headaches that can last for weeks to months [13]. The rash may be maculopapular or occasionally petechial. Splenomegaly may develop. Untreated or when treated with glucocorticoids, chronic meningococcemia may evolve into meningitis, fulminant meningococcemia or endocarditis.
Arthritis [14] occurs in 10% of patients with meningococcal disease. An arthritis developing during the first few days reflects direct meningococcal invasion of the joint. Arthritis beginning later is due to immune complex deposition. Primary meningococcal pneumonia occurs in 5-15% of adults [15], often military recruits and is due to serogroup Y. Meningococcal pericarditis, endocarditis and otitis media are occasionally seen. Primary meningococcal conjunctivitis [16] can be complicated by meningococcemia. Meningococcal urethritis [17] has been reported in individuals who practice oral sex.
Investigations
-
1
Examination of CSF: CSF examination confirms pyogenic meningitis. The typical CSF picture includes [18] an increased opening pressure (>200 mm water), turbid CSF (denoting >400 cells/mm3), increased white cell count (predominantly polymorphonuclear), decreased glucose level (<45 mg%), decreased CSF to serum glucose ratio of < 0.3, increased protein level (>45 mg%) and gram negative diplococci
-
2
Bacteriological culture: The definitive diagnosis is established by recovering N meningitides, its antigens or its DNA from blood (positive in 50%), CSF (positive in 75%) or skin lesions. Meningococci grow best on chocolate blood agar at 35°C in an atmosphere that contains 5 to 10% CO2. Specimens should be plated without delay. At least three sets of blood culture should be obtained.
-
3
Gram's stain of CSF: reveals intra-or extracellular organisms in 85% of patients with meningococcal meningitis [19].
-
4
Non-culture methods: These are commercially available kits, which detect polysaccharide antigen or it's DNA in CSF. These are rapid and specific. However, false negative results are common.
-
5
Serological testing: The latex agglutination test or ELISA for meningococcal polysaccharide can be used, as part of evaluation but is less sensitive. PCR amplification of bacterial DNA in buffy coat or CSF samples is more sensitive and can detect group specific antigens [20]. The IS-1106 PCR and detection of nspA gene is a rapid and sensitive test for confirmation of diagnosis.
-
6
Imaging studies: Indication for performing CT / MRI scan prior to lumber puncture include age more than 60 yrs, features of raised intracranial tension (altered level of consciousness, papilledema, dilated non reacting pupil, VI cranial nerve palsy), focal neurological deficit and seizures [21]. It may show meningeal enhancement, cerebral edema, cerebral ischemia and infarcts, hydrocephalus, aqueductal stenosis, subdural effusion or empyema.
Treatment
Meningococcal disease is potentially fatal. At presentation, meningitis due to N meningitides may be impossible to differentiate from other pyogenic meningitis. Therefore empirical therapy in adults with either ceftriaxone (2 g intravenously every 12 h) or cefotaxime (2 g intravenously every 4 h) is recommended. Ampicillin should be added in neonates and elderly individuals. An algorithm for approach to a suspected case of bacterial meningitis is shown in Fig. 3.
Fig. 3.
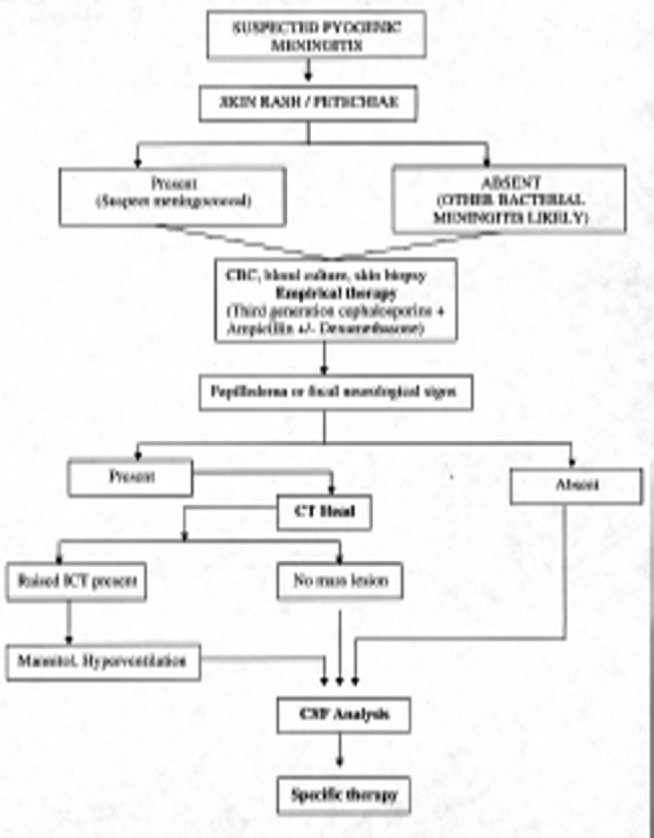
Algorithm for initial management of suspected meningitis. Empirical therapy should be started as soon as diagnosis of pyogenic meningitis is suspected without waiting for definitive diagnosis. Pre-lumbar puncture CT scan head is not indicated in all cases.
Once diagnosis of meningococcal meningitis has been made, appropriate changes in antibiotic are made. Penicillin G [18 to 24] million units intravenously per day is the first line of therapy. However, there is increasing prevalence of meningococcal disease with reduced susceptibility to penicillin. In such situations, a third generation cephalosporin, such as cefotaxime (2 g intravenously every 4 h) or ceftriaxone (2 g intravenously every 12 h) is the next choice. Other alternatives include meropenem (1 g intravenously every 8 h), and chloramphenicol (75 to 100 mg/kg per day) specially if patient is allergic to penicillin. Recently chloramphenicol resistant meningococci have been reported from Vietnam and France [22]. The newer fluoroquinolones gatifloxacin, moxifloxacin, and gemifloxacin have excellent in vitro activity against N. meningitides and appear promising in animal models. Patients with meningococcal meningitis should be given antimicrobial therapy for at least 7 days (usually given for 10-14 days). The use of glucocorticods in adult pyogenic meningitis is controversial. However many administer dexamethasone, 10 mg intravenously 15 to 20 min before the first antibiotic dose and then every 6 h for 4 days specially in meningitis due to S pneumoniae and H influenzae [23]. It is not recommended if septic shock is present.
Patients with fulminant meningococcemia often experience diffuse leakage of fluid into extravascular spaces, shock and multiple organ dysfunction. Myocardial depression may be prominent. Supportive therapy includes vigorous fluid resuscitation, elective ventilation and vasopressors. Some authorities recommend hemodialysis or hemofiltration. Fresh frozen plasma is often given to patients who are bleeding extensively or who have severely deranged clotting parameters. Patients with fulminant meningococcemia in whom shock persists should receive supplemental glucocorticoid treatment (hydrocortisone, 1 mg/kg every 6 h) pending tests of adrenal reserve. Activated protein C (drotrecogin alfa, Xigris) is approved for use in patients with severe sepsis and dysfunction of more than one organ (APACHE II score, <25). Patients with meningococcemia may represent a group most likely to benefit from activated protein C. The recommended dose is 24 g/kg per hour (2 g intravenously every 4 h), given as a continuous intravenous infusion for 96 h.
Prognosis
Most cases of meningococcal meningitis recover completely if appropriate antibiotic is promptly instituted. Prognosis is much worse if infection has a septicemic component. The poor prognostic factors include [24]: Shock, Presence of focal deficits, Mental obtundation or coma, Purpuric or ecchymotic rash, Age of >60 years, Absence of meningitic signs, Low or normal blood leukocyte count, Presence of anemia, Thrombocytopenia, Low blood concentrations of Antithrombin or proteins S and C, High blood levels of plasminogen activator inhibitor 1 (PAI-1), Low erythrocyte sedimentation rate (or C-reactive protein level). The fatality with treatment is 13% and 50-90% without treatment. Sequelae are seen in 3-4% of survivors mostly in children.
Prevention
Meningococcal Polysaccharide Vaccines are available for immunoprophylaxis. A single injection of quadrivalent meningococcal polysaccharide vaccine (serogroups A, C, W-135 and Y) can be given to immunocompetent adults. The duration of vaccine induced immunity in adults is <5 years. There is currently no effective vaccine for serogroup B. Monocomponent vaccines are also available. Children >3 months of age can be vaccinated to prevent serogroup A disease, but multiple doses are required. Prophylactic quadrivalent polysaccharide is indicated at times of meningococcal epidemic, persons with complement or properdin deficiency, persons with sickle cell anemia, asplenia, or splenectomy. Vaccination is also recommended for military recruits, pilgrims on Hajj, and individuals traveling to sub Saharan Africa during dry months.
New conjugated meningococcal vaccines utilizing capsular oligosaccharide and polysaccharide components A, C, Y and W-135) are being developed [25]. These vaccines are based on covalent linkage of the polysaccharide to a carrier protein, which converts the polysaccharide to thymus dependent antigen enhancing IgG anticapsular antibodies and memory B cells. The identification of new meningococcal protective antigens and the development of better meningococcal vaccines are areas of continued research and hold promise for the prevention of disease due to N meningitides.
Antimicrobials commonly used for chemoprophylaxis are rifampicin, ciprofloxacin, ofloxacin, azithromycin and ceftriaxone (Table 3).
Table 3.
Chemoprophylaxis against meningococcal disease
| Drug and age group | Dosage |
|---|---|
| Rifampicin (oral) | |
| Children<1month | 5mg/kg of body weight every 12 hr for 2 days |
| Children ≥ 1month | 10 mg/kg every 12 hr for 2 days |
| Adults | 600 mg every 12 hr for 2 days |
| Ciprofloxacin (oral) | 500 mg given in a single dose (adults) |
| Ceftriaxone | |
| Children<15 yr | 125 mg given in a single intramuscular dose |
| Children ≥ 15 yr/Adults | 250 mg given in a single intramuscular dose |
| Oflaxacin (oral) | 400 mg, given in a single dose (adults) |
| Azithromycin (oral) | 500 mg, given in a single dose (adults) |
An outbreak of meningococcal disease is defined as the occurrence of three or more cases in <3 months in persons who have a common affiliation or reside in the same area but who are not close contacts of one another. Also, the primary disease attack rate must be >10 cases per 100,000 persons, and strains of N meningitidis must be of the same type [11]. Mass vaccination should be considered when such outbreaks occur. Mass chemoprophylaxis is not recommended during epidemics. But, since the attack rate of meningococcal disease is > 400 fold, more among close contacts of cases than general population, all close contacts of a case should receive chemoprophylaxis to control school or other institution-based outbreaks.
References
- 1.Vieusseux M. Memoire sur la maladie qui a regne a Geneve au printemps de 1805. J Med Chir Pharmacol. 1805;11:163. [Google Scholar]
- 2.Weichselbaum A. Ueber die Aetiologie der akuten meningitis cerebrospinalis. Fortschr Med. 1887;5:573–583. [Google Scholar]
- 3.Caugant DA, Hoiby EA, Magnus P. Asymptomatic carriage of Neisseria meningitidis in randomly sampled population. J Clin Microbiol. 1994;32:323–330. doi: 10.1128/jcm.32.2.323-330.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roos KL, Tunkel AR, Scheld WM. Acute Bacterial Meningitis in Children and Adults. In: Mandell GL, Bleck TP, editors. Vol. 3. Lippencott- Raven; Philadelphia: 1997. pp. 335–401. (In Infections of Central Nervous System). [Google Scholar]
- 6.Rosenstein NE, Perkins BA, Stephens DS. The changing epidemiology of meningococcal disease in the United States, 1992–1996. J infect Dis. 1999;180(6):1894–1901. doi: 10.1086/315158. [DOI] [PubMed] [Google Scholar]
- 7.Schwartz B, Moore PS, Broome CV. Global epidemiology of meningococcal disease. Clin Microbiol Rev. 1989;2(Suppl):S118–S124. doi: 10.1128/cmr.2.suppl.s118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gondim FAA, Singh MK, Croul SE, Singh NP. Meningococcal Meningitis. eMedicine 09 March 2005. 23 May 2005 [Google Scholar]
- 9.World Health Organization Meningococcal disease in India 2005. WHO Meningococcal disease in India.htm. 23 May 2005 [Google Scholar]
- 10.Brundage JF, Zollinger WD. Evolution of meningococcal disease epidemiology in the US Army. In: Vedros NA, editor. Vol I. CRC press; Boca Raton Fla: 1987. pp. 5–23. (Evolution of meningococcal disease). [Google Scholar]
- 11.Stephens DS, Munford RS, Wetzler LM. Meningococcal infections. In: Kasper DL, Braunwald E, Fauci AS, editors. Harrison's Principles of Internal Medicine. 16th. McGraw-Hill; 2005. pp. 849–855. [Google Scholar]
- 12.Pettersson A, Poolman JT, van der Ley P, Tommassen J. Response of Neisseria meningitides to iron limitation. Antonie Van Leeuwenhock. 1997;71:139–146. doi: 10.1023/a:1000179301748. [DOI] [PubMed] [Google Scholar]
- 13.Gold R. Clinical aspects of meningococcal disease. In: Vedross NA, editor. Vol. 2. CRC Press; Boca Ratron Fla: 1987. pp. 69–97. (Evolution of meningococcal disease). [Google Scholar]
- 14.Schaad UB. Arthritis in disease due to Neisseria meningitides. Rev Infect Dis. 1980;2:880–888. doi: 10.1093/clinids/2.6.880. [DOI] [PubMed] [Google Scholar]
- 15.Racoosin JA, Whitney CG, Conver C, Diaz PS. Serogroup Y Meningococcal disease in Chicago, 1991–1997. JAMA. 1998;280:2094–2098. doi: 10.1001/jama.280.24.2094. [DOI] [PubMed] [Google Scholar]
- 16.Barquet N, Gasser I, Domingo P, Moraga FA, Macaya A, Elcuaz R. Primary meningococcal conjunctivitis: report of 21 patients and review. Rev infect Dis. 1990;12:838–847. doi: 10.1093/clinids/12.5.838. [DOI] [PubMed] [Google Scholar]
- 17.Miller M, Millikin P, Griffin PS, Saxton RA, Yousuf M. Neisseria meningitides urethritis: A case report. JAMA. 1979;242:1656–1657. [PubMed] [Google Scholar]
- 18.Durand ML, Calderwood SB, Weber DJ. Acute Bacterial Meningitis in Adults: a review of 493 episodes. N Engl J Med. 1993;328:21–28. doi: 10.1056/NEJM199301073280104. [DOI] [PubMed] [Google Scholar]
- 19.Dunbar SA, Eason RA, Musher DN, Clarridge JE. Microscopic examination and broth culture of cerebrospinal fluid in diagnosis of meningitis. J Clin Microboil. 1998;36:1617–1620. doi: 10.1128/jcm.36.6.1617-1620.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ni H, Knight AL, Cartwright K. Polymerase chain reaction for diagnosis of Meningococcal menigitis. Lancet. 1992;340:1432–1434. doi: 10.1016/0140-6736(92)92622-m. [DOI] [PubMed] [Google Scholar]
- 21.Hasbun R, Abrahams J, Jekel J, Quagliarello VJ. Computed Tomography of the head before lumber puncture in adults with suspected meningitis. N Engl J Med. 2001;345:1727–1733. doi: 10.1056/NEJMoa010399. [DOI] [PubMed] [Google Scholar]
- 22.Galimand M, Gerbaud G, Guibourdenche M, Riou JY, Courvalin P. High-level Chloramphenicol resistance in Neisseria meningitides. N Engl J Med. 1998;339:868–874. doi: 10.1056/NEJM199809243391302. [DOI] [PubMed] [Google Scholar]
- 23.Ganz JD, Beek DV. Dexamethasone in adults with bacterial meningitis. N Eng J Med. 2002;347:1549–1556. doi: 10.1056/NEJMoa021334. [DOI] [PubMed] [Google Scholar]
- 24.Beek van de D, Gans JD, Spanjaard L, Weisfelt M, Reitsma JB, Vermeulen M. Clinical Features and Prognostic Factors in Adults with Bacterial Meningitis. N Engl J Med. 2004;351:1849–1859. doi: 10.1056/NEJMoa040845. [DOI] [PubMed] [Google Scholar]
- 25.McDonald NE, Halporin SA, Law BJ et al: Induction of Immunologic memory by conjugated vs plain Meningococcal C polysaccharide vaccine in toddlers — a randomized controlled [DOI] [PubMed]
Uncited Reference
- 4.Rosenstien NE, Perkins BA, Stephens DS, Popovic T, Hughes JM. Meningococcal Disease. N Engl J Med. 2001;344:1378–1388. doi: 10.1056/NEJM200105033441807. [DOI] [PubMed] [Google Scholar]


