Abstract
A total of 40 patients with limb amputations were included in the present study aimed at evaluating the psychological status of amputees. All patients filled a specially designed proforma and the following psychological questionnaires: General Health Questionnaire, Carroll Rating Scale for Depression, State-Trait Anxiety Inventory, Michigan Alcoholism Screening Test and Disability Assessment Questionnaire. Analysis of the results showed that 29 (72.5%) of the amputees had psychiatric disorders and this number had reduced to 20 (50%) after therapy. The difference was statistically significant. Psychiatric treatment also resulted in a statistically significant reduction in level of depression as measured by Carroll Rating scale for Depression. The amputees had the highest score on vocational subscale of Dysfunction Analysis Questionnaire. Short term psychiatric treatment was found to be very useful in treating psychiatric morbidity and depression in amputees.
Key Words: Amputees, Depression, Psychiatric morbidity
Introduction
Amputation, at present, is mostly traumatic but it may be elective as in cases of Buerger's disease, gangrene, malignancy etc. With the loss of a limb, the individual's body image is distorted and he thinks that he is no longer a complete human being. He loses all the practical and expressive functions, which were formerly carried out by means of the limbs. For sometime he feels helpless. Many of them imagine in the early weeks of lower limb amputation that they will never be able to walk again. Apart from loss of physical functions, the amputee loses hopes and aspirations for the future; his plans and ambitions get shattered. Thus, he hasn't just lost his limb, but has lost a slice of his world and a large part of his future. It was strongly felt that even today there might be many amputees who continue to remain sad, depressed and mourn over their loss and feel dejected and despondent. There may be a considerable number who remain tense, worried and anxious over their future interpersonal relationship in their social, vocational, familial and marital sphere. Some will have an overt mental breakdown and need active psychiatric treatment. In others, where the mental symptoms are not so obvious, a careful psychiatric interview will help in bringing to the fore the inner turmoil that can only be resolved by a psychiatrist [1, 2, 3, 4, 5].
Keeping in view the psychological needs of the amputees, present work was planned to study the effect of short-term psychiatric intervention in amputees. The objectives of the study were to identify amputees requiring psychiatric treatment, provide them with the same and to evaluate the effect of brief psychiatric intervention in these patients.
Material and Methods
A total of 40 patients with amputation were approached and monitored over a period of 2 months. A specially designed proforma was filled and all patients underwent the following psychological tests:
General Health Questionnaire (GHQ) [6]
Carroll Rating Scale for Depression (CRSD) [7]
State-Trait Anxiety Inventory (STAI) [8]
Michigan Alcoholism Screening Test (MAST) [9]
Disability Assessment Questionnaire (DAQ) [10]
The scales were administered individually to the patients and scored as per the test manual. Analysis of the scores of the above questionnaire revealed the psychological status of the patient and helped to identify probable psychiatric patients. As the number of patients identified as psychiatric cases and depressed were small, all these patients were provided with psychopharmacological and psychotherapeutic treatment for a period of six weeks. Thus each patient served as his own control for comparison of effects of therapy. At the end of treatment the patients were reevaluated using the same psychological tests to assess the efficacy of treatment. The information, which was collected, was tabulated and statistically analyzed using Chi square test and Mann Whitney ‘U’ test.
Results
A total of 40 patients with amputations were included in the study with their consent. The mean (SD) age of the patients was 30.05 (8.43) years. The age of the patients ranged from 22 years to 52 years. Demographic variables of the patients are given in Table 1.
Table 1.
Demographic characteristics of the amputees
| Characteristics | No. of amputees |
|---|---|
| Age distribution | |
| 20-29 years | 26 |
| 30-39 years | 8 |
| 40-49 years | 4 |
| 50-59 years | 2 |
| Sex : Male | 37 |
| Female | 3 |
| Religion : | |
| Hindu | 36 |
| Sikh | 3 |
| Muslim | 1 |
| Marital status | |
| Married | 29 |
| Unmarried | 11 |
| Domicile | |
| Rural | 31 |
| Urban | 9 |
| Education | |
| 0-5 class | 6 |
| 6-10 class | 24 |
| 11 + | 10 |
| Occupation | |
| Student | 3 |
| Housewife | 3 |
| Service | 34 |
Majority of the patients were Hindu, married, servicemen, in the third decade, hailing from a rural background and educated between 6 to 10 class. One of the patients had a past history of psychiatric disorder and was under maintenance therapy for schizophrenia. One patient had a family history of psychiatric disorder. All the patients described their interpersonal relation with their family members as cordial.
On the GHQ-12 a cutoff of > 2 identified 29 (72.5%) patients before treatment as psychiatric cases and this number had reduced to 20 (50%) after therapy (Fig 1). The difference was statistically significant (X2 = 4.27; df=1; p <0.05). On the CRSD a cut off score of > 10 identified 16 (40%) patients as probably depressed prior to treatment. After treatment this fell to 11(27.5%) (Fig 2). The difference was not statistically significant (X2 = 1.397; df = 1; p > 1.64). On the MAST 12.5% of the amputees scored in the alcoholic range while a further 15% were in “probable alcoholic” category.
Fig. 1.
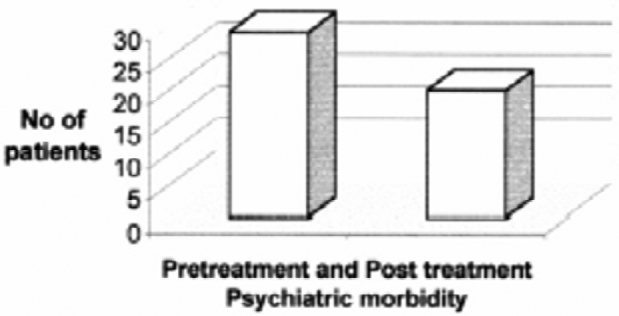
Psychiatric morbidity in amputees before and after psychiatric treatment
Fig. 2.
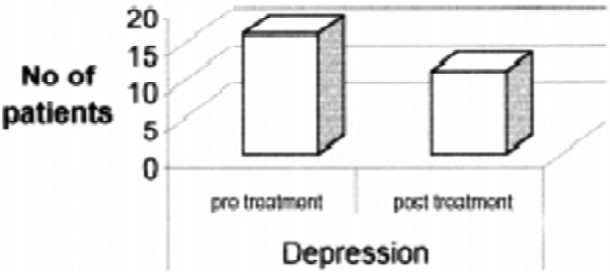
Depression in amputees before and after treatment
The scores obtained by the patients on the psychological tests are given in Table 2. Analysis revealed that after treatment a significant reduction in scores was noted on the GHQ and the CRSD. There was no significant reduction in the scores on the STAI, MAST and DAQ.
Table 2.
Psychological test results
| Test | Pretreatment Score Mean (SD) | Post treatment score Mean (SD) | Mann –Whitney 'U' test |
|---|---|---|---|
| General health questionnaire | 3.7 (1.49) | 2.45 (1.80) | S |
| Carroll rating scale for depression | 18.4 (7.04) | 11.8 (4.61) | S |
| State trait anxiety inventory-S | 40.7 (7.11) | 39.55 (5.42) | NS |
| State trait anxiety inventory-T | 37.6 (8.42) | 35.2 (6.39) | NS |
| Michigan alcoholism screening test | 3.1 (2.10) | 2.95 (1.93) | NS |
| Disability assessment | |||
| Questionnaire: | |||
| Social | 47.95 (8.61) | 47.05 (7.47) | NS |
| Vocational | 50.7 (9.95) | 49.7 (8.59) | NS |
| Personal | 45.0 (5.48) | 44.45 (4.88) | NS |
| Family | 44.6 (6.23) | 43.55 (4.31) | NS |
| Cognitive | 44.9 (6.73) | 43.75 (4.72) | NS |
S=Significant; NS=Not significant
Discussion
Amputation means a loss and psychological reaction to loss leads to bereavement, so much so that it is compared with the grief experienced by an individual when he loses his near and dear ones. This mourning is due to the fact that the personal satisfaction which the object of loss gave him in the past is not available to him any more. These reactions are manifested in different forms at different stages following amputation. In the early stage, these can present in the form of disbelief, stunned feeling, fear and panic, rage and anger, grief and despair, relief and happiness, horror and revulsion and shame or guilt. The late stage effects are in the form of depression, over activity and anxiety.
In the present study 40 amputees were studied for the period of two months. The majority of the cases were in the age range of 20-29 years (Table 1). This group of people is more at risk to accident and injury. In this regard the present study is comparable with that of Shukla et al [4] but not comparable to Pell et al [11]. The latter study included a large number of older age group amputees.
Various psychiatric disorders are commonly seen in amputees. In the present study utilizing the GHQ, we found psychiatric morbidity in 72.5% of amputees. This finding is in agreement with Shukla [4] who found psychiatric disorders in 65.27% of amputees. In agreement with a number of earlier studies [2, 4], in the present study the commonest psychiatric disorder was depression. Depression is an almost invariable concomitant of a disabling illness including amputation, either as an organic symptom or emotional consequence. Langer [12] characterized depression in amputees as being constituted by indecisiveness, thoughts of death, or ideas of self-harm, as opposed to guilt and body image changes with fatigue in patients with Parkinson's disease.
Pretreatment mean score on the GHQ was 3.7 and this decreased to 2.45 after treatment (difference statistically significant). This finding indicates the effectiveness and usefulness of psychiatric treatment in ameliorating the psychological distress of amputees. This conclusion is further strengthened by the observation that there was also a statistically significant reduction in the scores on the CRSD. These findings are in agreement with the findings of Shukla et al [4].
Majority of the studies have reported high anxiety in amputees [4]. As opposed to this in the present study only a few of the amputees showed high anxiety. This could be due to the fact that most of the patients were evaluated after fitting of prosthesis. On the MAST, 12.5% of the amputees scored in the alcoholic range while a further 15% were in “probable alcoholic” category. While the exact reason is not apparent, it is possible that this could be a reflection of the high prevalence of depression in our amputees. It is well known that some depressed individuals medicate their depression with alcohol.
On the DAQ the mean scores of the amputees on all the subscales ranged between 40-50. No change occurred with treatment. The lower scores on the DAQ in the present study may be due to the fact that most of our patients were using prosthesis and is in agreement with an earlier study [10]. Pershad et al [10] evaluated 30 amputees without prosthesis and 18 with prosthesis by the DAQ. They found that the mean dysfunction score of amputees without prosthesis was higher than those using artificial limbs. But the difference was significant in the vocational area alone. This showed that the amputated patients using artificial limbs have better vocational functioning than the amputated patients without artificial limbs. This is explained on the lines that the loss of a limb may make a person so handicapped that it may mean the loss of a job. Whereas with the supplement of an artificial limb, which of course does not compensate for the loss of a limb, at least may help him in resuming a job which in turn helps in lessening vocational dysfunction and leads to overall better functioning. In the present study also the highest score on the DAQ was on the vocational subscale. However, comparatively our patients had slightly less dysfunctional scores as compared to Pershad et al's [10] patients. This could be due to better social support system in the security forces. Another explanation could be that other factors like nursing care, interaction with doctors and other similar patients in the ward, visits by relatives and friends shielded him from the changed reality and immediate problems of practical day to day living, while the patient was in hospital.
The findings of the present study highlight the high incidence of psychiatric disability and depression in amputees. In view of the high incidence of psychological disorders in amputees, it is suggested that psychiatric evaluation should form a part of their overall management. The study had certain limitations. The sample was not very large due to constraint of time. For the same reason the patients could be treated for only six weeks and could not be followed up. Future studies in this area should include larger samples and after adequate treatment should follow-up the patients to evaluate the results of treatment.
References
- 1.Mall CP, Trivedi JK, Mishra US. Psychiatric sequelae of amputation. I:Immediate effects. Indian Journal of Psychiatry. 1997;39:313–317. [PMC free article] [PubMed] [Google Scholar]
- 2.Trivedi JK, Mall CP, Mishra US. Psychiatric sequelae of amputation. II:Long term effects. Indian Journal of Psychiatry. 1997;39:318–323. [PMC free article] [PubMed] [Google Scholar]
- 3.Srivastava S, Trivedi JK, Mall CP. Psychosocial aspects of amputation. Indian Journal of Psychiatry. 1997;39:247–252. [PMC free article] [PubMed] [Google Scholar]
- 4.Shukla GD, Sahu SC, Tripathi RP, Gupta DK. Psychiatric study of amputees. Br J Psychiatry. 1982;141:50–53. doi: 10.1192/bjp.141.1.50. [DOI] [PubMed] [Google Scholar]
- 5.Rybarczyk BD, Nyenhuis DL, Nicholas JJ, Schulz R, Alioto RJ, Blair C. Social discomfort and depression in a sample of adults with leg amputations. Arch Phys Med Rehabil. 1992;73:1169–1173. [PubMed] [Google Scholar]
- 6.Goldberg DP. Manual of the General Health Questionnaire. NFR; Windsor: 1978. [Google Scholar]
- 7.Carroll BJ, Feinberg M, Smouse PE, Rawson SG, Greden JF. The Carroll Rating scale for Depression. I.Development, Reliability and Validation. Br J Psychiatry. 1981;138:194–200. doi: 10.1192/bjp.138.3.194. [DOI] [PubMed] [Google Scholar]
- 8.Speilberger CD. Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press; California: 1977. [Google Scholar]
- 9.Selzer M. The Michigan Alcoholism Screening Test: The quest for a new diagnostic instrument. Am J Psychiatry. 1971;127:1653–1658. doi: 10.1176/ajp.127.12.1653. [DOI] [PubMed] [Google Scholar]
- 10.Pershad D, Verma SK, Malhotra AK, Malhotra S. Measurement of dysfunction and Dysfunction Analysis Questionnaire (DAQ) National Psychological Corp.; Agra: 1985. [Google Scholar]
- 11.Pell JP, Donnan PT, Fowkers FG. Quality of life following lower limb amputation for peripheral arterial disease. Eur J Vascular Surg. 1993;7:448–451. doi: 10.1016/s0950-821x(05)80265-8. [DOI] [PubMed] [Google Scholar]
- 12.Langer KG. Depression a disabling illness: Severity and patterns of self-reported symptoms in three groups. Journal of Geriatric Psychiatry and Neurology. 1994;7:1121–1128. doi: 10.1177/089198879400700208. [DOI] [PubMed] [Google Scholar]


