Abstract
Diabetes is often associated with chronic kidney disease (CKD) and is the primary cause of kidney failure in half of patients who receive dialysis therapy. Given the increasing prevalence of diabetes and its high morbidity and mortality, diabetic nephropathy is a serious drawback in individual patients and a tremendous socioeconomic burden on society. Despite growing concern for the management of diabetic nephropathy, the prevalence of CKD with diabetes is the same today as it was 20 years ago. The current strategy to manage diabetic nephropathy, including the control of hyperglycemia, dyslipidemia, and blood pressure and the wide-spread use of renin-angiotensin-aldosterone system inhibitors, is well established to be beneficial in the early stages of diabetic nephropathy. However, the effects are uncertain in patients with relatively progressed CKD. Therefore, early diagnosis or risk verification is extremely important in order to reduce the individual and socioeconomic burdens associated with diabetic nephropathy by providing appropriate management to prevent the development and progression of this condition. This review focuses on recent research and guidelines regarding risk assessment, advances in medical treatment, and challenges of and future treatments for diabetic nephropathy.
Keywords: Albuminuria; Renal insufficiency, chronic; Diabetic nephropathies; Early diagnosis; Glomerular filtration rate
INTRODUCTION
The increasing number of people with diabetes has had a major impact on the prevalence of diabetic nephropathy [1]. Diabetic nephropathy, which occurs in 20% to 40% of all patients with type 2 diabetes mellitus [2,3], is a metabolic disorder with high morbidity and mortality and is the leading cause of end-stage renal disease (ESRD) [4]. The overall burden for people with diabetic nephropathy is extremely high because of the strong associations of diabetic nephropathy and cardiovascular disease (CVD) with ESRD [2]. To improve the lives of people with diabetic nephropathy and to reduce the impact on society, early identification of the development or progression of diabetic nephropathy using appropriate screening and diagnostic tools is very important in order to provide timely and proper management. This review introduces the significant points of the recent research and guidelines regarding risk assessment, advances in medical treatment, and challenges of and future treatments for diabetic nephropathy.
LABORATORY ASSESSMENT
Depending on the clinical setting involved, identifying and monitoring diabetic nephropathy primarily involves two diagnostic modalities: assessment of kidney function in terms of estimated glomerular filtration rate (eGFR) and estimation of kidney damage in terms of albuminuria [2]. These methods are now used world-wide as clinical markers of diabetic nephropathy in real practice. Moreover, these markers help to decide whether or not to apply early therapeutic techniques and provide information to assess the risks of CVD and ESRD in diabetic nephropathy. However, these markers have several limitations with regard to identifying and monitoring diabetic nephropathy. Recognition of these limitations and the efforts to investigate better and new biomarkers are essential for the efficacious management of diabetic nephropathy.
Albuminuria
Albuminuria is considered as a sensitive marker of chronic kidney disease (CKD) and CVD risk and is used as the first clinical indicator of diabetic kidney disease [2]. Measuring the quantity of albumin in a 24-hour urine collection has been considered the gold standard for the diagnosis of diabetic nephropathy. However, collecting a 24-hour urine sample is difficult in routine practice. Moreover, this approach does not provide precise or accurate information [5]. Recently, guidelines recommend the use of the albumin-to-creatinine ratio (ACR) of a spot urine sample, a technique that can be performed easily in the clinic setting as a surrogate for the amount of urinary albumin in a 24-hour urine collection [5,6]. Simultaneous measurement of spot urine albumin and creatinine values, which allows normalization of these values, is helpful to overcome the variability in urine concentrations caused by hydration and is accepted widely as the marker for the screening of albuminuria.
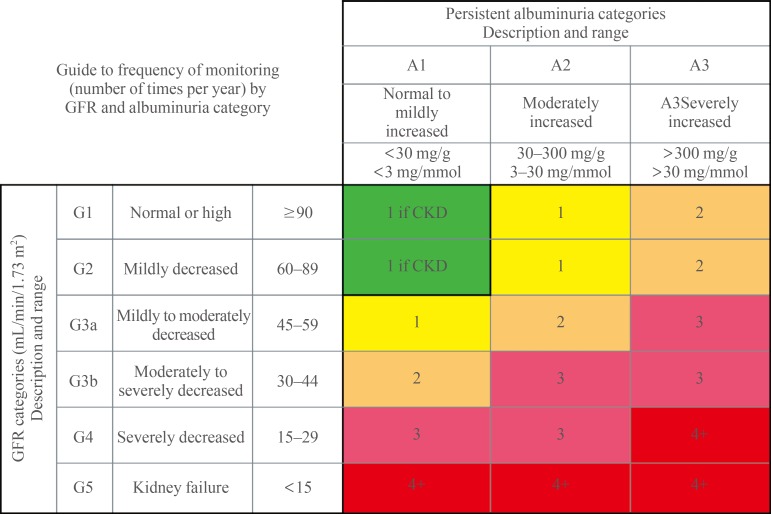
According to the urinary ACR, patients are classified into three albuminuria categories of Kidney Disease Improving Global Outcomes (KDIGO): A1, A2, or A3 (Fig. 1) [7]. Normal-to-mildly increased albuminuria (A1) is defined as <30 mg/g creatinine, and moderately increased albuminuria (A2) is defined as 30 to 300 mg/g creatinine. Previously, the range of albuminuria from 30 to 300 mg/g had been labeled "microalbuminuria," a term that can lead to misunderstanding. Thus, practical guidelines now recommend the use of "moderately increased albuminuria (A2)" instead of "microalbuminuria" [7]. Individuals with urine ACR greater than 300 mg/g are categorized as having severely increased albuminuria (A3), formerly referred to as "macroalbuminuria" [7,8]. The American Diabetes Association (ADA) recommends that a patient is considered to have albuminuria when at least two of three measurements of urine ACR examined within 6 months are abnormal [5].
Fig. 1. Albuminuria and glomerular filtration rate (GFR) categories for risk assessment of chronic kidney disease (CKD). The albuminuria and GFR grid reflects the risk of progression in terms of the intensity of the coloring (green, yellow, orange, red, and deep red). The numbers in the boxes are the frequency of monitoring (number of times per year). Green indicates stable disease, with follow-up measurements annually if CKD is present; yellow requires caution and measurements at least once per year; orange requires measurements twice per year; red requires measurements three times per year; and deep red requires the closest monitoring, approximately four or more times per year (at least every 1 to 3 months). Adapted from KDIGO [7], with permission from Elsevier.
The rate of progression from category A2 to category A3 is predicted to be 2% to 3% per year, and this progression is associated with a decrease in glomerular filtration rate (GFR) [9]. Persistently and moderately increased urinary ACR (A2) is an index of development of diabetic kidney disease and is also a well-established indicator of increased CVD risk [9,10,11]. Up to 40% of type 1 diabetic patients with moderately increased urine ACR (A2) show spontaneous remission to normal/mildly increased urine ACR (A1), while about 30% to 40% remain in albuminuria category A2 and do not progress to category A3 over 5 to 10 years of follow-up [12,13,14]. In contrast, patients with persistently and severely increased urine ACR (A3) usually progress to kidney failure or ESRD [15,16].
Estimated glomerular filtration rate
Although GFR is only one component of renal excretory function, it is commonly accepted as the best overall index of kidney function because it is generally reduced after widespread structural damage and, in CKD, most other kidney functions decline in parallel with GFR [7]. GFR is most commonly estimated using equations such as the Modification of Diet in Renal Disease (MDRD) study equation [17,18] or the Chronic Kidney Disease Epidemiology Collaboration equation [19]. Serum Cr is used to estimate these GFRs. Traditionally, the severity of CKD has been categorized into five stages according to eGFR [20]: G1, GFR ≥90 mL/min/1.73 m2; G2, 60 to 89 mL/min/1.73 m2; G3, 30 to 59 mL/min/1.73 m2; G4, 15 to 29 mL/min/1.73 m2; and G5 <15 mL/min/1.73 m2. The current classification further acknowledges the importance of dividing G3 based on data that support organizing different outcomes and risk profiles into the categories of G3a (GFR, 45 to 59 mL/min/1.73 m2) and G3b (GFR 30 to 44 mL/min/1.73 m2) [7].
Although the MDRD equation is used widely to screen and monitor for CKD, including diabetic kidney disease, it has been reported to underestimate the renal function in some populations, especially in patients with near-normal renal function [21]. Given this limitation, other candidate markers have been evaluated to enable more accurate predictions of GFR. Cystatin C, a cysteine protease inhibitor that is freely filtered by the renal glomeruli and metabolized by the proximal tubule, has been identified as a promising marker of renal failure [22]. Several studies have been performed to evaluate whether a cystatin C-based equation yields predictions that are superior to those produced by creatinine-based equations. Cystatin C was a more accurate serum marker than serum creatinine or the Cockcroft and Gault eGFR in discriminating type 2 diabetic patients with reduced GFR from those with normal GFR [23]. Although cystatin C is superior to creatinine for estimating GFR, it is not yet widely available in clinical practice. To date, serum creatinine-based eGFR remains the standard for assessing and monitoring diabetic kidney disease in most guidelines.
Risk assessment and monitoring based on both albuminuria and GFR categories
There is increasing evidence that both albuminuria and eGFR categories are valuable [7]. Increased albuminuria and decreased GFR are both associated with an increased risk of CKD and are synergistic (Fig. 1) [7]. The current KDIGO guidelines recommend that both albuminuria and GFR be monitored annually. More frequent measurements of eGFR and albuminuria should be considered in patients with a lower GFR and a higher albuminuria level because these conditions are more likely to progress in such patients. The frequency of measurements should also be individualized based on patient history and the underlying cause of kidney disease.
New biomarkers other than albuminuria and GFR
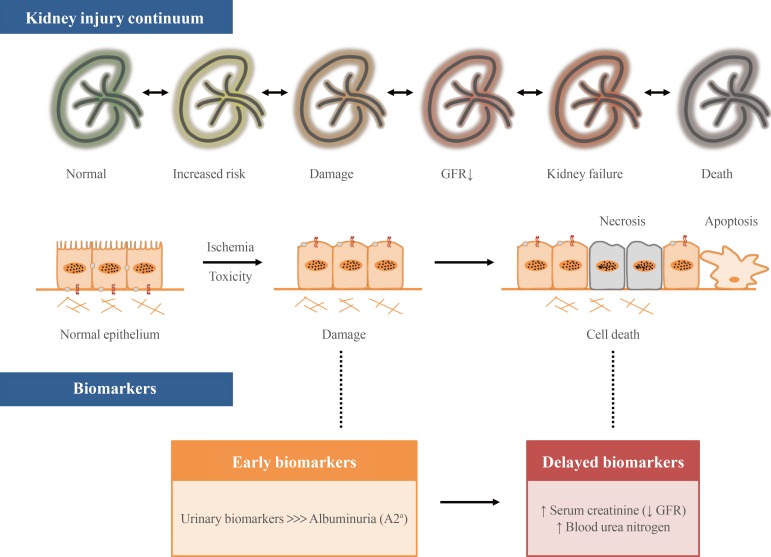
Although the presence of urinary albumin is recognized as an early marker of diabetic nephropathy, significant glomerular damage has already occurred by the time albuminuria is apparent [24]. It has been reported that a decrease in the renal function of a diabetic patient is not always accompanied by increased albuminuria in the clinic [25]. Several new biomarkers based on proteomics are being investigated with the hope of overcoming the limitations of current diagnostic tools for diabetic nephropathy [26]. Specifically, the use of urine as the diagnostic medium allows for the non-invasive detection of biomarkers of diabetic nephropathy [27]. Numerous urinary biomarkers can potentially provide a basis for the development of improved diagnostic tests other than that based on albuminuria (Fig. 2). Three main pathways for the sourcing of potential markers have been identified: kidney damage, oxidative stress, and low-grade inflammation, including atherosclerosis/vascular damage [27]. As tubulointerstitial damage can also play an important role in the pathogenesis of diabetic nephropathy, numerous investigators have been recently focusing on tubular damage markers as biomarkers of the development and progression of diabetic nephropathy [28,29,30].
Fig. 2. Early biomarkers of diabetic kidney disease along the kidney injury continuum. GFR, glomerular filtration rate. aAlbuminuria category A2, moderately increased albuminuria.
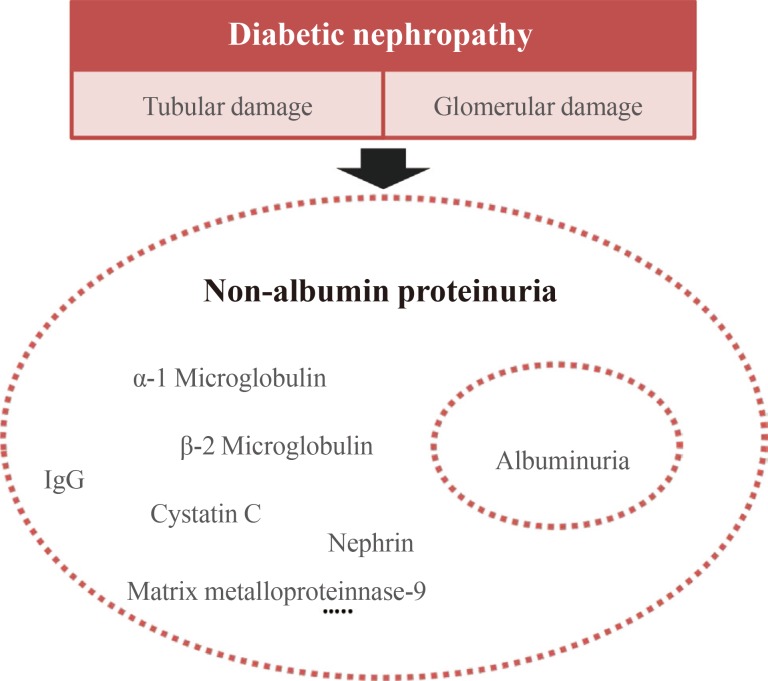
At a normal level of protein loss, albumin is considered a minor component of total urinary protein; however, it becomes the most significant single protein present as protein loss increases [31]. Albumin tends to be more variable at lower levels of proteinuria than at higher levels. Thus, it has been suggested that non-albumin proteinuria (NAP), rather than albuminuria, might be an important biomarker for early detection of the development and progression of diabetic nephropathy [32,33]. Urinary NAP includes numerous urinary proteins, some of which, including α-1 microglobulin, β-2 macroglobulin, immunoglobulin G, cystatin C, transferrin, nephrin, metalloproteinase-9, and tissue inhibitor of metalloproteinases-1, are associated with renal damage (Fig. 3) [34]. We recently demonstrated that urinary NAP might be a sensitive and specific marker of tubular damage that predicts renal impairment in type 2 diabetic patients [32,33]. Although it can be easily measured in clinical practice, NAP currently is not universally calibrated to be widely available in real practice.
Fig. 3. Non-albumin proteinuria as a diagnostic tool for diabetic nephropathy. IgG, immunoglobulin G.
ADVANCES IN MEDICAL TREATMENT
Glycemic control and management of comorbidities, such as hypertension, dyslipidemia, anemia, and hyperphosphatemia, are important in preventing and delaying renal and CVD events in patients with diabetic nephropathy. Thus, a multidisciplinary approaching is important for maximizing care for these complex patients. Moreover, novel treatments targeted at the complex pathophysiology of diabetic nephropathy are now receiving attention.
Glycemic control
Several observational studies have established a close relationship between poor glycemic control and microvascular complications, including diabetic nephropathy [35]. In contrast to the evidence for tight glycemic control on macrovascular complications, intensive glycemic control had a beneficial effect in delaying the onset and progression of albuminuria in recent large, randomized controlled trials [36,37,38]. Thus, recent guidelines recommend a target glycated hemoglobin of ~7.0% (53 mmol/mol) to prevent or delay the progression of the microvascular complications of diabetes, including diabetic kidney disease [7,8].
Blood pressure
There has been no randomized controlled trial to determine a target blood pressure in diabetic patients evaluated for CKD. Until recently, several guidelines, including those issued by the ADA and National Kidney Foundation, set a goal blood pressure of <130 mm Hg systolic and <80 mm Hg diastolic to reduce albuminuria and delay the progression of diabetic kidney disease [8,39,40]. Although intensive blood pressure control reduced the proportion of category A3 albuminuria in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, adverse events were also observed more frequently in the intensive blood pressure arm [41]. Based on recent trials, the Eight Joint National Committee recommended a blood pressure of 140/90 mm Hg for all patients with diabetes mellitus or CKD [40]. This target blood pressure is further supported by the recent ADA position statement [5]. Specifically, 130/80 mm Hg is considered the target blood pressure in subjects with albuminuria [41,42].
Either an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin receptor blocker (ARB) is recommended for the management of diabetes with moderately increased urinary albuminuria and is strongly recommended for those with severely increased albuminuria (A3) and/or an eGFR <60 mL/min/1.73 m2 (≥G3) [5]. However, ACE inhibitors and ARBs are not recommended for the primary prevention of diabetic kidney disease in patients with diabetes with normal blood pressure, normal/mildly increased albuminuria, and normal eGFR [5]. Two clinical trials studied dual therapy with ACE inhibitors and ARBs and revealed no beneficial effect on CVD or diabetic kidney disease; moreover, these combinations were associated with higher rates of adverse events [43,44]. Thus, the combination of ACE inhibitors and ARBs should be avoided in patients with diabetes [5].
CHALLENGES AND FUTURE TREATMENTS
The renin-angiotensin-aldosterone system (RAAS) pathway is the most important component in the development and progression of diabetic nephropathy. However, contrary to expectations, the results of recent studies of direct renin inhibitors were disappointing. One study showed that the combination of a renin inhibitor, aliskiren, and an ARB significantly reduced proteinuria in patients with type 2 diabetes [45]. However, use of the combination of an ACE inhibitor or ARB with aliskiren in type 2 diabetic patients was discontinued early in the Aliskiren Trial in Type 2 Diabetes Using Cardiovascular and Renal Disease Endpoints (ALTITUDE) study due to increased adverse events [46].
Emerging evidence shows that the use of mineralocorticoid receptor blockers in combination with ACE inhibitors or ARBs might have benefits on albuminuria in diabetic kidney disease, a phenomenon referred to as "aldosterone breakthrough" [47]. The combination of spironolactone with an ACE inhibitor or ARB significantly decreased albuminuria compared with the results of placebo [48]. More patients with diabetic nephropathy who received an ACE inhibitor or an ARB as well as finerenone showed an improvement in urinary ACR compared to the number of patients who received one of these plus a placebo [49].
Supporting evidence shows that lack of a vitamin D receptor resulted in an increase in RAAS activity and significant proteinuria [50]. The renal protective effects of 1,25(OH)2D3 and its analogs might involve suppression of renin gene transcription as well as high glucose-induced angiotensinogen production [51,52]. A recent large, randomized controlled trial revealed that paricalcitol reduced albuminuria in patients with type 2 diabetic nephropathy [53]. An ongoing trial is evaluating whether direct VDR activation can reduce the human RAAS in diabetes compared with the effect of an ACE inhibitor and whether this mechanism can translate to clinically relevant endpoints of diabetic kidney disease [54]. The outcomes of this trial will have major implications for the recommendation of vitamin D supplementation for the primary prevention of kidney complications in diabetes.
Studies performed in the last two decades have suggested that the endothelin (ET) system is an important therapeutic target for diabetic nephropathy [55]. ET-1 is a powerful vasoconstrictor and mitogenic factor that influences a wide variety of organ functions and, by virtue of its vasoactive, inflammatory, and profibrogenic properties, has been implicated in both CVDs and the progression of CKD [56]. ETA-selective antagonists have been shown to provide renoprotective effects, supplying a rationale for clinical trials involving administration of ETA-receptor antagonists in addition to RAAS blockade in patients with diabetic nephropathy [57,58]. The ongoing Study of Diabetic Nephropathy with Atrasentan is investigating the effect of atrasentan on the progression of diabetic nephropathy, and this study aims to clarify the cardiovascular and renal protective effects of ET receptor antagonists.
Sodium-glucose cotransporter-2 (SGLT2) inhibitors, as one of new therapeutic agents for diabetic patients, also demonstrated renal-protective effects on the basis of existing preclinical and clinical data using surrogate renal endpoints. SGLT2 inhibition is expected to reduce proximal tubular sodium reabsorption, thereby increasing distal sodium delivery, causing tubuloglomerular feedback, afferent vasoconstriction, and decreased hyperfiltration, which would be expected to reduce renal injury independent of the metabolic effect such as glycemic control and decreased inflammation [59]. The SGLT2 inhibitor was recently shown to reduce hyperfiltration in normotensive, normoalbuminuric patients with type 1 diabetes [60]. In clinical trials of type 2 diabetes, SGLT2 has been associated with significant renal effects, including modest, acute decreases in eGFR, followed by the maintenance of stable renal function and reduced albuminuria. SGLT2 inhibitors showed the renal effect of acute decrease in eGFR, which is followed by the maintenance of stable renal function and reduced albuminuria in clinical trials with type 2 diabetic patients [61,62]. An ongoing trial of renal outcomes of an SGLT2 inhibitor is currently underway (Evaluation of the Effects of Canagliflozin on Renal and Cardiovascular Outcomes in Participants with Diabetic Nephropathy [CREDENCE] trial, NCT02065791) and is exexpected to elucidate its renal protective effect.
CONCLUSIONS
Early and timely assessment with simple diagnostic modalities is beneficial for identifying and managing diabetic nephropathy. Many investigators are now focusing on early biomarkers to predict kidney damage beyond albuminuria. Furthermore, the combination of novel therapies and well-established conventional treatments might reduce the tremendous burden associated with diabetic nephropathy.
ACKNOWLEDGMENTS
This work was supported by a clinical research grant from Pusan National University Hospital in 2015.
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.de Boer IH, Rue TC, Hall YN, Heagerty PJ, Weiss NS, Himmelfarb J. Temporal trends in the prevalence of diabetic kidney disease in the United States. JAMA. 2011;305:2532–2539. doi: 10.1001/jama.2011.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tuttle KR, Bakris GL, Bilous RW, Chiang JL, de Boer IH, Goldstein-Fuchs J, et al. Diabetic kidney disease: a report from an ADA Consensus Conference. Diabetes Care. 2014;37:2864–2883. doi: 10.2337/dc14-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahn JH, Yu JH, Ko SH, Kwon HS, Kim DJ, Kim JH, et al. Prevalence and determinants of diabetic nephropathy in Korea: Korea National Health and Nutrition Examination Survey. Diabetes Metab J. 2014;38:109–119. doi: 10.4093/dmj.2014.38.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collins AJ, Foley RN, Chavers B, Gilbertson D, Herzog C, Johansen K, et al. United States Renal Data System 2011 Annual Data Report: atlas of chronic kidney disease & endstage renal disease in the United States. Am J Kidney Dis. 2012;59(1 Suppl 1):A7, e1–e420. doi: 10.1053/j.ajkd.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association. 9. Microvascular complications and foot care. Diabetes Care. 2016;39(Suppl 1):S72–S80. doi: 10.2337/dc16-S012. [DOI] [PubMed] [Google Scholar]
- 6.Eknoyan G, Hostetter T, Bakris GL, Hebert L, Levey AS, Parving HH, et al. Proteinuria and other markers of chronic kidney disease: a position statement of the National Kidney Foundation (NKF) and the national institute of diabetes and digestive and kidney diseases (NIDDK) Am J Kidney Dis. 2003;42:617–622. doi: 10.1016/s0272-6386(03)00826-6. [DOI] [PubMed] [Google Scholar]
- 7.KDIGO. Chapter 2: definition, identification, and prediction of CKD progression. Kidney Int Suppl (2011) 2013;3:63–72. doi: 10.1038/kisup.2012.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Kidney Foundation. KDOQI clinical practice guideline for diabetes and CKD: 2012 update. Am J Kidney Dis. 2012;60:850–886. doi: 10.1053/j.ajkd.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 9.Krolewski AS, Niewczas MA, Skupien J, Gohda T, Smiles A, Eckfeldt JH, et al. Early progressive renal decline precedes the onset of microalbuminuria and its progression to macroalbuminuria. Diabetes Care. 2014;37:226–234. doi: 10.2337/dc13-0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garg JP, Bakris GL. Microalbuminuria: marker of vascular dysfunction, risk factor for cardiovascular disease. Vasc Med. 2002;7:35–43. doi: 10.1191/1358863x02vm412ra. [DOI] [PubMed] [Google Scholar]
- 11.Klausen K, Borch-Johnsen K, Feldt-Rasmussen B, Jensen G, Clausen P, Scharling H, et al. Very low levels of microalbuminuria are associated with increased risk of coronary heart disease and death independently of renal function, hypertension, and diabetes. Circulation. 2004;110:32–35. doi: 10.1161/01.CIR.0000133312.96477.48. [DOI] [PubMed] [Google Scholar]
- 12.de Boer IH, Rue TC, Cleary PA, Lachin JM, Molitch ME, Steffes MW, et al. Long-term renal outcomes of patients with type 1 diabetes mellitus and microalbuminuria: an analysis of the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications cohort. Arch Intern Med. 2011;171:412–420. doi: 10.1001/archinternmed.2011.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Molitch ME, Steffes M, Sun W, Rutledge B, Cleary P, de Boer IH, et al. Development and progression of renal insufficiency with and without albuminuria in adults with type 1 diabetes in the diabetes control and complications trial and the epidemiology of diabetes interventions and complications study. Diabetes Care. 2010;33:1536–1543. doi: 10.2337/dc09-1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DCCT/EDIC Research Group. de Boer IH, Sun W, Cleary PA, Lachin JM, Molitch ME, et al. Intensive diabetes therapy and glomerular filtration rate in type 1 diabetes. N Engl J Med. 2011;365:2366–2376. doi: 10.1056/NEJMoa1111732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gall MA, Hougaard P, Borch-Johnsen K, Parving HH. Risk factors for development of incipient and overt diabetic nephropathy in patients with non-insulin dependent diabetes mellitus: prospective, observational study. BMJ. 1997;314:783–788. doi: 10.1136/bmj.314.7083.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The Diabetes Control and Complications (DCCT) Research Group. Effect of intensive therapy on the development and progression of diabetic nephropathy in the Diabetes Control and Complications Trial. Kidney Int. 1995;47:1703–1720. doi: 10.1038/ki.1995.236. [DOI] [PubMed] [Google Scholar]
- 17.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 18.Lee CS, Cha RH, Lim YH, Kim H, Song KH, Gu N, et al. Ethnic coefficients for glomerular filtration rate estimation by the Modification of Diet in Renal Disease study equations in the Korean population. J Korean Med Sci. 2010;25:1616–1625. doi: 10.3346/jkms.2010.25.11.1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139:137–147. doi: 10.7326/0003-4819-139-2-200307150-00013. [DOI] [PubMed] [Google Scholar]
- 21.Chudleigh RA, Dunseath G, Evans W, Harvey JN, Evans P, Ollerton R, et al. How reliable is estimation of glomerular filtration rate at diagnosis of type 2 diabetes? Diabetes Care. 2007;30:300–305. doi: 10.2337/dc06-1688. [DOI] [PubMed] [Google Scholar]
- 22.Knight EL, Verhave JC, Spiegelman D, Hillege HL, de Zeeuw D, Curhan GC, et al. Factors influencing serum cystatin C levels other than renal function and the impact on renal function measurement. Kidney Int. 2004;65:1416–1421. doi: 10.1111/j.1523-1755.2004.00517.x. [DOI] [PubMed] [Google Scholar]
- 23.Mussap M, Dalla Vestra M, Fioretto P, Saller A, Varagnolo M, Nosadini R, et al. Cystatin C is a more sensitive marker than creatinine for the estimation of GFR in type 2 diabetic patients. Kidney Int. 2002;61:1453–1461. doi: 10.1046/j.1523-1755.2002.00253.x. [DOI] [PubMed] [Google Scholar]
- 24.Barratt J, Topham P. Urine proteomics: the present and future of measuring urinary protein components in disease. CMAJ. 2007;177:361–368. doi: 10.1503/cmaj.061590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.MacIsaac RJ, Tsalamandris C, Panagiotopoulos S, Smith TJ, McNeil KJ, Jerums G. Nonalbuminuric renal insufficiency in type 2 diabetes. Diabetes Care. 2004;27:195–200. doi: 10.2337/diacare.27.1.195. [DOI] [PubMed] [Google Scholar]
- 26.Kamijo-Ikemori A, Sugaya T, Kimura K. Novel urinary biomarkers in early diabetic kidney disease. Curr Diab Rep. 2014;14:513. doi: 10.1007/s11892-014-0513-1. [DOI] [PubMed] [Google Scholar]
- 27.Matheson A, Willcox MD, Flanagan J, Walsh BJ. Urinary biomarkers involved in type 2 diabetes: a review. Diabetes Metab Res Rev. 2010;26:150–171. doi: 10.1002/dmrr.1068. [DOI] [PubMed] [Google Scholar]
- 28.Nauta FL, Boertien WE, Bakker SJ, van Goor H, van Oeveren W, de Jong PE, et al. Glomerular and tubular damage markers are elevated in patients with diabetes. Diabetes Care. 2011;34:975–981. doi: 10.2337/dc10-1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jeon YK, Kim MR, Huh JE, Mok JY, Song SH, Kim SS, et al. Cystatin C as an early biomarker of nephropathy in patients with type 2 diabetes. J Korean Med Sci. 2011;26:258–263. doi: 10.3346/jkms.2011.26.2.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim SS, Song SH, Kim IJ, Yang JY, Lee JG, Kwak IS, et al. Clinical implication of urinary tubular markers in the early stage of nephropathy with type 2 diabetic patients. Diabetes Res Clin Pract. 2012;97:251–257. doi: 10.1016/j.diabres.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 31.Ballantyne FC, Gibbons J, O'Reilly DS. Urine albumin should replace total protein for the assessment of glomerular proteinuria. Ann Clin Biochem. 1993;30(Pt 1):101–103. doi: 10.1177/000456329303000119. [DOI] [PubMed] [Google Scholar]
- 32.Kim SS, Song SH, Kim IJ, Jeon YK, Kim BH, Kwak IS, et al. Urinary cystatin C and tubular proteinuria predict progression of diabetic nephropathy. Diabetes Care. 2013;36:656–661. doi: 10.2337/dc12-0849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim SS, Song SH, Kim IJ, Kim WJ, Jeon YK, Kim BH, et al. Nonalbuminuric proteinuria as a biomarker for tubular damage in early development of nephropathy with type 2 diabetic patients. Diabetes Metab Res Rev. 2014;30:736–741. doi: 10.1002/dmrr.2546. [DOI] [PubMed] [Google Scholar]
- 34.Halimi JM, Matthias B, Al-Najjar A, Laouad I, Chatelet V, Marliere JF, et al. Respective predictive role of urinary albumin excretion and nonalbumin proteinuria on graft loss and death in renal transplant recipients. Am J Transplant. 2007;7:2775–2781. doi: 10.1111/j.1600-6143.2007.02010.x. [DOI] [PubMed] [Google Scholar]
- 35.Fioretto P, Bruseghin M, Berto I, Gallina P, Manzato E, Mussap M. Renal protection in diabetes: role of glycemic control. J Am Soc Nephrol. 2006;17(4 Suppl 2):S86–S89. doi: 10.1681/ASN.2005121343. [DOI] [PubMed] [Google Scholar]
- 36.ADVANCE Collaborative Group. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560–2572. doi: 10.1056/NEJMoa0802987. [DOI] [PubMed] [Google Scholar]
- 37.Ismail-Beigi F, Craven T, Banerji MA, Basile J, Calles J, Cohen RM, et al. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010;376:419–430. doi: 10.1016/S0140-6736(10)60576-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129–139. doi: 10.1056/NEJMoa0808431. [DOI] [PubMed] [Google Scholar]
- 39.Molitch ME, DeFronzo RA, Franz MJ, Keane WF, Mogensen CE, Parving HH, et al. Nephropathy in diabetes. Diabetes Care. 2004;27(Suppl 1):S79–S83. doi: 10.2337/diacare.27.2007.s79. [DOI] [PubMed] [Google Scholar]
- 40.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 41.ACCORD Study Group. Cushman WC, Evans GW, Byington RP, Goff DC, Jr, Grimm RH, Jr, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–1585. doi: 10.1056/NEJMoa1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015;313:603–615. doi: 10.1001/jama.2014.18574. [DOI] [PubMed] [Google Scholar]
- 43.ONTARGET Investigators. Yusuf S, Teo KK, Pogue J, Dyal L, Copland I, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547–1559. doi: 10.1056/NEJMoa0801317. [DOI] [PubMed] [Google Scholar]
- 44.Fried LF, Emanuele N, Zhang JH, Brophy M, Conner TA, Duckworth W, et al. Combined angiotensin inhibition for the treatment of diabetic nephropathy. N Engl J Med. 2013;369:1892–1903. doi: 10.1056/NEJMoa1303154. [DOI] [PubMed] [Google Scholar]
- 45.Persson F, Rossing P, Reinhard H, Juhl T, Stehouwer CD, Schalkwijk C, et al. Renal effects of aliskiren compared with and in combination with irbesartan in patients with type 2 diabetes, hypertension, and albuminuria. Diabetes Care. 2009;32:1873–1879. doi: 10.2337/dc09-0168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Parving HH, Brenner BM, McMurray JJ, de Zeeuw D, Haffner SM, Solomon SD, et al. Aliskiren trial in type 2 diabetes using cardio-renal endpoints (ALTITUDE): rationale and study design. Nephrol Dial Transplant. 2009;24:1663–1671. doi: 10.1093/ndt/gfn721. [DOI] [PubMed] [Google Scholar]
- 47.Bomback AS, Kshirsagar AV, Amamoo MA, Klemmer PJ. Change in proteinuria after adding aldosterone blockers to ACE inhibitors or angiotensin receptor blockers in CKD: a systematic review. Am J Kidney Dis. 2008;51:199–211. doi: 10.1053/j.ajkd.2007.10.040. [DOI] [PubMed] [Google Scholar]
- 48.Schjoedt KJ, Rossing K, Juhl TR, Boomsma F, Tarnow L, Rossing P, et al. Beneficial impact of spironolactone on nephrotic range albuminuria in diabetic nephropathy. Kidney Int. 2006;70:536–542. doi: 10.1038/sj.ki.5001580. [DOI] [PubMed] [Google Scholar]
- 49.Bakris GL, Agarwal R, Chan JC, Cooper ME, Gansevoort RT, Haller H, et al. Effect of finerenone on albuminuria in patients with diabetic nephropathy: a randomized clinical trial. JAMA. 2015;314:884–894. doi: 10.1001/jama.2015.10081. [DOI] [PubMed] [Google Scholar]
- 50.Zhou C, Lu F, Cao K, Xu D, Goltzman D, Miao D. Calcium-independent and 1,25(OH)2D3-dependent regulation of the renin-angiotensin system in 1alpha-hydroxylase knockout mice. Kidney Int. 2008;74:170–179. doi: 10.1038/ki.2008.101. [DOI] [PubMed] [Google Scholar]
- 51.Deb DK, Chen Y, Zhang Z, Zhang Y, Szeto FL, Wong KE, et al. 1,25-Dihydroxyvitamin D3 suppresses high glucose-induced angiotensinogen expression in kidney cells by blocking the NF-{kappa}B pathway. Am J Physiol Renal Physiol. 2009;296:F1212–F1218. doi: 10.1152/ajprenal.00002.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yuan W, Pan W, Kong J, Zheng W, Szeto FL, Wong KE, et al. 1,25-Dihydroxyvitamin D3 suppresses renin gene transcription by blocking the activity of the cyclic AMP response element in the renin gene promoter. J Biol Chem. 2007;282:29821–29830. doi: 10.1074/jbc.M705495200. [DOI] [PubMed] [Google Scholar]
- 53.de Zeeuw D, Agarwal R, Amdahl M, Audhya P, Coyne D, Garimella T, et al. Selective vitamin D receptor activation with paricalcitol for reduction of albuminuria in patients with type 2 diabetes (VITAL study): a randomised controlled trial. Lancet. 2010;376:1543–1551. doi: 10.1016/S0140-6736(10)61032-X. [DOI] [PubMed] [Google Scholar]
- 54.Brown JM, Secinaro K, Williams JS, Vaidya A. Evaluating hormonal mechanisms of vitamin D receptor agonist therapy in diabetic kidney disease: the VALIDATE-D study. BMC Endocr Disord. 2013;13:33. doi: 10.1186/1472-6823-13-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gagliardini E, Zoja C, Benigni A. Et and diabetic nephropathy: preclinical and clinical studies. Semin Nephrol. 2015;35:188–196. doi: 10.1016/j.semnephrol.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 56.Fligny C, Barton M, Tharaux PL. Endothelin and podocyte injury in chronic kidney disease. Contrib Nephrol. 2011;172:120–138. doi: 10.1159/000328692. [DOI] [PubMed] [Google Scholar]
- 57.Kohan DE, Pritchett Y, Molitch M, Wen S, Garimella T, Audhya P, et al. Addition of atrasentan to renin-angiotensin system blockade reduces albuminuria in diabetic nephropathy. J Am Soc Nephrol. 2011;22:763–772. doi: 10.1681/ASN.2010080869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.de Zeeuw D, Coll B, Andress D, Brennan JJ, Tang H, Houser M, et al. The endothelin antagonist atrasentan lowers residual albuminuria in patients with type 2 diabetic nephropathy. J Am Soc Nephrol. 2014;25:1083–1093. doi: 10.1681/ASN.2013080830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Skrtic M, Cherney DZ. Sodium-glucose cotransporter-2 inhibition and the potential for renal protection in diabetic nephropathy. Curr Opin Nephrol Hypertens. 2015;24:96–103. doi: 10.1097/MNH.0000000000000084. [DOI] [PubMed] [Google Scholar]
- 60.Cherney DZ, Perkins BA, Soleymanlou N, Maione M, Lai V, Lee A, et al. Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation. 2014;129:587–597. doi: 10.1161/CIRCULATIONAHA.113.005081. [DOI] [PubMed] [Google Scholar]
- 61.Barnett AH, Mithal A, Manassie J, Jones R, Rattunde H, Woerle HJ, et al. Efficacy and safety of empagliflozin added to existing antidiabetes treatment in patients with type 2 diabetes and chronic kidney disease: a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2014;2:369–384. doi: 10.1016/S2213-8587(13)70208-0. [DOI] [PubMed] [Google Scholar]
- 62.Yale JF, Bakris G, Cariou B, Yue D, David-Neto E, Xi L, et al. Efficacy and safety of canagliflozin in subjects with type 2 diabetes and chronic kidney disease. Diabetes Obes Metab. 2013;15:463–473. doi: 10.1111/dom.12090. [DOI] [PMC free article] [PubMed] [Google Scholar]