Abstract
Background
Cochlear implants are now an acceptable therapeutic option for those patients with irreversible hearing loss and deaf-mutism. The surgery is time consuming and complicated. Hence, the technique of anaesthesia plays a crucial role in success of cochlear implant surgery. Cochlear implant patients have various types of syndromes which are important from anaesthetic as well as surgical point of view. Pre-implant preparation requires objective assessment of hearing, plain X-rays of skull and a CT scan of the temporal bone. Anaesthesia is required for objective assessment of hearing in children under five years of age, to obtain X-rays of skull, magnetic resonance imaging (MRI), CT scan, brain evoked response audiometry (BERA) testing and finally for cochlear implant surgery. Anaesthetic considerations include preoperative familiarisation with the patient and his family. Syndromal illnesses have specific anaesthetic significance such as presence of difficult airway or prolonged QT interval. Parental presence is highly desirable during induction of anaesthesia. Electro-surgical instruments especially monopolar ones, should not be used once the cochlear implant is in place.
Methods
In our institution, all cases (15 children) received their cochlear implants under general anaesthesia and formed the study group. Children were administered midazolam orally and inj ketamine during CT scan. Our techniques of general anaesthesia were modified to permit use of nerve stimulators during surgery. To minimise the incidence of vertigo particularly after cochleostomy, postoperative nausea and vomiting, all patients received glycopyrrolate and fentanyl citrate intravenously prior to induction. Other agents used were, thiopentone, suxamethonium and end-tidal 1.3 MAC halothane in 1:2 mixture of oxygen and nitrous oxide (O2 and N2O). Electro diathermy was switched off, before the cochlear device was implanted on the patient. Patients were allowed to breathe spontaneously whenever nerve stimulator was used to locate the facial nerve. Inj Ondansetron 0.1 mg/kg was used as anti-emetic agent. Postoperative pain relief was initially provided with fentanyl 1 μg/kg IV and later with syrup ibuprofen.
Results
There were no remarkable anaesthetic or surgical complication in our series except perilymph leakage in two cases.
Key Words: Anaesthesia technique, Cochlear implantation, Deaf-mutism
Introduction
The field of cochlear implantation has been expanding rapidly and now it is an acceptable therapeutic option for those patients with irreversible hearing loss and deaf-mutism. It has been hailed as one of the greatest advances in otology [1]. Cochlear implants are extremely expensive computerised electric prostheses that partially replace the functions of the cochlea (Fig 1). The surgery is time consuming and is performed under general anaesthesia via a trans-mastoid approach. The operative technique is complicated and necessitates preservation of functional integrity of the facial and cochlear nerve. The anaesthesiologist is an integral member of the cochlear implant team whose anaesthetic as well as communication skills are put to test. The technique of anaesthesia plays a crucial role in success of cochlear implant surgery as the anaesthesiologist has to produce conditions which facilitate use of nerve stimulators and treat troublesome post-operative complications such as nausea, vomiting and vertigo.
Fig. 1.
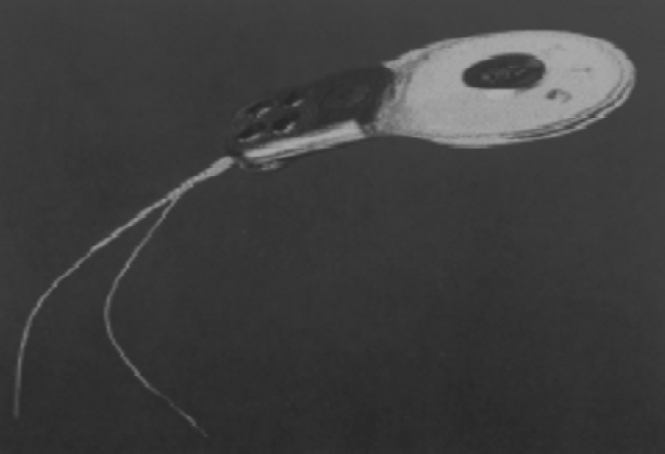
Cochlear Implant showing electrode arrangements
This paper highlights certain important technical aspects of the surgery and our anaesthetic experience in a series of cases performed till now. A brief review of literature is also presented.
Material and Methods
The present study was carried out in the form of retrospective analysis of medical, surgical and anaesthetic records of all the children (age upto 15 years) who underwent implantation of cochlear devices at our institute over last five years. The analysis included pre-implant work up and pre-operative screening of each child. Surgical aspects along with incidence of complications were also recorded. Anaesthetic technique was screened in detail and adverse events during entire peri-operative period were noted.
Patients with irreversible hearing loss and not responding to hearing aids, were selected by the implant surgeon. Each child was subjected to detailed audiological work-up along with CT scan and MRI. During pre-anaesthetic assessment, medical illness was ruled out and a rapport with the child was established. The basic surgical approach consisted of a post-aural incision, creation of an implant bed over mastoid and insertion of electrode after securing haemostasis.
The anaesthetic protocol involved a thorough assessment of general condition of the child with special reference to any congenital anomaly. General anaesthesia was administered for all the cases. No premedication was given. Monitoring included electrocardiogram (ECG), pulse oximetry, end tidal carbon-di-oxide and non-invasive blood pressure (NIBP). All patients received glycopyrollate 5 μg/kg and fentanyl citrate 1 μg/kg intravenously prior to induction. Thereafter, anaesthesia was induced with thiopentone and maintained with end-tidal 1.3 MAC halothane in 1:2 mixture of oxygen and nitrous oxide (O2 and N2O). Inj fentanyl was repeated on as required basis. The maintenance fluid consisted of N/5 saline in 5% dextrose. Electro diathermy was switched off, before the cochlear device was implanted on the patient. Patients were allowed to breathe spontaneously after the effect of suxamethonium wore off, however vecuronium was given whenever nerve stimulators were not used to locate the facial nerve.
Mild hypotension (systolic blood pressure < 85 mmHg) was maintained through out the surgery mainly with the help of inhalational agents, however inj clonidine was given in two cases as a single bolus of 2 μg/kg. Air warming blanket device was used for prevention of hypothermia. Inj ondansetron 0.1 mg/kg was added in the drip just prior to skin closure in all the cases. At the conclusion of surgery, inhalational agents were terminated and tracheal extubation was done when patients were fully awake.
Postoperative pain relief was initially provided with fentanyl 1 μg/kg IV and was later supplemented with syrup ibugesic (ibuprofen 10 mg/kg). All cases were observed in the intensive care unit (ICU) for 48 hrs, for any complication related to surgery and anaesthesia. In all the cases, the implanted receiver was ‘fired up’ (activated) 3 weeks later (Fig 2).
Fig. 2.
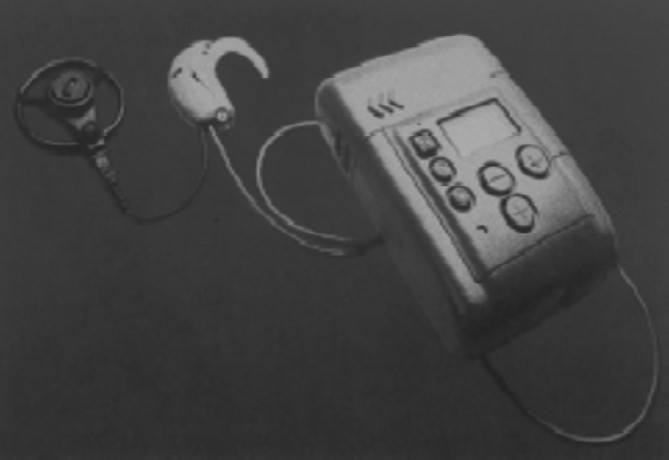
Receiver and speech processor
Results
A total of 15 children and two adults were anaesthetised for the implant surgery till October 2002. The adult cases were not included in the present study. The youngest patient was 2.5 years old whereas the oldest was 14 years of age. The male female ratio was 9:6 (Table-1). None of the patients had any airway difficulties, systemic illnesses or congenital syndromes. All the children had sensori-neural hearing loss of congenital onset. Five cases received implants in their left ear whereas the rest of them were fitted with the device in their right ear.
Table 1.
The patient details
| Age | Sex | Ear |
|---|---|---|
| 14 | M | Left |
| 5 y 6 m | F | Left |
| 11y 6 m | F | Right |
| 7y 8 m | F | Right |
| 6y 6m | M | Right |
| 4y 8m | M | Right |
| 12y 3m | M | Right |
| 11y 3m | M | Right |
| 6y 6m | F | Right |
| 7y 3m | M | Right |
| 10y 6m | F | Right |
| 12y | M | Left |
| 2y 6m | M | Left |
| 2y 9m | M | Right |
| 4y | F | Left |
There were no intra-operative haemodynamic or any other adverse events requiring intervention. The average duration of operation was 260 minutes and it ranged between 4 to 6 hours. Only two cases had post-operative nausea and vomiting. In all the cases, the outcome was uneventful and the implanted receiver was activated 3 weeks later. There were no remarkable surgical complications. Intra-operatively, one case had severe bleeding whereas two cases had perilymph leakage because of inner ear abnormalities. Postoperatively one child had flap necrosis and required revision surgery whereas another patient had haematoma necessitating drainage. All the cases are undergoing intensive auditory rehabilitation and are making satisfactory progress.
Discussion
In our country, cochlear implant programme was started in the city of Mumbai more than a decade ago. The cochlear implant programme in the Armed Forces is a relatively new venture. The first cochlear implant took place in the year 1997 and the paediatric cochlear implant programme was commissioned a year later which has now gained significant momentum. Our centre now boasts of a successful programme with appropriately laid down protocols for patient selection, surgery, anaesthesia and auditory rehabilitation.
In order to achieve optimal results after surgery, proper patient selection is a must. An early detection of hearing loss is desirable since it is evident that children receiving cochlear implants at an early age may show rapid acquisition of listening skills. In Australia, more and more children below two years are being detected to be suffering from deafness and in fact there has been a significant increase in the proportion of deaf children detected between the ages of 6 and 12 months [2]. Even though, the mean age of children (8 years) in our series is on the higher side, it is anticipated that with increased awareness of a therapeutic option being available, concerned parents may report early to our centre. Potential cochlear implant patients should meet certain rational diagnostic criteria and be preferably more than two years of age. The facial ridge is better developed in older children and allows ready identification of facial nerve. Candidature also requires that the child has an implantable cochlea and is fit for the surgery. There should not be any underlying medical problems such as labyrinthitis due to meningitis and chronic supportive otitis media, which may affect the conduct of surgery. Important medical contraindications are uncontrolled otitis media, autism, severe intellectual disability, and possibly, central nervous system disorders which are likely to affect the auditory pathways and compromise speech perception. Such patients are subjected to a battery of investigations to assess middle ear function (which includes impedance testing, tests for residual hearing etc). The children are initially given a hearing aid trial and only if speech and language acquisition are not progressing satisfactorily, decision to undertake cochlear implantation is made.
Counselling is an important part of pre-operative period while choosing a patient for cochlear implant. The patient and his family must be highly motivated and should be taken into confidence so as to allow them to have realistic expectations about the outcome. The parents should also be able to provide a satisfactory home environment for auditory rehabilitation. A large number of children presenting for cochlear implant surgery have deafness of unknown origin and no family history [3]. All the cases in the present series had deafness of unknown etiology. However, a significant number are of genetic origin and of autosomal recessive inheritance. The syndromes associated with hearing loss are usually hereditary and in most cases the genetic defect affects the development of both the ear and related systems. The various syndromes are designated as Usher, Pendred, Waardenburg, Treacher Collins, Klippel Feil, Jervel and Lange-Neilsen, Refsum, Albers-Schonberg, Cockayne and trisomy 13 and 18 syndromes. These syndromes are not only important from anaesthetic point of view but also are associated with various types of dysplasia of temporal bones and cochlea named after Michel, Mondini, Scheibe and the Bing-Siebenmann [4]. These dysplastic changes may necessitate change in the technique of placing the implant in the cochlea. Approximately 50% of the cases have acquired hearing loss mostly because of perinatal infections with TORCH group of organisms.
Preoperative assessment also includes certain psychological tests to exclude those patients who may have organic brain dysfunction, mental retardation and undetected psychosis. It is also important to rule out retro-cochlear hearing loss and to be sure that the child has a communication handicap not amenable to hearing aids. If the child has severe to profound hearing loss and is likely to need the implant, further preparation requires objective assessment of hearing, plain X-rays of skull and a high resolution computerized tomographic (HRCT) scan of the temporal bone. An objective assessment of hearing (steady state evoked potential, auditory brainstem evoked potential and electrocochleography) is needed when the child is under five years of age. HRCT scan of temporal bone is done to see the basal turn of cochlea, its patency and any abnormal ossification within the cochlea secondary to meningitis. It also gives an indication about degree of mastoid pneumatization, presence of fluid in middle ear and any congenital inner ear abnormality. All these factors have a bearing on insertion of electrode array. If cochlea is filled with fibrous tissue following labyrinthitis, then it is necessary to carry out an MRI examination under anaesthesia [4]. If the child has impaired vision because of congenital cataracts as associated with Usher Syndrome, it should be corrected so that maximum help can be obtained with lip-reading during post-surgical auditory rehabilitation.
Common post-operative complications are problems related to flap, delayed facial nerve palsy, dizziness and rarely electrode migration. In a series by Clarke et al the incidence of major complications requiring re-do surgery or intravenous antibiotics was recorded to be 3.9% [5]. However, there were no remarkable surgical complications in our series. Complications like device extrusion, facial palsy or non-auditory sensation following activation were not encountered. Intra-operatively, one case had severe bleeding whereas two cases had perilymph leakage because of inner ear abnormalities. Perilymph gusher, as it is termed, can be managed by letting the fluid drain off before inserting the electrode and then sealing around entry point with muscle or connective tissue. In our cases it was managed, in addition, with injection mannitol and re-positioning of head. This occurred due to the very thin cortical wall of the skull and the surgical field being close to the middle and posterior cranial fossa. It can also occur due to abnormal communication between sub-arachnoid space and peri-lymphatic space due to dilated and wide vestibular aqueduct.
Cochlear implants have been successfully done under local anaesthesia without any adverse effects on the implants [12]. In our institution however, we ventured to do all cases under general anaesthesia due to evolving experience in a time consuming surgery. Moreover, local anaesthesia requires some co-operation from the patients, which is not forthcoming in this category of patients, particularly the children. All the children in this series had been administered oral midazolam (0.5 mg/kg) and inj ketamine (2mg/kg i/v) as part of the anaesthetic technique during the CT scans. Our techniques of general anaesthesia were modified to permit use of nerve stimulators during surgery, to minimise the incidence of vertigo particularly after cochleostomy, postoperative nausea and vomiting. BERA was not done in our cases because of lack of facilities. Preoperative familiarisation with the patient and his family is of utmost importance as it not only helps in establishing rapport with the deaf mute patient but also works as additional confidence building measure and corroborates the easy communication skills needed in the post operative period. However, communication can be difficult with such patients and this should be kept in mind [6]. As children having a cochlear implant will have had a general anaesthetic for the CT scan and BERA testing, any difficulties associated with these procedures need to be reviewed. Occasionally, CT scan of temporal bone can be difficult in case of Klippel-Fiel anomaly, where the ability to take coronal views is restricted because of fusion of the cervical vertebrae. Preoperative evaluation should aim at assessing the development milestones and evaluating neurological deficits. The child's height, weight, blood pressure and head circumference must always be measured and recorded. The general appearance of the skull can suggest the presence of macrocephaly, microencephaly or craniosynostosis. The head and neck region should be carefully examined to look for features suggestive of cerebral palsy, congenital syphilis, microphthalmia, cataract, cranial nerve palsies as well as cutaneous lesions. A whorl pattern of hair can indicate the presence of cerebral malformation whereas presence of abnormal palmer creases should alert the anaesthesiologist to the possibility of Down's Syndrome. There are no routine investigations required but a complete haemogram and blood grouping can be done. However, in case of syndromal illnesses, specific investigations such as ECG or renal function tests should be asked for.
Children with congenital deafness have a variety of syndromal illnesses, each of them having specific anaesthetic significance. Abnormalities in facial appearance and therefore difficult airway may point at presence of Treacher Collins Syndrome whereas eye disorders could form a part of Usher syndrome. Klippel-Fiel anomaly is associated with fusion of the cervical vertebrae making the intubation of the trachea a difficult proposition. Alport syndrome is commonly associated with renal failure and endocrinal abnormalities, whereas goiter and metabolic disorders are features of Pendred syndrome. Children with congenital hearing loss may also have Jervell and Lange-Nielsen Syndrome. This syndrome is usually associated with a history of syncopal attacks or fits and the condition often manifests as prolonged QT interval on the ECG leading to dangerous ventricular arrhythmias. Therefore, these patients could be treated with beta blockers prior to cochlear implant surgery. There has been a report of a child suffering from this syndrome who became hypoglycaemic during preoperative period [7] whereas in another report the child was kept under cardiac monitor for 48 hours as an extreme precautionary measure. This child experienced a syncopal episode requiring placement of an automatic pacemaker and defibrillator subsequently, during auditory rehabilitation [8].
Parental presence is highly desirable during induction of anaesthesia since lack of communication is a big hurdle in establishing rapport. These deaf-mute children, similar to a normal child, are able to recognize strange environment as being alien and have fear of separation, pain and physical harm. Parental presence reduces separation anxiety significantly and has been shown to decrease the number of upset children during induction [9]. Initially oral midazolam was used as a premedicant, subsequently we changed our approach to induce the child in mother's lap with 3 mg/kg of thiopentone, whenever possible. Gaseous or intravenous induction, both are equally suitable. Choice of anaesthetic drugs is guided by the concern for post-operative nausea and vomiting and routine monitors are employed intra-operatively. Children having acute middle ear infection or meningitis are not posted for surgery. However, if the preoperative assessment reveals a temperature greater than 38°C, due to an upper respiratory tract infection, not only does this predispose to a post operative chest infection, but the elevated temperature can render a child susceptible to poor temperature control intraoperatively. Such cases should be deferred. Usually, hypothermia is not a problem as the child is well covered with drapes. Active heating with forced warm air can be used if there is any concern pertaining to poor temperature control because of low ambient temperature or any other reason. Blood loss is usually minimal but can be substantial if care is not taken in presence of a large mastoid emissary vein. It can be visualised on X-ray or CT scan preoperatively. In order to reduce bleeding into the operating field, mild hypotension and mild hypocapnia can be maintained.
During the conduct of surgery it is essential to identify the facial nerve and it is often done with the help of a nerve stimulator. This precludes use of muscle relaxants and therefore necessitates use of an appropriate technique. It is note worthy that since a cochlear implant is an electric device, a discharge of static electricity can damage the electrical component of the cochlear implant device and/or corrupt the programme in the speech processor. Hence, eletro-surgical instruments should not be used at all once the cochlear implant is in place. Haemostasis may be less than perfect on account of inability to use cautery, however it is not significant. During insertion of electrode array complete haemostasis is to be ensured and mono-polar cautery is contraindicated once the electrode has been inserted (Fig-1). At the conclusion of the operation, BERA testing of the electrode array is used or electrically evoked stapedius reflexes are evaluated to ensure proper function of the receiver stimulator, electrode array and to check the integrity of the implant. During these situations, the concentration of inhalation agents must be kept at the minimal level and no significant fluctuations in blood carbon-di-oxide levels should be allowed to occur. However, one study suggested that with the use of the right intravenous anaesthetics, the data pertaining to electrically evoked stapedius reflex obtained intraoperatively, can be used to prove immediately the functioning of the device, integrity of the peripheral auditory pathways and to predict comfort levels [10]. A post operative X-ray of the position of the array within the cochlea is also taken which serves both as record of the position of the electrode and to assist in making decisions regarding programming. The surgery can often be prolonged especially in new centres and the problems of fatigue related stress should always be addressed. Ear surgery also carries a high rate of PONV 40-50%, when compared with other head and neck surgery [11]. The incidence however was only 15% in our series, perhaps because of prophylactic use of ondansetron.
In the end it will be pertinent to mention that as the number of patients with cochlear implant grows, they are likely to come to hospital for other indications as well. While dealing with a patient with a cochlear implant it is worthwhile to remember that monopolar electro-surgical instruments should not be used on the head and neck of a patient with cochlear implant. This can damage the cochlea and permanently damage the implant. Bipolar electro surgical instruments can be used but direct use over the implant and near extra cochlear electrodes should be avoided. Electro convulsive therapy should not be used on such a patient because of similar reasons. In addition, radiotherapy should not be given directly over the implant as it will cause serious damage to the implant. Besides this, MRI is contraindicated in patients with cochlear implants. These patients should not enter a room with MRI scanner as it can cause extreme tissue damage and implant migration. However, with the newer implants the magnet can be removed by simple surgery and then MRI can be under taken and the magnet replaced after the procedure is complete. The cochlear implant child also should not receive an electric shock or direct blow over the implant or over the head especially while playing (Fig 3). Cochlear implantation is a challenging specialised surgery and anaesthesiologist's awareness of the pitfalls and resourcefulness in dealing with communication impaired, paediatric age group makes the task satisfying. Being an extremely expensive prosthesis the expectations from the surgery and anaesthesia outcome are naturally very high, and all care should be taken to provide the best possible results.
Fig. 3.
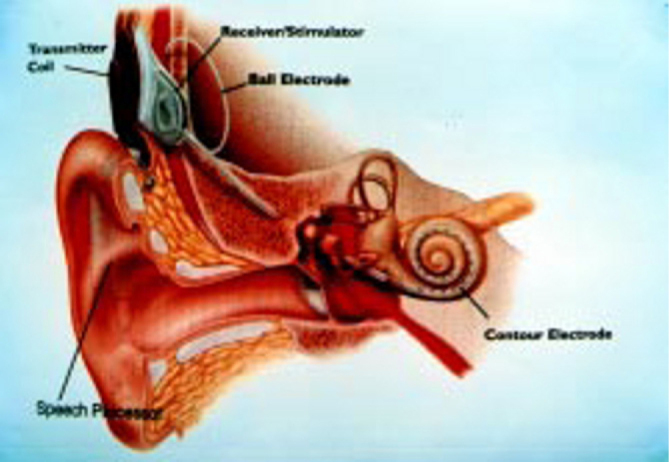
Schematic view of cochlear implant in situ
Acknowledgement
The authors thank Department of ENT, Armed Forces Medical College, Pune for their technical support in preparing the manuscript.
References
- 1.Pedersen CB, Jochumsen U, Madsen S, Koefoed-Nielsen B, Johansen LV. Results and experiences with 55 cochlear implantations. Ugeskr Laeger. 2000;162(40):5346–5350. [PubMed] [Google Scholar]
- 2.Clark GM. The Melbourne Cochlear Implant Programme. In: Clark GM, Cowan RSC, Dowell RC, editors. Cochlear Implantation for infants and children. Singular Publishing Group; San Diego: 1997. pp. 47–70. [Google Scholar]
- 3.O'Sullivan PG, Elli SM, Pyman BC, Clark GM. Proceedings of the XVI World Congress of Otorhinolaryngology. Head and Neck Surgery; Sydney, Australia: 1997. The relationship between aetiology of hearing loss and outcome following cochlear implantation in a paediatric population. [Google Scholar]
- 4.Clark GM, Pyman BC. Preoperative medical evaluation. In: Clark GM, Cowan RSC, Dowell RC, editors. Cochlear implantation for infants and children. Singular Publishing Group; San Diego: 1997. pp. 71–110. [Google Scholar]
- 5.Clark GM, Cohen NL. Surgical and safety considerations of multi-channel cochlear implants in children. Ear and Hearing. 1991;(supplement 12):15–24. doi: 10.1097/00003446-199108001-00004. [DOI] [PubMed] [Google Scholar]
- 6.Clark GM, Pyman BC, Webb RL. Surgery. In: Clark GM, Cowan RSC, Dowell RC, editors. Cochlear implantation for infants and children. Singular Publishing Group; San Diego: 1997. pp. 111–124. [Google Scholar]
- 7.Baines DB, Murrell D. Preoperative hypoglycaemia, propranolol and the Jervell and Lange-Nielsen syndrome. Paediatr Anaesth. 1999;9(2):156–158. doi: 10.1046/j.1460-9592.1999.9220293.x. [DOI] [PubMed] [Google Scholar]
- 8.Green JD, Schuh MJ, Maddern BR, Haymond J, Helffrich RA. Cochlear implantation in Jervell and Lange-Nielsen syndrome. Ann Otol Rhinol Laryngol Suppl. 2000;185:27–28. doi: 10.1177/0003489400109s1211. [DOI] [PubMed] [Google Scholar]
- 9.Hannallah RS, Rosales JK. Experiments with parent's presence during induction in children. Can Anaes Soc J. 1983;30:286. doi: 10.1007/BF03013809. [DOI] [PubMed] [Google Scholar]
- 10.Gnadeberg D, Battmer RD, Lullwitz E, Laszig R, Dybus U, Lenarz T. Effect of anaesthesia on the intraoperative elicited stapedius reflex. Laryngorhinootologie. 1994;73(3):132–135. doi: 10.1055/s-2007-997095. [DOI] [PubMed] [Google Scholar]
- 11.Kenny G. Risk factors for post operative nausea vomiting. Anaesthesia. 1994;49(supplement):6–10. doi: 10.1111/j.1365-2044.1994.tb03576.x. [DOI] [PubMed] [Google Scholar]
- 12.Toner JG, John G, McNaboe EJ. Cochlear implantation under local anaesthesia, the Belfast experience. Laryngol Otol. 1998;112(6):533–536. doi: 10.1017/s0022215100141027. [DOI] [PubMed] [Google Scholar]


