Introduction
Rosacea is a chronic hyperaemic disease of the skin involving the flush area of the face. It is characterized by persistent erythema and often by telangiectasia with acute episodes of oedema, papules, and pustules. It tends to occur more commonly in females between the ages of 30 and 50 years, but it follows a more severe course in males leading to formation of rhinophyma, gnathophyma, etc. Ocular involvement is the most serious complication and can cause conjunctivitis, blepharitis, episcleritis, iritis, and keratitis. Granulomatous rosacea is an atypical variant, characterized by papular and occasionally granulomatous lesions, which on diascopy appear as yellowish brown nodules and on histopathology exhibit epithelioid cell granulomas [1]. We present here one such case.
Case Report
A 35 year old serving soldier was admitted in March 2001 with complaints of recurrent asymptomatic erythematous papulonodular facial lesions of three years duration. These lesions healed spontaneously within 2–3 weeks of onset without scarring or any other sequelae. There was no history suggestive of flushing. The present episode, since the past three weeks was the severest. It was associated with redness and burning over the face, along with redness of the eyes and excessive lacrimation. He gave history of aggravation following sun exposure and intake of hot. spicy food and alcohol, 120 ml being his alcohol intake everyday.
General and systemic examination was normal. Dermatological examination revealed erythema over malar areas, glabella, chin, ala of the nose admixed with multiple erythematous papules, nodules (which turned yellowish on diascopy) and few pustules (Fig 1). The nasolabial folds were spared. Bilateral blepharitis, conjunctivitis photophobia and excessive lacrimation were present.
Fig. 1.
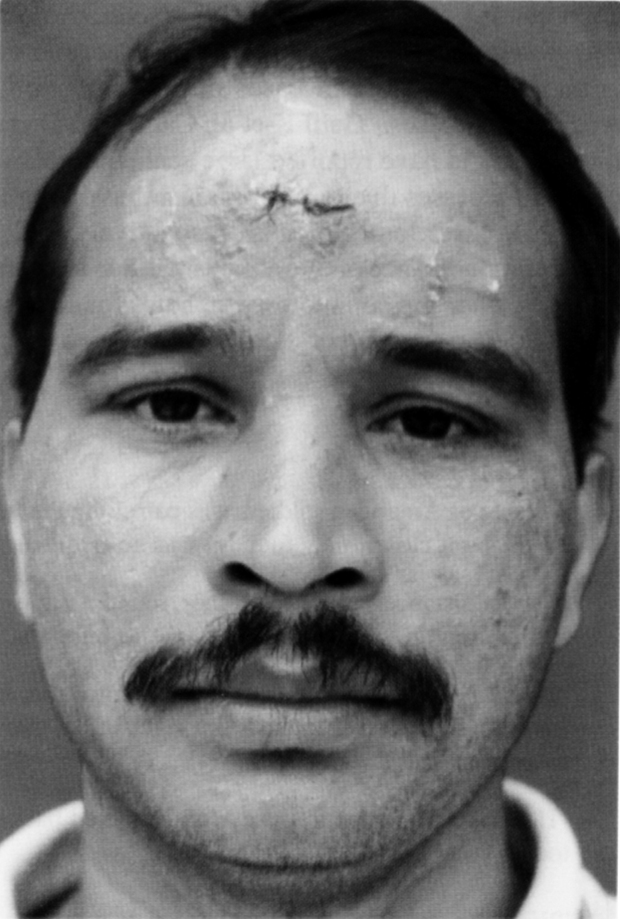
The photograph of the patient showing papulonodular and pustular lesions over the face
Haemogram, ESR, urinalysis, fasting and post prandial blood sugar, blood urea, serum creatinine, peripheral blood smear, platelet count and radiograph of chest were normal. LE cell and ANA were negative. VDRL was nonreactor and Mantoux test showed induration of 8 mm. Skin histopathology showed well defined epithelioid cell granulomas with surrounding mononuclear cell infiltrate and Langhans’ type giant cells in the superficial as well as deep dermis (Fig 2). The patient was diagnosed as a case of granulomatous rosacea, advised photoprotection and treated with Capsule Doxycycline 100 mg twice daily along with topical Norfloxacin, Homatropine and Betnesol eye drops with good response.
Fig. 2.
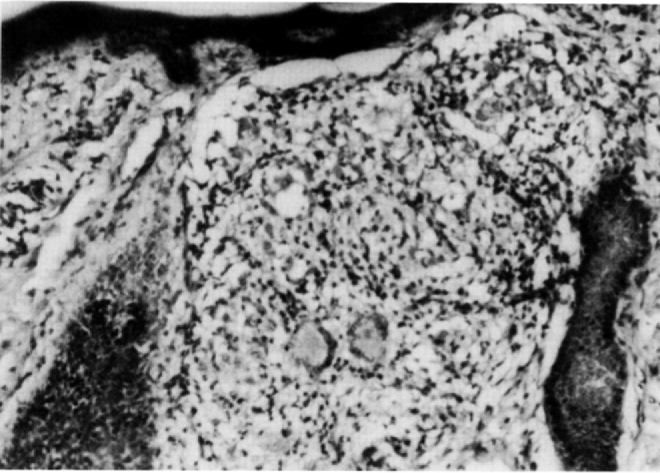
40 X skin histopathology showing epithelioid cells granuloma with Langhan's type giant cells in the dermis
Discussion
The above mentioned case did not evolve through the stages of episodic flushing, persistent erythema, telangiectasia and papular lesions, as is usually seen in a classical case of rosacea. Episodic erythematous papulonodular lesions occurring in the centrofacial area and the lack of laboratory support in favour of the clinical differentials like LE, secondary syphilis, tuberculids and sarcoidosis corroborated our clinical suspicion and the presence of granulomatous dermal infiltrates on histopathology confirmed the impression of granulomatous rosacea in this case. Because of its granulomatous histopathological appearance, the condition has been given misleading names such as rosacea-like tuberculid, lupoid rosacea, and micropapular tuberculid [2]. Epithelioid cell granulomas have been seen in about 10% of all cases of rosacea [3, 4]. Multinucleate giant cells of foreign body type have been seen more frequently [3, 5]. Occasionally, Langhans’ type giant cells may also be seen [6]. The probability of a histopathological dilemma consequent to such granulomatous dermal infiltrate can only be obviated by a meticulous history and a detailed clinical examination.
Fig. 3.
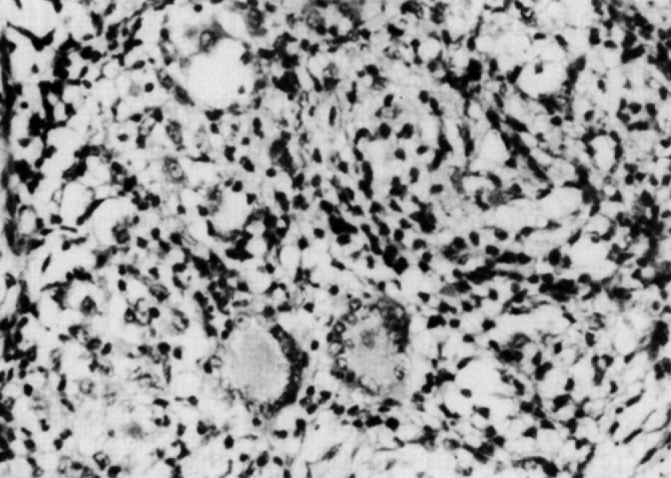
100 X skin histopathology showing Langhan's type giant cells in a case of granulomatous rosacea
References
- 1.Tolman El. Acne and acneiform dermatosis. In: Moschella SL, Hurley HJ, editors. Dermatology. 3rd ed. 1992. pp. 1477–1492. [Google Scholar]
- 2.White CR., Jr . Predominantly mononuclear cell granuloma. In: Farmer ER, Hood AF, editors. Pathology of the Skin. 2nd ed. McGraw Hill; New York: 1999. pp. 361–371. [Google Scholar]
- 3.Marks R, Harcourt Webster JN. Histopathology of rosacea. Arch Dermatol. 1969;100:683–691. [PubMed] [Google Scholar]
- 4.Helm KF, Menz J, Gibson LE, Dicken CH. A clinical and histopathological study of granulomatous rosacea. J Am Acad Dermatol. 1991;25:1038–1043. doi: 10.1016/0190-9622(91)70304-k. [DOI] [PubMed] [Google Scholar]
- 5.Ecker RI, Winkelman RK. Demodex granuloma. Arch Dermatol. 1979;115:343–344. doi: 10.1001/archderm.1979.04010030051021. [DOI] [PubMed] [Google Scholar]
- 6.Grosshans E, Kremer M, Maleville J. Du role des Demodex folliculorum dans Phistogenese de la rosacee granulomateuse. Bull Soc Fr Dermatol Syphilyr. 1972;79:639–646. [Google Scholar]


