Abstract
Purpose
To measure and compare the depth of cure (DOC) of two bulk fill composite resins using a monowave and polywave light curing unit (LCU) according to ISO 4049 and using custom tooth molds.
Methods
The DOC of Tetric Evoceram Bulk Fill (Ivoclar Vivadent) and Filtek Bulk Fill Posterior (3M ESPE) were measured using a monowave LED LCU (Elipar S10 / 3M ESPE) and a polywave LED LCU (Bluephase G2 / Ivoclar Vivadent). Metal molds were used to fabricate 10 mm long DOC specimens (n=10) according to ISO 4049. Uncured composite material was scraped away with a plastic instrument and half the length of remaining composite was measured as the DOC. Custom tooth molds were fabricated by preparing >10mm long square-shaped (4 × 4 mm) holes into the mesial/distal surfaces of extracted human molars. Composite resin was placed into one end of the prepared tooth and light polymerized. Uncured composite resin was removed from the opposite side from which the tooth was irradiated and the tooth was sectioned mesio-distally. Half the length of remaining cured composite was measured as the DOC. Data were analyzed by three-way ANOVA (alpha=0.05) for factors material, LCU, and mold.
Results
The main effect LCU was not significant (p=.58). The interaction effect between material × mold was significant (p=.0001). The DOC of the composites differed significantly only with the stainless steel mold in which Tetric Evoceram Bulk Fill showed a deeper DOC than Filtek Bulk Fill Posterior (4.03 ± 0.14 vs 3.56 ± 0.38 mm, p<.0001).
INTRODUCTION
With resin-based composites (RBC) comprising over 95% of direct anterior restorations and 50% of direct posterior restorations,1 the demand for improved mechanical properties has encouraged further investigation and development of these materials. One of the disadvantages of many current RBCs is the requirement to incrementally place and cure 2 mm layers of the material;2–5 however, recently developed bulk-fill composites have demonstrated depth of cure (DOC) measurements of 4 mm.6–10 The polymerization of a dental composite is the underlying source of its strength, hardness, wear resistance, and prevention of monomer elution.11–19 Recurrent caries and bulk fracture are the leading causes of composite restoration failure,20–22 and a reduced DOC has been shown to lead to inadequate physical properties that can ultimately lead to clinical failure.16
The DOC of dental composites can be measured using a variety of different methods. The most accurate means of measuring the extent of resin polymerization is to determine the degree of double bond conversion by either fourier transform infra-red or Raman spectroscopy.23 The extent of polymerization has also been shown to correlate to microhardness, allowing for the measurement of hardness at incremental depths to more easily determine the DOC.2, 24–27 The ISO 4049 standard evaluates DOC by dispensing composite resin into a 4 mm diameter opening of a stainless steel mold. After light polymerization, the uncured composite is removed with a plastic spatula, and the height of the intact composite is divided in half to determine the DOC.28 Half of the height of the specimen is used to determine the DOC because the entirety of the specimen is not sufficiently cured.18, 26
Stainless steel molds in the ISO 4049 standard may not accurately reflect the DOC obtained clinically due to the differences in the optical properties of stainless steel and tooth structure. Light transmittance through translucent tooth structure29, 30 may enhance the DOC of composite materials similar to the increased DOC reported with Teflon molds.31, 32 On the other hand, the walls of stainless steel molds exhibit greater reflectivity than those of natural tooth structure. Stainless steel has an index of refraction (IOR) of 2.533 while cementum, dentin, enamel have IORs of 1.58, 1.54, and 1.63, respectively.34–36 The difference in light absorbance and reflectivity of stainless steel may lead to an increased curing ability that does not effectively mimic light curing in natural tooth structure.
Bulk-fill composites use different mechanisms to increase the DOC. While some composites have increased translucency to create deeper light penetration and DOC, others incorporate additional photoinitiators.36,37 Current RBCs utilize a variety of alpha diketone initiators such as camphorquinone (CQ), phenylpropanedione (PPD), and acylphosphine oxide (Lucerin TPO) and germanium-based compounds such as bis-(4-methoxybenzoyl)diethyl-germane (Ivocerin) that can be irradiated using visible light.38 The activation of these photoinitiators is dependent upon the appropriate dental LCU irradiating at wavelengths that overlap the absorption of the photoinitiator. Two common types of dental LCUs are quartz halogen tungsten (QHT) and high-intensity light-emitting diode (LED). LED LCUs have become increasingly popular and are more efficient than their QHT counterparts due to their ability to generate narrow ranges of wavelength output near the maximum absorbance of CQ (about 468 nm).39 The narrow spectrum of monowave LCUs may hinder their ability to optimally cure bulk-fill composites that incorporate multiple photoinitiators with varying peak absorption ranges; however, polywave curing lights use multiple LEDs which emit different wavelengths of light to polymerize different photoinitiators.
The purpose of this study was to compare the depth of cure of two bulk-fill resin-based composites when irradiated with a monowave and polywave LED LCU. The study also compared the ability to accurately measure DOC in the metal molds described in ISO 4049 versus custom tooth molds. The first null hypothesis was that both the monowave and polywave LCUs would achieve similar DOC values when irradiating either resin-based composite. The second null hypothesis was that both resin-based composites would achieve similar DOC values when irradiated in the metal mold and the tooth mold.
MATERIAL AND METHODS
A stainless steel mold containing a rectangular hole (4 mm × 4 mm × 10 mm) was fabricated for ISO DOC measurements. The rectangular shape of the hole differs slightly from the traditional ISO mold, however, this shape was chosen to allow hardness measurements in future studies. Specimens were prepared by dispensing composite material into the mold in a single increment. The two composite materials were Tetric EvoCeram Bulk Fill (Ivoclar Vivadent, shade IVA) containing the initiators CQ and Ivocerin and Filtek Bulk Fill Posterior (3M ESPE, shade A2) containing the initiator CQ. A mylar film and glass slide were placed over the composite with the LCU centered over the hole and held in contact with the glass slide using a fixed arm. Each composite was irradiated once for the length of time recommended by the manufacturer (10 seconds for Tetric EvoCeram and 20 seconds for Filtek Bulk Fill Posterior). Each material was tested with both a monowave LED LCU (Elipar S10; 3M ESPE) and a polywave LED LCU (Bluephase G2; Ivoclar Vivadent). Light emittance was measured daily using a radiometer (Power Max; Molectron Detector, Inc.) to ensure consistent irradiance. The specimens were then removed from the mold, and the uncured RBC was manually removed by scraping with a plastic spatula. The intact length of the specimens was measured with digital calipers to the nearest 0.01 mm and divided in half to determine DOC.
40 extracted human first, second, and third maxillary and mandibular molars were collected and mounted in acrylic. A square-shaped hole (4 mm × 4 mm) extending the length of the mesial-distal axis of the tooth (>10mm) was prepared by two trained operators under water lubrication using dental diamond burs (8856DF.31.016, Brasseler) in a high speed handpiece (Figure 1). The holes were examined with a periodontal probe to ensure dimensions were accurate to within 0.5 mm. If small perforations (less than 1 mm) occurred through the occlusal surface or pulp chamber, they were repaired with A3 resin composite (Z100, 3M ESPE). If a large perforation occurred, the tooth was discarded. An opaque adhesive strip was placed to cover one end of the hole (bottom), and the resin composite was then condensed into the other end of the hole (top). The LCU was centered over the top hole and positioned in contact with the composite material. Each composite was irradiated with both LCUs for the length of time recommended by the manufacturer. The adhesive strip was then removed, and the uncured resin composite was removed from the bottom hole. Using a diamond disc in a laboratory handpiece, the tooth was sectioned mesio-distally through the middle of the square-shaped hole into an occlusal and apical section (Figure 2). Any remaining uncured composite was scraped away with a plastic spatula. The maximum intact length of the RBC was measured with digital calipers to the nearest 0.01 mm and divided in half to determine DOC.
Figure 1.
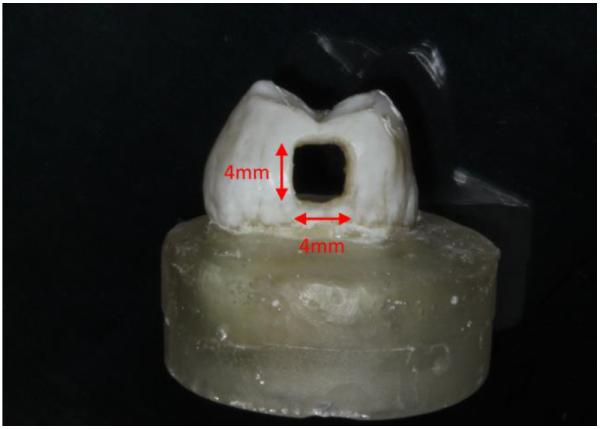
Mounted tooth mold
Figure 2.
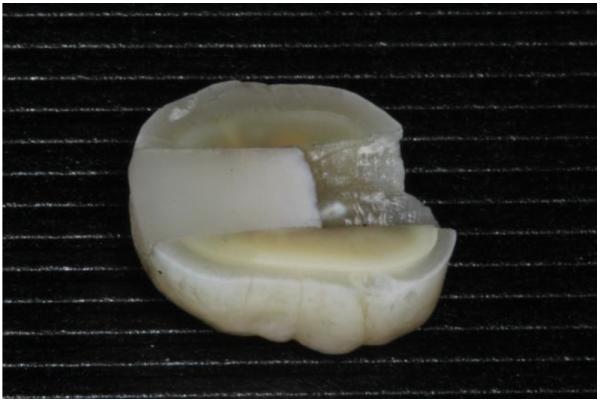
Apical section of tooth mold containing cured composite
The DOC data were analyzed using a three-way ANOVA, followed by a post-hoc test for any significant factor or interaction. A p-value < 0.05 was considered statistically significant in two-tailed statistical tests. All analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC, USA). The graphical displays were created by R 3.2.0.
The mean irradiance (mW/cm2), total energy density (J/cm2), energy distribution per spectrum (J/cm2), and spectral irradiance (mW/cm2/nm) of each LED light was obtained by MARC® PS system (Blue Light Analytics). The MARC® device has built-in laboratory grade UV-VIS spectrometer (USB4000, Ocean Optics), spectral range from 365 – 515 nm and a laboratory-grade cosine-corrected sensor. This can measure intensity up to 10,000 mW/cm2 (integration times are used to enable changes in intensity and prevent saturation). The tested LCU light probe was set 0 mm from the sensor and the reading was rendered in 10 seconds utilizing MARC® software v. 3.04.
RESULTS
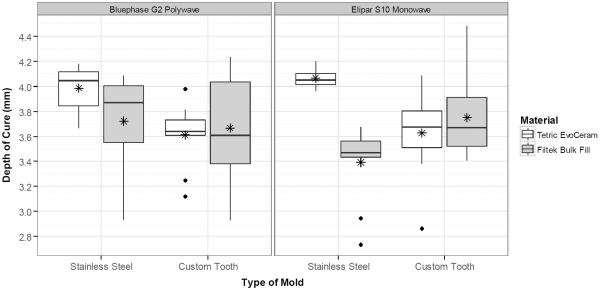
Result of the three-way ANOVA is presented in Table 1. The DOC of two resin-based composites irradiated with two different LCUs in two different mold types are shown in Figure 3. The main effects of mold (p=.07) and LCU (p=.58) on DOC were not significant. Only the effect of material on DOC was significant (p=.007). However this effect was dependent on the mold and characterized by a significant interaction between the material and type of mold used (p=.0001). Using the stainless steel mold, Tetric Evoceram Bulk Fill produced a higher DOC compared to Filtek Bulk Fill Posterior (4.03 ± 0.14 vs 3.56 ± 0.38 mm, p<.0001). Conversely, there was no significant difference in the DOC between the two resin-based composites with the use of the tooth mold (3.62 ± 0.29 vs 3.71 ± 0.37 mm, p=0.36).
Table 1.
Result of three-way ANOVA
| Source of Variation | DF | Sum of Squares | Mean Squares | F | p |
|---|---|---|---|---|---|
| Mold | 1 | 0.325 | 0.325 | 3.48 | 0.07 |
| Material | 1 | 0.724 | 0.724 | 7.76 | 0.007* |
| LCU | 1 | 0.029 | 0.029 | 0.31 | 0.58 |
| Material × LCU | 1 | 0.144 | 0.144 | 1.54 | 0.22 |
| Mold × LCU | 1 | 0.151 | 0.151 | 1.62 | 0.21 |
| Material × Mold | 1 | 1.551 | 1.551 | 16.6 | 0.0001* |
| Mold × Material × LCU | 1 | 0.286 | 0.286 | 3.06 | 0.08 |
Denotes statistical significance at p < 0.05
Figure 3.
Depth of cure comparison of two resin-based composites irradiated with two different LCUs in two different mold types. The asterisk denotes the mean value for depth of cure.
For the Elipar S10 monowave LCU, the mean irradiance was 1328 mW/cm2, total energy density was 13.5 J/cm2, and energy distribution was 0.1 J/cm2 at the 380-420 nm spectrum and 13.4 J/cm2 at the 420-540 nm spectrum. For the Bluephase G2 polywave LCU, the mean irradiance was 1069 mW/cm2, total energy density was 10.9 J/cm2, and energy distribution was 1.2 J/cm2 at the 380-420n m spectrum and 9.7 J/cm2 at the 420-540 nm spectrum. The spectral peak for the Elipar S10 monowave LCU was 450.2 nm, while the Bluephase G2 polywave LCU spectral peaks were 453.7 and 409.3 nm.
DISCUSSION
The first null hypothesis of this study was that type of LCU would not affect the DOC of the two materials. The main effect LCU was not significant (p=.58); therefore, we fail to reject the first null hypothesis. This result was surprising due to the expectation that a polywave LCU was necessary to excite the Ivocerin initiator present in Tetric Evoceram Bulk Fill. Ivocerin, the germanium-based compound bis-(4-methoxybenzoyl)diethyl-germane, has a peak absorbance at 408 nm; however, nearly 50% of its peak absorbance occurs at 440nm.40 The monowave Elipar S10 LCU has an utilizable wavelength range of 430–480 nm with a peak at 455 nm ± 10 nm. Therefore, there is some overlap in the absorbance of Ivocerin and the spectral irradiance of the Elipar S10 LCU; and this overlap may have allowed initiation of the Ivocerin.
The inability of the polywave LCU to achieve a deeper DOC may be due to absorbance of violet range of light (~410nm) in the top layers of the composite. A recent study performed with a phenanthrenequinone (PQ) initiator measured its peak absorption at 413 nm as 8× the absorbance of CQ;41 however, a composite resin with the PQ initiator registered nearly half the depth of cure (scrape method) as a similar CQ-based composite. The authors of that study postulated that due to the high absorbance of PQ, most of the light photons were depleted in the top layers of the composite without making it into the depth of the material. Similarly, Ivocerin has a higher absorbance than CQ40 and therefore, may absorb violet light in the top layers of the composite preventing it from traveling deeper within the material.
Another explanation for the lack of effectiveness of the polywave light is due to the relationship that exists between the wavelength of the light from the LCU and the dimensions of the filler particles in the resin composite according to the Rayleigh effect.42 According to the Rayleigh effect, filler particles will be more likely to scatter shorter wavelengths of light. Thus, the violet spectrum of the polywave LCU used in this study was attenuated significantly within the composite, so that most radian exposure at the depth of the specimen was delivered from blue light spectrum.43
The second null hypothesis was that both resin-based composites would achieve similar depth of cure values when irradiated in the metal mold and the tooth mold. The main effect material and the interaction between material and mold were significant (p<.05), so we failed to accept the second null hypothesis. There was a significant difference between the materials in the metal mold but not the tooth mold. There was also greater deviation in data with the tooth mold that may have limited the discerning ability of this mold. This result is expected due to the numerous sources of variation that were inherent in this testing method, including thickness of enamel and dentin, orientation of enamel rods and dentinal tubules, desiccation of teeth, dimensions of holes, and roughness of the holes. The elimination of these variables in addition to ease of fabrication are two arguments to favor stainless steel molds.
Although differences were seen between the discerning power of the two mold types (metal and tooth), there was no significant difference between the main effect mold (p=.07). This result was surprising as stainless steel and tooth structure (enamel and dentin) have very different optical properties. When light interacts with a solid structure, it may be transmitted, reflected, or absorbed. Since stainless steel is an opaque metal, it does not transmit light, unlike ceramic or polymeric materials. Previous studies which used Teflon molds reported exaggerated DOC values since light was transmitted through the Teflon more than it was through the composite resin.31, 32 Tooth structure is only partially translucent with 1 mm of enamel attenuating 67% of light (430–550 nm) and 1 mm of dentin attenuating 85–90% of light (400–550 nm).29, 30 Therefore, light from the LCU likely did not transmit much more than 2–3 mm through the walls of the mold, and the transmitted light would have been significantly attenuated. The index of refraction (IOR) of the stainless steel was greater than the IOR of dentin or enamel, suggesting that more light would have been reflected off the walls of the stainless steel mold.33–36 Additionally, since stainless steel is a metal, light would be more likely to be reflected from its surface than absorbed. A previous study found that molds lined with black vinyl tape produced lower DOC than those lined with white tape, since black tape absorbs more light.44 In the current study, the cured composite that remained in the tooth appears convex (Figure 2) which may be an indication that the walls of the tooth mold absorbed light.
Based on the results of this study, there was no significant difference in the DOC achieved with a metal mold and stainless steel mold, however, the stainless steel mold had greater discerning ability between materials. These results suggest the dual relevance and practicality of using a stainless steel mold for DOC testing. One major limitation of the study was that rectangular shaped holes were used instead of circular shaped holes. A previous study demonstrated that the size of the hole significantly affects DOC.44 The rectangular hole was chosen in the current study to use a mold that could also be used for hardness testing. This choice, however, limits the ability of this study to validate the ISO DOC standard.
No significant difference was noted between the monowave and polywave LCU in the DOC of Tetric Evoceam Bulk Fill. Therefore, the use of a polywave LCU is not mandatory to achieve optimal DOC of a new bulk fill composite with a germanium-based photoinitiator. Other properties, such as degree of conversion, strength, or hardness may be affected by choice of LCU and these properties should be addressed in future studies.
Clinical relevance.
The use of a polywave LCU is not mandatory to achieve optimal DOC of a new bulk fill composite with a germanium–based photoinitiator. However, other properties, such as degree of conversion, strength, or hardness may be affected by choice of LCU.
ACKNOWLEDGEMENTS
This project is based upon a grant from Ivoclar Vivadent, however, they had no role in study design, data collection, analysis or interpretation, or manuscript preparation. Statistical analysis of research reported in this publication was partially supported by National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR00165. The authors thank Hillary Sawyer and Aarika Mitchell for their assistance with the project.
REFERENCES
- [1].Stein PS, Sullivan J, Haubenreich JE, Osborne PB. Composite resin in medicine and dentistry. J Long Term Eff Med Implants. 2005;15:641–654. doi: 10.1615/jlongtermeffmedimplants.v15.i6.70. [DOI] [PubMed] [Google Scholar]
- [2].Santos GB, Medeiros IS, Fellows CE, Muench A, Braga RR. Composite depth of cure obtained with QTH and LED units assessed by microhardness and micro-Raman spectroscopy. Oper Dent. 2007;32:79–83. doi: 10.2341/06-26. [DOI] [PubMed] [Google Scholar]
- [3].Monte Alto RV, Guimaraes JG, Poskus LT, da Silva EM. Depth of cure of dental composites submitted to different light-curing modes. J Appl Oral Sci. 2006;14:71–76. doi: 10.1590/S1678-77572006000200002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Moore BK, Platt JA, Borges G, Chu TM, Katsilieri I. Depth of cure of dental resin composites: ISO 4049 depth and microhardness of types of materials and shades. Oper Dent. 2008;33:408–412. doi: 10.2341/07-104. [DOI] [PubMed] [Google Scholar]
- [5].de Camargo EJ, Moreschi E, Baseggio W, Cury JA, Pascotto RC. Composite depth of cure using four polymerization techniques. J Appl Oral Sci. 2009;17:446–450. doi: 10.1590/S1678-77572009000500018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Alrahlah A, Silikas N, Watts DC. Post-cure depth of cure of bulk fill dental resin-composites. Dent Mater. 2014;30:149–154. doi: 10.1016/j.dental.2013.10.011. [DOI] [PubMed] [Google Scholar]
- [7].Benetti AR, Havndrup-Pedersen C, Honore D, Pedersen MK, Pallesen U. Bulk-fill resin composites: polymerization contraction, depth of cure, and gap formation. Oper Dent. 2015;40:190–200. doi: 10.2341/13-324-L. [DOI] [PubMed] [Google Scholar]
- [8].Garcia D, Yaman P, Dennison J, Neiva G. Polymerization shrinkage and depth of cure of bulk fill flowable composite resins. Oper Dent. 2014;39:441–448. doi: 10.2341/12-484-L. [DOI] [PubMed] [Google Scholar]
- [9].Jang JH, Park SH, Hwang IN. Polymerization shrinkage and depth of cure of bulk-fill resin composites and highly filled flowable resin. Oper Dent. 2015;40:172–180. doi: 10.2341/13-307-L. [DOI] [PubMed] [Google Scholar]
- [10].Rouhollahi M, Mohammadibasir M, Talim S. Comparative depth of cure among two light-cured core build-up composites by surface vickers hardness. J Dent (Tehran) 2012;9:255–261. [PMC free article] [PubMed] [Google Scholar]
- [11].Ferracane JL. Developing a more complete understanding of stresses produced in dental composites during polymerization. Dent Mater. 2005;21:36–42. doi: 10.1016/j.dental.2004.10.004. [DOI] [PubMed] [Google Scholar]
- [12].Esmaeili B, Safarcherati H, Vaezi A. Hardness evaluation of composite resins cured with QTH and LED. J Dent Res Dent Clin Dent Prospects. 2014;8:40–44. doi: 10.5681/joddd.2014.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kawai K, Iwami Y, Ebisu S. Effect of resin monomer composition on toothbrush wear resistance. J Oral Rehabil. 1998;25:264–268. doi: 10.1111/j.1365-2842.1998.00246.x. [DOI] [PubMed] [Google Scholar]
- [14].Musanje L, Ferracane JL, Ferracane LL. Effects of resin formulation and nanofiller surface treatment on in vitro wear of experimental hybrid resin composite. J Biomed Mater Res B Appl Biomater. 2006;77:120–125. doi: 10.1002/jbm.b.30400. [DOI] [PubMed] [Google Scholar]
- [15].Cook WD. Factors affecting the depth of cure of UV-polymerized composites. J Dent Res. 1980;59:800–808. doi: 10.1177/00220345800590050901. [DOI] [PubMed] [Google Scholar]
- [16].Ferracane JL, Mitchem JC, Condon JR, Todd R. Wear and marginal breakdown of composites with various degrees of cure. J Dent Res. 1997;76:1508–1516. doi: 10.1177/00220345970760081401. [DOI] [PubMed] [Google Scholar]
- [17].Poskus LT, Placido E, Cardoso PE. Influence of adhesive system and placement technique on microleakage of resin-based composite restorations. J Adhes Dent. 2004;6:227–232. [PubMed] [Google Scholar]
- [18].Ruyter IE, Oysaed H. Conversion in different depths of ultraviolet and visible light activated composite materials. Acta Odontol Scand. 1982;40:179–192. doi: 10.3109/00016358209012726. [DOI] [PubMed] [Google Scholar]
- [19].Yearn JA. Factors affecting cure of visible light activated composites. Int Dent J. 1985;35:218–225. [PubMed] [Google Scholar]
- [20].Bernardo M, Luis H, Martin MD, Leroux BG, Rue T, Leitao J, DeRouen TA. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. J Am Dent Assoc. 2007;138:775–783. doi: 10.14219/jada.archive.2007.0265. [DOI] [PubMed] [Google Scholar]
- [21].Opdam NJ, Bronkhorst EM, Roeters JM, Loomans BA. A retrospective clinical study on longevity of posterior composite and amalgam restorations. Dent Mater. 2007;23:2–8. doi: 10.1016/j.dental.2005.11.036. [DOI] [PubMed] [Google Scholar]
- [22].Rasines Alcaraz MG, Veitz-Keenan A, Sahrmann P, Schmidlin PR, Davis D, Iheozor-Ejiofor Z. Direct composite resin fillings versus amalgam fillings for permanent or adult posterior teeth. Cochrane Database Syst Rev. 2014;3:CD005620. doi: 10.1002/14651858.CD005620.pub2. [DOI] [PubMed] [Google Scholar]
- [23].Pianelli C, Devaux J, Bebelman S, Leloup G. The micro-Raman spectroscopy, a useful tool to determine the degree of conversion of light-activated composite resins. J Biomed Mater Res. 1999;48:675–681. doi: 10.1002/(sici)1097-4636(1999)48:5<675::aid-jbm11>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- [24].Ferracane JL. Correlation between hardness and degree of conversion during the setting reaction of unfilled dental restorative resins. Dent Mater. 1985;1:11–14. doi: 10.1016/S0109-5641(85)80058-0. [DOI] [PubMed] [Google Scholar]
- [25].Rueggeberg FA, Ergle JW, Mettenburg DJ. Polymerization depths of contemporary light-curing units using microhardness. J Esthet Dent. 2000;12:340–349. doi: 10.1111/j.1708-8240.2000.tb00243.x. [DOI] [PubMed] [Google Scholar]
- [26].Bouschlicher MR, Rueggeberg FA, Wilson BM. Correlation of bottom-to-top surface microhardness and conversion ratios for a variety of resin composite compositions. Oper Dent. 2004;29:698–704. [PubMed] [Google Scholar]
- [27].Yan YL, Kim YK, Kim KH, Kwon TY. Changes in degree of conversion and microhardness of dental resin cements. Oper Dent. 2010;35:203–210. doi: 10.2341/09-174-L. [DOI] [PubMed] [Google Scholar]
- [28].ISO 4049: Polymer-based restorative materials. 2009. pp. 1–28. [Google Scholar]
- [29].Arikawa H, Kanie T, Fujii K, Ban S, Takahashi H. Light-attenuating effect of dentin on the polymerization of light-activated restorative resins. Dent Mater J. 2004;23:467–473. doi: 10.4012/dmj.23.467. [DOI] [PubMed] [Google Scholar]
- [30].Arikawa H, Kanie T, Fujii K, Fukui K, Homma T. Mechanical properties of light-cured composite resins cured through filters that simulate enamel. Dent Mater J. 2002;21:147–155. doi: 10.4012/dmj.21.147. [DOI] [PubMed] [Google Scholar]
- [31].Dunne SM, Davies BR, Millar BJ. A survey of the effectiveness of dental light-curing units and a comparison of light testing devices. Br Dent J. 1996;180:411–6. doi: 10.1038/sj.bdj.4809107. [DOI] [PubMed] [Google Scholar]
- [32].Harrington E, Wilson HJ. Depth of cure of radiation-activated materials- effect of mould material and cavity size. J Dent. 1993;21:305–311. doi: 10.1016/0300-5712(93)90114-6. [DOI] [PubMed] [Google Scholar]
- [33].Stokkers GJ, van Silfhout A, Bootsma GA, Fransen T, Gellings PJ. Interaction of oxygen with an AISI 314 stainless steel surface studied by ellipsometry and auger electron spectroscopy in combination with ion bombardment. Corros Sci. 1983;23:195–204. [Google Scholar]
- [34].Meng Z, Yao XS, Yao H, Liang Y, Liu T, Li Y, Wang G, Lan S. Measurement of the refractive index of human teeth by optical coherence tomography. J Biomed Opt. 2009;14:034010. doi: 10.1117/1.3130322. [DOI] [PubMed] [Google Scholar]
- [35].Wang XJ, Milner TE, de Boer JF, Zhang Y, Pashley DH, Nelson JS. Characterization of dentin and enamel by use of optical coherence tomography. Appl Opt. 1999;38:2092–2096. doi: 10.1364/ao.38.002092. [DOI] [PubMed] [Google Scholar]
- [36].Arikawa H, Shinohara N, Takahashi H, Kanie T, Fujii K, Ban S. Light transmittance characteristics and refractive indices of light-activated pit and fissure sealants. Dent Mater J. 2010;29:89–96. doi: 10.4012/dmj.2009-042. [DOI] [PubMed] [Google Scholar]
- [37].Shortall AC, Palin WM, Burtscher P. Refractive index mismatch and monomer reactivity influence composite curing depth. J Dent Res. 2008;87:84–8. doi: 10.1177/154405910808700115. [DOI] [PubMed] [Google Scholar]
- [38].Arikawa H, Takahashi H, Kanie T, Ban S. Effect of various visible light photoinitiators on the polymerization and color of light-activated resins. Dent Mater J. 2009;28:454–460. doi: 10.4012/dmj.28.454. [DOI] [PubMed] [Google Scholar]
- [39].Jimenez-Planas A, Martin J, Abalos C, Llamas R. Developments in polymerization lamps. Quintessence In. 2008;39:e74–84. [PubMed] [Google Scholar]
- [40].Moszner N, Zeuner F, Lamparth I, Fischer UK. Benzoylgermanium derivatives as novel visible-light photoinitiators for dental composites. Macromol Mater Eng. 2009;294:877–886. [Google Scholar]
- [41].Albuquerque PP, Bertolo ML, Cavalcante LM, Pfeifer C, Schneider LF. Degree of conversion, depth of cure, and color stability of experimental dental composite formulated with camphorquinone and phenanthrenequinone photoinitiators. J Esthet Restor Dent. 2015;27:S49–57. doi: 10.1111/jerd.12131. [DOI] [PubMed] [Google Scholar]
- [42].Watts DC. Kinetic mechanism of visible-light-cured resins and resin-composites. In: Watts DC, editor. Setting mechanisms of dental materials, symposium proceedings. 1992. pp. 1–26. [Google Scholar]
- [43].Watts DC. Reaction kinetics and mechanics in photo-polymerized networks. Dent Mater. 2005;21:27–35. doi: 10.1016/j.dental.2004.10.003. [DOI] [PubMed] [Google Scholar]
- [44].Erickson RL, Barkmeier WW. Curing characteristics of a composite. Part 2: the effect of curing configuration on depth and distribution of cure. Dent Mater. 2014;30:e134–45. doi: 10.1016/j.dental.2014.02.013. [DOI] [PubMed] [Google Scholar]