Abstract
Background:
Hand hygiene has been described as the cornerstone and starting point in all infection control programs, with the hands of healthcare staff being the drivers and promoters of infection in critically ill patients. The objectives of this study were to access healthcare workers compliance with the World Health Organization (WHO) prescribed five moments of hand hygiene as it relates to patient care and to determine the various strata of healthcare workers who are in default of such prescribed practices.
Methods:
The study was an observational, cross-sectional one. Hand hygiene compliance was monitored using the hand hygiene observation tool developed by the WHO. A nonidentified observer was used for monitoring compliance with hand hygiene. The observational period was over a 60-day period from August 2015 to October 2015.
Results:
One hundred and seventy-six observations were recorded from healthcare personnel. The highest number of observations were seen in surgery, n = 40. The following were found to be in noncompliance before patient contact – anesthetist P = 0.00 and the Intensive Care Unit P = 0.00 while compliance was seen with senior nurses (certified registered nurse anesthetist [CRNA]) P = 0.04. Concerning hand hygiene after the removal of gloves, the following were areas of noncompliance - the emergency room P = 0.00, CRNA P = 0.00, dental P = 0.04, and compliance was seen with surgery P = 0.01. With regards to compliance after touching the patient, areas of noncompliance were the anesthetists P = 0.00, as opposed to CRNA P = 0.00, dental P = 0.00, and Medicine Department P = 0.02 that were compliant. Overall, the rates of compliance to hand hygiene were low.
Discussion:
The findings however from our study show that the rates of compliance in our local center are still low. The reasons for this could include lack of an educational program on hand hygiene; unfortunately, healthcare workers in developing settings such as ours regard such programs as being mundane.
Conclusion:
The observance of hand hygiene is still low in our local environment. Handwashing practices in our study show that healthcare workers pay attention to hand hygiene when it appears there is a direct observable threat to their wellbeing. Educational programs need to be developed to address the issue of poor hand hygiene.
Keywords: Alcohol hand rub, compliance, hand washing, healthcare associated infections, healthcare workers, infection control
INTRODUCTION
Hand hygiene has been described as the cornerstone and starting point in all infection control programs, with the hands of healthcare staff being the drivers and promoters of infection in critically ill patients. Hand hygiene has been identified as the treating intervention strategy that will drive down cross-transmission of pathogens in the healthcare environment. It has been proven to reduce the incidence of nosocomial infections.1,2
Appropriate hand hygiene practices have been shown to reduce the rates of gastrointestinal, respiratory tract, and skin infections. Such hand hygiene practices of the recent time have included the application of alcohol-based lotions or rubs.3
Healthcare workers handle animate objects which are colonized with bacteria and other microbes. Hands have two microbial floras: Resident and transient. The highest rates of hand colonization are found in the areas such as in the Intensive Care Unit (ICU), in such critical care areas merely touching inanimate objects may lead to contamination.4
It has been postulated that if adequate hand hygiene protocols are strictly followed by healthcare personnel, it could lead to a significant 15–30% reduction in hospital acquired infection; however, observational studies show that hand hygiene compliance rates are about 50% of opportunities in hospitals.5,6
The impact of nonadherence to hand hygiene on the part of healthcare workers is seen in the high rates of nosocomial infections. This is fueled by the lack of improvement strategies in healthcare institutions. Effective strategies targeted at improving hand hygiene should include education and training on hand washing and the donning of gloves.7
The World Health Organization (WHO) has developed an evidence-based measure of hand hygiene called the five moments of hand hygiene which refer to washing hands before touching a patient, before performing an aseptic or clean procedure, after potentials exposure to body fluids, after touching a patient, and after touching the patient surroundings.8
There are varying reports on the rates of contamination of the hand of healthcare workers. Some studies report rates as high as 10–78% among health practitioners with Staphylococcus aureus the predominant organism implicated.9
Contamination of hands by other pathogens in the healthcare environment includes vancomycin-resistant enterococci, Clostridium difficile, and Enterobactereaceae, and some of these organisms persist on the hands for several weeks after colonization.10
Hand hygiene if done properly is the cheapest means of reducing the scaring rates of transmissible infections from healthcare workers to patients. Past studies have demonstrated that efficient hand washing reduces the carriage rates of methicillin resistance S. aureus on the hands of hospital staff.11
Infection control is a Germaine issue germanine in clinical practice with hand hygiene described as the single most effective tool in achieving an efficient infection control program. At Babcock University Teaching Hospital no study has been conducted on the level of compliance of healthcare personnel with regards to hand hygiene practices. This study will avail us the opportunity to assess the prevalent practices of hand hygiene across all strata of personnel.
The data obtained will also be used to develop rational interventional programs for the hospital in achieving best practices with respect to hand hygiene and ultimately efficient infection control programs.
The aim of the study is to assess the level of compliance of healthcare personnel at the Babcock University Teaching Hospital with respect to appropriate hand hygiene practices.
MATERIALS AND METHODS
The study is an observational, cross-sectional one that is to be carried out at the Babcock University Teaching Hospital. These observations are during routine patients care at this semi-urban teaching hospital. The hospital is a 140-bed facility serving both a local and a university community. The hospital consists of both single and multiple room units and shared rooms for inpatients with eleven outpatients clinics. Observation on hand hygiene was conducted both at the inpatients and outpatients units and also within the wards and the ICU.
Hand hygiene compliance was monitored using the hand hygiene observation form developed by the WHO. A nonidentified observer will be used for monitoring compliance with hand hygiene. The observation was conducted in a discreet manner in order not to raise awareness on the part of healthcare staff that their hand hygiene practices were monitored. The observational period was over a 60-day period from August 2015 to October 2015.
The checklist in the assessment included the presence or absence of hand washing facilities with alcohol-based hand rubs. The nature and frequency of hand hygiene were also recorded for analysis. The assessment tools had the following components such as compliance with hand hygiene before touching a patient, after contact with the patient surroundings, after performing an invasive procedure, after contact with body fluids, and after the removal of gloves. Confidentiality was maintained as personal identity was not recorded.
Data were entered into the EPI Info version 3.5.1 system developed by the World Health Organization (WHO) and analyzed with Chi-square; risk ratio and odds ratio calculated with the signification P value set at <0.05. In addition, the confidence interval was set at 95%.
RESULTS
A total of One hundred and seventy six observations were recorded from healthcare personnel. The highest number of observation was seen in the Surgery n = 40 and ICU n = 34, followed by the Emergency Department n = 33 and Internal Medicine n = 32. The GOPD had 21 observations while Dental and Pediatrics had 17 and 10 respectively [Figure 1].
Figure 1.
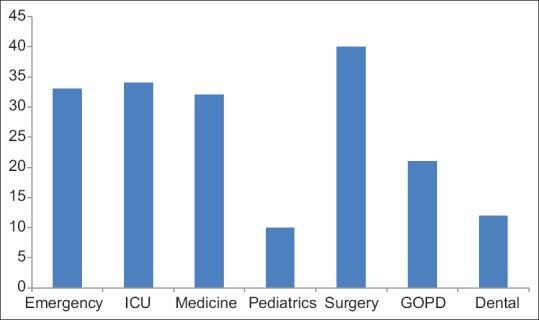
Observations of hand washing by wards
With respect to personnel the nursing department had the highest number of observations as 92 Circulating Nurses were sampled followed by 18 Senior Nurses (CRNA). There were also 18 Anesthetists and Resident Doctors, 11 Surgeons, 5 Post-operative Nurses, 3 Surgical Technologists and 1 Medical student [Figure 2].
Figure 2.
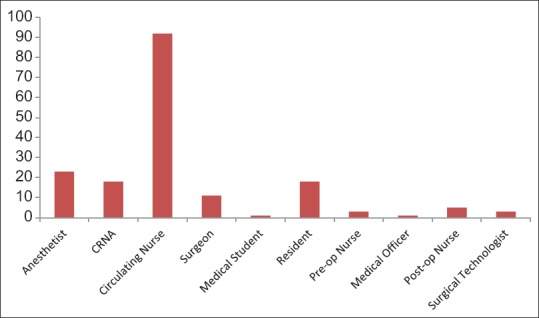
Observations of compliance with hand washing by personnel
With regards to overall compliance in the observance of hand hygiene 10 of the hospital staff were found to be compliant before touching the patient while 165 were non compliant, 48 performed hand hygiene after touching the patient as against 128 that did not, 91 performed hand hygiene before and invasive procedure while 71 did not. In addition 105 washed their hands after removing gloves as opposed to 66 that did not and 72 personnel observed hand hygiene after contact with body fluids and 40 did not [Figure 3].
Figure 3.
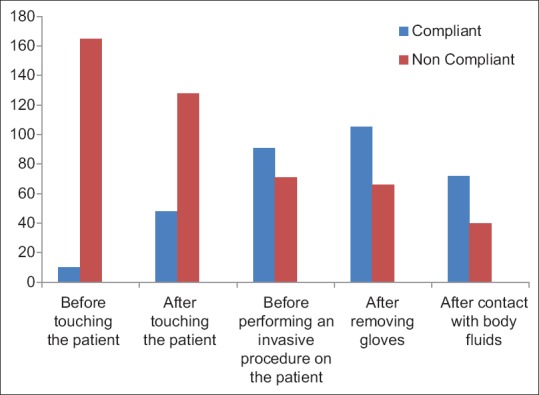
Compliance with the five moments of hand hygiene
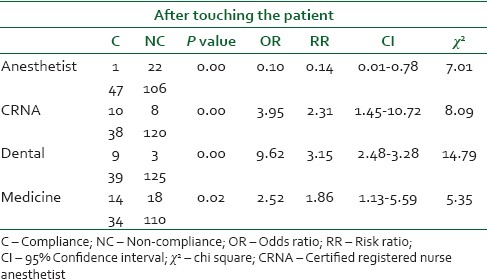
In the statistical analysis of personnel and departments who were compliant with hand hygiene practices before contact with patients in comparison with the hospital population the following were found to be in non-compliance statistically – Anesthetist P = 0.00, and the Intensive Care Unit (ICU) P = 0.00 while compliance was seen with Senior Nurses (CRNA) P = 0.04. Concerning hand hygiene after the removal of gloves the following were areas of non compliance - the Emergency room P = 0.00, CRNA P = 0.00, Dental P = 0.04 and compliance was seen with Surgery P = 0.01. With regards to compliance after touching the patient, areas of non compliance were the Anesthetists P = 0.00, as opposed to CRNA P = 0.00, Dental P = 0.00 and Medicine Department P = 0.02 that were compliant [Tables 1 and 2].
Table 1.
Distribution of personnel and departments with non compliance to appropriate hand hygiene
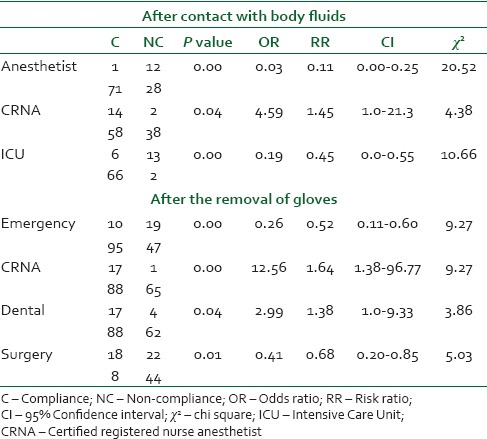
Table 2.
The distribution of personnel and departments with non compliance to appropriate hand hygiene
DISCUSSION
The findings however from our study show that the rates of compliance in our local center are still low. The reasons for this could include lack of an educational program on hand hygiene; unfortunately, healthcare workers in developing settings such as ours regard such programs as being mundane. A similar study to ours conducted by Albert and Condie in the ICU showed that despite the various advancement in infection control, healthcare workers still do not fully adhere to the recommended hand hygiene practices and as such compliances are still low.12
In a systematic review conducted by Erasmus et al., on hand hygiene practices, it was discovered that in ICUs and general wards, the compliance rate was 40% among physicians. This goes show that even in critical care units in hospitals compliance with hand hygiene is still a topical issue.13
In the present study, our observation was that several personnel did not perform hand hygiene before conducting an invasive procedure but simply went on to don their gloves. This also buttresses the fact that for them hand hygiene was basically for their own protection and not that of the patient or the immediate environment.
A variety of factors have seen described as for why healthcare workers do not sanitize their hands before and after patient contact, and these include a high workload, insufficient time, forgetfulness huge workload, lack of running water, and nonavailability of alcohol hand lotions. Hand hygiene has therefore been promoted as one of the tools that will help to mitigate this rise in antimicrobial resistance.14,3
This behavioral pattern is also seen in our study with low levels of compliance with the WHO prescribed five moments of hand hygiene. A worrisome trend is the high noncompliance rates of hand hygiene after touching the patient as the hands of healthcare workers could then become a reservoir for the transmission of pathogens among patients. The several microorganisms causing healthcare-associated infections are regularly mutating and as such their antimicrobial resistance rates are higher in the hospital compared to the community. Such pathogens may enter into the local community via three means: Healthcare workers, discharged patients, or the relatives of such patients who visit the hospital.
Healthcare-associated infections are an important cause of morbidity and mortality in clinical practice and pose a challenge in efficient healthcare delivery, and one of the easily identified routes of transmission of such infections is the hands of healthcare workers. Healthcare-associated infections are a burden to both physicians and patients, as they lead to complications in therapy, overall increase in admission days, increase healthcare costs and may result in mortality.7,15
At the moment, the situation in developing countries is such that hand washing facilities are suboptimal. The nonavailability of sufficient sinks or running water is also impediments. In addressing hand hygiene, however, this is now being addressed with the use of alcohol-based hand rubs. Educational programs must also be supplemented with the presence of an effective infection control team. There must also be an active surveillance system in place to rapidly detect cases of healthcare-associated infections and rip further ones in the bud.16,17,18
Such surveillance systems may also use personnel who have high rates of patient contact to drive the process. The highest rates of direct patient contact in the study were the circulating nurses and the anesthetists. These two categories of healthcare workers are points of easy access to both patients and other healthcare personnel and as such interventional measures may be fashioned around them. In addition, they attract a high degree of respect from their colleagues and as such would be effective in achieving a change in hand hygiene behavior.
The WHO has recommended guidelines for hand hygiene and its central theme is to wash hands with soap and water when it is visibly dirty or soiled with blood or other body fluids or after toilet use. The guidelines recommend washing with water and soap or an alcohol-based hand rub. Studies on the efficiency of alcohol-based hand rubs show that they have good efficacy. This concentration of alcohol ranges from 62% to 95% thus ensuring that they are rapidly bactericidal.19,20
Promoting the use of alcohol-based hand rubs in hospitals in developing countries such as ours will also help drive down the rates of healthcare-associated infections as running water is not always available after patient contact or the performance of invasive procedures. Such alcohol-based hand rubs can be reconstituted in our local pharmacies and made available on a regular basis for hospital use.
CONCLUSION
The observance of hand hygiene is still low in our local environment. Handwashing practices in our study show that healthcare workers pay attention to hand hygiene, when it appears, there is a direct observable threat to their wellbeing. Educational programs need to be developed to address the issue of poor hand hygiene.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Scheithauer S, Kamerseder V, Petersen P, Brokmann JC, Lopez-Gonzalez LA, Mach C, et al. Improving hand hygiene compliance in the emergency department: Getting to the point. BMC Infect Dis. 2013;13:367. doi: 10.1186/1471-2334-13-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pittet D, Hugonnet S, Harbarth S, Mourouga P, Sauvan V, Touveneau S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet. 2000;356:1307–12. doi: 10.1016/s0140-6736(00)02814-2. [DOI] [PubMed] [Google Scholar]
- 3.Bloomfield SF, Asello AE, Cookson B, O'Boyle C, Larson EL. The effectiveness of hand hygiene procedures in reducing the risks of the infections in home and community settings including hand washing and alcohol-based hand sanitizers. Am J Infect Control. 2007;10:27–64. [Google Scholar]
- 4.Boyce JM, Pittet D. Healthcare Infection Control Practices Advisory Committee; HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Guideline for Hand Hygiene in Health-Care Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society for Healthcare Epidemiology of America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR Recomm Rep. 2002;51:1–45. [PubMed] [Google Scholar]
- 5.Grol R, Grimshaw J. From best evidence to best practice: Effective implementation of change in patients' care. Lancet. 2003;362:1225–30. doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]
- 6.Larson E. A causal link between handwashing and risk of infection? Examination of the evidence. Infect Control Hosp Epidemiol. 1988;9:28–36. doi: 10.1086/645729. [DOI] [PubMed] [Google Scholar]
- 7.Andersson AE, Bergh I, Karlsson J, Nilsson K. Patients' experiences of acquiring a deep surgical site infection: An interview study. Am J Infect Control. 2010;38:711–7. doi: 10.1016/j.ajic.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 8.Sax H, Allegranzi B, Uçkay I, Larson E, Boyce J, Pittet D. ‘My five moments for hand hygiene’: A user-centred design approach to understand, train, monitor and report hand hygiene. J Hosp Infect. 2007;67:9–21. doi: 10.1016/j.jhin.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 9.Kampf G, Kramer A. Epidemiologic background of hand hygiene and evaluation of the most important agents for scrubs and rubs. Clin Microbiol Rev. 2004;17:863–93. doi: 10.1128/CMR.17.4.863-893.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mathai E, Allegranzi B, Kilpatrick C, Pittet D. Prevention and control of health care-associated infections through improved hand hygiene. Indian J Med Microbiol. 2010;28:100–6. doi: 10.4103/0255-0857.62483. [DOI] [PubMed] [Google Scholar]
- 11.Peacock Jr, JE, Marsik FJ, Wenzel RP. Methicillin-resistant Staphylococcus aureus: Introduction and spread within a hospital. Ann Intern Med. 1980;93:526–32. doi: 10.7326/0003-4819-93-4-526. [DOI] [PubMed] [Google Scholar]
- 12.Albert RK, Condie F. Hand-washing patterns in medical intensive-care units. N Engl J Med. 1981;304:1465–6. doi: 10.1056/NEJM198106113042404. [DOI] [PubMed] [Google Scholar]
- 13.Erasmus V, Daha TJ, Brug H, Richardus JH, Behrendt MD, Vos MC, et al. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol. 2010;31:283–94. doi: 10.1086/650451. [DOI] [PubMed] [Google Scholar]
- 14.Pittet D. Compliance with hand disinfection and its impact on hospital-acquired infections. J Hosp Infect. 2001;48(Suppl A):S40–6. doi: 10.1016/s0195-6701(01)90012-x. [DOI] [PubMed] [Google Scholar]
- 15.Huis A, Actherberg TV, De Bruin M, Grol R, Schoonhaven L, Hulscher M. A systematic review of hand hygiene improvement strategies: A behavioral approach. BMC Nurs Implement Sci. 2012;7:92. doi: 10.1186/1748-5908-7-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Megeus V, Nilsson K, Karlsson J, Eriksson BI, Andersson AE. Hand hygiene and aseptic techniques during routine anesthetic care - Observations in the operating room. Antimicrob Resist Infect Control. 2015;4:5. doi: 10.1186/s13756-015-0042-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pittet D, Allegranzi B, Storr J, Bagheri Nejad S, Dziekan G, Leotsakos A, et al. Infection control as a major World Health Organization priority for developing countries. J Hosp Infect. 2008;68:285–92. doi: 10.1016/j.jhin.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 18.Sarma JB, Ahmed GU. Infection control with limited resources: Why and how to make it possible? Indian J Med Microbiol. 2010;28:11–6. doi: 10.4103/0255-0857.58721. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization. WHO Guidelines on Hand Hygiene in Health Care. Geneva: World Health Organization; 2009. [Google Scholar]
- 20.Zaragoza M, Sallés M, Gomez J, Bayas JM, Trilla A. Handwashing with soap or alcoholic solutions? A randomized clinical trial of its effectiveness. Am J Infect Control. 1999;27:258–61. doi: 10.1053/ic.1999.v27.a97622. [DOI] [PubMed] [Google Scholar]


