Abstract
Background:
Galactorrhea is a common manifestation of hyperprolactinemia but may not always be present in women with hyperprolactinemia. This study was, therefore, undertaken to assess the serum prolactin levels of infertile women presenting with galactorrhea and to determine the prevalence of hyperprolactinemia among them.
Materials and Methods:
This was a retrospective study of serum prolactin levels of 63 female partners of infertile couples attending the gynecological clinic of Federal Medical Centre, Birnin Kudu, Jigawa State, Nigeria, who were found to have galactorrhea from January 1, 2012, to December 31, 2013. Ethical clearance was obtained. Solid phase enzyme-linked immunosorbent assay was used to measure serum prolactin. Sociodemographic characteristics were determined. The data obtained were analyzed using SPSS version 17.0 statistical software. Absolute numbers and simple percentages were used to describe categorical variables. Similarly, quantitative variables were described using measures of central tendency (mean, median) and measures of dispersion (range, standard deviation) as appropriate.
Results:
The average age of the women was 27.9 ± 5.6 years. In half of the cases (50%), galactorrhea was associated with menstrual disturbances, mainly amenorrhea (23.3%). Although most (63.3%) of the clients had normal serum prolactin level despite being galactorrheic, averagely there was a marked elevation in serum prolactin of as high as 40.3 ± 52.3 ng/mL.
Conclusion:
We conclude, therefore, that the prevalence of hyperprolactinemia in this study was low when compared with other studies and that galactorrhea does not always indicate raised serum prolactin levels.
Keywords: Galactorrhea, hyperprolactinemia, infertility, Nigeria
INTRODUCTION
Infertility is a common reproductive health issue with incidence ranging from 20% to 46% in parts of West Africa1,2 and it accounts for 45–65% of gynecological consultation.3,4 Hormonal factors are the less common cause of female infertility in sub-Saharan Africa, compared to tubal pathology which is mostly secondary to sexually transmitted disease.1 Emerging result from study done in North Eastern region of Nigeria showed an increase in the trend of hyperprolactinemia among infertile females where a prevalence of 31.7% has been reported.5
Galactorrhea is one of the complaints often associated with infertility. Its relationship with amenorrhea and infertility is well-established.6 Galactorrhea is the inappropriate secretion of breast milk.7 It is a relatively common symptom as 20–25% of women experience galactorrhea at some time in their life.8,9 Lactation requires the presence of estrogen, progesterone, and most importantly, prolactin. Galactorrhea is a common manifestation of hyperprolactinemia but may not always be present in women with hyperprolactinaemia.10 Hyperprolactinemia may also be associated with a variety of menstrual cycle disturbances such as amenorrhea. One study has reported galactorrhea in approximately 40% of hyperprolactinemic patients.11
Galactorrhea may also be due to pituitary tumors, drugs that inhibit hypothalamic dopamine, hypothyroidism, excessive estrogen intake, for example, oral contraceptives, stress, or hypothalamic lesion. Tricyclic antidepressants such as imipramine and dopamine-depleting agents such as α-methyldopa are known to cause galactorrhea.
Although galactorrhea has been reported with normal serum prolactin levels,12 in patients with both galactorrhea and amenorrhea, approximately two-third will have hyperprolactinemia.13 Pathologic hyperprolactinemia inhibits the pulsatile secretion of gonadotropin-releasing hormone, and the reduction of circulatory prolactin level restores menstrual function. Isolated galactorrhea, with normal menstrual cycle and normal serum prolactin levels, has been estimated to occur in up to 20% of women at some point in their lives.14
Nahid, in his evaluation of infertile women who had galactorrhea, concluded that all gynecologists should consider galactorrhea even in women with normal serum prolactin.15 Patients with isolated galactorrhea and normal serum prolactin levels do not require treatment if they are not bothered by the galactorrhea, do not wish to conceive and do not show evidence of hypogonadism or reduced bone density.16
Because of the episodic and labile nature of prolactin secretion, elevated prolactin levels should be confirmed on at least two occasions when the patient is in a fasting, nonexercised state, with no breast stimulation. Correlation exists between serum prolactin levels and presence of prolactinoma, therefore, levels >200 ng/mL (200 mcg/L) are strongly suggestive of prolactinoma.17
Magnetic resonance imaging of the pituitary fossa should be considered if the serum prolactin level is significantly elevated or if a pituitary tumor is suspected.16,18,19 Computed tomography may not be sensitive enough to identify small lesions or large lesions that are isodense with surrounding structures.17
Galactorrhea is a relatively common gynecological symptom and some general practitioners in Nigeria would normally recommend bromocriptine without recourse to serum prolactin levels. The research questions would be, does galactorrhea always indicate raised prolactin levels? does galactorrhea with normal serum prolactin requires treatment? This study was, therefore, undertaken to assess the serum prolactin levels of infertile women presenting with galactorrhea and to determine the prevalence of hyperprolactinemia among them.
MATERIALS AND METHODS
This was a retrospective study of serum prolactin levels of female partners of infertile couples attending the gynecological clinic of Federal Medical Centre, Birnin Kudu, Jigawa State, Nigeria, who were found to have galactorrhea from January 1, 2012, to December 31, 2013. Ethical clearance was obtained from Health Research Ethics Committee of FMC, Birnin Kudu. The FMC is one of the tertiary health facilities in Jigawa State. It was established for provision of service, teaching, and research to cater for the needs of the local and wider community. Patients from other hospitals and clinics are referred here. Birnin Kudu is a rural setting made predominantly of Hausa Muslims.
Laboratory records and case files of 60 female partners of infertile couples were retrieved and studied. These women who presented with galactorrhea were sent for serum prolactin assay.
Solid phase enzyme-linked immunosorbent assay (ELISA) was used to measure serum prolactin and values were expressed in nanogram per milliliter (ng/mL). The kit was produced by Diagnostic Automation/Coates Diagnostics, Inc.
The standard operating procedure for assessment of serum prolactin in the laboratory was as described by.20 The Prolactin Quantitative Test Kit is based on a solid phase ELISA. The assay system utilizes one anti-prolactin antibody for solid phase (microtiter wells) immobilization, and another mouse monoclonal anti-prolactin antibody in the antibody-enzyme (horseradish peroxidase) conjugate solution. The test sample is allowed to react simultaneously with the antibodies, resulting in the prolactin molecules being sandwiched between the solid phase and enzyme-linked antibodies. After a 60 min incubation at room temperature, the wells are washed with water to remove unbound labeled antibodies. A solution of 3,3′,5,5′-tetramethylbenzidine (TMB) is added and incubated for 20 min, resulting in the development of a blue color. The color development is stopped with the addition of 2N HCl, and the color is changed to yellow and measured spectrophotometrically at 450 nm. The concentration of prolactin is directly proportional to the color intensity of the test sample.
Serum prolactin was measured before commencement of treatment. Normal fasting values generally are <30 ng/mL (2–29 ng/mL) usually 1–25 ng/mL20 in nonpregnant women and 10–209 ng/mL in pregnant women depending on the individual laboratory. Although no single test can help determine the etiology of hyperprolactinemia, a prolactinoma is likely if the prolactin level is 250 ng/mL and less likely if the level is <100 ng/mL.
The data obtained were analyzed using SPSS version 17.0 statistical software (SPSS Inc, Chicago, Iloinis, USA). Absolute numbers and simple percentages were used to describe categorical variables. Similarly, quantitative variables were described using measures of central tendency (mean, median) and measures of dispersion (range, standard deviation) as appropriate.
RESULTS
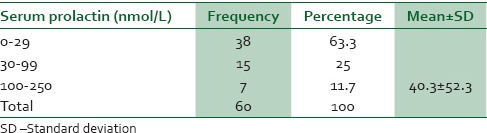
The average age of the women was 27.9 ± 5.6 years [Table 1]. As shown in Table 2, in half of the cases (50%), galactorrhea was associated with menstrual disturbances, mainly amenorrhea (23.3%). Although most (63.3%) of the clients had normal serum prolactin level while 36.7% had elevated serum prolactin levels despite being galactorrheic, averagely there was a marked elevation in serum prolactin of as high as 40.3 ± 52.3 ng/mL [Table 3]. Therefore, the proportion of patients with hyperprolactinemia in the study was 36.7%.
Table 1.
Age distribution of the study population
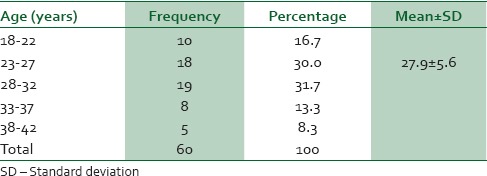
Table 2.
Distribution of menstrual patterns among the study population
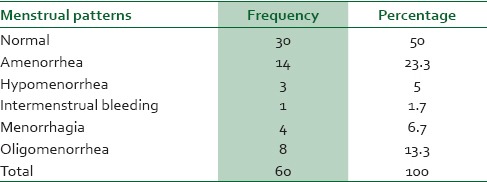
Table 3.
Distribution of serum prolactin levels among the study population
DISCUSSION
Most of the patients were 28-32 years of age and the mean age was 27.9 ± 5.6 years. This age bracket is similar to that in a previous study.21
Our study reports that half (50%) of the clients had normal menstrual patterns, whereas 23.3% had amenorrhea. Our finding was consistent with previous studies where amenorrhea was considered as the most common menstrual disorder associated with galactorrhea.21 Another study where galactorrhea was reported in 75% of hyperprolactinemic patient was, however, on the contrary stating that oligomenorrhea as the most common menstrual disorder occurring in 51.3% of cases.22 In another study, hyperprolactinemia was reported in 61% and galactorrhea in 48% of cases of menstrual disturbance.23 Although what caused the amenorrhea or other menstrual disturbances, whether the hyperprolactinemia or galactorrhea was not stated, we infer from previous studies it was probably due to the hyperprolactinemia.23,24
Our study reports that 63% of the client had normal serum prolactin levels despite presenting with galactorrhea and 37% had serum hyperprolactinemia. The prevalence of hyperprolactinemia among women presenting with galactorrhea in this study is therefore 37%. This is higher than 31.7%5 and 33.5%25 but lower than 80%21 and 90% reported from previous similar studies.26 Reported in an earlier study, the prevalence of hyperprolactinemia ranges from 0.4% in an unselected normal adult population to as high as 9–17% in women with reproductive disorders.27 Hyperprolactinemia has been considered the most common hormonal abnormality observed among infertile women.28 Conversely, studies have reported galactorrhea in 25%,29 40%,11 and 76.9%21 of hyperprolactinemic women. This was not determined in this study because serum prolactin test is not routine done for infertile women in our center due to cost and is only indicated where there are clinical features such as galactorrhea or menstrual disturbances. However, where cost permits it will be prudent to recommend serum prolactin assays for all infertile women.
This study has answered the question, the first research question, does galactorrhea always indicate raised prolactin levels? Obviously, from the study galactorrhea does not always indicate raised prolactin levels. The question of whether galactorrhea with normal serum prolactin requires treatment or not is a question for experimental research.
CONCLUSION
We conclude, therefore, that the prevalence of hyperprolactinemia in this study was low when compared with other studies and that galactorrhea does not always indicate raised serum prolactin levels.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cates W, Farley TM, Rowe PJ. Worldwide patterns of infertility: Is Africa different? Lancet. 1985;2:596–8. doi: 10.1016/s0140-6736(85)90594-x. [DOI] [PubMed] [Google Scholar]
- 2.Belsey MA. The epidemiology of infertility: A review with particular reference to sub-Saharan Africa. Bull World Health Organ. 1976;54:319–41. [PMC free article] [PubMed] [Google Scholar]
- 3.Idrisa A, Ojiji E. Pattern of infertility in North Eastern Nigeria. Trop J Obstet Gynaecol. 2000;17:27–9. [Google Scholar]
- 4.Otubu JA. Infertility. Trop J Obstet Gynaecol. 1995;12:68–71. [Google Scholar]
- 5.Idrisa A, Kawuwa MB, Habu SA, Adebayo AA. Prolactin levels among infertile women in Maiduguri, Nigeria. Trop J Obstet Gynaecol. 2003;20:97–100. [Google Scholar]
- 6.Kalsum A, Jalali S. Role of hyperprolactinemia in fertility. Pak J Med Res. 2002;41:94–100. [Google Scholar]
- 7.Whitman-Elia GF, Windham NQ. Galactorrhea may be clue to serious problems. Patients deserve a thorough workup. Postgrad Med. 2000;107:165–8, 171. doi: 10.3810/pgm.2000.06.1129. [DOI] [PubMed] [Google Scholar]
- 8.Peña KS, Rosenfeld JA. Evaluation and treatment of galactorrhea. Am Fam Physician. 2001;63:1763–70. [PubMed] [Google Scholar]
- 9.Kleinberg DL, Noel GL, Frantz AG. Galactorrhea: A study of 235 cases, including 48 with pituitary tumors. N Engl J Med. 1977;296:589–600. doi: 10.1056/NEJM197703172961103. [DOI] [PubMed] [Google Scholar]
- 10.Frantz AG, Wilson JD, editors. Williams Textbook of Endocrinology. 8th ed. Philadelphia: W.B. Saunders Company; 1992. Endocrine disorders of the breast; pp. 953–75. [Google Scholar]
- 11.Ogedemgbe OK. Anovulation and induction of ovulation. In: Kwawukume EY, Emuveyan EE, editors. Comprehensive Gynaecology in the Tropics. 1st ed. Dansoman: Asante & Hittscher Printing Press Limited; 2005. pp. 318–24. [Google Scholar]
- 12.Agarwal M, Das A, Singh SA. Hyperprolactinemia with normal serum prolactin: Its clinical significance. J Hum Reprod Sci. 2010;3:111–2. doi: 10.4103/0974-1208.69334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avner H, Mathew PC. Endocrine disorders. In: Jonathan BS, editor. Novak's Gynecology. 13th ed. Philadelphia: Lippincott Williams and Wilkins; 2002. p. 899. [Google Scholar]
- 14.Eastman RC. Acromegaly, hyperprolactinemia, gonadotrophin secreting tumours and hypopituitarism. In: Moore WT, Eastman RC, editors. Diagnostic Endocrinology. USA: The University of Michigan, Mosby; 1990. pp. 33–56. [Google Scholar]
- 15.Nahid E. Fertility rate with bromocriptine in infertile women with galactorrhoea and normal prolactin level. Int Congr Ser. 2004;1271:22–5. [Google Scholar]
- 16.Mah PM, Webster J. Hyperprolactinemia: Etiology, diagnosis, and management. Semin Reprod Med. 2002;20:365–74. doi: 10.1055/s-2002-36709. [DOI] [PubMed] [Google Scholar]
- 17.Serri O, Chik CL, Ur E, Ezzat S. Diagnosis and management of hyperprolactinemia. CMAJ. 2003;169:575–81. [PMC free article] [PubMed] [Google Scholar]
- 18.Bankowski BJ, Zacur HA. Dopamine agonist therapy for hyperprolactinemia. Clin Obstet Gynecol. 2003;46:349–62. doi: 10.1097/00003081-200306000-00013. [DOI] [PubMed] [Google Scholar]
- 19.Morrison C. The significance of nipple discharge: Diagnosis and treatment regimes. Lippincotts Prim Care Pract. 1998;2:129–40. [PubMed] [Google Scholar]
- 20.Diagnostic Automation/Cortez Diagnostics Inc. Enzyme immunoassay for the quantitative determination of prolactin concentration in human serum. USA: Diagnostic Automation/Cortez Diagnostics Inc; 2010. [CA] [Google Scholar]
- 21.Jeremiah I, Chris A, Oriji V. The impact of galactorrhoea on infertility in Port Harcourt. Niger Health J. 2009;9:8–11. [Google Scholar]
- 22.Gbadebo AA, Nkiruka A, Ijeoma OW, Austin O, Hajara U. Treatment outcome of hyperprolactinaemic infertility with carbegoline in sub Saharan Africa. Pak J Med Sci. 2008;24:512–6. [Google Scholar]
- 23.Eftekhari N, Mirzaei F, Karimi M. The prevalence of hyperprolactinemia and galactorrhea in patients with abnormal uterine bleeding. Gynecol Endocrinol. 2008;24:289–91. doi: 10.1080/09513590701672355. [DOI] [PubMed] [Google Scholar]
- 24.Binita G, Suprava P, Mainak C, Koner BC, Alpana S. Correlation of prolactin and thyroid hormone concentration with menstrual patterns in infertile women. J Reprod Infertil. 2009;10:207–12. [PMC free article] [PubMed] [Google Scholar]
- 25.Emokpae MA, Osadolor HB, Omole Ohonsi A. Sub-clinical hypothyroidism in infertile Nigerian women with hyperprolactinaemia. Niger J Physiol Sci. 2011;26:35–8. [PubMed] [Google Scholar]
- 26.Kumkum A, Jasmine K, Shweta G, Ajeshwar NP. Hyperprolactinema and its correlation with hypothyroidism in infertile women. J Obstet Gynecol India. 2006;56:68–71. [Google Scholar]
- 27.Biller BM, Luciano A, Crosignani PG, Molitch M, Olive D, Rebar R, et al. Guidelines for the diagnosis and treatment of hyperprolactinemia. J Reprod Med. 1999;44(12 Suppl):1075–84. [PubMed] [Google Scholar]
- 28.Emokpae MA, Uadia PO, Mohammed AZ. Hormonal evaluations and endometrial biopsy in infertile women in Kano, Northern Nigeria: A comparative study. Ann Afr Med. 2005;4:99–103. [Google Scholar]
- 29.Motazedian S, Babakhani L, Fereshtehnejad SM, Mojthahedi K. A comparison of bromocriptine and cabergoline on fertility outcome of hyperprolactinemic infertile women undergoing intrauterine insemination. Indian J Med Res. 2010;131:670–4. [PubMed] [Google Scholar]


