Abstract
Background:
Chronic kidney disease (CKD) has become a public health problem in Nigeria. Efforts are being geared toward early diagnosis and prevention of CKD. This study involved the evaluation of the referral pattern and mode of presentation of CKD patients at first contact in a tertiary health institution.
Patients and Methods:
Patients' records over an 18 month period were retrieved and the following information extracted: Sociodemographic data, referral hospital, mode of presentation, etiology of CKD, packed cell volume, blood pressure, and estimated glomerular filtration rate (GFR) at first presentation.
Results:
There were 202 CKD patients with a male: female ratio of 1.7:1 and a mean age of 48.15 ± 16.69 years. The median estimated GFR of the patients at presentation was 3.17 ml/min/1.73 m2. The common etiologies of CKD were chronic glomerulonephritis, hypertension, diabetes mellitus, obstructive nephropathy in 69 (34.2%), 47 (23.3%), 38 (18.8%), and 21 (10.4%) respectively. Among these patients, 111 (55%) and 98 (48.6%) had moderate to severe hypertension and anemia, respectively, 173 (85.6%) presented in CKD Stage 5, 101 (50%) required urgent hemodialysis whereas 123 (60.9%) required in-hospital admission. Only (18) 9% of these CKD patients presented by self-referral while (103) 51% were referred from secondary and private health facilities.
Conclusion:
Most Nigerian CKD patients still present very late to nephrologists implying that the present preventive strategies have not yielded desired results. Early diagnosis and referral of CKD patients could be better achieved through regular education of the public and retraining of health workers especially those in primary and secondary health institutions.
Keywords: Chronic kidney disease, late, pattern, presentation, referral
INTRODUCTION
Chronic kidney disease (CKD) has become a public health problem due to its increasing prevalence globally and associated high morbidity and mortality.1,2,3 The burden of CKD is more felt in developing countries like Nigeria where there is no health insurance to meet the huge financial demands the disease places on its sufferers and their families.4
Majority of CKD patients in Nigeria present late to nephrologists when they are already uremic and requiring renal replacement therapy (RRT).3 This may be due to both patient and primary physician-related factors. Early referral of CKD patients to nephrologists is key to retarding progression to end-stage renal disease, reducing hospitalization, cost of health care, and improving patients' survival before and eventually after commencement of RRT.5,6,7
Prevention and early detection of CKD are the main instruments for combating CKD in the world today. To this effect, programs have been initiated to actualize this goal. One of such is the World Kidney Day initiative established by the International Society of Nephrology and International Federation of Kidney Foundation marked yearly worldwide for the past 10 years with the primary objective of educating and enlightening the public on prevention and early detection of kidney disease as well as giving support to kidney disease sufferers. Nigerian nephrologists have been actively involved in the World Kidney Day initiative, and there has been an increase in public enlightenment campaigns on CKD.
The goal of this study was to assess the sociodemographic, clinical characteristics, and referral pattern of CKD patients at the time of first presentation to a tertiary hospital in southwest Nigeria. This will help determine if existing preventive nephrology programs and strategies are achieving desired results and also to identify areas requiring improvement.
PATIENTS AND METHODS
This study was a descriptive retrospective survey carried out in Kidney Care Centre, Ondo City, a tertiary health institution in Southwest Nigeria. CKD patients who presented to the center over an 18 month period from July 2014 to December 2015 were recruited for the study. Patients below the age of 18 years and those already on RRT were excluded. The case records of the patients were retrieved, and the following information extracted: Sociodemographic data, clinical characteristics at presentation and mode of referral to the nephrologist. Ethical approval was gotten from the hospital's ethical committee on research.
The Modification of Diet in Renal Disease (MDRD) equation was used to estimate glomerular filtration rate (GFR). CKD staging was done using estimated GFR as follows: Stage 1 (GFR of ≥90 ml/min with evidence of kidney damage), Stage 2 (GFR of 60–89 ml/min with evidence of kidney damage), Stage 3 (GFR of 59–30 ml/min with or without evidence of kidney damage), Stage 4 (GFR of 15–29 ml/min with or without evidence of kidney damage), and Stage 5 (GFR <15 ml/min with or without evidence of kidney damage).8
Hypertension was graded according to the JNC7 guidelines as mild hypertension: Blood pressure (BP) between 140–159/90–99 mmHg, moderate hypertension: BP between 160–179/99–109 mmHg and severe hypertension: BP ≥180/110 mmHg.9
Anemia was defined as hematocrit <36% in females and <39% in males.10
Anemia was graded as severe anemia (hematocrit <18%), moderate anemia (hematocrit of 18–25%), and mild anemia (hematocrit of 26–35% for females and 26–38% for males).
Data analysis
Data generated were analyzed using the Statistical Package for Social Sciences Inc®, Chicago released 2008, IBM Corp, New York). Results were presented in tabular form. Discrete variables were presented as frequency and percentages. Continuous variables were presented as mean and standard deviation for unskewed data and median, interquartile range for skewed data.
RESULTS
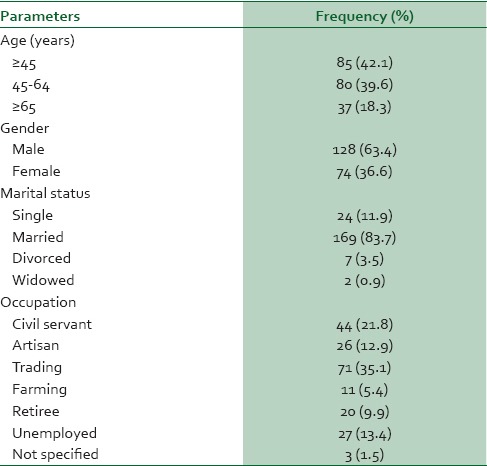
A total of 202 CKD patients seen during the period reviewed, met the inclusion criteria. The male: female ratio was 1.7:1. The majority of the CKD subjects were married and below 65 years of age; accounting for 169 (83.7%) and 165 (81.7%) of the CKD subjects respectively. About 75% of the CKD patients were gainfully employed [Table 1].
Table 1.
Sociodemographic characteristics of study population
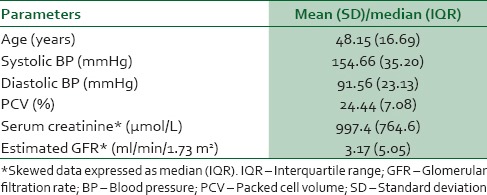
The mean age, systolic BP, diastolic BP, hematocrit of the study population were 48.15 ± 16.69 years, 154.66 ± 35.20 mmHg, 91.56 ± 23.13 mmHg and 24.44 ± 7.08%, respectively. The median serum creatinine and estimated GFR of the study population were 997 (764.6) μmol/L and 3.17 (5.05) ml/min/1.73 m2 respectively [Table 2].
Table 2.
Physical, hematological and biochemical parameters of chronic kidney disease patients
The common presenting complaints of the study patients were body swelling in 143 (70.8%), malaise in 100 (49.5%), nausea and vomiting in 104 (51.5%), and oliguria in 95 (47%) [Table 3]. Forty-three (21.3%) had mild hypertension, 46 (22.8%) had moderate hypertension, and 65 (32.2%) had severe hypertension at presentation [Figure 1]. Severe, moderate, and mild anemia were present in 30 (14.9%), 68 (33.7%), and 43 (21.3%) respectively at presentation. Seven (3.5%) were in CKD Stage 3, 22 (10.9%) in Stage 4 and 173 (85.6%) in Stage 5. At the time of presentation, 123 (60.9) required in-patient's care and 101 (50%) required urgent RRT. None of these patients had been vaccinated against hepatitis B [Table 3].
Table 3.
Clinical characteristics of study population
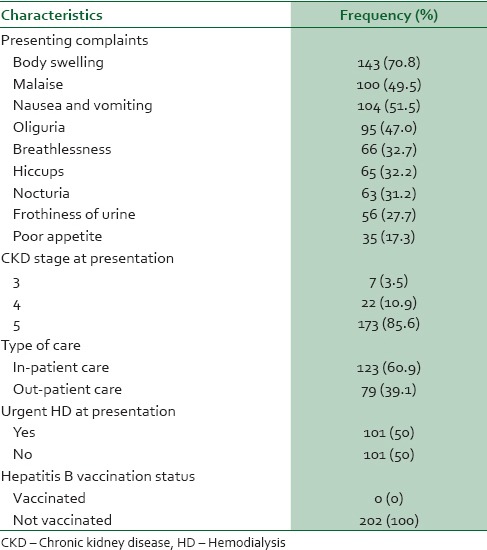
Figure 1.
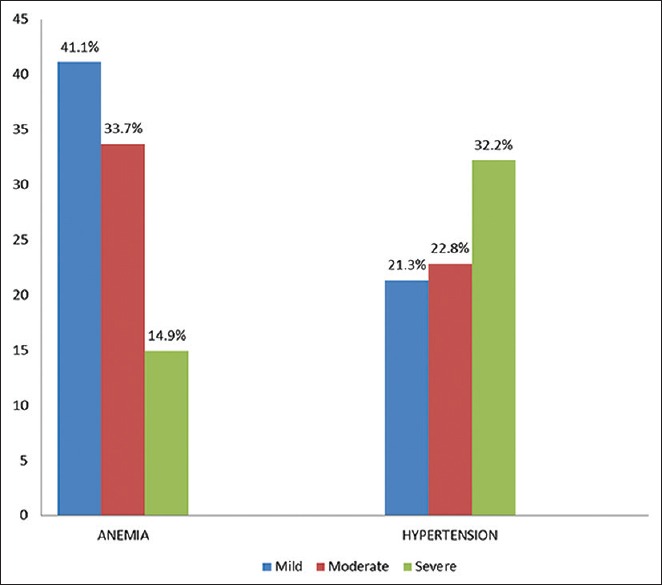
Degree of hypertension and anemia among chronic kidney disease Patients at first presentation
The common etiologies of CKD were chronic glomerulonephritis, hypertension, diabetes mellitus, obstructive nephropathy in 69 (34.2%), 47 (23.3%), 38 (18.8%), and 21 (10.4%) respectively [Figure 2].
Figure 2.
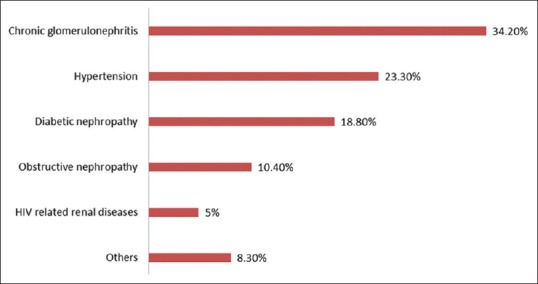
Etiology of chronic kidney disease
Only (18) 9% of these CKD patients presented by self-referral while (103) 51% were referred from secondary and private health facilities [Figure 3].
Figure 3.
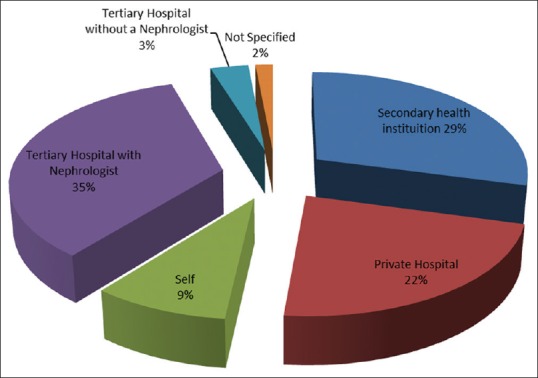
Referral pattern of CKD patients presenting at Kidney Care Centre
DISCUSSION
This study showed that most CKD patients still present very late, requiring in-patient care and emergency RRT despite present efforts geared towards prevention and early detection of CKD. There were more male CKD patients in this study which is similar to previous studies.3,11,12,13 This may be because CKD is more common in males and men tend to have more financial power to access health care services. More than 80% of these patients were young and middle aged which also agreed with previous reports from Nigeria and other parts of sub-Saharan Africa3,11,12 unlike in developed countries where the elderly are more commonly affected by CKD.1,14
Common etiologies of CKD in this study are chronic glomerulonephritis, hypertension, diabetes mellitus, and obstructive uropathy similar to the findings in previous studies.1,3,11,12,15 Therefore, persons with risk factors of the aforementioned conditions should be identified early and treated to therapeutic targets as recommended by standard guidelines, to reduce the incidence of CKD.
Most of the patients were in CKD Stage 5 at the time of first presentation similar to findings from previous reports.3,12 A major proportion of the patients already had uremic symptoms at the time of first presentation to the nephrologist and required emergency RRT. Several problems may crop up when CKD patients require emergency RRT. One of such is the lack of appropriate vascular access for hemodialysis.
About half of the CKD patients in this study were referred from private hospitals and secondary health facilities where there were no nephrologists. This reiterates the need for health workers at this level of care to be familiar with CKD management guidelines to reduce the burden of the disease through early risk identification, prevention, and early referral to the nephrologist. This could be achieved by incorporating such guidelines into the continuing medical education programs organized for health workers.
Although factors associated with late presentation were not assessed in this study, both physician and patient-related factors have been reported to be responsible in previous studies. Patient-related factors include poor health seeking behavior, erroneous belief that their health problems resulted from spiritual attack and lack of funds to seek proper health care while physician-related factors include perception preferences and knowledge deficits.16,17,18 An increase in public awareness and education on early features of kidney disease geared toward improving appropriate health-seeking attitude among Nigerians is necessary. This can be achieved by collaborating with religious institutions since some of these patients present initially to spiritual homes because of the erroneous belief that spiritual forces are the source of their ill-health.
A significant proportion of these patients presented with moderate to severe hypertension and anemia, both of which are cardiovascular risk factors that contribute to left ventricular hypertrophy and subsequent mortality in CKD patients.19,20,21 Anemia has been reported to be associated with increased expenditure and hospitalization rates in CKD patients.22,23 Those with severe anemia had to receive blood transfusions thereby increasing the cost of care.
None of the patients had received vaccination against hepatitis B, which is part of the predialysis care in CKD patients because of the increased risk of hepatitis B virus infection during hemodialysis and blood transfusion. It is recommended that hepatitis B vaccination be administered early in CKD for it to be effective.24
Furthermore, due to the late presentation of these patients, they do not have the opportunity to benefit from interventions such as early correction and treatment of anemia, hypertension, proteinuria, calcium, and phosphate abnormalities with appropriate and recommended therapeutic agents which have been reported to be cost-effective and also have indirect effects in reducing disability and improving productivity in early stages of CKD.25,26
Sixty-one percent of the patients in this study required in-patient's care at the time of first presentation due to the fact that they were quite ill. The time spent by these patients on admission has adverse effects on the overall nation's economic activities and their families because most of these patients were gainfully employed and constituted the economically productive age group in our nation. Furthermore, hospitalization of CKD patients has been associated with increased morbidity and mortality.27 This is avoidable if patients are seen earlier before reaching advanced stages of CKD.
All the patients in this study who required dialysis used temporary vascular access due to their poor clinical state at the time of presentation. This is more expensive compared to native arteriovenous fistula which offers higher blood flow rates and better dialysis efficiency. Initiating hemodialysis with temporary vascular access is also associated with infection, hospitalization, poor patient survival, increased cost and mortality in CKD patients compared to the use of arteriovenous fistula.28,29
The limitation of this study is that we depended on the accuracy of previous documentation in the patients' records. The strength of this study, however, lies in the fact that it showed a cogent need to re-strategize efforts toward prevention and early detection of CKD as the present strategies have not achieved the desired results.
The following recommendations are proposed:
Regular health education of Nigerians aimed toward improving their health seeking attitude and the adoption of lifestyles that supports healthy kidneys
Religious institutions should be involved in educating and encouraging their followers to improve their health seeking attitudes while yet seeking spiritual intervention and healing
There should be continuous medical education for health workers, especially those in primary and secondary health institutions aimed at early diagnosis, treatment, and referral of CKD patients to nephrologists
There is also need to adequately upgrade more health institutions to train more nephrologists in Nigeria.
CONCLUSION
This study concludes that CKD is more common in males and the economically productive age group in Nigeria, with majority of them presenting very late to nephrologists in uremic state and commencing RRT without adequate predialysis care. The present strategies toward prevention and early detection of CKD have not yet yielded the desired results. Furthermore, most of the causes of CKD in Nigeria are preventable if at-risk individuals are identified early and effectively managed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Alebiosu CO, Ayodele OE. The global burden of chronic kidney disease and the way forward. Ethn Dis. 2005;15:418–23. [PubMed] [Google Scholar]
- 2.Levey AS, Atkins R, Coresh J, Cohen EP, Collins AJ, Eckardt KU, et al. Chronic kidney disease as a global public health problem: Approaches and initiatives - A position statement from Kidney Disease Improving Global Outcomes. Kidney Int. 2007;72:247–59. doi: 10.1038/sj.ki.5002343. [DOI] [PubMed] [Google Scholar]
- 3.Ulasi II, Ijoma CK. The enormity of chronic kidney disease in Nigeria: The situation in a teaching hospital in South-East Nigeria. J Trop Med. 2010;2010:501957. doi: 10.1155/2010/501957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ijoma CK, Ulasi II, Kalu AO. Cost implications of treatment of end-stage renal disease in Nigeria. J Coll Med. 1998;3:95–6. [Google Scholar]
- 5.Smart NA, Titus TT. Outcomes of early versus late nephrology referral in chronic kidney disease: A systematic review. Am J Med. 2011;124:1073–80.e2. doi: 10.1016/j.amjmed.2011.04.026. [DOI] [PubMed] [Google Scholar]
- 6.Cass A, Cunningham J, Arnold PC, Snelling P, Wang Z, Hoy W. Delayed referral to a nephrologist: Outcomes among patients who survive at least one year on dialysis. Med J Aust. 2002;177:135–8. doi: 10.5694/j.1326-5377.2002.tb04698.x. [DOI] [PubMed] [Google Scholar]
- 7.Kinchen KS, Sadler J, Fink N, Brookmeyer R, Klag MJ, Levey AS, et al. The timing of specialist evaluation in chronic kidney disease and mortality. Ann Intern Med. 2002;137:479–86. doi: 10.7326/0003-4819-137-6-200209170-00007. [DOI] [PubMed] [Google Scholar]
- 8.Kidney Disease Improving Global Outcome (KDIGO) 2012. KDIGO 2012 clinical practice guideline of evaluation and management of CKD. Kidney Int Suppl. 2013;3:1–150. doi: 10.1038/ki.2013.243. [DOI] [PubMed] [Google Scholar]
- 9.Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure. The seventh report of the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure (JNC VII) Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization (WHO) A guide for programme manager. Geneva, Switzerland: WHO; 2001. Iron deficiency anaemia: Assessment, prevention and control. [Google Scholar]
- 11.Agbaji OO, Ebonyi AO, Gimba ZM, Abene EE, Ogiator MO, Agaba EI. Clinical and laboratory characteristics of adults with chronic kidney disease in Jos, Nigeria. Trop J Nephrol. 2014;10:23–9. [Google Scholar]
- 12.Amoako YA, Laryea DO, Bedu-Addo G, Andoh H, Awuku YA. Clinical and demographic characteristics of chronic kidney disease patients in a tertiary facility in Ghana. Pan Afr Med J. 2014;18:274. doi: 10.11604/pamj.2014.18.274.4192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agarwal R, Light RP. Determinants and prognostic significance of electrocardiographic left ventricular hypertrophy criteria in chronic kidney disease. Clin J Am Soc Nephrol. 2011;6:528–36. doi: 10.2215/CJN.07770910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Naicker S. End stage renal disease in sub-Saharan Africa. Kidney Int Suppl. 2013;3:161–3. doi: 10.1046/j.1523-1755.63.s83.25.x. [DOI] [PubMed] [Google Scholar]
- 15.Arogundade FA, Sanusi AA, Hassan MO, Akinsola A. The pattern, clinical characteristics and outcome of ESRD in Ile-Ife, Nigeria: Is there a change in trend? Afr Health Sci. 2011;11:594–601. [PMC free article] [PubMed] [Google Scholar]
- 16.Okwuonu CG, Chukwuonye II, Ogah SO, Abali C, Adejumo OA, Oviasu E. Awareness level of kidney functions and diseases among adults in a Nigerian population. Indian J Nephrol. 2015;25:158–63. doi: 10.4103/0971-4065.139096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chukwuezi CO, Anelechi AB. Factors associated with delay in seeking medical care among educated Nigerians. Asian J Med Sci. 2009;1:30–2. [Google Scholar]
- 18.Fischer MJ, Ahya SN, Gordon EJ. Interventions to reduce late referrals to nephrologists. Am J Nephrol. 2011;33:60–9. doi: 10.1159/000322704. [DOI] [PubMed] [Google Scholar]
- 19.Ulasi II, Arodiwe EB, Ijoma CK. Left ventricular hypertrophy in African black patients with chronic renal failure at first evaluation. Ethn Dis. 2006;16:859–64. [PubMed] [Google Scholar]
- 20.Jesurobo DE, Odia JO, Uchenna DI. Left ventricular hypertrophy and its correlates in CKD patients in a Nigerian tertiary hospital. Int J Med. 2012;1:11–6. [Google Scholar]
- 21.Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990;322:1561–6. doi: 10.1056/NEJM199005313222203. [DOI] [PubMed] [Google Scholar]
- 22.Li S, Collins AJ. Association of hematocrit value with cardiovascular morbidity and mortality in incident hemodialysis patients. Kidney Int. 2004;65:626–33. doi: 10.1111/j.1523-1755.2004.00425.x. [DOI] [PubMed] [Google Scholar]
- 23.Collins AJ, Li S, Ebben J, Ma JZ, Manning W. Hematocrit levels and associated medicare expenditures. Am J Kidney Dis. 2000;36:282–93. doi: 10.1053/ajkd.2000.8972. [DOI] [PubMed] [Google Scholar]
- 24.Grzegorzewska AE. Hepatitis B vaccination in chronic kidney disease: Review of evidence in non-dialyzed patients. Hepat Mon. 2012;12:e7359. doi: 10.5812/hepatmon.7359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trivedi H. Cost implications of caring for chronic kidney disease: Are interventions cost-effective? Adv Chronic Kidney Dis. 2010;17:265–70. doi: 10.1053/j.ackd.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 26.Menzin J, Lines LM, Weiner DE, Neumann PJ, Nichols C, Rodriguez L, et al. A review of the costs and cost effectiveness of interventions in chronic kidney disease: Implications for policy. Pharmacoeconomics. 2011;29:839–61. doi: 10.2165/11588390-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 27.Panocchia N, Tazza L, Di Stasio E, Liberatori M, Vulpio C, Giungi S, et al. Mortality in hospitalized chronic kidney disease patients starting unplanned urgent haemodialysis. Nephrology (Carlton) 2016;21:62–7. doi: 10.1111/nep.12561. [DOI] [PubMed] [Google Scholar]
- 28.Dhingra RK, Young EW, Hulbert-Shearon TE, Leavey SF, Port FK. Type of vascular access and mortality in U.S. hemodialysis patients. Kidney Int. 2001;60:1443–51. doi: 10.1046/j.1523-1755.2001.00947.x. [DOI] [PubMed] [Google Scholar]
- 29.Krzanowski M, Janda K, Chowaniec E, Sulowicz W. Hemodialysis vascular access infection and mortality in maintenance hemodialysis patients. Przegl Lek. 2011;68:1157–61. [PubMed] [Google Scholar]


