Abstract
Infraorbital dark circles represent a common and multifactorial challenge in the world of aesthetic medicine and are the result of a variety of factors including deep facial anatomy, soft tissue changes, as well as contributions from the skin. A variety of treatment options exist, and a customised management strategy can be developed for the particular anatomic changes present. A literature search using MEDLINE and non-MEDLINE sources was performed utilising keywords including: ‘Dark circles’ ‘infraorbital dark circles’, ‘infraorbital pigment’, ‘under-eye circles’ and ‘lower eyelid bags’. A comprehensive review of the literature was performed and the data were assimilated with evidence from our practice. This review provides a detailed discussion of the aetiology, pathogenesis, evaluation and management of infraorbital dark circles. An understanding of the deep and superficial anatomy is crucial to the management of this complex entity. The armamentarium for treatment includes minimally invasive interventions such as makeup and cosmeceuticals, a variety of laser and chemical treatments, fillers and fat transfer, as well as more invasive surgical manoeuvres.
KEYWORDS: Dark circles, infraorbital dark circles, infraorbital pigment, lower eyelid bags, under-eye circles
INTRODUCTION
Perceptions regarding the degree of a person's fatigue and age are preferentially based on periorbital aesthetics.[1] Throughout cultures, societal perceptions are similar, in that periorbital dark circles contribute to a tired, aged and even sad appearance. On an average, a woman in the United States spends $15,000 (USD) in her lifetime on cosmeceuticals and makeup, a large percentage of which is spent on under-eye concealers.[2] This expenditure phenomenon is worldwide, as the global beauty industry has been projected to be valued at $390.07 billion (USD) by 2020, and the skin care segment is anticipated to be the fastest growing subcategory.[3] This data do not include the resources that will be spent on surgical and other more invasive treatments to the periorbital region. The American Academy of Plastic Surgeons recently revealed data indicating that a total of $12.6 billion (USD) was spent on cosmetic procedures in the United States; an increase of 15% from the previous year. The group went on to report that in 2013, 15.1 million cosmetic procedures were performed in the United States, a 3% increase over the previous year. This includes 1.6 million surgical procedures and 13.4 million minimally invasive procedures. Eyelid surgery was the third most commonly performed surgical procedure with 216,000 procedures performed in 2013. Soft tissue filler injection was the second most common minimally invasive procedure performed with 2.2 million procedures performed, an increase of 13% over the previous year. A substantial percentage of these injections were used to treat the lower eyelid–cheek interface.[4] Facial ageing, and periorbital ageing in particular, is an area of great concern; reflected by a considerable societal investment in measures to conceal the facial stigmata of age and fatigue. As dark circles play a central role in the appearance of the ageing and fatigued lower eyelid, this review will describe the pathogenesis, evaluation and treatment of dark circles.
AETIOLOGY OF INFRAORBITAL DARK CIRCLES
A detailed understanding of facial anatomy is crucial to properly diagnose the aetiology of infraorbital dark circles. Various anatomic factors may contribute to the appearance of periocular dark circles including the facial ligamentous architecture, the bony structure, midface soft tissue including prominence of the orbicularis oculi muscle and vasculature and thin eyelid skin with minimal to no subcutaneous tissue[5] [Figure 1].
Figure 1.
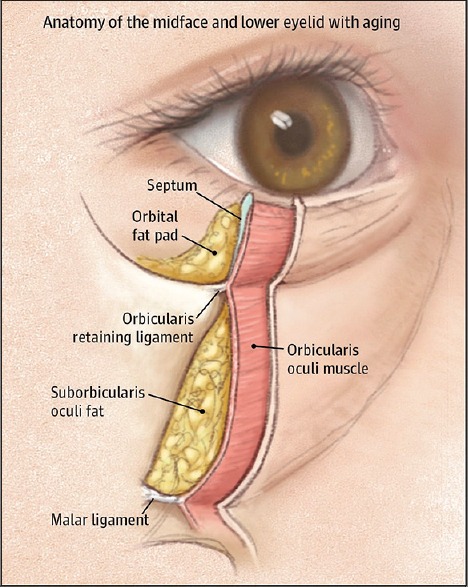
Age-related changes involving the osseous, ligamentous and soft tissue anatomy in the ageing eyelid resulting in infraorbital dark circles (adapted from Nakra, 2015)
UNDERLYING LIGAMENT AND BONE STRUCTURE
The underlying facial ligament and bone structure are important in providing a framework for supporting facial soft tissue and influence the overall appearance of the face. The osseo-cutaneous facial ligaments comprise the primary structural divisions of the facial fat compartments.[6] Age-related changes in the midface result in relative orbital rim recession and midfacial and malar bone volume loss, leading to tightening of the orbital and facial retaining ligaments.[7] As facial fat descends and fat volume decreases, the relatively inflexible ligaments result in tethering and associated orbital rim and facial hollowing. These hollows lead to worsening of shadowing, which can particularly be noted in the tear trough area in the inferomedial orbit.[8] Overhead lighting can worsen the appearance of periorbital dark circles, while direct light may mask the appearance[9] [Figures 1 and 2].
Figure 2.
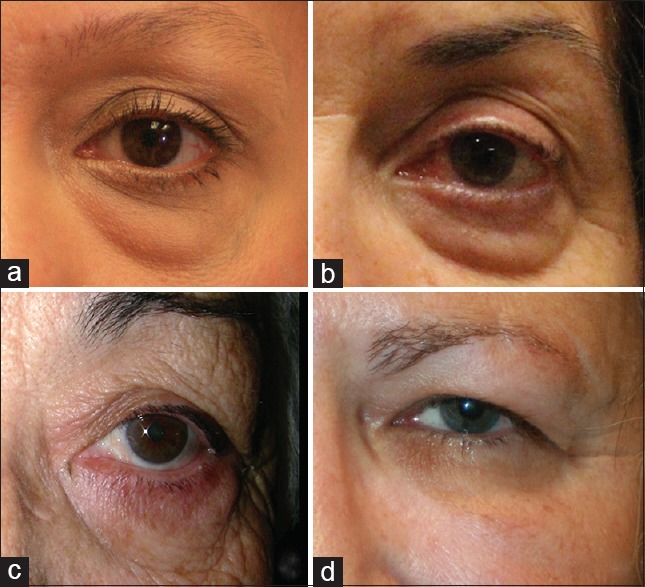
Patient with infraorbital dark circles due to shadowing and orbicularis prominence (a). Patient with infraorbital dark circles due to shadowing (b). Patient with infraorbital dark circles due to hyperaemia and hemosiderin deposition (c). Patient with infraorbital dark circles due to pigment deposition (d)
MIDFACE SOFT TISSUE CONTRIBUTIONS
The thin and somewhat transparent eyelid skin provides little camouflage to the prominence of the underlying midface soft tissue including the robust subcutaneous vascular network and the orbicularis oculi muscle. This results in a darkened appearance of the skin.[10,11] Infraorbital eyelid fluid may accumulate in the infraorbital soft tissue area and further contribute to the darkened and aged appearance in this area. Extravasation of haemoglobin breakdown products such as hemosiderin and biliverdin contributes to visible pigmentation changes in the cutaneous and subcutaneous layers. A variety of pathologic and age-related processes result in increased permeability of the local vasculature resulting in these pigmentary changes. The lower eyelid tissues may have an increased tendency to accumulate fluid due to local processes such as atopy as well as systemic fluid retention and can be limited inferiorly by the orbital rim because of the cutaneous ligaments. Eyelid oedema as a manifestation of fluid accumulation is often worse after a salty meal or in the morning. This fluid often takes on a purplish colour due to the prominent role of the orbicularis muscle in the lower eyelid[12] [Figure 2].
Age-related anatomic changes of the midface soft tissue include subcutaneous fat atrophy and volume loss, hypertrophy of orbicularis oculi muscle, pseudoherniation of suborbicularis oculi fibroadipose tissue and volume loss in the malar region. These features further accentuate the appearance of dark circles.
CONTRIBUTIONS FROM THE SKIN
The quality of the infraorbital skin may contribute to the appearance of infraorbital dark circles. The lower eyelid skin is one of the thinnest parts in the body and allows subdermal features to be accentuated. With minimal to no subcutaneous tissue, the skin has an intimate relationship with the orbicularis muscle. This results in ageing changes that are more exaggerated compared with the rest of the facial skin.[8] Skin ageing and environmental-related changes throughout the face include a loss of elasticity and turgor as a result of collagen and/or elastin loss. Furthermore, thinning of the skin, dyschromia, telangiectasia, seborrhoeic changes and actinic changes contribute to ageing of the skin[5,8] [Figures 1 and 2].
Multiple factors may be implicated in congenital and acquired hyperpigmentation of the periorbital skin. Causes may include melasma, nevi, dermal melanocytosis, excessive ultraviolet light exposure, hemosiderin deposition, hormonal changes or a multifactorial aetiology. Inflammation from various conditions including atopy and contact dermatitis may also lead to hyperpigmentation.[10,11] Medications such as oral contraceptives or ophthalmic prostaglandin F2a use have been found to increase pigmentation.[9,11]
Although skin may contain pigmentation, there may be fluctuation of the appearance based on subdermal characteristics. Watanabe et al. studied periorbital biopsies of 12 Japanese patients and found that although they all had dermal melanosis on histology, they had daily fluctuation in their appearance. The authors speculate that oedema and thickening of the dermis lead to an enhanced incidence of diffused light reflection from the pigmented areas, resulting in increased darkness of the skin.[13] The multifactorial aetiology may explain why patients complain of infraorbital dark circles experience and fluctuations of their appearance.
Infraorbital dark circles can be the result of a number of different aetiologies with contributions from deep skeletal elements, soft tissue and skin [Figures 1 and 2].
MANAGEMENT
The first step in managing infraorbital dark circles is to identify the specific constellation of aetiologic factors present so that a customised therapy can be crafted. A spectrum of interventions exist, including non-invasive options such as concealment and camouflage, to minimally invasive treatments such as soft tissue fillers and resurfacing, as well as more invasive treatments including surgical intervention.
CONCEALERS AND COSMECEUTICALS
Concealers and cosmeceuticals are the least invasive option for the treatment of dark circles. Mineral makeup foundation can be used to blend the hue of the skin to conceal undesirable darker pigment in the infraorbital region. In addition, by using opposite colour wheel techniques, opposite hues can be used to minimise colour irregularities. For example, to minimise an erythematous area, one adds green pigment to the base.[14,15]
Optical diffusers are a useful adjunct in the concealment of infraorbital dark circles. These compounds are composed of microionised mineral particles that are designed to reflect light away from the skin. These compounds utilise differing sized particles with large-sized molecules filing relative depressions in the skin and smaller particles resting on the areas of relative elevation. The refractive indexes of these molecules differ such that a combination of transmittance, spectral and diffuse reflection results in an optically smooth surface. Molecules commonly used as optical diffusers include boron nitride, mica, nylon, polymethylmethacrylate, polyurethane powder, sericite, silica, silicone powder, talc, Teflon, titanium dioxide and zinc oxide. Optical diffusers are an important adjunct in the camouflage of dark circles in the periorbital region.[16,17]
Retinoids are vitamin A derivatives that impact multiple pathways to decrease the appearance of dark circles in the infraorbital region. First, they promote collagen synthesis and promote reorganisation of collagen bundles to improve skin turgor and quality. They also decrease melanin content and reduce the size of melanocyte Golgi complex and endoplasmic reticulum. The sum of these effects results in increased skin smoothness and decreased discolouration and dyschromia.[18]
Hydroquinone is a competitive antagonist for tyrosinase, which plays a critical role in the pigmentation pathway. A range of concentrations of hydroquinone is available, typically through a compounding pharmacy. Using low concentrations such as 2–6% hydroquinone is typically sufficient to achieve melanocyte stabilisation as a means to decrease the pigment deposition in the periorbital region. Higher concentrations may result in paradoxical increase in pigment. Hydroquinone may not be available in some countries due to regulatory challenges. In Europe and in Asia, hydroquinone has become unavailable due to concerns regarding carcinogenesis and melanocyte toxicity.[19] Much of the concern regarding carcinogenesis emanates from a study that demonstrated that large amounts of oral hydroquinone caused cancer in rodents.[20] In areas where hydroquinone may not be available, several other compounds can be used, such as arbutin and kojic acid. Arbutin is a botanical extract with a structure very similar to hydroquinone and has demonstrated similar efficaciousness. Kojic acid also acts in blocking the tyrosinase pathway by binding to copper.[21]
Topical caffeine is an effective means of treating infraorbital dark circles. When applied topically, it can be an asset in treating dark circles that result from subcutaneous vascularisation, telangiectasias and oedema due to leaky vessels. A randomised, double-blinded, placebo-controlled study demonstrated the ability of a caffeine-based gel to penetrate the lower eyelid skin and diminish the lower eyelid oedema and pigmentation.[22]
Peptides are an increasingly common component of the armamentarium against dark circles. At present, there are more than 25 distinct peptide formulations used in compounds designed to improve skin quality. In general, these molecules act within the extracellular matrix (ECM) in the skin to promote the formation of collagen. Cosmeceutical peptides are classified into signal peptides, enzyme inhibitor peptides and carrier peptides.[23] Signal peptides such as palmitoyl pentapeptide-4 stimulate ECM that modulates fibroblast activity to increase in type I and III collagen and fibronectin production.[24,25] Signal peptides also increase elastin, proteoglycan, glycosaminoglycan and fibronectin proliferation – the building blocks of robust skin. Enzyme inhibitor peptides primarily block proteinase formation and activity, including matrix metalloproteinases, thereby aiding in maintaining a robust ECM in the skin. Carrier peptides' primary function is to deliver enzymatic cofactors such as copper and manganese that are critical in wound healing and regenerative properties of skin following solar damage. One of the most commonly used carrier peptides is glycyl-L-histidyl-L-lysine which stabilises and delivers copper for use in enzymatic processes. In these various ways, peptides improve the quality and turgor of the skin.[25]
NON-INVASIVE TREATMENTS
Intense pulsed light
Intense pulsed light (IPL) devices emit light in the visible spectrum and is applied to the skin via a coupling gel. A high-output lamp emits a broad wavelength of light in the 500–1200 nm range using electrical current passed through a xenon-filled chamber. The chromophore of this light is dermal and epidermal pigments in the form of haemoglobin and melanin; which results in selective photothermolysis of pigmented and/or hypervascular areas of skin. The result is improved homogenous tone and hue of the skin. Settings can be adjusted to treat particular targets of varying degrees of pigment; for example, preferential treatment of haemoglobin over melanin for the treatment of telangiectatic areas. Treatment parameters are individualised and IPL is ideal for patients with Fitzpatrick types I–III.[26]
Radiofrequency
Radiofrequency (RF) devices use energy produced by an electric current (as opposed to a light source as in a laser) to create a thermal effect that results in collagen contraction and neocollagenesis while minimising collateral damage. RF energy is not subjected to diminution by tissue absorption or scattering and can be used to treat deep tissue layers such as the dermis and subcutaneous fat without producing thermal burns. Moreover, RF devices can be used to treat a wide variety of skin types as they do not use light-based energy. The use of RF devices to achieve tightening of the skin in the periorbital region has been reported. These devices produce collagen tightening that many authors describe as mild to moderate and more subtle than the effects seen with ablative or fractionated lasers; however, the inherent low morbidity makes RF a desirable choice if mild effects are desired with a low risk profile.[27,28,29,30]
Q-switched lasers
Q-switched lasers are an effective means of treating dark circles that are primarily due to hyperpigmentary changes in the skin. Given the rapid thermal relaxation time of melanosomes, Q-switched lasers with nanosecond pulse technology are ideal for selectively treating melanosomes while causing minimal trauma to the surrounding structures. Q-switched ruby lasers use a 694 nm wavelength resulting in melanosome disruption within melanocytes, melanophages and keratinocytes. This relatively low wavelength is well suited for patients with Fitzpatrick types I and II skin, but the high rate of melanosome disruption is not ideal for patients with more pigmented skin. Two separate studies have demonstrated a >40% improvement in pigmented dark circles following treatment with ruby Q-switched lasers.[13,31] Adjuvant or neoadjuvant retinoids and hydroquinone can be used to improve the safety profile and to treat any hyperpigmentation issues.[32] Q-switch alexandrite lasers present a mid-spectrum 755 nm wavelength, resulting in less trauma to melanosomes and increased safety in higher Fitzpatrick skin types. Nd: Yag lasers penetrate deep into the skin and have minimal effect on melanosomes, given their high wavelength (1063 nm). This allows for increased safety when treating more pigmented individuals, such as Fitzpatrick type V and VI skin.[33,34,35]
Pulsed dye lasers
Pulsed dye lasers are well suited for the treatment of dark circles with a vascular aetiology. Pulsed dye lasers use the principle of selective thermolysis with haemoglobin as the chromophore. These lasers produce visible light at a wavelength of 585–595 nm with pulse durations of 0.45–40 ms. Pulse dye laser is ideal for patients with Fitzpatrick I–III skin types and is typically repeated at intervals of 4–6 weeks and often requires 3 or more sessions to be effective. Investigations in pulsed dye laser in the treatment of other forms of skin hyperpigmentation have been controversial; however, some studies indicate that pulsed dye laser may be useful in the treatment of solar lentigines.[36,37,38]
INVASIVE SUPERFICIAL TREATMENTS
Chemical peel
Chemical peeling is often combined with other interventions or used alone in the treatment of dark circles. This modality is effective in the treatment of dark circles due to both pigment irregularities in the skin as well as contributions from rhytids. Improved skin collagen following peeling can also aid in camouflaging the underlying orbicularis and vasculature than can contribute to dark circles. Trichloroacetic acid (TCA) peels are available in a variety of concentrations and can be used to achieve deeper treatments with increasing concentration. Peeling agents remove melanin from the stratum corneum and epidermis, with deeper peels modulating melanin content in the dermis. Resurfacing with TCA peels is an effective means of treating dark circles in patients in the Fitzpatrick I–III range. Chemical peels in more pigmented individuals must be performed cautiously as they are at a risk for pigmentary complications.[5,39] Vavouli et al. treated patients with Fitzpatrick II, III and IV with 3.75% TCA and 15% lactic acid and reported an improvement in the appearance of dark circles in more than 90% of the patients.[40]
Medical tattoos
Tattooing in the infraorbital region, also known as blepharopigmentation, was first described by Angres in 1984.[41] This technique makes use of a hollow round tip needle that injects pigment into the superficial dermis. The pigment initially is deposited as free granules in the epidermis and dermis, but eventually migrates into the orbicularis connective tissue. The pigment granules become endocytosed by fibroblasts and remain in place permanently. Blepharopigmentation is commonly performed to enhance the lower eyelid margin; however, tattooing has also been used to smooth transitions in hyperpigmentation in the lower eyelids. Several complications have been reported; however, blepharopigmentation is typically a well-tolerated procedure.[42,43,44,45]
Ablative laser resurfacing
Ablative resurfacing is a powerful means to improve infraorbital dark circles by resurfacing the skin to treat pigmentary irregularity as well as enhancing skin tightness and the collagen and ECM to improve concealment of the underlying orbicularis and vascular network. The mechanism of laser resurfacing is controlled tissue injury to the skin with the resultant reparative process resulting in the formation of skin layers with increased collagen, decreased pigment irregularities and a decrease in rhytids. Laser resurfacing is a powerful means of addressing dark circles in a multi-modal fashion. First, the superficial layers of the skin can be ablated resulting in the regeneration of superficial layers that are less pigmented. In addition, the improved collagen content in the resurfaced skin results in improved camouflage of the underlying orbicularis and associated vasculature that is often responsible for the appearance of dark circles. CO2 and erbium-doped yttrium aluminium garnet (Er: YAG) lasers are the most commonly used non-fractioned laser technologies. CO2 lasers use water as the chromophore and at fluences of 5 J/cm2 and pulse durations of <1 ms result in optical penetration of 20–30 µm with residual thermal damage extending to 100–150 µm. ER: Yag lasers also target water, however demonstrate more precision with a more limited depth of penetration and minimal thermal damage. Optic penetration is in the 1–3 µm/J/cm 2 with thermal damage extending 10–40 µ.[45,46]
Fractionated laser technology utilises the same technology as full ablative lasers; however, fractionated laser resurfacing reduces the confluent thermal damage of full ablative lasers to a subtotal pixelated pattern of ablation, leaving behind untreated skin which allows for less downtime and a lower complication rate. The results of fractionated CO2 laser resurfacing have been shown to be comparable to traditional ablative resurfacing; however, with a lower rate of complication and less downtime[47,48,49,50] [Figure 3].
Figure 3.

Before and after examples of patients with infraorbital dark circles who underwent treatment with: Volume enhancement with hyaluronic gel injection (a). Volume enhancement with autologous fat transfer (b). Laser skin resurfacing (c). Lower eyelid blepharoplasty with inferior orbit fat transposition (d) (adapted from Nakra, 2015)
Hyaluronic acid gel soft tissue fillers
Hyaluronic acid (HA) fillers have become a treatment of choice in many settings to address under-eye contour irregularities that can result in dark shading. Their ease of use, wide availability and potential for reversal with hyaluronidase make for an effective treatment modality to address volume deficiency in the periorbital region that may result in shadowing in the under-eye region. Goldberg describes three separate periorbital hollows that benefit from volumisation: The orbital rim hollow, the zygomatic hollow and the septal confluence hollow. These anatomic areas correspond to dense attachments between the skin and deeper tissue and bone created by the orbitomalar ligament, the orbitozygomatic ligament, and the confluence of the lower eyelid retractors, orbital septum and tarsal plate. Filling directly into the deep ligamentous structures and in a pre-periosteal plane can aid in volumetrically expanding these areas of dense attachments to soften contours in the infraorbital region.[51,52,53,54,55] Profound improvement in infraorbital dark shadows can be achieved using HA filler alone [Figure 3].
INVASIVE DEEP TREATMENTS
Fat transfer
Fat transfer is a powerful means to achieve facial rejuvenation and efface the infraorbital rim hollow. By injecting directly into the orbicularis retaining ligament, deep volume augmentation that minimises superficial irregularity can be produced, thereby effacing the facial hollows, yielding a smoother lower eyelid-midface contour. Using similar principles as described above for HA filler combined with the knowledge of the fat compartments of the face,[6] fat transfer can be a very effective means of softening the eyelid–cheek transition to minimise infraorbital dark circles. Fat transfer has been demonstrated to have a high rate of patient satisfaction[56,57,58] [Figure 3].
Surgery
Lower eyelid blepharoplasty can be used to address dark circles related to shadowing effects from overhead lighting. Adjuvant chemical peel or laser resurfacing can be used to treat pigmentary causes. A variety of lower eyelid blepharoplasty techniques are available. Transconjunctival fat excision blepharoplasty is an effective means of treating relative volume excess superior to the orbitomalar ligament that, when combined with age-related volume loss in the cheek, contributes to dark circles. When the dense attachments of the orbitomalar ligament prevent fat excision blepharoplasty from smoothing the eyelid–cheek contour, transposition lower eyelid blepharoplasty is an effective means of treating these contour irregularities. The orbicularis-retaining ligament is released directly and orbital fat is transposed into the infraorbital rim hollow.[8] Advancing the orbicularis and upper superficial musculoaponeurotic system (SMAS) is an effective means of further softening the lower eyelid–cheek contour. In patients with prominent festooning, SMAS elevation can aid in compressing festoons and elevating malar soft tissue to volumise the infraorbital rim hollow. These manoeuvres are particularly useful in situations where gravitational descent plays a prominent role in the aetiology of infraorbital dark circles[59] [Figure 3].
Surgical implants
Tear trough implants and cheek implants are effective means of augmenting age-related bone and soft tissue loss in the treatment of infraorbital dark circles. A variety of implant types are available, and treatment must be individualised; however, in general, these manoeuvres are best suited for patients with substantial relative bony under projection in the submalar and tear trough regions. Patients with ‘negative vector’ periorbital anatomy may benefit particularly from the volume and projection enhancement that submalar and tear trough implants provide.[60,61]
CONCLUSIONS
Infraorbital dark circles are caused by a variety of anatomic features, with contributions from the skin, subcutaneous tissues, orbicularis muscle, vasculature and ligamentous architecture of the lower eyelid and cheek. A detailed understanding of the regional anatomy is crucial to the management of dark circles, which encompasses a wide variety of modalities. The treatment strategy depends on the aetiology, and treatment must be individualised. Treatment modalities range from concealment and camouflage to non-invasive treatments such as lasers, as well as more invasive treatments such as volume augmentation and resurfacing, as well as deep invasive procedures such as blepharoplasty.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Nguyen HT, Isaacowitz DM, Rubin PA. Age- and fatigue-related markers of human faces: An eye-tracking study. Ophthalmology. 2009;116:355–60. doi: 10.1016/j.ophtha.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 2.Mint.com. Ross Crooks. Splurge vs Save: Which Beauty Products are Worth the Extra Cost? [Last cited on 2016 Jan 05]. Available from: https://www.blog.mint.com/consumer-iq/splurge-vs-save-which-beauty-products-are-worth-theextra-cost-0413/?display=wide .
- 3.Prnewswire.com. Cosmetics Market is Expected to Reach 39007 Billing Globally by 2020. [Last cited on 2016 Jan 05]. Available from: http://www.prnewswire.com/news-releases/cosmetics-market-is-expected-to-reach-39007-billion-globally-by-2020---allied-market-research-505160571.html .
- 4.Plastic Surgery Statistics. The American Board of Plastic Surgery. [Last cited on 2016 Jan 05]. Available from: http://www.plasticsurgery.org/Documents/news-resources/statistics/2013-statistics/plastic-surgery-statistics-full-report-2013.pdf .
- 5.Gendler EC. Treatment of periorbital hyperpigmentation. Aesthet Surg J. 2005;25:618–24. doi: 10.1016/j.asj.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 6.Rohrich RJ, Pessa JE. The fat compartments of the face: Anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119:2219–27. doi: 10.1097/01.prs.0000265403.66886.54. [DOI] [PubMed] [Google Scholar]
- 7.Pessa JE, Zadoo VP, Mutimer KL, Haffner C, Yuan C, DeWitt AI, et al. Relative maxillary retrusion as a natural consequence of aging: Combining skeletal and soft-tissue changes into an integrated model of midfacial aging. Plast Reconstr Surg. 1998;102:205–12. doi: 10.1097/00006534-199807000-00034. [DOI] [PubMed] [Google Scholar]
- 8.Nakra T. Biplanar contour-oriented approach to lower eyelid and midface rejuvenation. JAMA Facial Plast Surg. 2015;17:374–81. doi: 10.1001/jamafacial.2015.0860. [DOI] [PubMed] [Google Scholar]
- 9.Friedmann DP, Goldman MP. Dark circles: Etiology and management options. Clin Plast Surg. 2015;42:33–50. doi: 10.1016/j.cps.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 10.Roh MR, Chung KY. Infraorbital dark circles: Definition, causes, and treatment options. Dermatol Surg. 2009;35:1163–71. doi: 10.1111/j.1524-4725.2009.01213.x. [DOI] [PubMed] [Google Scholar]
- 11.Epstein JS. Management of infraorbital dark circles. A significant cosmetic concern. Arch Facial Plast Surg. 1999;1:303–7. doi: 10.1001/archfaci.1.4.303. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg RA, McCann JD, Fiaschetti D, Ben Simon GJ. What causes eyelid bags? Analysis of 114 consecutive patients. Plast Reconstr Surg. 2005;115:1395–402. doi: 10.1097/01.prs.0000157016.49072.61. [DOI] [PubMed] [Google Scholar]
- 13.Watanabe S, Nakai K, Ohnishi T. Condition known as “dark rings under the eyes” in the Japanese population is a kind of dermal melanocytosis which can be successfully treated by Q-switched ruby laser. Dermatol Surg. 2006;32:785–9. doi: 10.1111/j.1524-4725.2006.32161.x. [DOI] [PubMed] [Google Scholar]
- 14.Guerrero D. Dermocosmetic management of the red face and rosacea. Ann Dermatol Venereol. 2011;138(Suppl 3):S215–8. doi: 10.1016/S0151-9638(11)70093-X. [DOI] [PubMed] [Google Scholar]
- 15.Sidle DM, Decker JR. Use of makeup, hairstyles, glasses, and prosthetics as adjuncts to scar camouflage. Facial Plast Surg Clin North Am. 2011;19:481–9. doi: 10.1016/j.fsc.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 16.DeJohn A. Light Diffusing Technology To Mask Visible Signs Of Skin Aging. 2012. Jun 13, [Last cited on 2016 Jan 05]. Available from: http://www.cosmeticsdesign-asia.com/Formulation-Science/Light-diffusing-technology-to-mask-visible-signs-of-skin-aging .
- 17.Bierman A, Figueiro MG, Rea MS. Measuring and predicting eyelid spectral transmittance. J Biomed Opt. 2011;16:067011. doi: 10.1117/1.3593151. [DOI] [PubMed] [Google Scholar]
- 18.Darlenski R, Surber C, Fluhr JW. Topical retinoids in the management of photodamaged skin: From theory to evidence-based practical approach. Br J Dermatol. 2010;163:1157–65. doi: 10.1111/j.1365-2133.2010.09936.x. [DOI] [PubMed] [Google Scholar]
- 19.Draelos ZD. Skin lightening preparations and the hydroquinone controversy. Dermatol Ther. 2007;20:308–13. doi: 10.1111/j.1529-8019.2007.00144.x. [DOI] [PubMed] [Google Scholar]
- 20.Nordlund JJ, Grimes PE, Ortonne JP. The safety of hydroquinone. J Eur Acad Dermatol Venereol. 2006;20:781–7. doi: 10.1111/j.1468-3083.2006.01670.x. [DOI] [PubMed] [Google Scholar]
- 21.Garcia A, Fulton JE., Jr The combination of glycolic acid and hydroquinone or kojic acid for the treatment of melasma and related conditions. Dermatol Surg. 1996;22:443–7. doi: 10.1111/j.1524-4725.1996.tb00345.x. [DOI] [PubMed] [Google Scholar]
- 22.Amnuaikit T, Maneenuan D, Boonme P. Evaluation of caffeine gels on physicochemical characteristics and in vivo efficacy in reducing puffy eyes. J Appl Pharm Sci. 2011;1:56. [Google Scholar]
- 23.Mohammed YH, Yamada M, Lin LL, Grice JE, Roberts MS, Raphael AP, et al. Microneedle enhanced delivery of cosmeceutically relevant peptides in human skin. PLoS One. 2014;9:e101956. doi: 10.1371/journal.pone.0101956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang L, Falla TJ. Cosmeceuticals and peptides. Clin Dermatol. 2009;27:485–94. doi: 10.1016/j.clindermatol.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 25.Gorouhi F, Maibach HI. Role of topical peptides in preventing or treating aged skin. Int J Cosmet Sci. 2009;31:327–45. doi: 10.1111/j.1468-2494.2009.00490.x. [DOI] [PubMed] [Google Scholar]
- 26.Goldberg DJ. Current trends in intense pulsed light. J Clin Aesthet Dermatol. 2012;5:45–53. [PMC free article] [PubMed] [Google Scholar]
- 27.Ruiz-Esparza J. Noninvasive lower eyelid blepharoplasty: A new technique using nonablative radiofrequency on periorbital skin. Dermatol Surg. 2004;30(2 Pt 1):125–9. doi: 10.1111/j.1524-4725.2004.30052.x. [DOI] [PubMed] [Google Scholar]
- 28.Alster TS, Lupton JR. Nonablative cutaneous remodeling using radiofrequency devices. Clin Dermatol. 2007;25:487–91. doi: 10.1016/j.clindermatol.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 29.Biesman BS, Baker SS, Carruthers J, Silva HL, Holloman EL. Monopolar radiofrequency treatment of human eyelids: A prospective, multicenter, efficacy trial. Lasers Surg Med. 2006;38:890–8. doi: 10.1002/lsm.20452. [DOI] [PubMed] [Google Scholar]
- 30.Carruthers J, Carruthers A. Shrinking upper and lower eyelid skin with a novel radiofrequency tip. Dermatol Surg. 2007;33:802–9. doi: 10.1111/j.1524-4725.2007.33173.x. [DOI] [PubMed] [Google Scholar]
- 31.Lowe NJ, Wieder JM, Shorr N, Boxrud C, Saucer D, Chalet M. Infraorbital pigmented skin. Preliminary observations of laser therapy. Dermatol Surg. 1995;21:767–70. [PubMed] [Google Scholar]
- 32.Momosawa A, Kurita M, Ozaki M, Miyamoto S, Kobayashi Y, Ban I, et al. Combined therapy using Q-switched ruby laser and bleaching treatment with tretinoin and hydroquinone for periorbital skin hyperpigmentation in Asians. Plast Reconstr Surg. 2008;121:282–8. doi: 10.1097/01.prs.0000293869.00522.ec. [DOI] [PubMed] [Google Scholar]
- 33.Jang KA, Chung EC, Choi JH, Sung KJ, Moon KC, Koh JK. Successful removal of freckles in Asian skin with a Q-switched alexandrite laser. Dermatol Surg. 2000;26:231–4. doi: 10.1046/j.1524-4725.2000.09243.x. [DOI] [PubMed] [Google Scholar]
- 34.Wang CC, Chen CK. Effect of spot size and fluence on Q-switched alexandrite laser treatment for pigmentation in Asians: A randomized, double-blinded, split-face comparative trial. J Dermatolog Treat. 2012;23:333–8. doi: 10.3109/09546634.2011.560929. [DOI] [PubMed] [Google Scholar]
- 35.Saedi N, Metelitsa A, Petrell K, Arndt KA, Dover JS. Treatment of tattoos with a picosecond alexandrite laser: A prospective trial. Arch Dermatol. 2012;148:1360–3. doi: 10.1001/archdermatol.2012.2894. [DOI] [PubMed] [Google Scholar]
- 36.Liu A, Moy RL, Ross EV, Hamzavi I, Ozog DM. Pulsed dye laser and pulsed dye laser-mediated photodynamic therapy in the treatment of dermatologic disorders. Dermatol Surg. 2012;38:351–66. doi: 10.1111/j.1524-4725.2011.02293.x. [DOI] [PubMed] [Google Scholar]
- 37.Arora P, Sarkar R, Garg VK, Arya L. Lasers for treatment of melasma and post-inflammatory hyperpigmentation. J Cutan Aesthet Surg. 2012;5:93–103. doi: 10.4103/0974-2077.99436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ghaninejhadi H, Ehsani A, Edrisi L, Gholamali F, Akbari Z, Noormohammadpour P. Solar lentigines: Evaluating pulsed dye laser (PDL) as an effective treatment option. J Lasers Med Sci. 2013;4:33–8. [PMC free article] [PubMed] [Google Scholar]
- 39.Roberts WE. Periorbital hyperpigmentation: Review of etiology, medical evaluation, and aesthetic treatment. J Drugs Dermatol. 2014;13:472–82. [PubMed] [Google Scholar]
- 40.Vavouli C, Katsambas A, Gregoriou S, Teodor A, Salavastru C, Alexandru A, et al. Chemical peeling with trichloroacetic acid and lactic acid for infraorbital dark circles. J Cosmet Dermatol. 2013;12:204–9. doi: 10.1111/jocd.12044. [DOI] [PubMed] [Google Scholar]
- 41.Angres GG. Angres permalid-liner method: A new surgical procedure. Ann Ophthalmol. 1984;16:145–8. [PubMed] [Google Scholar]
- 42.Hurwitz JJ, Brownstein S, Mishkin SK. Histopathological findings in blepharopigmentation (eyelid tattoo) Can J Ophthalmol. 1988;23:267–9. [PubMed] [Google Scholar]
- 43.De M, Marshak H, Uzcategui N, Chang E. Full-thickness eyelid penetration during cosmetic blepharopigmentation causing eye injury. J Cosmet Dermatol. 2008;7:35–8. doi: 10.1111/j.1473-2165.2008.00340.x. [DOI] [PubMed] [Google Scholar]
- 44.Moshirfar M, Espandar L, Kurz C, Mamalis N. Inadvertent pigmentation of the limbus during cosmetic blepharopigmentation. Cornea. 2009;28:712–3. doi: 10.1097/ICO.0b013e318190737b. [DOI] [PubMed] [Google Scholar]
- 45.Goldberg RA, Shorr N. Complications of blepharopigmentation. Ophthalmic Surg. 1989;20:420–3. [PubMed] [Google Scholar]
- 46.Ortiz AE, Goldman MP, Fitzpatrick RE. Ablative CO2 lasers for skin tightening: Traditional versus fractional. Dermatol Surg. 2014;40(Suppl 12):S147–51. doi: 10.1097/DSS.0000000000000230. [DOI] [PubMed] [Google Scholar]
- 47.Nestor MS. Prophylaxis for and treatment of uncomplicated skin and skin structure infections in laser and cosmetic surgery. J Drugs Dermatol. 2005;4(6 Suppl):s20–5. [PubMed] [Google Scholar]
- 48.Tierney EP, Hanke CW, Watkins L. Treatment of lower eyelid rhytids and laxity with ablative fractionated carbon-dioxide laser resurfacing: Case series and review of the literature. J Am Acad Dermatol. 2011;64:730–40. doi: 10.1016/j.jaad.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 49.Kotlus BS, Schwarcz RM, Nakra T. Upper eyelid fractional CO2 laser resurfacing with incisional blepharoplasty. Ophthal Plast Reconstr Surg. 2015 doi: 10.1097/IOP.0000000000000495. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 50.Brightman LA, Brauer JA, Anolik R, Weiss E, Karen J, Chapas A, et al. Ablative and fractional ablative lasers. Dermatol Clin. 2009;27:479–89. doi: 10.1016/j.det.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 51.Carruthers J, Rzany B, Sattler G, Carruthers A. Anatomic guidelines for augmentation of the cheek and infraorbital hollow. Dermatol Surg. 2012;38(7 Pt 2):1223–33. doi: 10.1111/j.1524-4725.2012.02478.x. [DOI] [PubMed] [Google Scholar]
- 52.Hirmand H. Anatomy and nonsurgical correction of the tear trough deformity. Plast Reconstr Surg. 2010;125:699–708. doi: 10.1097/PRS.0b013e3181c82f90. [DOI] [PubMed] [Google Scholar]
- 53.Kane MA. Treatment of tear trough deformity and lower lid bowing with injectable hyaluronic acid. Aesthetic Plast Surg. 2005;29:363–7. doi: 10.1007/s00266-005-0071-7. [DOI] [PubMed] [Google Scholar]
- 54.Griepentrog GJ, Lemke BN, Burkat CN, Rose JG, Jr, Lucarelli MJ. Anatomical position of hyaluronic acid gel following injection to the infraorbital hollows. Ophthal Plast Reconstr Surg. 2013;29:35–9. doi: 10.1097/IOP.0b013e318272d4b0. [DOI] [PubMed] [Google Scholar]
- 55.Goldberg RA. The three periorbital hollows: A paradigm for periorbital rejuvenation. Plast Reconstr Surg. 2005;116:1796–804. doi: 10.1097/01.prs.0000185623.36795.38. [DOI] [PubMed] [Google Scholar]
- 56.Ciuci PM, Obagi S. Rejuvenation of the periorbital complex with autologous fat transfer: Current therapy. J Oral Maxillofac Surg. 2008;66:1686–93. doi: 10.1016/j.joms.2006.06.274. [DOI] [PubMed] [Google Scholar]
- 57.Trepsat F. Periorbital rejuvenation combining fat grafting and blepharoplasties. Aesthetic Plast Surg. 2003;27:243–53. doi: 10.1007/s00266-003-2126-y. [DOI] [PubMed] [Google Scholar]
- 58.Tomar S, Obagi S. Autologous fat augmentation: Results of a patient satisfaction survey. Cosmet Dermatol. 2004;17:343. [Google Scholar]
- 59.Yin VT, Chou E, Nakra T. The transeyelid midface lift. Clin Plast Surg. 2015;42:95–101. doi: 10.1016/j.cps.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 60.Hirmand H, Codner MA, McCord CD, Hester TR, Jr, Nahai F. Prominent eye: Operative management in lower lid and midfacial rejuvenation and the morphologic classification system. Plast Reconstr Surg. 2002;110:620–8. doi: 10.1097/00006534-200208000-00040. [DOI] [PubMed] [Google Scholar]
- 61.Goldberg RA, Soroudi AE, McCann JD. Treatment of prominent eyes with orbital rim onlay implants: Four-year experience. Ophthal Plast Reconstr Surg. 2003;19:38–45. doi: 10.1097/00002341-200301000-00005. [DOI] [PubMed] [Google Scholar]


