Abstract
Conventional acne treatment presents several challenges such as intolerable side effects and antibiotic resistance. Dermocosmetic products may be used to reduce these unwanted effects. Dermocosmetics include skin cleansers, topical sebum-controllers, skin antimicrobial/anti-inflammatory agents, moisturizers, sunscreens, and camouflage products. Appropriate use of these products may help augment the benefit of acne treatment, minimize side effects, and reduce the need for topical antibiotics. In Asia, there is currently limited scientific data on the application and recommendations for dermocosmetic use in acne vulgaris (AV). This article reviews the evidence on dermocosmetics for AV and provides practice recommendations as discussed during the 4th Asia-Pacific Acne Leaders' Summit held in Bangkok, Thailand, on 7 and 8 February 2015. Through a premeeting survey, a series of plenary lectures, a stepwise program of discussion sessions, and Medline article review, the Expert Panel set forth relevant recommendations on the role of dermocosmetics as adjunct for treating AV in Asian patients.
KEYWORDS: Acne, adjuvant, Asian, cosmeceuticals, dermocosmetics
INTRODUCTION
In this region, there are limited educational materials highlighting the role of dermocosmetics in the management of acne vulgaris (AV). This review summarizes the perspectives of dermatologists from different centers around Asia-Pacific that regularly treat and provide advice on dermocosmetics as adjuvant therapy in AV with a particular focus on the uniqueness of Asian skin.
Twenty-one Asian dermatologists (from Hong Kong, India, Indonesia, Malaysia, Philippines, Singapore, Taiwan, Thailand, and Vietnam) and one from Italy met in February 2015 in Bangkok, Thailand to discuss and provide their insights on current practices in AV therapy, specifically recommendations on dermocosmetic options.
Through a premeeting opinion poll with questions based on clinician experience on dermocosmetics for AV, a series of plenary lectures, and a stepwise program of discussion sessions, the expert panel set forth relevant recommendations on dermocosmetics as an adjunct for treating AV in Asian patients. Subsequently, a search on the Medline database using the keywords “acne, cosmetics, cosmeceuticals, cleanser, moisturizer, sunblock, sunscreen, sebum-controller, sebostatic, sebosuppressive, corneolytics, chemical peels, glycolic acid, salicylic acid, camouflage, maquillage, Asians, Chinese, Japanese, Koreans, Thais, Malays, Indians, ethnic skin, and dark skin” was done. All in vivo or prospective clinical trials conducted on Asians within the last 10 years were included. Finally, only studies published or translated into English were reviewed.
THE IMPACT OF ACNE
Acne therapy and its limitations
AV is a chronic inflammatory disease of the pilosebaceous unit. It is a distressing condition among adolescents and young adults because it can lead not only to physical complications, such as permanent scarring but also to long-lasting psychosocial effects.[1]
The conventional model of AV pathogenesis begins with follicular hyperkeratinization, followed by sebum accumulation leading to comedone formation. Inflammation was believed to be secondary following these steps.[2] However, subclinical inflammation has been found to occur even without preceding microcomedone formation, and it takes place early during the emergence of visible lesions, through progression, and even during resolution when the scars are forming.[2] Thus, AV pathogenesis is currently believed to be caused not only by Propionibacterium acnes proliferation, but also by inflammatory mechanisms due to factors such as genetic predisposition, diet, sebaceous gland activity, inflammatory mediators, and their target receptors.[2]
P. acnes resistance has been found to be progressing at an alarming rate due to continued irrational antibiotic use.[3] Changing patterns of antibiotic susceptibility have led to significant alterations in prescribing patterns as well as the widespread recognition of the need for alternative nonantibiotic treatment for AV.[4]
Throughout the decades, AV therapy has remained largely the same: Comedolytics, antimicrobials, anti-inflammatory substances, and isotretinoin. The current advances in the understanding of normal skin physiology and the pathophysiologic mechanisms leading to acne have allowed for the development of other therapies that have a wide spectrum of treatment targets.[5]
Dermocosmetics
Cosmetics were initially intended to enhance esthetic appearance. Nonmedicinal raw materials are incorporated into these products to have functional effects on the skin. These are then used as supplementary agents in the treatment of dermatologic conditions such as AV. These cosmetics are referred to as “cosmeceuticals.”[6] However, worldwide, there is variable recognition of this term by regulatory agencies. This is because of the fundamental differences in policies for market approval of cosmetics, which only improve physical appearance versus topical medicinal agents, which have true physiologic effects on the skin.[6,7] “Dermocosmetics,” a term synonymously used as “cosmeceuticals,” has been coined to describe cosmeceuticals which are used as adjuvant in the management of a variety of skin disorders.[8] These dermocosmetics, are believed to either target various etiopathogenic factors, for example, antibacterial, anti-inflammatory, reductant of sebum, dryness, irritation, and photosensitivity or enhance the penetration of prescribed topical medications.[7] For the purpose of consistency, the term “dermocosmetics” is used in this article.
There has been a growing consumer demand for personal care products in Asia-Pacific in light of increasing affluence and the growing influence of mass media in this region.[9] These products include dermocosmetics that are used for people with a variety of skin conditions including AV. Most of these agents are made up of components that target inflammation, wound healing, photoaging, hyperpigmentation, or uneven skin texture by mechanisms acting on fibroblasts, keratinocytes, or melanocytes. It is common to find botanical ingredients or vitamins in these agents.[10]
The Asian skin
It is generally believed that the Asian skin is more prone to irritation to certain topical agents compared to other skin types, most notably, Caucasian skin.[11] This is generally thought to be a factor of the skin's ability to provide a barrier (i.e., thicker stratum corneum and higher eccrine gland sensitivity correlates with decreased somatosensory perception) against toxic, sensitizing, or irritating substances. Asian skin was reported to have an elevated neurosensory response to insults when compared to the skin of Caucasians, which were also observed to be more reactive than the skin of African-Americans.[12,13] In particular, the East Asian skin has been found to have the least skin barrier strength, the lowest degree of maturation, and consequently, the highest degree of skin sensitivity as compared to whites or blacks.[14]
Because of its relatively increased level of melanin pigmentation, Asian skin has also been observed to be more prone to develop postinflammatory hyperpigmentation when inflamed or injured.[13,15]
In addition, Asians are a diverse group of individuals inclusive of various skin phototypes ranging from Fitzpatrick Type III to V in the East Asians to Type IV and V in South Asians. It is possible that different subsets of Asian subjects may react differently to topical agents.[16] For example, in a Singaporean study done by Goh et al., Chinese patients were observed to be more readily irritated by retinoids than patients with Malay or Indian ethnicity.[17]
Dermatologists should therefore take these differences into consideration when providing advice on dermocosmetics.
Meeting the challenges of acne treatment
For many decades, oral and topical antibiotics have been a primary treatment in AV with the initial goal of targeting P. acnes.[18] Systemic antibiotics used for acne include tetracyclines (e.g., tetracycline, oxytetracycline, doxycycline, lymecycline, and minocycline), macrolides (e.g., erythromycin, azithromycin, clarithromycin, roxithromycin), and co-trimoxazole. Topical antibiotics include clindamycin, erythromycin, and nadifloxacin.[19]
Prolonged use of antibiotics is known to promote antibiotic resistance. Since the late 1970s, there has been a documented increase in resistant P. acnes strains in western countries,[20,21,22,23,24,25] with Asian countries gradually following suit.[26,27,28,29,30] Among the antibiotics, erythromycin has the highest rates of P. acnes resistance, followed by clindamycin.[31,32]
Acne is generally not considered as a classical bacterial infection where resistance to an antibiotic is directly correlated to treatment failure. Nevertheless, P. acnes resistance can result in a poor therapeutic response in a significant proportion of patients.[33]
Antibiotics continue to be prescribed for AV as it is effective and because of the clear association between P. acnes growth and acne pathogenesis. Antibiotics also have an anti-inflammatory effect that is independent of bacterial killing.[34] Regardless, it is recommended that antibiotics should never be used alone either as topical or systemic agents.[35] Their combination with retinoids or benzoyl peroxide can prevent antibiotic resistance. Fixed-dose combinations have been shown to be a good option for treatment of AV, whereas nonantibiotic pharmacological agents, such as retinoids, benzoyl peroxide, and azelaic acid, are useful options.[35]
Inflammation, irritation, and patient compliance
Topical treatment of AV may be associated with side effects including skin dryness, erythema, scaling, stinging or burning, and itching. These are symptoms and signs of skin irritation. Skin irritation and inflammation can lead to reduced patient compliance. One global study reported poor adherence to therapy in 50% of patients with acne, with 48% having poor adherence in the Asian cohort.[36] The risk factors found to be linked to poor adherence include experience with side effects, inadequate knowledge about AV, nonuse of moisturizing cream, and cleansers, and those with poor clinical improvement.[37]
The evidence for dermocosmetic use in Asian acne patients
Skin care is integral in reducing and preventing AV lesions and maintaining healthy skin. A study on the treatment-seeking behaviors in Korean patients showed that majority of patients sought treatment advice on skin care from the internet, television/radio, magazines, and newspapers. It was found that in general, patients with AV favored traditional medicine, visiting beauty clinics, increasing water intake, and using nonprescription topical therapies over seeking treatment by a dermatologist. However, 77% of these patients were found to be dissatisfied with treatment and had to eventually seek specialist care.[38]
Since there are a lot of dermocosmetic options available for selection, treating physicians should be well-equipped with in-depth knowledge on dermocosmetics to advise patients on products suitable for their skin. A dermatologist-directed skin care regimen instils an impression on the patient that there is a strong professional interest in the management of AV. This helps lessen confusion in patients when choosing their regimen, and will prevent them from using nonprescription products with unsubstantiated claims.[39]
In general, preliminary in vitro results may be not confirmed in vivo and substances active in vitro are still in need of supportive clinical trials. Most dermocosmetics have been evaluated in vivo studies with a limited number of patients and follow no strict protocol criteria. Only a few studies are supported by histological evaluation, and because dermocosmetics usually contain multiple different active compounds, the efficacy of these agents should be tested as single ingredients as well as combination treatment.[8]
The following is a review of current evidence on cleansers, moisturizers, topical sebum-controlling agents with anti-inflammatory properties, corneolytics, photoprotecting agents, camouflage, and nonantibiotic antimicrobial products that are commonly found in Asian countries. Some formulations claim to have more than one mode of action on the skin (e.g., some may exert concomitant anti-inflammatory, antimicrobial, and photoprotective effects), and it is also not uncommon to find combination products with more than one agent.[8] This review is limited to agents that have been evaluated at least in vivo or clinically on Asian populations. The need for research on dermocosmetic agents (i.e., botanicals, traditional medicines, personalized combinations, and quasi-drugs) exists as this is a new and fast-growing science. More information will undoubtedly be available in the future.
Facial cleansers
Cleansers are used to remove makeup, oil, dirt, dead skin cells, and bacteria and are useful for acne patients. A cleanser may be used as part of a skin care regimen together with other dermocosmetics. The types of cleansers used for acne include lipid-free cleansers, synthetic detergents (syndets), astringents, exfoliants, or mild abrasives and may be in the form of cleansing bars or liquid.[40]
All patients with AV should be educated on the use of cleansers because these agents have been found to promote compliance to treatment.[41] Facial washing with cleansers has also been found to reduce both inflammatory and noninflammatory lesions when done twice daily.[42,43]
The regimen and the choice of the cleanser should be suited to the patient's skin profile. For example, scrubs or other mechanical treatments can help facilitate exfoliation of the skin in many patients; however, these should not be suggested in patients who are known to have sensitive skin. Furthermore, some products may contain allergens, such as fragrances and preservatives, and should not be used by susceptible patients (i.e., history of allergic contact dermatitis).[44]
Controlled studies done in Japan on cleansers utilized combinations of sodium laureth carboxylate and alkyl carboxylates showing efficacy for mild to moderate grade facial acne.[45] A study in Korea showed that triclosan, salicylic acid, and azelaic acid-based cleanser reduced both inflammatory and noninflammatory acne lesion.[43]
In accordance with the South-East Asia Study Alliance guidelines on the management of AV, ideal cleansers are those that are noncomedogenic, nonacnegenic, hypoallergenic, and nonirritating to the skin. The recommendation is to provide mild cleansers with slightly acidic or neutral pH, are alcohol-free, nonabrasive, can be easily rinsed/are residue free, optionally contain benzoyl peroxide or salicylic acid, and to be used twice daily.[41]
Moisturizers for acne
Dermocosmetic moisturizers can overcome the side effects of dryness and stinging caused by induction or maintenance therapy. Moisturizers specifically made for AV therapy were found to improve the tolerability by decreasing the dryness and stinging sensation associated with barrier disruption, thus improving compliance to treatment.[46,47,48,49]
A review done by Chularojanamontri et al. analyzed key components of 52 moisturizers that claim to be suitable for skin with AV.[50] Dimethicone and glycerin were found to be the most commonly utilized agents as they can reduce transepidermal water loss. Hyaluronic acid and sodium pyrrolidone carboxylic acid are used in addition to counterbalance the stickiness of glycerin. Some botanical components have putative anti-inflammatory effects, for example, witch hazel and aloe vera while some metals, for example, zinc are added for their anti-inflammatory or wound healing effects.[50]
The ideal acne moisturizers should be noncomedogenic, nonacnegenic, hypoallergenic, nonirritating, and is compatible with the patient's treatment regimens.[41,51] Moisturizers are often incorporated in cleansers and photoprotecting agents.[52]
The general recommendation is to use water-based and nongreasy moisturizers once daily (i.e., in the morning for photoprotecting moisturizers)[53] or as often as deemed necessary by the treating physician. To reduce the drying and stinging effects of topical acne treatment, the panel recommends that moisturizers be applied initially before other topical agents.
Topical sebum-control agents with anti- inflammatory properties
Mattifying agents found in topical sebum-control products have been shown to absorb and retain sebum, correcting the oily, or shiny appearance of the skin as well as decrease the risk of formation of comedones and inflammatory acne lesions.[54,55] Results of a few in vivo and clinical studies have shown the sebum-reducing activity of retinoids, specifically adapalene, as well as low-dose clindamycin, nicotinamide, benzoyl peroxide, azelaic acid, zinc compounds, and L-carnitine.[54,55,56,57,58] A study in Japanese subjects showed that 2% nicotinamide can reduce the sebum excretion rate of facial skin.[55]
In addition, certain sebum-controlling agents have been shown to possess complementary antipruritic, antimicrobial, vasoactive, photoprotective, skin-lightening, antioxidant, and anti-inflammatory activities. Nicotinamide is one of the most useful and evaluated of these agents.[59,60,61] Used as monotherapy, nicotinamide 4% has been shown to decrease the severity of mild to moderate AV as measured by the global acne grading system in a series of double-blind, multicentric, randomized vehicle-controlled trials.[62] It has comparable efficacy to clindamycin in the treatment of AV[63,64,65,66] and is available alone or in combination with other agents.
The effectiveness of sebum-controlling agents in the control and treatment of AV in Asian patients remains to be determined.
Corneolytics or comedolytics
Topical corneolytics, such as retinaldehyde, retinol, alpha-hydroxy acids (e.g., glycolic acid), beta-hydroxy acids (e.g., salicylic acid), and polyhydroxy acids (e.g., lactobionic acid and gluconolactone) found in low concentrations in a wide variety of over the counter formulations, have comedolytic and skin-lightening effects. These can help facilitate skin absorption of topical medications enhancing patient satisfaction.[8,67] Both alpha-hydroxy and beta-hydroxy are key agents found in comedolytic and/or exfoliant dermocosmetics and may have the potential to cause a pH-dependent irritation of the skin. Salicylic acid formulated at pH 6.50 induced relatively no stinging compare to a formulation at pH 3.12.[68]
The general approach is to use these agents in patients with darker skin to simultaneously treat active lesions and to correct postinflammatory changes.[69,70] In addition, acne scars have been found to improve using these agents.[71] Although multiple studies done on Asian patients have shown beneficial effects and safety of interventional peeling on both inflammatory and noninflammatory lesions, the lack of evidence on the effects of dermocosmetics with corneolytics properties in different Asian skin types remains to be a challenge.
Photoprotecting and bleaching agents
Sunscreens are strongly recommended in acne patients at high risk of postinflammatory hyperpigmentation (Fitzpatrick skin Type IV or higher, or significant occupational, or recreational sun exposure), and in patients who already have signs of postinflammatory hyperpigmentation. There are two known types of sunscreens depending on one of two mechanisms: Ultraviolet (UV) blocking and UV absorbing. UV-blocking agents typically contain titanium dioxide and zinc dioxide, which provide physical filtering against UV light and tend to be chalky in consistency. UV-absorbing agents (e.g., avobenzone), on the other hand, are chemical agents commonly found in an aqueous base. Because of this, patients of ethnic origin with oily skin and acne prefer UV-absorbing sunscreens because of their cosmetic acceptability.[72,73,74] For at-risk patients, the recommendation is to use a broad-spectrum photoprotecting agent with UVB and UVA filter (sun protection factor 30–50 and protective clothing when exposed to the sun).[69]
Since dyspigmentation is a common outcome of AV in Asians, prevention and treatment of this condition is of great research interest.[16] Application of dermocosmetics with a skin bleaching component (e.g., azelaic acid, hydroquinone) in combination with a photoprotecting agent (e.g., dioxybenzone, oxybenzone) may improve patient compliance in skin phototype above IV.[75,76] Salicylic acid has been found to be an effective and safe therapy for the treatment of AV in Asians and has been seen to improve postinflammatory hyperpigmentation in dark-skinned patients.[77,78,79]
Camouflage
Cosmetic camouflage or corrective maquillage aims to disguise disfiguring skin lesions by improving the appearance of the skin. They can be used to contour and correct pigment abnormalities, control oil, moisturize, protect against UV light, increase absorption of acne treatment, improve the skin barrier, and improve personal well-being.[80,81] These products that come as cover creams, powders, or liquids can quickly conceal visible scars or active lesions.[82]
An ideal acne camouflage should have a natural appearance, be nongreasy, noncomedogenic, and can be easily applied. The product of choice depends largely on patient preference and market availability of the agent, available shades as well as the presence of specific ingredients.[70] For instance, some products may contain botanical agents with natural beta-hydroxy acids (e.g., willow bark) or essential oils (e.g., Matricaria recutita) with supposedly anti-inflammatory and antimicrobial properties, or vitamins (e.g., Vitamin E), which may act as antioxidants.[82]
In Asian markets, use of makeup to conceal postinflammatory color changes is common in adult females.[83]
In general, the panel recommends that cosmetic camouflage agents should be avoided in patients with active AV as the occlusive effects of some of their ingredients (e.g., talc) may aggravate acne. However, in exceptional situations, it may be used as an adjunct to overcome psychosocial effects of AV lesions and scars as well as to improve dermatology-specific quality of life.[82,84]
Another recommendation is to use camouflage agents that are complementary to the color of the lesion (e.g., green concealer used on red acne lesions, yellow concealer for purple scars) before using a product of the same skin tone.[80]
Nonantibiotic antimicrobial products
Some nonantibiotic agents commonly found in dermocosmetics are reported to exhibit antimicrobial properties. Antibacterial adhesive (ABA) agents have demonstrated anti-proliferative, anti-adhesive, and antibiofilm properties. This can lower the P. acnes bacterial load while avoiding antibacterial resistance.[85]
Alkylglycoside, a nonionic surfactant for cleanser preparations, or sucrose stearate, for oil-free cream preparations, inhibit bacterial proliferation in vitro. Alkylglycoside displays a dose-dependent inhibitory effect, with a minimal inhibitory concentration (MIC) of 40 μg/mL. Sucrose stearate also has a 40 μg/mL MIC. In contrast, the MIC of nicotinamide is higher (20 mg/mL). ABA as a mixture also has an inhibitory effect on P. acnes adhesion ranging from 50% to 97% as measured by decreases in average intensities of immunofluorescence.[85] Alkylglycoside alone or sucrose stearate alone prevents adhesion and induces detachment of P. acnes on corneocytes. The addition of nicotinamide to either or both compounds enhances these anti-adhesive effects.
CONCLUSIONS
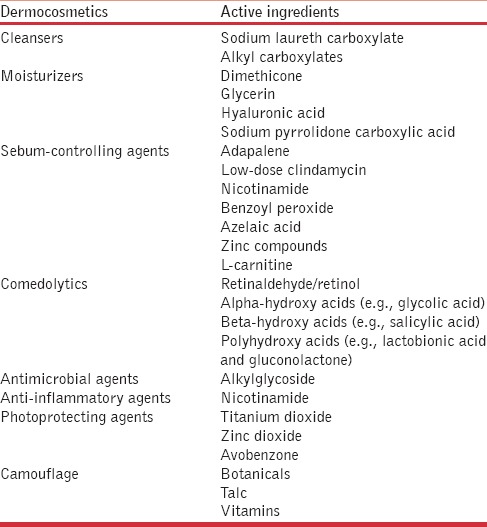
Despite recent advances in therapy, AV remains a significant skin condition encountered in the clinic. The major challenges of treatment of AV include increasing the incidence of P. acnes resistance to antibiotics and poor patient compliance due to the side effects of topical and systemic treatment. Adjunctive therapies have been introduced to mitigate these side effects. Dermocosmetics are useful adjuncts to standard pharmacotherapy and help to reduce the incidence of side effects such as dryness, irritation, and photosensitivity. Dermocosmetics may come in the form of cleansers, sebum-controlling agents, antimicrobial/anti-inflammatory agents, topical comedolytics, moisturizers specific for acne, photoprotecting agents, and camouflage products/skin-lightening agents [Table 1]. To optimize dermocosmetic therapy, it is necessary to educate patients so that they use the most appropriate products, chosen in consideration of ongoing pharmacological therapy.
Table 1.
Examples of dermocosmetic agents for acne and their main active ingredients available in Asia
Financial support and sponsorship
This review was made possible by an unrestricted educational grant from A. Menarini Asia Pacific, Pte Ltd.
Conflicts of interest
The authors of the article have received honoraria from A. Menarini Asia Pacific, Pte Ltd., for their participation in the meeting.
Acknowledgement
The authors would like to acknowledge Dr. Dennis Malvin H. Malgapo of MIMS Pte Ltd., Medical Education Division for editorial support.
REFERENCES
- 1.Gieler U, Gieler T, Kupfer JP. Acne and quality of life – Impact and management. J Eur Acad Dermatol Venereol. 2015;29(Suppl 4):12–4. doi: 10.1111/jdv.13191. [DOI] [PubMed] [Google Scholar]
- 2.Del Rosso JQ, Kircik LH. The sequence of inflammation, relevant biomarkers, and the pathogenesis of acne vulgaris: What does recent research show and what does it mean to the clinician? J Drugs Dermatol. 2013;12(8 Suppl):s109–15. [PubMed] [Google Scholar]
- 3.Kircik LH. Re-evaluating treatment targets in acne vulgaris: Adapting to a new understanding of pathophysiology. J Drugs Dermatol. 2014;13:s57–60. [PubMed] [Google Scholar]
- 4.Del Rosso JQ, Leyden JJ, Thiboutot D, Webster GF. Antibiotic use in acne vulgaris and rosacea: Clinical considerations and resistance issues of significance to dermatologists. Cutis. 2008;82(2 Suppl 2):5–12. [PubMed] [Google Scholar]
- 5.Millikan LE. Cosmetology, cosmetics, cosmeceuticals: Definitions and regulations. Clin Dermatol. 2001;19:371–4. doi: 10.1016/s0738-081x(01)00195-x. [DOI] [PubMed] [Google Scholar]
- 6.Draelos ZD. Cosmeceuticals: Undefined, unclassified, and unregulated. Clin Dermatol. 2009;27:431–4. doi: 10.1016/j.clindermatol.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 7.Dreno B, Bensadoun RJ, Humbert P, Krutmann J, Luger T, Triller R, et al. Algorithm for dermocosmetic use in the management of cutaneous side-effects associated with targeted therapy in oncology. J Eur Acad Dermatol Venereol. 2013;27:1071–80. doi: 10.1111/jdv.12082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dall'oglio F, Tedeschi A, Fabbrocini G, Veraldi S, Picardo M, Micali G. Cosmetics for acne: Indications and recommendations for an evidence-based approach. G Ital Dermatol Venereol. 2015;150:1–11. [PubMed] [Google Scholar]
- 9.Cosmetics & Toiletries Market Overviews 2014 [Database on the Internet] 2014. [Last accessed on 2015 Dec 29]. Available from: http://www.export.gov/hongkong/build/groups/public/@eg_hk/documents/webcontent/eg_hk_089943.pdf .
- 10.Kumari S, Khurana SP. Cosmeceuticals: Current trends and market preparations. IOSR J Pharm Biol Sci. 2013;8:45–8. [Google Scholar]
- 11.Aramaki J, Kawana S, Effendy I, Happle R, Löffler H. Differences of skin irritation between Japanese and European women. Br J Dermatol. 2002;146:1052–6. doi: 10.1046/j.1365-2133.2002.04509.x. [DOI] [PubMed] [Google Scholar]
- 12.Rawlings AV. Ethnic skin types: Are there differences in skin structure and function? Int J Cosmet Sci. 2006;28:79–93. doi: 10.1111/j.1467-2494.2006.00302.x. [DOI] [PubMed] [Google Scholar]
- 13.Yu SS, Grekin RC. Aesthetic analysis of Asian skin. Facial Plast Surg Clin North Am. 2007;15:361–5, vii. doi: 10.1016/j.fsc.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Muizzuddin N, Hellemans L, Van Overloop L, Corstjens H, Declercq L, Maes D. Structural and functional differences in barrier properties of African American, Caucasian and East Asian skin. J Dermatol Sci. 2010;59:123–8. doi: 10.1016/j.jdermsci.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 15.Chan HH, Alam M, Kono T, Dover JS. Clinical application of lasers in Asians. Dermatol Surg. 2002;28:556–63. doi: 10.1046/j.1524-4725.2002.01307.x. [DOI] [PubMed] [Google Scholar]
- 16.Ho SG, Chan HH. The Asian dermatologic patient: Review of common pigmentary disorders and cutaneous diseases. Am J Clin Dermatol. 2009;10:153–68. doi: 10.2165/00128071-200910030-00002. [DOI] [PubMed] [Google Scholar]
- 17.Goh CL, Tang MB, Briantais P, Kaoukhov A, Soto P. Adapalene gel 0.1% is better tolerated than tretinoin gel 0.025% among healthy volunteers of various ethnic origins. J Dermatolog Treat. 2009;20:282–8. doi: 10.1080/09546630902763164. [DOI] [PubMed] [Google Scholar]
- 18.Tzellos T, Zampeli V, Makrantonaki E, Zouboulis CC. Treating acne with antibiotic-resistant bacterial colonization. Expert Opin Pharmacother. 2011;12:1233–47. doi: 10.1517/14656566.2011.553192. [DOI] [PubMed] [Google Scholar]
- 19.Dréno B, Bettoli V, Ochsendorf F, Layton A, Mobacken H, Degreef H, et al. European recommendations on the use of oral antibiotics for acne. Eur J Dermatol. 2004;14:391–9. [PubMed] [Google Scholar]
- 20.Ross JI, Snelling AM, Carnegie E, Coates P, Cunliffe WJ, Bettoli V, et al. Antibiotic-resistant acne: Lessons from Europe. Br J Dermatol. 2003;148:467–78. doi: 10.1046/j.1365-2133.2003.05067.x. [DOI] [PubMed] [Google Scholar]
- 21.Rosen T. Antibiotic resistance: An editorial review with recommendations. J Drugs Dermatol. 2011;10:724–33. [PubMed] [Google Scholar]
- 22.Leyden JJ, Del Rosso JQ. Oral antibiotic therapy for acne vulgaris: Pharmacokinetic and pharmacodynamic perspectives. J Clin Aesthet Dermatol. 2011;4:40–7. [PMC free article] [PubMed] [Google Scholar]
- 23.Mendoza N, Hernandez PO, Tyring SK, Haitz KA, Motta A. Antimicrobial susceptibility of Propionibacterium acnes isolates from acne patients in Colombia. Int J Dermatol. 2013;52:688–92. doi: 10.1111/j.1365-4632.2011.05403.x. [DOI] [PubMed] [Google Scholar]
- 24.Schafer F, Fich F, Lam M, Gárate C, Wozniak A, Garcia P. Antimicrobial susceptibility and genetic characteristics of Propionibacterium acnes isolated from patients with acne. Int J Dermatol. 2013;52:418–25. doi: 10.1111/j.1365-4632.2011.05371.x. [DOI] [PubMed] [Google Scholar]
- 25.Eady EA. Bacterial resistance in acne. Dermatology. 1998;196:59–66. doi: 10.1159/000017869. [DOI] [PubMed] [Google Scholar]
- 26.Moon SH, Roh HS, Kim YH, Kim JE, Ko JY, Ro YS. Antibiotic resistance of microbial strains isolated from Korean acne patients. J Dermatol. 2012;39:833–7. doi: 10.1111/j.1346-8138.2012.01626.x. [DOI] [PubMed] [Google Scholar]
- 27.Nakase K, Nakaminami H, Noguchi N, Nishijima S, Sasatsu M. First report of high levels of clindamycin-resistant Propionibacterium acnes carrying erm(X) in Japanese patients with acne vulgaris. J Dermatol. 2012;39:794–6. doi: 10.1111/j.1346-8138.2011.01423.x. [DOI] [PubMed] [Google Scholar]
- 28.Abdel Fattah NS, Darwish YW. In vitro antibiotic susceptibility patterns of Propionibacterium acnes isolated from acne patients: An Egyptian university hospital-based study. J Eur Acad Dermatol Venereol. 2013;27:1546–51. doi: 10.1111/jdv.12057. [DOI] [PubMed] [Google Scholar]
- 29.Tan HH, Goh CL, Yeo MG, Tan ML. Antibiotic sensitivity of Propionibacterium acnes isolates from patients with acne vulgaris in a tertiary dermatological referral centre in Singapore. Ann Acad Med Singapore. 2001;30:22–5. [PubMed] [Google Scholar]
- 30.Luk NM, Hui M, Lee HC, Fu LH, Liu ZH, Lam LY, et al. Antibiotic-resistant Propionibacterium acnes among acne patients in a regional skin centre in Hong Kong. J Eur Acad Dermatol Venereol. 2013;27:31–6. doi: 10.1111/j.1468-3083.2011.04351.x. [DOI] [PubMed] [Google Scholar]
- 31.Mills O, Jr, Thornsberry C, Cardin CW, Smiles KA, Leyden JJ. Bacterial resistance and therapeutic outcome following three months of topical acne therapy with 2% erythromycin gel versus its vehicle. Acta Derm Venereol. 2002;82:260–5. doi: 10.1080/000155502320323216. [DOI] [PubMed] [Google Scholar]
- 32.Ozolins M, Eady EA, Avery AJ, Cunliffe WJ, Po AL, O'Neill C, et al. Comparison of five antimicrobial regimens for treatment of mild to moderate inflammatory facial acne vulgaris in the community: Randomised controlled trial. Lancet. 2004;364:2188–95. doi: 10.1016/S0140-6736(04)17591-0. [DOI] [PubMed] [Google Scholar]
- 33.Tan HH. Antibacterial therapy for acne: A guide to selection and use of systemic agents. Am J Clin Dermatol. 2003;4:307–14. doi: 10.2165/00128071-200304050-00002. [DOI] [PubMed] [Google Scholar]
- 34.Thiboutot D, Dreno B, Gollnick H, Bettoli V, Kang S, Leyden JJ, et al. A call to limit antibiotic use in acne. J Drugs Dermatol. 2013;12:1331–2. [PubMed] [Google Scholar]
- 35.Thiboutot D, Gollnick H, Bettoli V, Dréno B, Kang S, Leyden JJ, et al. New insights into the management of acne: An update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol. 2009;60(5 Suppl):S1–50. doi: 10.1016/j.jaad.2009.01.019. [DOI] [PubMed] [Google Scholar]
- 36.Dréno B, Thiboutot D, Gollnick H, Finlay AY, Layton A, Leyden JJ, et al. Large-scale worldwide observational study of adherence with acne therapy. Int J Dermatol. 2010;49:448–56. doi: 10.1111/j.1365-4632.2010.04416.x. [DOI] [PubMed] [Google Scholar]
- 37.Pawin H, Beylot C, Chivot M, Faure M, Poli F, Revuz J, et al. Creation of a tool to assess adherence to treatments for acne. Dermatology. 2009;218:26–32. doi: 10.1159/000165628. [DOI] [PubMed] [Google Scholar]
- 38.Suh DH, Shin JW, Min SU, Lee DH, Yoon MY, Kim NI, et al. Treatment-seeking behaviors and related epidemiological features in Korean acne patients. J Korean Med Sci. 2008;23:969–74. doi: 10.3346/jkms.2008.23.6.969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Del Rosso JQ. The role of skin care as an integral component in the management of acne vulgaris: Part 1: The importance of cleanser and moisturizer ingredients, design, and product selection. J Clin Aesthet Dermatol. 2013;6:19–27. [PMC free article] [PubMed] [Google Scholar]
- 40.Mukhopadhyay P. Cleansers and their role in various dermatological disorders. Indian J Dermatol. 2011;56:2–6. doi: 10.4103/0019-5154.77542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goh CL, Abad-Casintahan F, Aw DC, Baba R, Chan LC, Hung NT, et al. South-East Asia study alliance guidelines on the management of acne vulgaris in South-East Asian patients. J Dermatol. 2015;42:945–53. doi: 10.1111/1346-8138.12993. [DOI] [PubMed] [Google Scholar]
- 42.Choi JM, Lew VK, Kimball AB. A single-blinded, randomized, controlled clinical trial evaluating the effect of face washing on acne vulgaris. Pediatr Dermatol. 2006;23:421–7. doi: 10.1111/j.1525-1470.2006.00276.x. [DOI] [PubMed] [Google Scholar]
- 43.Choi YS, Suh HS, Yoon MY, Min SU, Kim JS, Jung JY, et al. A study of the efficacy of cleansers for acne vulgaris. J Dermatolog Treat. 2010;21:201–5. doi: 10.3109/09546630903401454. [DOI] [PubMed] [Google Scholar]
- 44.Decker A, Graber EM. Over-the-counter Acne Treatments: A Review. J Clin Aesthet Dermatol. 2012;5:32–40. [PMC free article] [PubMed] [Google Scholar]
- 45.Isoda K, Takagi Y, Endo K, Miyaki M, Matsuo K, Umeda K, et al. Effects of washing of the face with a mild facial cleanser formulated with sodium laureth carboxylate and alkyl carboxylates on acne in Japanese adult males. Skin Res Technol. 2015;21:247–53. doi: 10.1111/srt.12183. [DOI] [PubMed] [Google Scholar]
- 46.Draelos ZD, Ertel KD, Berge CA. Facilitating facial retinization through barrier improvement. Cutis. 2006;78:275–81. [PubMed] [Google Scholar]
- 47.Munehiro A, Murakami Y, Shirahige Y, Nakai K, Moriue T, Matsunaka H, et al. Combination effects of cosmetic moisturisers in the topical treatment of acne vulgaris. J Dermatolog Treat. 2012;23:172–6. doi: 10.3109/09546634.2010.551109. [DOI] [PubMed] [Google Scholar]
- 48.Hayashi N, Kawashima M. Study of the usefulness of moisturizers on adherence of acne patients treated with adapalene. J Dermatol. 2014;41:592–7. doi: 10.1111/1346-8138.12520. [DOI] [PubMed] [Google Scholar]
- 49.Matsunaga K, Leow YH, Chan R, Kerrouche N, Paliargues F. Adjunctive usage of a non-comedogenic moisturizer with adapalene gel 0.1% improves local tolerance: A randomized, investigator-blinded, split-face study in healthy Asian subjects. J Dermatolog Treat. 2013;24:278–82. doi: 10.3109/09546634.2012.661037. [DOI] [PubMed] [Google Scholar]
- 50.Chularojanamontri L, Tuchinda P, Kulthanan K, Pongparit K. Moisturizers for acne: What are their constituents? J Clin Aesthet Dermatol. 2014;7:36–44. [PMC free article] [PubMed] [Google Scholar]
- 51.Bikowski J. The use of therapeutic moisturizers in various dermatologic disorders. Cutis. 2001;68(5 Suppl):3–11. [PubMed] [Google Scholar]
- 52.Draelos ZD. The art and science of new advances in cosmeceuticals. Clin Plast Surg. 2011;38:397–407, vi. doi: 10.1016/j.cps.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 53.Del Rosso JQ, Gold M, Rueda MJ, Brandt S, Winkelman WJ. Efficacy, safety, and subject satisfaction of a specified skin care regimen to cleanse, medicate, moisturize, and protect the skin of patients under treatment for acne vulgaris. J Clin Aesthet Dermatol. 2015;8:22–30. [PMC free article] [PubMed] [Google Scholar]
- 54.Stinco G, Bragadin G, Trotter D, Pillon B, Patrone P. Relationship between sebostatic activity, tolerability and efficacy of three topical drugs to treat mild to moderate acne. J Eur Acad Dermatol Venereol. 2007;21:320–5. doi: 10.1111/j.1468-3083.2006.01914.x. [DOI] [PubMed] [Google Scholar]
- 55.Draelos ZD, Matsubara A, Smiles K. The effect of 2% niacinamide on facial sebum production. J Cosmet Laser Ther. 2006;8:96–101. doi: 10.1080/14764170600717704. [DOI] [PubMed] [Google Scholar]
- 56.Stinco G, Piccirillo F, Valent F, Errichetti E, di Meo N, Trevisan G, et al. Efficacy, tolerability, impact on quality of life and sebostatic activity of three topical preparations for the treatment of mild to moderate facial acne vulgaris. G Ital Dermatol Venereol. 2014 [Epub ahead of print] [PubMed] [Google Scholar]
- 57.Peirano RI, Hamann T, Düsing HJ, Akhiani M, Koop U, Schmidt-Rose T, et al. Topically applied L-carnitine effectively reduces sebum secretion in human skin. J Cosmet Dermatol. 2012;11:30–6. doi: 10.1111/j.1473-2165.2011.00597.x. [DOI] [PubMed] [Google Scholar]
- 58.Piérard-Franchimont C, Goffin V, Visser JN, Jacoby H, Piérard GE. A double-blind controlled evaluation of the sebosuppressive activity of topical erythromycin-zinc complex. Eur J Clin Pharmacol. 1995;49:57–60. doi: 10.1007/BF00192359. [DOI] [PubMed] [Google Scholar]
- 59.Wohlrab J, Kreft D. Niacinamide – Mechanisms of action and its topical use in dermatology. Skin Pharmacol Physiol. 2014;27:311–5. doi: 10.1159/000359974. [DOI] [PubMed] [Google Scholar]
- 60.Namazi MR. Nicotinamide in dermatology: A capsule summary. Int J Dermatol. 2007;46:1229–31. doi: 10.1111/j.1365-4632.2007.03519.x. [DOI] [PubMed] [Google Scholar]
- 61.Rolfe HM. A review of nicotinamide: Treatment of skin diseases and potential side effects. J Cosmet Dermatol. 2014;13:324–8. doi: 10.1111/jocd.12119. [DOI] [PubMed] [Google Scholar]
- 62.Veraldi S, Micali G, Barbareschi M, Bettoli V, Fabbrocini G, Monfrecola G, et al. Treatment of mild to moderate acne with topical nicotinamide: Results of three Italian, multicentre clinical studies. [Last accessed on 2015 Dec 29];Eur J Acne Rel Dis. 2009 4:26–4. Available from: http://www.europeanjournalofacne.it/index.php/it/history . [Google Scholar]
- 63.Shalita AR, Smith JG, Parish LC, Sofman MS, Chalker DK. Topical nicotinamide compared with clindamycin gel in the treatment of inflammatory acne vulgaris. Int J Dermatol. 1995;34:434–7. doi: 10.1111/j.1365-4362.1995.tb04449.x. [DOI] [PubMed] [Google Scholar]
- 64.Morganti P, Berardesca E, Guarneri B, Guarneri F, Fabrizi G, Palombo P, et al. Topical clindamycin 1% vs. linoleic acid-rich phosphatidylcholine and nicotinamide 4% in the treatment of acne: A multicentre-randomized trial. Int J Cosmet Sci. 2011;33:467–76. doi: 10.1111/j.1468-2494.2011.00658.x. [DOI] [PubMed] [Google Scholar]
- 65.Khodaeiani E, Fouladi RF, Amirnia M, Saeidi M, Karimi ER. Topical 4% nicotinamide vs 1% clindamycin in moderate inflammatory acne vulgaris. Int J Dermatol. 2013;52:999–1004. doi: 10.1111/ijd.12002. [DOI] [PubMed] [Google Scholar]
- 66.Shahmoradi Z, Iraji F, Siadat AH, Ghorbaini A. Comparison of topical 5% nicotinamid gel versus 2% clindamycin gel in the treatment of the mild-moderate acne vulgaris: A double-blinded randomized clinical trial. J Res Med Sci. 2013;18:115–7. [PMC free article] [PubMed] [Google Scholar]
- 67.Rendon MI, Berson DS, Cohen JL, Roberts WE, Starker I, Wang B. Evidence and considerations in the application of chemical peels in skin disorders and aesthetic resurfacing. J Clin Aesthet Dermatol. 2010;3:32–43. [PMC free article] [PubMed] [Google Scholar]
- 68.Merinville E, Laloeuf A, Moran G, Jalby O, Rawlings AV. Exfoliation for sensitive skin with neutralized salicylic acid? [Last accessed 2015 Dec 29];Int J Cosmet Sci. 2009 31:243–4. Available from: http://onlinelibrary.wiley.com/doi/10.1111/j.1468-2494.2009.00501_2.x/abstract . [Google Scholar]
- 69.Davis EC, Callender VD. A review of acne in ethnic skin: Pathogenesis, clinical manifestations, and management strategies. J Clin Aesthet Dermatol. 2010;3:24–38. [PMC free article] [PubMed] [Google Scholar]
- 70.Davis EC, Callender VD. Postinflammatory hyperpigmentation: A review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol. 2010;3:20–31. [PMC free article] [PubMed] [Google Scholar]
- 71.Handog EB, Datuin MS, Singzon IA. Chemical peels for acne and acne scars in asians: Evidence based review. J Cutan Aesthet Surg. 2012;5:239–46. doi: 10.4103/0974-2077.104911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cole PD, Hatef DA, Taylor S, Bullocks JM. Skin care in ethnic populations. Semin Plast Surg. 2009;23:168–72. doi: 10.1055/s-0029-1224795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Beasley DG, Meyer TA. Characterization of the UVA protection provided by avobenzone, zinc oxide, and titanium dioxide in broad-spectrum sunscreen products. Am J Clin Dermatol. 2010;11:413–21. doi: 10.2165/11537050-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 74.Sambandan DR, Ratner D. Sunscreens: An overview and update. J Am Acad Dermatol. 2011;64:748–58. doi: 10.1016/j.jaad.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 75.Poli F. Acne on pigmented skin. Int J Dermatol. 2007;46(Suppl 1):39–41. doi: 10.1111/j.1365-4632.2007.03463.x. [DOI] [PubMed] [Google Scholar]
- 76.Levy LL, Zeichner JA. Management of acne scarring, part II: A comparative review of non-laser-based, minimally invasive approaches. Am J Clin Dermatol. 2012;13:331–40. doi: 10.2165/11631410-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 77.Joshi SS, Boone SL, Alam M, Yoo S, White L, Rademaker A, et al. Effectiveness, safety, and effect on quality of life of topical salicylic acid peels for treatment of postinflammatory hyperpigmentation in dark skin. Dermatol Surg. 2009;35:638–44. doi: 10.1111/j.1524-4725.2009.01103.x. [DOI] [PubMed] [Google Scholar]
- 78.Lee HS, Kim IH. Salicylic acid peels for the treatment of acne vulgaris in Asian patients. Dermatol Surg. 2003;29:1196–9. doi: 10.1111/j.1524-4725.2003.29384.x. [DOI] [PubMed] [Google Scholar]
- 79.Ahn HH, Kim IH. Whitening effect of salicylic acid peels in Asian patients. Dermatol Surg. 2006;32:372–5. doi: 10.1111/j.1524-4725.2006.32075.x. [DOI] [PubMed] [Google Scholar]
- 80.Draelos ZD. Colored facial cosmetics. Dermatol Clin. 2000;18:621–31. doi: 10.1016/s0733-8635(05)70213-8. [DOI] [PubMed] [Google Scholar]
- 81.Couteau C, Paparis E, Coiffard LJ. BB creams and their photoprotective effect. Pharm Dev Technol. 2016;21:39–42. doi: 10.3109/10837450.2014.965322. [DOI] [PubMed] [Google Scholar]
- 82.Levy LL, Emer JJ. Emotional benefit of cosmetic camouflage in the treatment of facial skin conditions: Personal experience and review. Clin Cosmet Investig Dermatol. 2012;5:173–82. doi: 10.2147/CCID.S33860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Callender VD, Alexis AF, Daniels SR, Kawata AK, Burk CT, Wilcox TK, et al. Racial differences in clinical characteristics, perceptions and behaviors, and psychosocial impact of adult female acne. J Clin Aesthet Dermatol. 2014;7:19–31. [PMC free article] [PubMed] [Google Scholar]
- 84.Matsuoka Y, Yoneda K, Sadahira C, Katsuura J, Moriue T, Kubota Y. Effects of skin care and makeup under instructions from dermatologists on the quality of life of female patients with acne vulgaris. J Dermatol. 2006;33:745–52. doi: 10.1111/j.1346-8138.2006.00174.x. [DOI] [PubMed] [Google Scholar]
- 85.Rougier N, Verdy C, Chesne C. The inhibitive capabilities of a bacterial anti-adhesion gel on the adhesion of Propionibacterium acnes on the corneocytes of subjects with acne. Nouv Dermatol. 2003;22:7–11. [Google Scholar]


