Abstract
Introduction and aims
Gastric mucosa-associated lymphoid tissue (MALT) lymphoma is closely associated with Helicobacter pylori (HP) infection. Our aim was to evaluate demographic, clinical and endoscopic characteristics of gastric MALT lymphoma patients, as well as to analyse response to treatment and factors that affect complete remission (CR) and relapse. We also assessed the long-term prognosis.
Methods
The study involved a retrospective evaluation of consecutive patients admitted with gastric MALT lymphoma (1993–2013).
Results
A total of 144 patients (76 men; mean age 56) were included. At stage EI, 94/103 patients (92%) received HP eradication and 78 (83%) achieved CR after a mean period of 7 months (2–63 months) and 67 (86%) remained in CR after a mean follow-up time of 105 months. HP infection status (p = 0.004) and lymphoma localisation to the antrum plus body (p = 0.016) were associated with higher and lower CR rates, respectively. Relapse occurred in 11/78 (14%) patients after a mean period of 21 months. The absence of HP re-infection (p = 0.038), the need of only one eradication regimen (p = 0.009) and antrum lymphomas (p = 0.031) correlated with lower relapse rates. At stage EII, HP eradication was performed in 17/24 patients but only five experienced CR (30%). Among 16 patients diagnosed at stage EIV, nine achieved CR after chemotherapy ± surgery and 3/7 without remission died due to disease progression. The 5- and 10-year overall disease free survival rates were 90.5% and 79.1%, respectively.
Conclusions
Most patients were diagnosed at an early stage. Eradication therapy was highly effective in inducing complete remission. Long-term evaluation showed that the long-term prognosis was very favourable.
Keywords: Gastric mucosa-associated lymphoid tissue lymphoma, Helicobacter pylori, eradication therapy, complete remission, long-term prognosis
Introduction
Gastric marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT) type, commonly known as gastric MALT lymphoma, is derived from marginal zone B-cells, accounts for 30–40% of all extranodal lymphomas and represents 2–8% of all gastric cancers.1 Helicobacter pylori (HP) infection plays an important role in the development of virtually all gastric MALT lymphomas. This relation was first suggested in 1993 when Hussel et al. showed that lymphoma growth could be stimulated in culture by HP strain-specific T cells exposed to the bacteria.2 Finally, Wotherspoon et al. showed that HP eradication resulted in regression of the lymphoma.3 Thus, this entity represents the paradigm for the association between tumorigenesis and a chronic inflammatory stimulus.4
Eradication therapy is now a well-established therapy for the treatment of gastric MALT lymphoma, independently of stage.5,6 In fact, at early stages HP eradication is associated with complete gastric MALT lymphoma regression in 60–80% of cases.7–9 On the other hand, about 10% of patients at early stages have no evidence of HP infection and for these the best treatment strategy is still controversial.5
In the present study we report our experience in the management of this entity in order to evaluate demographic, clinical and endoscopic characteristics of patients admitted with gastric MALT lymphoma, as well as to analyse responses to therapy and factors that affect remission and relapse. We also assessed the long-term prognosis in this group of patients.
Materials and methods
To address the outcomes we conducted a retrospective evaluation of all consecutive patients admitted with gastric MALT lymphoma in the Gastroenterology Department of Lisbon Oncology Institute between 1993–2013. The diagnosis of gastric MALT lymphoma was established by histological and immunophenotypic analysis of gastric biopsies and supplemented by molecular study using polymerase chain reaction to demonstrate clonal proliferation in equivocal cases. The presence of HP infection, both at the time of diagnosis and after eradication therapy, was evaluated by histopathologic and culture examination of gastric biopsies in all subjects and, in doubtful cases, by immunohistochemistry. More recently, the urea breath test was also applied.
Patients were staged according to the Ann Arbor staging system modified by Musshoff.10 Staging procedure included clinical examination, full blood count, biochemistry, cervical, chest, abdomen and pelvis computed tomography scan, gastric endoscopic ultrasound, bone marrow biopsy and aspiration and flow cytometric immunophenotyping of peripheral blood and bone marrow aspirate.
Treatment options were based on HP status and stage. Most of the patients diagnosed at an early stage (EI not beyond the muscular propria) were only treated with eradication therapy. According to the regimens used for HP eradication, patients were treated with the first line regimen in the respective period. Thus, most patients were treated with triple therapy with a combination of proton pump inhibitor plus amoxicillin and clarithromycin or metronidazole, in the earlier years for seven days but some years later for 14 days according to the updated recommendations. When the first regimen had failed, patients were retreated with an alternative one, sometimes with a quinolone, and few patients received quadruple therapy. Patients diagnosed at a more advanced stage received additional therapies (surgery, radiotherapy and/or chemotherapy).
About eight weeks after completion of therapy, an upper gastrointestinal endoscopy with multiple biopsies for histologic and cultural evaluation was performed. Complete remission (CR) was defined as no macroscopic lesion and an absence of histologic evidence of lymphoma on biopsies in two upper gastrointestinal endoscopies. Partial remission was defined as at least a 50% tumour reduction in endoscopic evaluation and histologically by the presence of signs of lymphoma regression. The histological response was evaluated according to the histological scoring of lymphoid infiltrations in the stomach proposed by Wotherspoon et al.3 Fischbach et al. defined minimal histological residuals after HP eradication as ‘disappearance of any endoscopic lesion with the exception of harmless features of post-HP gastritis and the presence of a lymphoid infiltrate in post-treatment biopsies, revealing monotonous infiltrates of centrocyte-like cells or lymphoepithelial lesions, or both.11 In these cases, we considered that the patients had histologic residual disease corresponding to a partial remission and we adopted a watch-and-wait strategy. Most of the patients who did not achieve CR within 12–18 months after eradication therapy, or patients with evidence of disease progression, were proposed for alternative therapies, mainly chemotherapy. In recent years, a small subgroup of patients with relapse after CR were also treated with immunotherapy isolated or combined with chemotherapy. Patients who achieved CR were followed regularly with upper gastrointestinal endoscopy, every three or four months during the first year, every six months in the following year and yearly after that, but a clinical surveillance without endoscopy was performed when the patient refused further endoscopies or due to comorbidities. Causes of death were reported during the follow-up.
Statistical analysis was conducted using IBM SPSS software version 20. Exact and chi-squared tests were performed for group comparison. Logistic regression analysis was performed to find factors associated with CR and relapse of lymphoma. Overall survival was calculated from time of diagnosis to time of death of any cause or last follow-up. Survival curves were estimated by Kaplan Meier method. Values of p of 0.05 or less were taken as statistically significant.
Results
Patients’ demography is summarised in Table 1. One hundred and forty-four patients were included in this study, 76 males, with a mean age at diagnosis of 56 years. Most patients presented with dyspeptic symptoms and only 11% showed B symptoms. The endoscopic findings more often documented were erosions or ulcers, specially localised in the antrum. Most of the patients were diagnosed at an early stage (Table 2).
Table 1.
Patient demographics
| Characteristics | n = 144 |
|---|---|
| Age (years) | 56 ± 13 (13–83) |
| Gender | |
| Male | 76 (53%) |
| Female | 68 (47%) |
| Clinical presentation | |
| Epigastric pain | 53 (36%) |
| Bloating | 45 (32%) |
| GI bleeding | 15 (10%) |
| Nausea and vomiting | 9 (6%) |
| Gastric perforation | 1 (1%) |
| Others | 11 (8%) |
| Unknown | 10 (7%) |
| B symptoms | 11 (8%) |
| Endoscopic findings | |
| Erosions/ulcers | 67 (46%) |
| Hyperaemia | 26 (18%) |
| Thickened folds | 24 (17%) |
| Ulcerated mass | 21 (14%) |
| Polypoid lesion | 6 (4%) |
| Location | |
| Antrum/incisura angularis | 65 (45%) |
| Body | 47 (33%) |
| Antrum + body | 25 (17%) |
| Fundus | 5 (4%) |
| Diffuse | 2 (1%) |
GI: gastro-intestinal.
Table 2.
Classification of Ann Arbor modified by Musshoff
| Limited to the stomach | Stage EI | 103 |
| Confined to the mucosa and submucosa | EI1 | 80 |
| Extended over the submucosa | EI2 | 23 |
| Involvement of stomach and regional nodes | Stage EII | 24 |
| Lymph-nodes contiguous with the stomach | EII1 | 17 |
| Non-contiguous sub-diaphragmatic lymph nodes | EII2 | 7 |
| Involvement of lymph nodes on both sides of the diaphragm | Stage EIII | 0 |
| Involvement of distant organs | Stage EIV | 17 |
Treatment outcome by stage
Stage EI
Out of 103 patients at the stage EI, HP infection was documented in 84 (82%). Surgery was the first treatment option in two HP patients who were diagnosed in the first years of our series and had gastric wall involvement beyond the muscular propria. Thus, eradication of the bacteria was the first treatment option in almost all of these patients (82/84) and successful eradication was achieved in all but one. Seventy-three patients achieved CR with this treatment option but nine did not despite successful eradication in eight of them. Eradication therapy was also tried in 12 patients in whom HP was not documented and five of them achieved CR. Thus, we had 103 patients at stage EI and 94 of them (92%) were treated with eradication therapy, which was successful in 78 patients (83%), of whom five were HP negative, after a mean period of seven months (2–63 months). By detailing, we observed that 86% (67/78) of these patients achieved CR within 12 months after eradication therapy and only 5% (4/78) took longer than 24 months. The remaining patients at this stage were treated with additional therapies and two were still in the ‘watch-and-wait’ period.
The comparison between responders and non-responders to eradication therapy showed that, besides no evidence of HP infection (p = 0.001), diffuse infiltration of the stomach as well as lymphoma localisation to the body plus antrum were significantly (p = 0.007) associated with lower remission rates. In multivariate analysis, HP infection maintained prognostic value in predicting CR (odds ratio (OR) 10.1, 95% confidence interval (CI): 2.132–47.754, p = 0.004). In contrast, antrum plus body lymphomas were associated with lower CR rates (OR 0.12, 95% CI: 0.023–0.674, p = 0.016) (Table 3).
Table 3.
Factors associated to remission after Helicobacter pylori (HP) eradication in patients with limited stage disease
| Variable | Remission (n = 78) | No remission (n = 16) | Univariate analysis (p value) | Multivariate analysis |
|
|---|---|---|---|---|---|
| (p value) | OR (95% CI) | ||||
| Mean age (years) | 58 ± 12 | 55 ± 13 | 0.820 | 0.432 | 0.98 (0.921–1.036) |
| Gender | |||||
| Male | 42/50 (84%) | 8/50 (16%) | 0.791 | 0.541 | 0.64 (0.151–2.699) |
| Female | 36/44 (82%) | 8/44 (18%) | |||
| Location | |||||
| Antrum | 38/42 (90%) | 4/42 (10%) | |||
| Body | 24/29 (83%) | 5/29 (17%) | 0.381 | 0.48 (0.094–2.469) | |
| Antrum + body | 10/15 (67%) | 5/15 (33%) | 0.007 | 0.016 | 0.12 (0.023–0.674) |
| Fundus | 5/6 (83%) | 1/6 (17%) | 0.607 | 0.49 (0.034–7.174) | |
| Diffuse | 0/2 | 2/2 (100%) | |||
| Depth | |||||
| EI2 | 63/74 (85%) | 11/74 (15%) | 0.256 | 0.621 | 0.591 (0.074–4.751) |
| EI1 | 15/20 (75%) | 5/20 (25%) | |||
| H. pylori | |||||
| HP− | 73/82 (89%) | 9/82 (11%) | 0.001 | 0.004 | 10.1 (2.132–47.754) |
| HP+ | 5/12 (42%) | 7/12 (58%) | |||
CI: confidence interval: OR: odds ratio.
During the follow-up period – mean time of 105 months (12–232 months) – the majority of patients (67/78, 86%) remained in CR. Relapse occurred in 11 patients (14%) after a mean period of 21 months (4–89 months). By discriminating, we found that four patients (36%) relapsed within the first 12 months. Among them, HP infection was documented again in three and all of them achieved and maintained CR with another eradication treatment. Table 4 shows the characteristics of relapsed patients diagnosed at the earliest stage.
Table 4.
Characterisation of patients with gastric mucosa-associated lymphoid tissue (MALT) lymphoma at stage EI who have relapsed
| Sex | Age (years) | HP | Therapy | Time to relapse (months) | HP reinfection | Local of relapse | Relapse therapy | Response | Additional therapies | End of follow-up | DFS (months) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 45 | Yes | HP eradication | 14 | Yes | Gastric | HP eradication | No remission | RCHOP Radiation | Alive without disease | 41 |
| 2 | F | 29 | Yes | HP eradication | 15 | Yes | Gastric | HP eradication | Remission | Alive without disease | 153 | |
| 3 | M | 58 | Yes | HP eradication | 30 | No | Upper limb mass and perigastric lymph nodes | RCHOP | Remission | Alive without disease | 37 | |
| 4 | M | 69 | Yes | HP eradication | 89 | Yes | Gastric | HP eradication | Remission | Alive without disease | 6 | |
| 5 | M | 61 | Yes | HP eradication | 14 | No | Gastric and perigastric lymph nodes | CVP | Remission | Dead without disease | 114 | |
| 6 | M | 57 | No | HP eradication Chlorambucila | 24 | No | Gastric | Rituximab | Remission | Radiation (2nd relapse) | Alive without disease | 44 |
| 7 | F | 46 | No | HP eradication Chlorambucila | 16 | No | Gastric | RCHOP | Remission | Alive without disease | 56 | |
| 8 | M | 49 | Yes | HP eradication | 11 | No | Gastric | Radiation | Remission | Alive without disease | 37 | |
| 9 | F | 42 | Yes | HP eradication | 9 | Yes | Gastric | HP eradication | Remission | Alive without disease | 29 | |
| 10 | M | 56 | Yes | HP eradication | 11 | Yes | Gastric | HP eradication | Remission | Chlorambucil (2nd relapse) RCVP (3th relapse) | Alive without disease | 33 |
| 11 | F | 78 | Yes | HP eradication | 4 | Yes | Gastric | HP eradication | Remission | Alive without disease | 18 |
CVP: cyclophosphamide, vincristine, prednisone; DFS: disease free survival; F/M: female/male; HP: Helicobacter pylori; RCHOP-rituximab, cyclophosphamide, doxorubicin (hydroxydaunomycin), vincristine (oncovin), prednisolone; RCVP: rituximab, cyclophosphamide, vincristine, prednisone.
These patients did not achieve complete remission after HP eradication and watch-and-wait strategy, and thus received an alternative therapy.
We also tried to identify factors, such as HP re-infection, age at diagnosis, gender, location, depth of infiltration and number of eradication regimens needed, associated with the relapse after complete remission in patients treated with antibiotics. In multivariate analysis, HP re-infection (OR = 7.08, 95% CI: 1.110–45.086, p = 0.038) showed prognostic value in predicting the relapse. In contrast, the need of only one eradication regimen (OR = 0.063, 95% CI: 0.008–0.495, p = 0.009) and antrum lymphomas (OR = 0.039, 95% CI: 0.002–0.743, p = 0.031) were associated with lower relapse rates.
Stage EII
At this stage 13 patients had HP infection and 11 did not. Eradication therapy was the first treatment option in 11 and six patients, respectively, and CR was achieved in 4/11 and 1/6 patients. Thus, only 30% of patients achieved remission after eradication therapy. Concerning the remaining patients, 17 out of 24 patients achieved remission with other treatment options (surgery n = 2, radiotherapy n = 6, chemotherapy ± surgery/radiotherapy n = 8, surgery plus chemotherapy n = 1), one was under radiotherapy and one patient never achieved remission even after several courses of chemotherapy and radiotherapy (alive with disease). One patient that had achieved remission after chemotherapy experienced gastric MALT lymphoma relapse and died due to disease progression.
Stage EIV
Among 17 patients diagnosed at stage IV, 10 patients had evidence of disseminated disease by computerized tomography (CT) evaluation. The remaining patients had normal CT evaluation but had evidence of bone marrow infiltration. Ten patients achieved remission after chemotherapy ± surgery and three out of seven patients without remission died due to disease progression. One patient that had achieved remission after chemotherapy experienced gastric MALT lymphoma relapse and died due to disease progression.
Long-term prognosis
After a mean follow-up time period of 109 months (4–246 months), 112 patients were still alive (99 without disease) and 32 died (five due to disease progression). The mean age at the end of the follow up was 66 ± 13 years (20–93 years). A second cancer was the cause of death in 11 patients: haematologic (n = 4), colon (n = 1), lung (n = 1), pancreas (n = 1), sarcoma (n = 1), breast (n = 1), head and neck (n = 1) and brain (n = 1). The remaining patients died due to other several diseases: neurologic (n = 3), infection (n = 3), cardiovascular (n = 2), liver (n = 1), accident (n = 1), unknown (n = 6). There were no patients with gastric carcinoma during the follow-up and diffuse large B-cell lymphoma was diagnosed in five patients. Among them, three patients, stage EI (n = 1), stage EII (n = 1), stage EIV (n = 1), had never achieved CR of gastric MALT lymphoma despite several treatment options (chemotherapy ± immunotherapy/radiotherapy) and diffuse large B-cell lymphoma was diagnosed 144, 151 and 17 months after diagnosis, respectively. The first one was alive with disease but the others died due do disease progression. In the two other patients (stage EI) it was diagnosed 12 and 33 months after CR, which was achieved with eradication of HP. Both of them achieved again and maintained remission after chemotherapy.
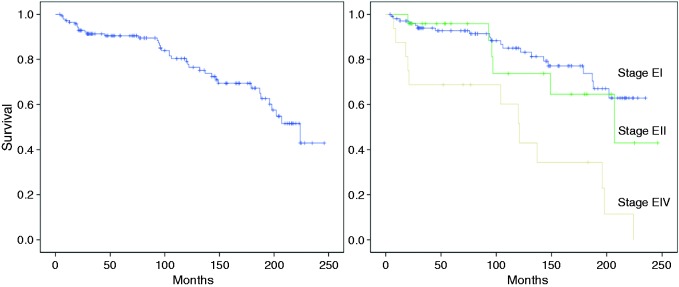
The 5-, 10- and 15-year overall disease-free survival rates were 90.5%, 79.1% and 67.3%, respectively. Disease free survival correlated with stage (log rank test, p = 0.001) – Figure 1.
Figure 1.
Overall disease free survival estimate of all patients (left) and by stage (right).
Discussion
In recent years the prevalence of primary gastric lymphoma has been increasing,12 although gastric MALT lymphoma remains a rare disease, accounting for 2–8% of all gastric cancers.1 Here we present one of the largest series, with the longest follow-up, of patients with gastric MALT lymphoma, independently of stage.
It is now widely accepted that chronic HP infection provides the antigen stimulus to gastric MALT lymphoma, through the clonal expansion of lymphoid cells.4 Eradication therapy is now widely accepted as the standard treatment for gastric MALT lymphoma.4 Patients at early stages can achieve CR with HP eradication, which is supported by several studies that showed high remission rates after eradication therapy.7–9 In our study, we found that the CR rate was 83% for patients at stage EI, but it was much lower (30%) in patients at stage EII, which is in line with previous findings.13 At stage EI, 86% of patients achieved CR in a period less than 12 months (mean time seven months), but interestingly, one patient took 63 months to achieve it. The delay in achieving complete histological remission was already reported in other studies,14 which is the base for the adoption of a watch and wait strategy.5,6 Actually, current European Society for Medical Oncology (ESMO) guidelines state that is reasonable to wait for at least 12 months before starting another treatment in patients who achieve clinical and endoscopic remission together with eradication of HP, albeit having persistent (residual) lymphoma at the histological level.5
Patients who are not infected with HP, not responding to antibiotics, have relapsed or have advanced disease, should be considered for other therapeutic modalities. Nowadays, surgery is reserved for complications, such as perforation or endoscopically uncontrollable bleeding. Radiation therapy has shown good results in early/localised disease with respect to efficacy and safety.6 Fischbach et al. compared surgery with radiation in 19 patients with early/localised gastric MALT lymphoma and showed that both therapies presented excellent long-term outcome. However, radiotherapy was associated with a significant higher quality of life.15 Different types of chemotherapy and immunotherapy are effective treatment modalities for gastric MALT lymphoma in both limited and advanced stages of the disease. Rituximab, an anti-CD20 antibody, has been studied as an isolated treatment or in combination with chemotherapy, showing high rates of disease control.6 Zucca et al. have recently reported a randomised study comparing chlorambucil versus chlorambucil plus rituximab and concluded that although both treatments were active, a higher complete remission rate and 5-year event-free survival were achieved with combined therapy.16
With regard to clinical and endoscopic presentation, in our series most patients presented with dyspeptic symptoms (only 11% showed B symptoms) and the more frequent endoscopic findings were erosions and ulcers most often localised in the antrum. This is in accordance with previous reports.17
Several predictive factors for non-response to eradication therapy have been identified, including the absence of HP infection, advanced stage, deep tumour invasion in the gastric wall, proximal gastric location and API2-MALT1 translocation.9,18–20 In our study, the comparison between responders and non-responders to eradication therapy at the stage EI, showed that both the absence of HP infection (p = 0.004) and a more extensive location, body plus antrum lymphomas, (p = 0.016) were associated with lower CR rates.
The management strategy for gastric MALT lymphoma without evidence of HP infection remains controversial.5 In our study, HP infection was initially excluded with at least two different diagnostic tests. Eradication therapy was tried in 12 and six HP negative patients at stages EI and EII, respectively. Remission was achieved in five (41%) and one (17%), respectively. A recent systematic review, including data of 110 HP negative patients, showed that eradication therapy achieved complete lymphoma regression in 17 (15.5%; 95% CI 8.7–22.2).21 As possible explanations, it has been suggested either that HP infection can be present, despite the negative results of several diagnostic tests, or that antibiotic therapy may act against other bacteria potentially involved in gastric MALT lymphoma pathogenesis.17
An aspect to consider in the management of gastric MALT lymphoma patients is the possibility of relapse. In our study, the relapse rate was 14%, which is higher compared to the relapse rates reported in other studies.9 Interesting, 36% of these patients relapsed within the first 12 months and among them, HP infection was documented again in three, and all of them achieved and maintained CR with another eradication therapy. We also documented that patients who needed two or more eradication regimens had higher recurrence rates. Furthermore, it is also known that recrudescence (recolonisation with the same strain) rather than reinfection (colonisation with a new strain) is considered more likely to happen.22 Given this background, we can speculate than the phenomenon of HP recrudescence implies a period in which the amount of HP is so low that it is not detectable by diagnostic tests and even allows lymphoma regression due to low antigenic stimulation. Thus, our relapse rate during the first year is more likely secondary to recrudescence of HP infection rather HP re-infection.
Gastric MALT lymphomas have an indolent course with long disease-free and overall survival,8,23 which is also supported by our results. However, long-term and regular monitoring is recommended for all patients.5 Indeed, the risk of gastric adenocarcinoma among these patients has been reported to be six-fold higher than in the general population24 and also the risk of other neoplasms, namely non-Hodgkin’s lymphomas, may be increased.25 We did not report cases of gastric adenocarcinoma but 11 patients died due to a second cancer. However, we did not calculate the cancer incidence rate for the general population adjusted for age and sex. Further studies are needed to clarify if these patients are at increased risk of developing second cancers.
With this study, we conclude that most patients were diagnosed at an early stage and, among these HP eradication was an effective therapy. The indolent course of the disease can justify, in a group of selected patients who do not achieve CR with antibiotics, a ‘watch-and-wait’ strategy. In our series the overall prognosis was favourable with good long-term survival rates.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Swerdlow SH, Campo E, Seto M, et al. Mantle cell lymphoma. In: Swerdlow SH, International Agency for Research on Cancer; World Health Organization, eds. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: International Agency for Research on Cancer, 2008, pp. 229–232.
- 2.Hussell T, Isaacson PG, Crabtree JE, et al. The response of cells from low-grade B-cell gastric lymphomas of mucosa-associated lymphoid tissue to Helicobacter pylori. Lancet 1993; 342: 571–574. [DOI] [PubMed] [Google Scholar]
- 3.Wotherspoon AC, Doglioni C, Diss TC, et al. Regression of primary low-grade B-cell gastric lymphoma of mucosa-associated lymphoid tissue type after eradication of Helicobacter pylori. Lancet 1993; 342: 575–577. [DOI] [PubMed] [Google Scholar]
- 4.Owens SR, Smith LB. Molecular aspects of H. pylori-related MALT lymphoma. Patholog Res Int 2011; 2011: 193149–193149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zucca E, Copie-Bergman C, Ricardi U, et al. Gastric marginal zone lymphoma of MALT type: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 2013; 24: vi144–vi148. [DOI] [PubMed] [Google Scholar]
- 6.Ruskoné-Fourmestraux A, Fischbach W, Aleman BPM, et al. EGILS consensus report. Gastric extranodal marginal zone B-cell lymphoma of MALT. Gut 2011; 60: 747e758–747e758. [DOI] [PubMed] [Google Scholar]
- 7.Fischbach W, Goebeler-Kolve ME, Dragosics B, et al. Long term outcome of patients with gastric marginal zone B cell lymphoma of mucosa associated lymphoid tissue (MALT) following exclusive Helicobacter pylori eradication therapy: Experience from a large prospective series. Gut 2004; 53: 34–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stathis A, Chini C, Bertoni F, et al. Long-term outcome following Helicobacter pylori eradication in a retrospective study of 105 patients with localized gastric marginal zone B-cell lymphoma of MALT type. Ann Oncol 2009; 20: 1086–1093. [DOI] [PubMed] [Google Scholar]
- 9.Zullo A, Hassan C, Cristofari F, et al. Effects of Helicobacter pylori eradication on early stage gastric mucosa-associated lymphoid tissue lymphoma. Clin Gastroenterol Hepatol 2010; 8: 105–110. [DOI] [PubMed] [Google Scholar]
- 10.Musshoff K. Clinical staging classification of non-Hodgkin's lymphomas (author's transl). Strahlentherapie 1977; 153: 218–221. [PubMed] [Google Scholar]
- 11.Fischbach W, Goebeler ME, Ruskone–Fourmestraux A, et al. Most patients with minimal histological residuals of gastric MALT lymphoma after successful eradication of Helicobacter pylori can be managed safely by a watch and wait strategy: Experience from a large international series. Gut 2007; 56: 1685–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Severson RK, Davis S. Increasing incidence of primary gastric lymphoma. Cancer 1990; 66: 1283–1287. [DOI] [PubMed] [Google Scholar]
- 13.Ruskoné-Fourmestraux A, Lavergne A, Aegerter PH, et al. Predictive factors for regression of gastric MALT lymphoma after anti-Helicobacter pylori treatment. Gut 2001; 48: 297–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee SK, Lee YC, Chung JB, et al. Low grade gastric mucosa associated lymphoid tissue lymphoma: Treatment strategies based on 10 year follow-up. World J Gastroenterol 2004; 10: 223–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fischbach W, Schramm S, Goebeler E. Outcome and quality of life favour a conservative treatment of patients with primary gastric lymphoma. Z Gastroenterol 2011; 49: 430–435. [DOI] [PubMed] [Google Scholar]
- 16.Zucca E, Conconi A, Laszlo D, et al. Addition of rituximab to chlorambucil produces superior event-free survival in the treatment of patients with extranodal marginal-zone B-cell lymphoma: 5-Year analysis of the IELSG-19 randomized study. J Clin Oncol 2013; 31: 565–572. [DOI] [PubMed] [Google Scholar]
- 17.Zullo A, Hassan C, Ridola A, et al. Gastric MALT lymphoma: Old and new insights. Ann Gastroenterol 2014; 27: 27–33. [PMC free article] [PubMed] [Google Scholar]
- 18.Nakamura S, Sugiyama T, Matsumoto T, et al. Long-term clinical outcome of gastric MALT lymphoma after eradication of Helicobacter pylori: A multicentre cohort follow-up study of 420 patients in Japan. Gut 2012; 61: 507–513. [DOI] [PubMed] [Google Scholar]
- 19.Nakamura S, Ye H, Bacon CM, et al. Clinical impact of genetic aberrations in gastric MALT lymphoma: A comprehensive analysis using interphase fluorescence in situ hybridisation. Gut 2007; 56: 1358–1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu H, Ye H, Ruskone-Fourmestraux A, et al. T(11; 18) is a marker for all stage gastric MALT lymphomas that will not respond to H. pylori eradication. Gastroenterology 2002; 122: 1286–1294. [DOI] [PubMed] [Google Scholar]
- 21.Zullo A, Hassan C, Ridola L, et al. Eradication therapy in Helicobacter pylori-negative, gastric low-grade mucosa–associated lymphoid tissue (MALT) lymphoma patients. A systematic review. J Clin Gastroenterol 2013; 47: 824–827. [DOI] [PubMed] [Google Scholar]
- 22.Xia HX, Talley NJ, Keane CT, et al. Recurrence of Helicobacter pylori infection after successful eradication: Nature and possible causes. Dig Dis Sci 1997; 42: 1821–1834. [DOI] [PubMed] [Google Scholar]
- 23.Wündisch T, Thiede C, Morgner A, et al. Long-term follow-up of gastric MALT lymphoma after Helicobacter pylori eradication. J Clin Oncol 2005; 23: 8018–8024. [DOI] [PubMed] [Google Scholar]
- 24.Capelle LG, de Vries AC, Looman CW, et al. Gastric MALT lymphoma: Epidemiology and high adenocarcinoma risk in a nation-wide study. Eur J Cancer 2008; 44: 2470–2476. [DOI] [PubMed] [Google Scholar]
- 25.Wündisch T, Dieckhoff P, Greene B, et al. Second cancers and residual disease in patients treated for gastric mucosa-associated lymphoid tissue lymphoma by Helicobacter pylori eradication and followed for 10 years. Gastroenterology 2012; 143: 936–942. [DOI] [PubMed] [Google Scholar]