Abstract
Objective
Endoscopic mucosal resection (EMR) is widely practiced in western countries. Endoscopic submucosal dissection (ESD) is very effective for treating complex polyps but colonic ESD in the western setting remains challenging. We have developed a novel technique of knife-assisted snare resection (KAR) for the resection of these complex lesions. Here we aim to describe the technique, evaluate its outcomes, identify outcome predictors and define its learning curve.
Methods
We conducted a prospective cohort study of patients who had large and refractory polyps resected by KAR at our institution from 2007 to 2013. Polyp characteristics and procedure details were recorded. Endoscopic follow-up was performed to identify recurrence.
Results
A total of 170 patients with polyps 20–170 mm in size were treated by KAR and followed up for a mean of 31.5 months (range 12–84 months). 29% of the polyps were >50 mm, 22% had fibrosis from previous unsuccessful interventions and 25% were in the right colon.
The perforation rate (1.2%) and bleeding rate (4.7%) were acceptable and managed conservatively in most patients. Recurrence rate after the first attempt was 13.1%. Recurrence was significantly increased by polyp size >50 mm (p = 0.008; OR 5.03, 95% CI 1.54–16.48), presence of fibrosis (p = 0.002; OR 6.59, 95% CI 1.97–22.07) and piecemeal resection (p < 0.001; OR 0.31, CI 0.078–1.12). Cure rates were 87% after the first attempt, improving to 95.6% with further attempts. En bloc resection rate showed a linear increase and reached almost 80% as the endoscopist’s cumulative experience approached 100 cases.
Conclusion
This is the largest reported Western series on KAR in the colon. We have demonstrated the feasibility, efficacy and safety of this technique in the treatment of complex polyps, with or without fibrosis and at all sites. KAR has shown better outcomes than either EMR or ESD.
We have also managed to identify significant outcome predictors and define the learning curve.
Keywords: Endoscopic mucosal resection, EMR, endoscopic submucosal dissection, ESD, colonoscopy, colonic polyps, difficult polyps
Introduction
Endoscopic resection has become the preferred way to treat the majority of large benign colonic polyps, with reduced morbidity and mortality compared to conventional surgical resections.1 Endoscopic mucosal resection (EMR) is an established technique for the resection of large and flat colonic polyps. This involves a submucosal injection, followed by resection of the lesion using an endoscopic snare. This is effective, with low complication rates. However, lesion regrowth can occur, with recurrence rates of up to 50%.2 However, if EMR of large lesions is performed in multiple pieces, the histological evaluation of the specimen is compromised, especially relating to the completeness of excision.3 It is also associated with high recurrence rates.3
Endoscopic submucosal dissection (ESD) is a technique which enables large lesions to be resected en bloc. The technique was developed in Japan as a means of achieving en bloc resection of gastric cancer and has been increasingly used for the treatment of colorectal neoplasms.4–6 The key advantage of ESD is en bloc resection. This reduces recurrence rates and allows very good histological evaluation of the specimen (completeness of excision, depth of invasion of cancer). However, the procedure time and complication rate is greater with ESD than with EMR.7–9 ESD is technically more challenging, with a steep learning curve,10 and that is one of the big reasons for the poor uptake of this technique in the West, especially for colonic neoplasia.
We have developed the technique of knife-assisted snare resection (KAR) by combining some principles of EMR and ESD. It involves submucosal injection followed by a mucosal incision in the normal mucosa adjacent to the lesion and a degree of submucosal dissection, with gradual extension of the mucosal incision until it becomes circumferential. This is followed by snare-assisted resection of the lesion in a piecemeal or en bloc fashion depending on the size of the lesion and the extent of submucosal dissection. The aim of the technique is to reduce recurrence rates, shorten the learning curve for ESD, shorten procedure times and reduce complication rates related to ESD. However, none of the above benefits related to the technique have been proven.
Aims
The aim of our study was to assess the feasibility, safety and outcome of KAR in the resection of large and refractory polyps. We also aimed to identify polyp features that can help predict outcome and define the learning curve of KAR.
Methods
This is a prospective cohort study of patients referred to our centre for resection of large and difficult colonic polyps from 2007 to 2013. Institutional review board approval was obtained (PHT/2744). Informed consent for the procedure was obtained and data were prospectively recorded in an electronic database. All patients who had KAR for the resection of their colonic polyps were included. Polyps <20 mm in size were excluded. Warfarin was discontinued five days prior to the procedure. Aspirin or clopidogrel alone was not discontinued but if taken in combination then as per advice from the cardiologists, either clopidogrel or aspirin was discontinued.
All procedures were performed under conscious sedation with midazolam 1–5 mg and fentanyl 25–100 mcg by a single experienced endoscopist (PB) who had performed more than 200 complex colonic EMR procedures before starting the study. Procedures were performed using Olympus or Fujinon endoscopes with Lucera CCV260 or EPX4400 processors. Lesions were assessed using non-magnifying endoscopes and chromoendoscopy with 0.2% indigo carmine dye spray. Polyps with features suggestive of invasive malignancy were excluded. Polyp characteristics and complication details were recorded. Details on resection type (en bloc KAR vs. piecemeal KAR) were recorded.
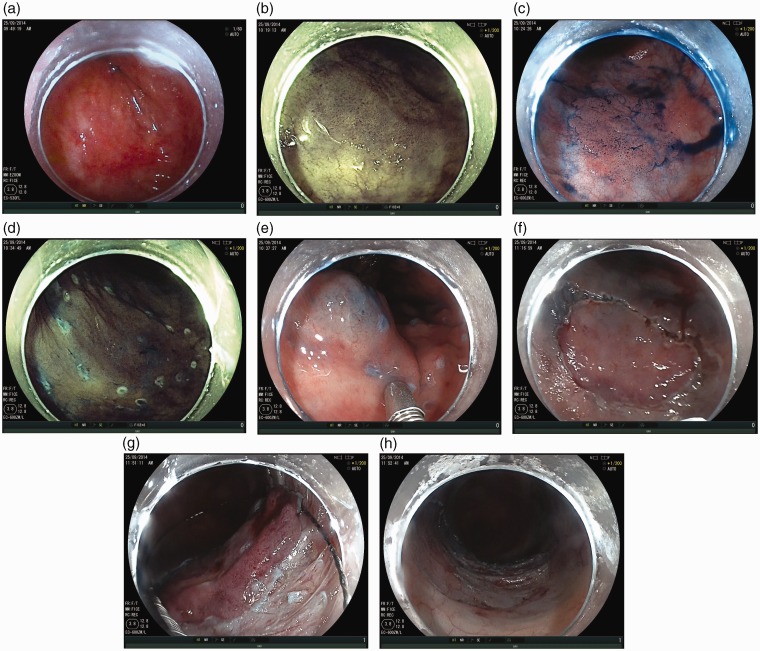
Technique (see Figure 1)
Figure 1.
(a) DALM in transverse colon assessed with HDWL; (b) Same lesion with FICE; (c) Same lesion with indigo carmine; (d) Marking of the lesion; (e) Lesion following submucosal injection; (f) Circumferential mucosal incision; (g) Snare resection following circumferential dissection and (h) KAR resection base.
The lesion was cleaned thoroughly with flushes of water to remove the adherent mucus and then sprayed with indigo carmine to allow detailed assessment of the pit pattern, to decide on the suitability of endoscopic resection, and to allow for accurate delineation of the margins.
Submucosal injection was started on the distal (anal) side of the lesion with lifting solution (500 ml gelofusin + 1 ml adrenaline + 2 ml of 1% indigo carmine). Mucosal incision was started on the anal side of the lesion with a flush knife (Fujinon) or dual knife (Olympus). The initial incision was very superficial to expose the submucosa and identify any vessels which were then coagulated with the knife before dissecting through them and deepening the mucosal incision. This was immediately followed by further submucosal dissection before extending the mucosal incision further and repeating the same process till a circumferential incision was achieved. The aim of the submucosal dissection was to continue the dissection till at least a 10 mm mucosal flap was raised all around the lesion to allow for snare application. At this stage depending on the size of the lesion and the degree of submucosal dissection performed, a snare-assisted resection of the lesion was performed in a piecemeal or en bloc fashion.
If the lesion was scarred from previous interventions, then this technique was modified. It is difficult to achieve a lift with submucosal injection in a scarred area. In these cases, submucosal injection was performed repeatedly from different angles to gradually achieve a lift, which was usually suboptimal. Normal mucosa next to the scarred area was then lifted and mucosal incision followed by some submucosal dissection was performed in this normal mucosa. Once the submucosal dissection plane was identified in the normal area, it was then extended slowly through the scarred area by gradually dissecting through the fibrosis. For laterally spreading tumours (LSTs) that spread beyond half the circumference of the bowel, a lot more dissection had to be performed in order to dissect the lateral spread of the tumour and allow the snare to capture it en bloc. When it was not possible to perform that much submucosal dissection, the lesion was resected in a piecemeal fashion after achieving circumferential mucosal incision. The same principle was applied to lesions larger than 40 mm in size.
The knives used for KAR included the flush knife (Fujinon DK2618J), dual knife (Olympus KD-650 L), IT nano knife (Olympus KD-612U) and IT2 knife (Olympus KD-611 L). We used the ERBE VIO 200 diathermy generator for all our procedures. We used a standard diathermy setting with all the knives (Endo cut effect 2, cut duration 3, cut interval 3 and forced coagulation Effect 2, max watts 50).
The snares used were of sizes 15 mm (Olympus SD-210U-15), 20 mm (Olympus SD-230U-20) and 25 mm (SD-210U-25). Coag graspers and clips were used during the resection if required. The resected lesion was retrieved with a Roth net.
First endoscopic follow-up was performed at three to six months and then again at one year to check for local recurrence before prolonging the surveillance interval. As a routine, biopsies were taken from the resection site at follow-up. Recurrence was defined as visual or microscopic evidence of polyp tissue regrowth at the site of resection at any follow-up.
Perforation was defined as a full thickness breach in muscularis propria with or without symptoms. Bleeding was defined as a significant bleed resulting in the procedure being abandoned or post-procedure bright red rectal bleeding resulting in hospital admission, blood transfusion or requiring endoscopic or surgical intervention. Post-polypectomy syndrome (PPS) was defined as pain (with or without fever) after the procedure that resulted in hospital admission.
Results
Patient population
During a six-year period from 2007 to 2013, 348 patients with polyps >2 cm were referred to our unit. KAR was performed in 170 patients. KAR was the preferred resection technique in lesions meeting the following criteria: large lesions with stable access, lesions with fibrosis/scarring related to previous intervention, lesions in colitic bowels, lesions for which there was a suspicion of submucosal invasion, sessile serrated polyps in the right colon and non-granular-type LSTs (LST-NGs). The average age of the patients was 71 years, with a range of 31 to 94 years. The male to female ratio was 1.26:1. All patients were referred after another experienced endoscopist found them to have a difficult polyp.
Polyp characteristics
The mean size of the polyps resected was 46 mm, with a range of 20 to 170 mm. A total of 120 of 170 (71%) were 20–50 mm in size and 50/170 (29%) were >50 mm. Of the 170, 141 (83%) lesions were flat and 29/170 (17%) were sessile. Of the 141 flat lesions, 117 (83%) were granular-type LST (LST-G), 17 (12%) were LST-NG and 7 (5%) were felt to be dysplasia-associated lesions or masses (DALMs) in colitic bowels. 37 of 170 (22%) resections were performed on polyps scarred from previous unsuccessful interventions. 43 of 170 (25%) of the polyps were in the right colon (Table 1).
Table 1.
Lesion characteristics
| 20–50 mm | >50 mm | Fibrosis | L colon | R colon | |
|---|---|---|---|---|---|
| KAR (N = 170) | 120 (71%) | 50 (29%) | 37 (22%) | 127 (75%) | 43 (25%) |
KAR:knife-assisted snare resection; L: left; R: right.
Type of resection
KAR was attempted in a total of 170 polyps and was completed in 165 (97%). The remaining five could not be completely resected endoscopically and had to be referred for surgery. Procedure time varied from 80 to 240 minutes with a mean of 150 minutes. Of the 170 polyps, 70 (41%) were performed en bloc. Table 2 shows the factors affecting en bloc resection rate.
Table 2.
Predictors of en bloc resection. Multivariate analysis
| SIZE |
FIBROSIS |
SITE |
||||
|---|---|---|---|---|---|---|
| 20–50 mm n = 120 | >50 mm n = 50 | Yes n = 37 | No n = 133 | LC n = 127 | RC n = 43 | |
| EN BLOC RESECTION 70/170 (41%) | 64/120 (53%) | 6/50 (12%) | 12/37 (32%) | 58/133 (44%) | 49/127 (39%) | 21/43 (49%) |
| p < 0.001; OR 0.114, 95% CI 0.044–0.293 | p = 0.107; OR 0.509, 95% CI 0.224–1.156 | p = 0.900; OR 0.953, 95% CI 0.449–2.021 | ||||
LC: left colon; RC: right colon; OR: odds ratio; CI: confidence interval.
Analysis showed that of the 120 polyps that were 20–50 mm in size, 64/120(53%) were resected en bloc. Of the 50 polyps that were >50 mm in size, only 6 of 50 (12%) were resected en bloc. Size was a significant (p < 0.001; odds ratio (OR) 0.114, 95% confidence interval (CI) 0.044–0.293) predictor of achieving en bloc resection. The site of the polyp in the colon and the presence of fibrosis in the polyp did not significantly predict en bloc resection.
Histology
Of the 170 polyps, there were 137 (80.5%) adenomas and 20 (12%) sessile serrated polyps. 3 (1.7%) lesions were reported as DALMS and 10 (6%) were adenocarcinomas. Of the 10 patients with adenocarcinomas, 6 went on to have surgery and the other 4 continued with endoscopic follow-up.
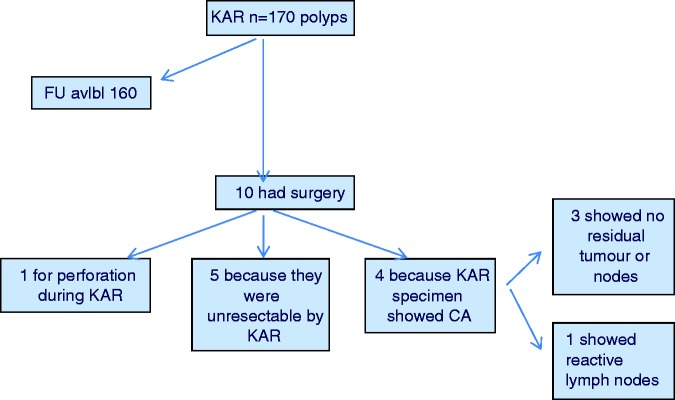
Follow-up data
Follow up data were available for 160 out of 170 patients. The remaining 10 had surgery (see Figure 2 for details). Patients had a mean follow-up of 31.5 months (range 12–84 months). The overall recurrence rate in our series was 13.1% (21 out of 160). Table 3 shows the factors associated with recurrence.
Figure 2.
Patient outcomes after KAR.
KAR: knife-assisted snare resection; FU: follow-up; CA: cancer.
Table 3.
Factors associated with recurrence. Multivariate analysis
| SIZE |
FIBROSIS |
SITE |
RESECTION TYPE |
|||||
|---|---|---|---|---|---|---|---|---|
| 20–50 mm | >50 mm | Yes | No | LC | RC | En bloc | Piecemeal | |
| RECURRENCE 21/160 (13.1%) | 9/116 (7.7%) | 12/44 (27%) | 9/33 (27%) | 12/127 (9.4%) | 18/118 (15.2%) | 3/42 (7%) | 3/69 (4.3%) | 18/91 (19.7%) |
| p = 0.008; OR 5.03, 95% CI 1.54–16.48 | p = 0.002; OR 6.59, 95% CI 1.97–22.07 | p = 0.319; OR 2.08, CI 0.492–8.78 | p < 0.001; OR 0.31, 95% CI 0.078–1.12 | |||||
LC: left colon; RC: right colon; OR: odds ratio; CI: confidence interval.
The overall complication rate in our series was 8.2% (14 out of 170). Table 4 shows an analysis of factors affecting complication rates. The occurrence of complications was not significantly associated with the size of the polyp, the presence of fibrosis, the site of resection (left colon vs. right colon) or the type of resection (en bloc vs. piecemeal).
Table 4.
Factors associated with complications
| COMPLICATIONS | SIZE |
FIBROSIS |
SITE |
RESECTION TYPE |
||||
|---|---|---|---|---|---|---|---|---|
| 20–50 mm | >50 mm | Yes | No | LC | RC | En bloc | Piecemeal | |
| BLEEDING 8/170 (4.7%) | 7/120 (5.8%) | 1/50 (2%) | 1/37 (2.7%) | 7/133 (5.3%) | 6/127 (4.7%) | 2/43 (4.6%) | 5/70 (7.1%) | 3/100 (3%) |
| PERFORATION 2/170 (1.2%) | 2/120 (1.6%) | 0/50 (0%) | 1/37 (2.7%) | 1/133 (0.7%) | 2/127 (1.6%) | 0/43 (0%) | 1/70 (1.4%) | 1/100 (1%) |
| PPS 4/170 (2.3%) | 2/120 (1.6%) | 2/50 (4%) | 1/37 (2.7%) | 3/133 (2.2%) | 4/127 (3.1%) | 0/43 (0%) | 0/70 (0%) | 4/100 (4%) |
| TOTAL 14/170 (8.2%) | 11/120 (9.1%) | 3/50 (6%) | 3/37 (8.1%) | 11/133 (8.3%) | 12/127 (9.4%) | 2/43 (4.6%) | 6/70 (8.6%) | 8/100 (8%) |
| p = 0.73 | p = 0.34 | p = 0.19 | p = 0.75 | |||||
LC: left colon; RC: right colon; PPS: post-polypectomy syndrome.
The overall perforation rate was 1.2% (2 out of 170). The first perforation occurred in the first year of the start of the service and required surgery, but the second perforation was managed endoscopically without the need for surgery. Significant bleeding was seen in 8 of 170 (4.7%) patients with 3 patients requiring blood transfusion. There were 4 cases (2.3%) of PPS. They were all managed with a brief course of antibiotics and hospital admission for two to three days.
Overall cure rate
Complete endoscopic cure (as assessed by visual inspection and confirmed by histology) was achieved in 139/160 (87%) patients after a single attempt with KAR. This improved to 95.6% (153/160) with further attempts.
Predictors of clinical success
Polyp size >50 mm (p = 0.008; OR 5.03, 95% CI 1.54–16.48), the presence of fibrosis (p = 0.002; OR 6.59, 95% CI 1.97–22.07) and piecemeal polyp resection (p < 0.001; OR 0.31, CI 0.078–1.12) were found to be independent predictors of recurrence on multivariate analysis. On analysis of polyps 20–50 mm in size without fibrosis, the recurrence rate was found to be 3.4%.
One of the aims of KAR was to achieve en bloc resection. We used this as a surrogate marker for the learning curve. This analysis was restricted to polyps <50 mm and without fibrosis. We found a distinct learning curve effect on the outcome. The en bloc resection rate improved from 33% to 77% as the cumulative experience grew from the first 41 procedures to 90 procedures (Figure 3).
Figure 3.
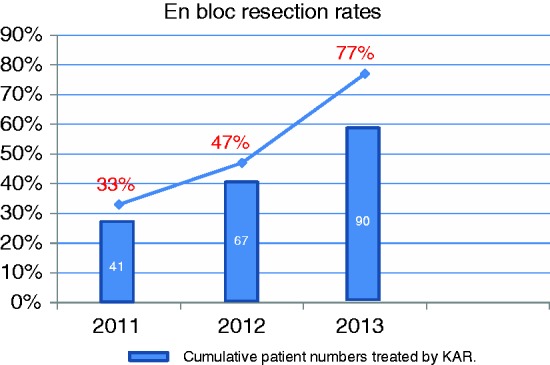
En bloc resection rates and numbers of patients treated.
Cumulative patient numbers treated by knife-assisted snare resection (KAR).
Discussion
This is the largest reported series demonstrating the feasibility, safety and efficacy of KAR for the resection of large and refractory colonic polyps in the Western setting. Our study has identified the predictors of good outcomes with KAR and has thrown light on the learning curve in a Western setting.
Colonic ESD remains challenging even in Japanese hands, and the Japanese government’s medical insurance system limits colorectal ESD to a maximum size of 2–5 cm and no larger.11 Twenty-nine per cent of the polyps in our series were larger than this size. We believe that conventional EMR in these polyps would have resulted in high recurrence rates of up to 20%–50% as reported in other Western series.12,13 Full ESD in the Western setting would have resulted in very high complication rates as reported in the French series.14
The polyps included in this series were all tertiary referrals from other endoscopists who could not resect them due to the size (20–170 mm), difficult access, flat morphology or extensive scarring and fibrosis (22% of the cases). These can be referred to as large and refractory polyps and we believe that this novel technique achieved very good outcomes with cure rates of 86% at the first attempt and rising to 95% after further attempts.
Our data show that KAR can achieve en bloc resection rates of 53% in polyps <50 mm in size. When en bloc resection was achieved, the recurrence rates were 4.3%, which are not dissimilar to the large ESD series from Japan.10 We believe that KAR has the potential to become a new standard for the treatment of flat polyps 20–50 mm in size in the Western setting.
The overall complication rate in our series was 8.8%, similar to published complication rates of Western EMR.15–20 Our perforation rate was only 1.2%, compared to the reported perforation rates of 10%–20% for ESD in the West10 and 4%–6% for ESD in Japan.4,21 Only one patient needed surgical intervention and that happened in the first year of the introduction of the technique. Apart from this case, all other complications were managed conservatively. The complication rate was not dependent on the size, fibrosis or location of the polyp.
We believe that our findings could form the basis for Western guidelines on the type of polyps for which KAR can achieve very good outcomes without the need for full ESD. KAR as a technique harnesses the best outcome features of both EMR and ESD, while avoiding the major problems associated with both these techniques.
The en bloc resection rate remains the best surrogate marker of the efficacy of this technique, as it is a significant independent negative predictor of recurrence. Our data show that the en bloc resection rate shows a linear increase and reaches almost 80% as the cumulative experience of the endoscopist approaches 100 cases. This clearly demonstrates a learning curve effect. This is the first study to throw light on the learning curve in the Western setting. These data should help in setting future training and service delivery standards in the West.
There are certain limitations to our study design. This was a single-centre cohort study where lesion selection was based on the endoscopist’s judgement; the data therefore reflect the outcomes of normal clinical practice. No comparison with EMR or ESD was performed and therefore we cannot comment on the superiority or inferiority of KAR vs. EMR or ESD. The strength of our study is the large number of patients included in these data and that these procedures were performed in a Western setting by a Western endoscopist involving polyps of all sizes and locations.
Conclusions
This is the largest reported Western series on KAR in the colon. We have demonstrated the feasibility, efficacy and safety of this technique for polyps of all sizes, with or without scarring and at all sites.
We have also managed to identify significant outcome predictors and define the learning curve. This can inform future standards of training and practice in the Western setting.
Acknowledgements
Author contributions are as follows: Bhattacharyya: Study design; analysis and interpretation of the data; literature review; drafting of the article; critical revision of the article, final approval of the article.
Chedgy: Analysis and interpretation of the data; literature review; drafting of the article.
Kandiah: Drafting of the article; preparation of video.
Longcroft-Wheaton: Drafting of the article, critical revision of the article, final approval of the article.
Bhandari: Conception and study design, interpretation of data, critical revision of article; final approval of the article.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
None declared.
References
- 1.Swan MP, Bourke MJ, Alexander S, et al. Large refractory colonic polyps: Is it time to change our practice? A prospective study of the clinical and economic impact of a tertiary referral colonic mucosal resection and polypectomy service (with videos). Gastrointest Endosc 2009; 70: 1128–1136. [DOI] [PubMed] [Google Scholar]
- 2.Khasab M, Eid E, Rusche M, et al. Incidence and predictors of “late” recurrences after endoscopic piecemeal resection of large sessile adenomas. Gastrointest Endosc 2009; 70: 344–349. [DOI] [PubMed] [Google Scholar]
- 3.Kedia P, Waye JD. Colon polypectomy: A review of routine and advanced techniques. J Clin Gastroenterol 2013; 47: 657–665. [DOI] [PubMed] [Google Scholar]
- 4.Niimi K, Fujishiro M, Kodashima S, et al. Long-term outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms. Endoscopy 2010; 42: 723–729. [DOI] [PubMed] [Google Scholar]
- 5.Toyonaga T, Man-i M, Fujita T, et al. Retrospective study of technical aspects and complications of endoscopic submucosal dissection for laterally spreading tumors of the colorectum. Endoscopy 2010; 42: 714–722. [DOI] [PubMed] [Google Scholar]
- 6.Terasaki M, Tanaka S, Oka S, et al. Clinical outcomes of endoscopic submucosal dissection and endoscopic mucosal resection for laterally spreading tumors larger than 20 mm. J Gastroenterol Hepatol 2012; 27: 734–740. [DOI] [PubMed] [Google Scholar]
- 7.Saito Y, Fukuzawa M, Matsuda T, et al. Clinical outcome of endoscopic submucosal dissection versus endoscopic mucosal resection of large colorectal tumors as determined by curative resection. Surg Endosc 2010; 24: 343–352. [DOI] [PubMed] [Google Scholar]
- 8.Oka S, Tanaka S, Kanao H, et al. Current status in the occurrence of postoperative bleeding, perforation and residual/local recurrence during colonoscopic treatment in Japan. Dig Endos 2010; 22: 376–380. [DOI] [PubMed] [Google Scholar]
- 9.Matsumoto A, Tanaka S, Oba S, et al. Outcome of endoscopic submucosal dissection for colorectal tumors accompanied by fibrosis. Scand J Gastroenterol 2010; 45: 1329–1337. [DOI] [PubMed] [Google Scholar]
- 10.Saito Y, Uraoka T, Yamaguchi Y, et al. A prospective, multicentre study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc 2010; 72: 1217–1225. [DOI] [PubMed] [Google Scholar]
- 11.Saito Y, Yamanda M, So E, et al. Colorectal endoscopic submucosal dissection: Technical advantages compared to endoscopic mucosal resection and minimally invasive surgery. Dig Endosc 2014; 26(Suppl 1): 52–61. [DOI] [PubMed] [Google Scholar]
- 12.Moss A, Bourke MJ, Williams SJ, et al. Endoscopic mucosal resection outcomes and prediction of submucosal cancer from advanced colonic mucosal neoplasia. Gastroenterology 2011; 140: 1909–1918. [DOI] [PubMed] [Google Scholar]
- 13.Friedland S, Banerjee S, Kochar R, et al. Outcomes of repeat colonoscopy in patients with polyps referred for surgery without biopsy-proven cancer. Gastrointest Endosc 2014; 79: 101–107. [DOI] [PubMed] [Google Scholar]
- 14.Farhat S, Chaussade S, Ponchon T, et al. Endoscopic submucosal dissection in a European setting. A multi-institutional report of a technique in development. Endoscopy 2011; 43: 664–670. [DOI] [PubMed] [Google Scholar]
- 15.Ferrara F, Luigiano C, Ghersi S, et al. Efficacy, safety and outcomes of ‘inject and cut’ endoscopic mucosal resection for large sessile and flat colorectal polyps. Digestion 2010; 82: 213–220. [DOI] [PubMed] [Google Scholar]
- 16.Church JM. Avoiding surgery in patients with colorectal polyps. Dis Colon Rectum 2003; 46: 1513–1516. [DOI] [PubMed] [Google Scholar]
- 17.Doniec JM, Löhnert MS, Schniewind B, et al. Endoscopic removal of large colorectal polyps: Prevention of unnecessary surgery? Dis Colon Rectum 2003; 46: 340–348. [DOI] [PubMed] [Google Scholar]
- 18.Katsinelos P, Kountouras J, Paroutoglou G, et al. Endoscopic mucosal resection of large sessile colorectal polyps with sub-mucosal injection of hypertonic 50 percent dextrose-epinephrine solution. Dis Colon Rectum 2006; 49: 1384–1392. [DOI] [PubMed] [Google Scholar]
- 19.Katsinelos P, Paroutoglou G, Beltsis A, et al. Endoscopic mucosal resection of lateral spreading tumors of the colon using a novel solution. Surg Laparosc Endosc Percutan Tech 2006; 16: 73–77. [DOI] [PubMed] [Google Scholar]
- 20.Longcroft-Wheaton G, Duku M, Mead R, et al. Risk stratification system for evaluation of complex polyps can predict outcomes of endoscopic mucosal resection. Dis Colon Rectum 2013; 56: 960–966. [DOI] [PubMed] [Google Scholar]
- 21.Tanaka S, Tamegai Y, Tsuda S, et al. Multicenter questionnaire survey on the current situation of colorectal endoscopic sub-mucosal dissection in Japan. Dig Endosc 2010; 22(Suppl): S2–S8. [DOI] [PubMed] [Google Scholar]