Abstract
Over the last decade, the apparent increase in placebo responses in randomized controlled trials (RCTs) of neuropathic pain have complicated and potentially limited development and availability of new effective pain medication. Placebo analgesia and nocebo hyperalgesia effects are well described in nociceptive and idiopathic pain conditions, but less is known about the magnitude and mechanisms of placebo and nocebo effects in neuropathic pain. In neuropathic pain, placebo treatments have primarily been used as control conditions for active agents under investigation in RCTs and these placebo responses are typically not controlled for the natural history of pain and other confounding factors. Recently, mechanistic studies that control for the natural history of pain have investigated placebo and nocebo effects in neuropathic pain in their own right. Large placebo analgesia but no nocebo hyperalgesic effects have been found, and the underlying mechanisms are beginning to be elucidated. Here we review placebo and nocebo effects and the underlying mechanisms in neuropathic pain and compare them with those of nociceptive and idiopathic pain. This allows for a novel discussion on how knowledge of psychological, neurobiological, and genetic factors underlying well-controlled placebo effects may help improve the information that can be obtained from and potentially restore the utility of RCTs.
Keywords: Placebo analgesia, Nocebo hyperalgesia, Neuropathic pain, Randomized controlled trial
1. Introduction
1.1. Background
Most placebo analgesia and nocebo hyperalgesia studies have been carried out in healthy volunteers exposed to experimental pain stimuli1–4 or in patients suffering from acute postoperative pain,5–8 both of which describe pain arising from direct activation of nociceptors, ie, nociceptive pain.9 Although a few studies of placebo and nocebo effects have been carried out in patients with chronic pain,10–15 these studies have primarily involved patients with irritable bowel syndrome where the underlying pathophysiology is unclear (eg, Refs. 16,17), ie, idiopathic pain.18,19 Hence, although placebo and nocebo effects are well-described in nociceptive and idiopathic pain, it is unknown to what extent the findings apply to neuropathic pain where pain arises as a direct consequence of a lesion or disease affecting the somatosensory system.20 In neuropathic pain, placebos have primarily been used as controls for active medications under study in randomized controlled trials (RCTs; see eg, references in Ref. 21). In these trials, the natural history of the pain is not controlled for and therefore it is difficult to deduce whether the response following placebo administration is due to placebo factors or bias.
During the last decade, the magnitude of the placebo response seems to have increased in nociceptive and neuropathic RCTs,22 thereby making it difficult to show an effect of supposedly new active medication over placebo and even get approval of medications previously approved.23 Several attempts have been made to overcome this problem, such as eliminating placebo responders via enriched design or placebo run in phases, but in general, they have not been successful.24 Knowledge of underlying placebo mechanisms may help improve the information that can be obtained from RCTs.24–26
This is, to our knowledge, the first article to review the emerging literature on well-controlled placebo and nocebo effects in neuropathic pain and to compare the findings with knowledge of placebo and nocebo effects in nociceptive and idiopathic pain. Furthermore, we discuss how the knowledge of psychological, neurobiological, and genetic mechanisms underlying placebo and nocebo effects may help improve the information that can be obtained from RCTs and potentially improve development of pain medication and optimize treatment in clinical practice.
1.2. Definitions
As pain levels fluctuate over time, it is important to differentiate between the natural history of the pain (Fig. 1A), the placebo response (Fig. 1B), and the placebo effect (Fig. 1C).27 Despite several attempts to create consensus definitions, the terms placebo response and placebo effect are used interchangeably in the literature.26 Placebos are inactive agents, such as sugar pills or saline injections. In clinical trials, where the aim is to use placebo treatment as a control condition for the active medication under study, the placebo response refers to the change in a symptom following administration of an inert placebo agent.27 The placebo response is typically not compared to the effect of a no-treatment control arm, and therefore, the response to the placebo treatment cannot be separated from confounding factors such as changes in the natural history of pain.27,28
Figure 1.
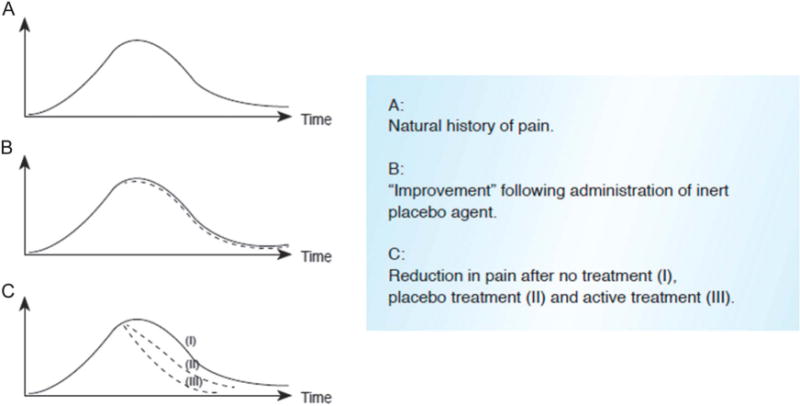
Natural history of the pain (A), the placebo response (B), and the placebo effect (C).
In placebo mechanistic studies, however, where the purpose is to investigate the mechanisms underlying placebo effects, the placebo effect is generally calculated as the “measured difference in pain across an untreated and a placebo-treated group or across an untreated and placebo treated condition within the same group (as in cross over studies).”4,29 Thus, the natural history of pain and other confounding factors are controlled for in the estimate of the placebo effect, which thus conveys changes in pain due to the placebo intervention27,28 (Fig. 1C).
Conceptually, the placebo effect has been related to the social context28 and meaning associated with the treatment.30 More specifically, the placebo effect is derived from the participants’ perception and experience of receiving a pain-reducing treatment, ie, seeing, smelling, and hearing verbal information about the treatment as well as the integration of this sensory information with memories of previous experiences and current expectations.26,29
The term nocebo effect was originally coined to describe the negative side effects of a placebo treatment and the term may still be used in that manner.31–33 However, today the nocebo effect is primarily conceptualized as an independent phenomenon that mirrors the placebo effect.28,34 Accordingly, the nocebo effect is seen as the effect that follows the administration of an inert treatment along with behavioral procedures and/or verbal suggestions that tend to worsen symptoms. When patients expect to feel worse, they eventually tend to do so.34
It is important to be aware that the perception of receiving a treatment does not only contribute to the efficacy of inert treatments but also to the efficacy of active treatment.13,28 Thus, more recently, the placebo and nocebo component of a treatment has also been investigated in relation to placebo or nocebo-like effects where an active pain medication is given without the patients’ knowledge (hidden) to test the pharmacological effect of the drug or in full view of the patients (open) to test the pharmacological effect plus the placebo effect.1,5,8
2. Magnitude and mechanisms of placebo and nocebo effects
2.1. The magnitude of placebo and nocebo effects
2.1.1. Placebo effects
The magnitude of well-controlled placebo analgesia effects has been shown to be highly variable.29,35,36 Yet, in placebo mechanism studies, the average placebo analgesia effect in nociceptive and idiopathic pain conditions is large as indicated by a Cohen’s d above 0.8.29,36 Numerous studies have tested uncontrolled placebo responses in RCTs of neuropathic pain (see eg, references in Ref. 21), but, to our knowledge, only 2 studies have directly investigated well-controlled placebo effects in neuropathic pain.37,38
Petersen et al.37,38 exposed patients who had developed chronic neuropathic pain following thoracotomy to a placebo manipulation by an open vs hidden administration of lidocaine and a natural history no-treatment control. Outcomes were evaluated using quantitative sensory testing in an area close to the surgery site. In the studies, patients went through 3 randomized sessions: open administration of lidocaine, hidden administration of lidocaine, and no treatment (Fig. 2).37,38 The open vs hidden administration was made possible by a disinfection napkin, which is typically used in quantitative sensory testing studies to disinfect the testing area. In the open condition, lidocaine was applied to the disinfection napkin in full view of the patients, and the patients were told: “The agent you have just been given is known to powerfully reduce pain in some patients.” In the hidden condition, lidocaine was applied to the disinfection napkin without the patients’ knowledge and the patients were told: “This is a control condition for the active medication.” In the control condition, patients were not given any medication on the disinfection napkin and they were told: “We will test your response to different types of stimuli in order to get a better understanding of how (your) pain is processed.” In each session or condition, the patients’ spontaneous pain levels were measured and evoked pain like brush, wind-up-like pain, and area of hyperalgesia were assessed.37,38
Figure 2.
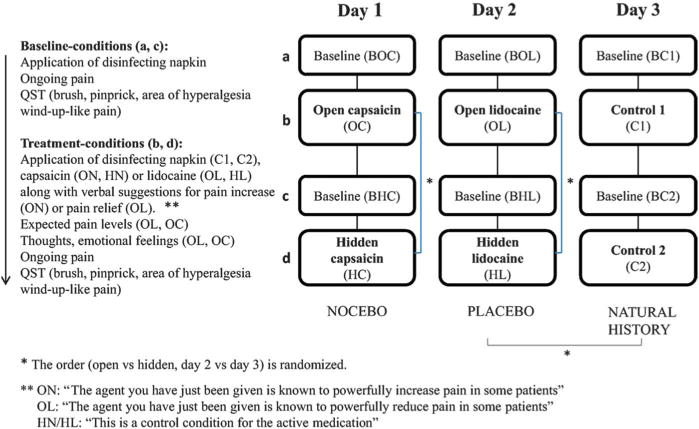
Design.
As long as patients experienced spontaneous pain levels of at least 3 on a 0 to 10 numerical rating scale at the time of testing, large and significant placebo effects were observed on ongoing pain.37 Also large and significant placebo effects were seen on wind-up-like pain37 and area of hyperalgesia38 (Figs. 3A–C and 4). Like findings on nociceptive and idiopathic pain, the effect sizes of the placebo effects in neuropathic pain were above a Cohen’s d of 0.8 (Cohen’s d = 1.01, 1.63, and 2.01, respectively).37
Figure 3.
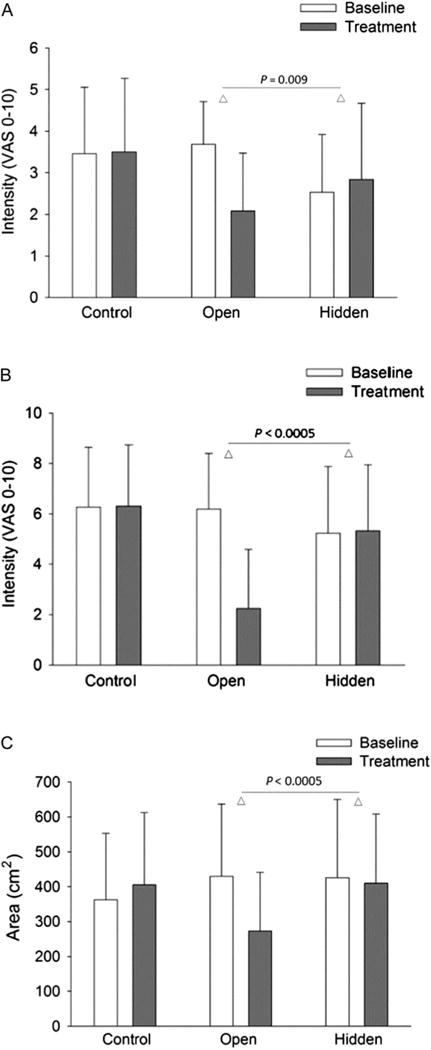
Placebo effect on (A) ongoing pain, (B) wind-up-like pain, and (C) area of hyperalgesia.
Figure 4.
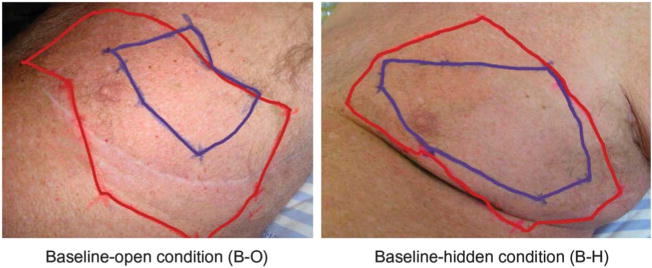
Picture of the placebo effect on area of hyperalgesia.
Interestingly, these findings show that placebo effects exert inhibitory effects on 3 measures that are likely to be associated with hyperalgesia and central sensitization: (1) maximum windup-like pain intensity, (2) area of secondary hyperalgesia, and (3) ongoing clinical pain.39–41 Previous studies have suggested that wind-up and central sensitization are related to secondary hyperalgesia40 and help maintain ongoing clinical pain.39–43 These results add to the increasing evidence that at least some forms of placebo analgesia reflect antihyperalgesic mechanisms.4,13,14,38
2.1.2. Nocebo effects
The magnitude of well-controlled nocebo hyperalgesic effects in nociceptive and idiopathic pain is moderate to large as indicated by Cohen’s d around 0.65 to 1.07.34 So far, only one study has directly investigated well-controlled nocebo effects in neuropathic pain.
In the study by Petersen et al.,37 patients with neuropathic pain also received open and hidden administration of capsaicin via the disinfection napkin in dosages that had previously been shown to increase pain. A no-treatment control was also included in the study. In the open condition, capsaicin was administered to the disinfection napkin in full view of the patients, who were told: “The agent you have just been given is known to powerfully increase pain in some patients.” The hidden and control condition followed the same procedure as the placebo intervention (see above). No nocebo effects were obtained in spontaneous pain or any of the evoked pain measures. The lack of a nocebo effect in this study was perhaps due to the intervention not being sufficiently negative (eg, frightening, unpleasant) or painful (for further discussion see below). It should, however, be noted that in the few studies investigating the nocebo effect in chronic pain patients in a hospital setting the nocebo effect has also been non-significant.13,37,44 Whether this is due to methodological issues or to patients generally not feeling frightened in a well-defined test setting at a hospital has yet to be elucidated. Still, adverse events have consistently been reported in studies of chronic pain patients, including patients with neuropathic pain,31,33 and although these studies are not controlled for the natural history of the pain, they indicate that negative outcomes are indeed likely to contribute to the overall treatment outcome.
2.2. The contribution of psychological factors
2.2.1. Placebo effects
Expected pain levels and emotional feelings, such as reduced anxiety and the experience of relief (reward), have been shown to contribute to placebo effects in nociceptive and idiopathic pain conditions.4,14,45–49 In the neuropathic placebo mechanisms studies outlined above, patients’ expected pain levels and emotional feelings were assessed immediately after the disinfection napkin was applied and before the potential administration of lidocaine had taken effect.37,38 In the second study,37 measures of expected pain levels were specifically targeted at each pain measure by asking: “What do you expect your pain level to be” in relation to spontaneous pain and each of the evoked pain measures (brush, pinprick, area of hyperalgesia, wind-up-like pain). With respect to the area of hyperalgesia, patients were asked: “Do you expect your area of hyperalgesia to be the same, larger, or smaller than before (ie, compared with baseline).” Patients were also asked to rate the intensity of emotional feelings on a 0 to 10 visual analogue scale and to qualitatively describe these emotions.50
The placebo effects on spontaneous pain, areas of hyperalgesia, and wind-up-like pain were related to the expected pain levels that accounted for between 24% and 53% of the variance in pain levels following the open administration of lidocaine.37 Also, patients reported a much higher intensity of positive (6.97) than negative emotions (0.34) following the open administration of lidocaine (Fig. 5A), and in general, they expressed “Hope that the cream will bring relief.”
Figure 5.
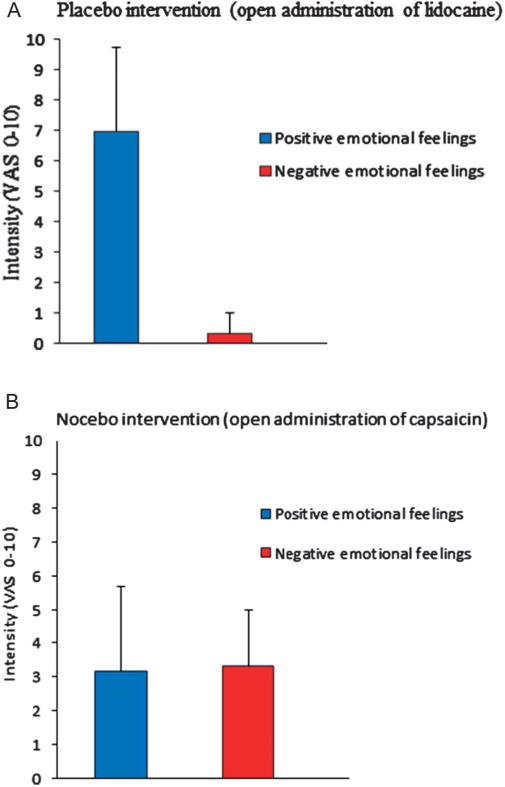
Emotional feelings in (A) placebo and (B) nocebo conditions.
2.2.2. Nocebo effects
Expected pain levels and increase in negative emotions like anxiety have been associated with nocebo hyperalgesic effects in nociceptive pain conditions.28,51,52 In the well-controlled study of nocebo effects in neuropathic pain outlined above, expectations and emotional feelings were also measured. During the nocebo intervention (open capsaicin), patients reported a similar intensity of negative (3.3) and positive (3.2) emotional feelings (Fig. 5B). Hence, patients reported higher intensity of negative emotional feelings during the nocebo intervention compared to the placebo intervention, but the intensity of positive emotional feelings was still high during the nocebo intervention, which may indicate that the nocebo intervention was not sufficiently adversive for patients to develop negative emotional feelings and thereby experience nocebo effects.
Overall, patients’ expectations and emotional feelings during the nocebo intervention were different from those observed during the placebo intervention, where patients expected lower pain levels and high levels of positive and low levels of negative emotional feelings. These finding are consistent with the literature on nociceptive and idiopathic placebo and nocebo effects, indicating that placebo and nocebo interventions are related to different psychological profiles. This further emphasizes that psychological factors contribute to placebo and nocebo effects in neuropathic pain. Also, it illustrates that patients’ expectations of a treatment effect are not neutral but embedded in emotional feelings that may be especially important to consider when treating patients with chronic pain.
2.3. The contribution of neurobiological and genetic factors
2.3.1. Placebo effects
In nociceptive and idiopathic pain, expected pain intensity and emotional feelings of relief (reward) have been related to the placebo analgesia effect4,45–49 and to enhanced or altered activity in areas of the brain known to be involved in reward or aversion, emotion, and classical descending pain inhibitory pathways.53–56 The latter includes core rACC-amygdala-PAG-rostroventral medulla–spinal cord connection, and one study has directly shown reduced neural activity in the spinal cord during placebo analgesia in nociceptive pain.57 The neurobiological mechanisms underlying placebo effects in neuropathic pain have still to be elucidated. Although the antihyperalgesic placebo effects in neuropathic pain (cf section 2.1.1.) could be mediated by several possible mechanisms, an efficient one might include inhibition of dorsal horn neurons that are sensitized.37
Even though the pathophysiology of neuropathic pain is distinct from nociceptive and idiopathic pain, opioid and dopamine signaling represent key overlapping molecular pathways involved in pain relief.58 In neuroimaging studies of brain activity during placebo-induced analgesia, the expectation of benefit has been shown to activate opioid and dopamine neurotransmission in brain regions associated with pain, reward, and affect, including the prefrontal cortex, rostral anterior cingulate, insula, nucleus accumbens, amygdala, thalamus, hypothalamus, and periaqueductal gray.59–61 The magnitude of these changes in neurotransmission has been correlated with level of placebo analgesia reported. The magnitude of the placebo analgesia effect is highly variable (cf above), and unsurprisingly genetic variation in opioid and dopamine metabolic and regulatory genes has been shown to modify the placebo effect in nociceptive and idiopathic pain.62
Interestingly, the catechol-O-methyltransferase (COMT) gene that was shown to be associated with nociceptive63 and neuropathic pain sensitivity64,65 is emerging as a locus in placebo genetics. The COMT metabolizes and thus regulates the activity of catecholamine neurotransmitters epinephrine, norepinephrine, and dopamine. The well-studied COMT val158met polymorphism that modifies the activity of COMT and inversely the levels of dopamine in the prefrontal cortex66 has been shown to modify the placebo effect in idiopathic67 and nociceptive pain.68 Likewise genetic variation in the genes encoding the mu-opioid receptor (OPRM1)69 and fatty acid amide hydrolase (FAAH),70 an enzyme that degrades endocannabinoids, was also shown to be associated with changes in analgesia and more positive affective states after placebo treatment.
Further insights into the mechanisms underlying placebo effects in pain come from the pharmacological effect of drugs that interact with the neurotransmitters involved in the molecular placebo pathway. The dopaminergic antagonist haloperidol did not block the placebo analgesia effect in nociceptive pain in a recent study.71 Yet, the mu-opioid receptor antagonist naloxone has been shown to block placebo-induced analgesia in nociceptive pain.8,28,72 Cholecystokinin (CCK) blocks opioid signaling, and the CCK antagonist proglumide has been shown to enhance placebo-induced analgesia. The endocannabinoid antagonist remifentanil was shown to block non-opioid–mediated placebo effects, thereby indicating that the endocannabinoid system may also be involved in placebo analgesia effects in nociceptive pain.73,74
Recent studies have examined the effect of neuropeptides oxytocin and vasopressin on placebo analgesia in nociceptive pain. Intranasally administered oxytocin was shown to enhance placebo analgesia.75 The authors speculate that oxytocin effects on empathy and trust may have enhanced the believability of the study physician although its anxiolytic effects could have increased response to the placebo treatment. These findings are in agreement with studies showing that psychological traits, such as empathy, dispositional optimism, and altruism, may be linked to placebo effects.76 Another study found that vasopressin (a neuropeptide involved in regulating water retention and arterial blood flow) as well as social cues and interpersonal interactions enhanced placebo analgesia.77 Still, the involvement of these neurotransmitter systems in neuropathic placebo effects has yet to be investigated.
2.3.2. Nocebo effects
In nociceptive pain, brain imaging studies have shown increased activity in pain-processing areas during nocebo hyperalgesia,3,52,78 and neurotransmitter studies have documented release of the opioid agonist CCK during nocebo hyperalgesia.2,79 A recent genetic study furthermore found that genetic variation in COMT also influenced nocebo and complaint reporting such that the COMT high-activity homozygotes, which were the placebo nonresponders, tended to be more sensitive to nocebo80 and reported more complaints.81 Thus, also at the neural level, nocebo hyperalgesia effects seem to exert effects opposite to placebo analgesia.
3. Discussion
3.1. The magnitude of the placebo response in randomized controlled trials
The apparent increase in the magnitude of the placebo response in nociceptive and neuropathic pain trials22 has led to a renewed focus on the placebo response and on assay sensitivity, ie, the ability of a clinical trial to distinguish an effective treatment from a less effective or ineffective treatment.23 One of the basic assumptions in RCTs is the additivity assumption, where the effect of the placebo agent and the effect of the active agent are assumed to be additive. In other words, the efficacy of the active medication can be deduced by subtracting the pain outcome in the placebo arm from the active treatment arm. Recent studies and meta-analyses have challenged the additivity assumption in so far as the drug effect plus the placebo effect may be larger than the total treatment effect, especially for high placebo responders.62,82,83 One strategy to reduce the placebo response is to eliminate placebo responders by enriched design or placebo run in phases.24 Although the studies were designed to minimize the placebo response, they did not always do so.24,84 Furthermore, some studies suggest that participants with the highest drug response also tend to have the highest placebo response.85 Hence, eliminating the placebo response may not be the optimum solution for improving RCTs.
3.2. Prediction of the placebo response
Alternatively, knowledge of the psychological, neurobiological, and genetic factors that influence the magnitude of well-controlled placebo effects may guide the development of new strategies to manage this problem in RCTs. From the placebo literature, it is well-known that expected pain levels and emotional feelings influence the placebo effect, but in RCTs, these factors are typically not addressed. Still, based on the design of the clinical trial, it maybe possible to propose potential expectancy predictors of the placebo response, such as information about the type of active medication being tested (opioid vs non-opioid), randomization ratio (1:1 vs 4:1), and number and quality of interactions with the health care provider; assuming that opioid treatment, a higher randomization ratio of active over placebo and a higher number of interactions with the health care provider would lead to higher expectations of treatment efficacy and hence a higher placebo response.26,31,86–90 Such an approach has been examined in a meta-analysis of individual placebo data from 2017 patients suffering from chronic nociceptive pain participating in trials sponsored by the pharmaceutical industry (see futher details in Ref. 91). Opioid trials and high number of face-to-face visits was found to be related to a higher placebo response, thereby supporting the expectancy hypothesis. Higher randomization ratio in favor of active over placebo was, however, not related to larger placebo responses.91
In general, explorative analyses testing if patient and study characteristics predicted the placebo response found no support for such an association.91 This is consistent with the variability in the placebo effect and with the importance of assessing specific expectations and emotional feelings. In other words, placebo responding does not seem to be easily explained by for example a “placebo responder personality” or single study designs. Yet, in the explorative analysis, higher baseline pain intensity, age, long washout periods, and discontinuation due to adverse events were significantly related to a higher placebo response. The findings in relation to baseline pain levels indicate that high placebo responses may at least in part be due to regression to the mean and other factors that are unrelated to placebo effects controlled for the natural history of pain (cf above). The finding on adverse events is interesting because it suggest that patients who discontinue due to adverse events may think they have received the active agent. It is well-known that patients experience adverse events in the placebo arm of a trial even though typically to a lower extent than in the active arm.33 Although most RCTs are set up to be double blind, they are often unblinded by, for example, the experience of adverse events,24,91 so to understand the factors that influence the placebo response of a trial, it will be important to test patients’ specific expectations and to test whether the trial was indeed double blind. This can be done by asking patients about their expected pain levels and by asking them which treatment they believe they have received. Such an approach may be helpful in understanding and predicting the magnitude of the placebo response in nociceptive and neuropathic pain conditions in order to understand the magnitude of the response that is due to placebo factors as opposed to confounding factors like spontaneous remission.
In addition, the potential for placebo gene–drug interactions is an important consideration in evaluating the placebo response in neuropathic pain because it raises the possibility that other drugs which target the neurotransmitter pathways involved in pain may also influence the component of the drug response that is attributed to the placebo response.62 Furthermore, this component of the drug response attributed to the placebo response may not always be additive and may vary as a function of individual genotype.
4. Summary
Large placebo analgesia effects exist in neuropathic pain (Cohen’s d > 0.8), and knowledge of the underlying mechanisms may help improve overall treatment outcome in clinical practice and potentially improve the information that can be obtained from RCTs. First, by including a no-treatment condition in RCTs, it will be possible to differentiate between the changes in pain levels that are due to the placebo phenomenon and the changes that arise from confounding factors, such as regression to the mean. Ethical challenges may be met by subsequently offering the no-treatment control group the active treatment under study, ie, a wait-list control. Second, by adding 2 simple questions to RCTs: (1) What do you expect your pain levels to be? (2) Which treatment do you think that you received (active or placebo)? it may be possible to test to what extent blinding is maintained and it may also be possible to explain the variance of the placebo response to a higher extent. Third, by genotyping patients it may be possible to better understand how the pain condition and gene–drug interaction may influence placebo and treatment responses. Ultimately, knowledge of placebo mechanisms may help improve the approval of new analgesics and optimize the treatment of patients in clinical practice.
Acknowledgments
The work mentioned in this article was part of the Europain Collaboration and funded by the Innovative Medicines Initiative Joint Undertaking (IMI JU) Grant No 115007, resources which are composed of financial contributions from the European Union’s Seventh Framework Program (FP7/2007-2013) and EFPIA companies in kind contribution (www.imi.europa.eu).
Footnotes
Conflict of interest statement
The authors have no conflicts of interest to declare.
References
- 1.Benedetti F. Mechanisms of placebo and placebo-related effects across diseases and treatments. Annu Rev Pharmacol Toxicol. 2008;48:33–60. doi: 10.1146/annurev.pharmtox.48.113006.094711. [DOI] [PubMed] [Google Scholar]
- 2.Benedetti F, Amanzio M, Vighetti S, Asteggiano G. The biochemical and neuroendocrine bases of the hyperalgesic nocebo effect. J Neurosci. 2006;26:12014–22. doi: 10.1523/JNEUROSCI.2947-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kong J, Gollub RL, Polich G, Kirsch I, Laviolette P, Vangel M, Rosen B, Kaptchuk TJ. A functional magnetic resonance imaging study on the neural mechanisms of hyperalgesic nocebo effect. J Neurosci. 2008;28:13354–62. doi: 10.1523/JNEUROSCI.2944-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Price DD, Finniss DG, Benedetti F. A comprehensive review of the placebo effect: recent advances and current thought. Annu Rev Psychol. 2008;59:565–90. doi: 10.1146/annurev.psych.59.113006.095941. [DOI] [PubMed] [Google Scholar]
- 5.Amanzio M, Pollo A, Maggi G, Benedetti F. Response variability to analgesics: a role for non-specific activation of endogenous opioids. PAIN. 2001;90:205–15. doi: 10.1016/S0304-3959(00)00486-3. [DOI] [PubMed] [Google Scholar]
- 6.Benedetti F, Pollo A, Lopiano L, Lanotte M, Vighetti S, Rainero I. Conscious expectation and unconscious conditioning in analgesic, motor, and hormonal placebo/nocebo responses. J Neurosci. 2003;23:4315–23. doi: 10.1523/JNEUROSCI.23-10-04315.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levine JD, Gordon NC. Influence of the method of drug administration on analgesic response. Nature. 1984;312:755–6. doi: 10.1038/312755a0. [DOI] [PubMed] [Google Scholar]
- 8.Levine JD, Gordon NC, Fields HL. The mechanism of placebo analgesia. Lancet. 1978;2:654–7. doi: 10.1016/s0140-6736(78)92762-9. [DOI] [PubMed] [Google Scholar]
- 9.Loeser JD, Treede RD. The Kyoto protocol of IASP Basic Pain Terminology. PAIN. 2008;137:473–7. doi: 10.1016/j.pain.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 10.Craggs JG, Price DD, Verne GN, Perlstein WM, Robinson MM. Functional brain interactions that serve cognitive-affective processing during pain and placebo analgesia. Neuroimage. 2007;38:720–9. doi: 10.1016/j.neuroimage.2007.07.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaptchuk TJ, Friedlander E, Kelley JM, Sanchez MN, Kokkotou E, Singer JP, Kowalczykowski M, Miller FG, Kirsch I, Lembo AJ. Placebos without deception: a randomized controlled trial in irritable bowel syndrome. PLoS One. 2010;5:e15591. doi: 10.1371/journal.pone.0015591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Price DD, Craggs J, Verne GN, Perlstein WM, Robinson ME. Placebo analgesia is accompanied by large reductions in pain-related brain activity in irritable bowel syndrome patients. PAIN. 2007;127:63–72. doi: 10.1016/j.pain.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 13.Vase L, Robinson ME, Verne GN, Price DD. The contributions of suggestion, desire, and expectation to placebo effects in irritable bowel syndrome patients. An empirical investigation. PAIN. 2003;105:17–25. doi: 10.1016/s0304-3959(03)00073-3. [DOI] [PubMed] [Google Scholar]
- 14.Vase L, Robinson ME, Verne GN, Price DD. Increased placebo analgesia over time in irritable bowel syndrome (IBS) patients is associated with desire and expectation but not endogenous opioid mechanisms. PAIN. 2005;115:338–47. doi: 10.1016/j.pain.2005.03.014. [DOI] [PubMed] [Google Scholar]
- 15.Verne GN, Robinson ME, Vase L, Price DD. Reversal of visceral and cutaneous hyperalgesia by local rectal anesthesia in irritable bowel syndrome (IBS) patients. PAIN. 2003;105:223–30. doi: 10.1016/s0304-3959(03)00210-0. [DOI] [PubMed] [Google Scholar]
- 16.Kupers R, Maeyaert J, Boly M, Faymonville ME, Laureys S. Naloxone-insensitive epidural placebo analgesia in a chronic pain patient. Anesthesiology. 2007;106:1239–42. doi: 10.1097/01.anes.0000265418.68005.8a. [DOI] [PubMed] [Google Scholar]
- 17.Piche M, Bouin M, Arsenault M, Poitras P, Rainville P. Decreased pain inhibition in irritable bowel syndrome depends on altered descending modulation and higher-order brain processes. Neuroscience. 2011;195:166–75. doi: 10.1016/j.neuroscience.2011.08.040. [DOI] [PubMed] [Google Scholar]
- 18.Tirlapur SA, Priest L, Daniels JP, Khan KS. How do we define the term idiopathic? Curr Opin Obstet Gynecol. 2013;25:468–73. doi: 10.1097/GCO.0000000000000025. [DOI] [PubMed] [Google Scholar]
- 19.Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, Cohen M, Evers S, Finnerup NB, First MB, Giamberardino MA, Kaasa S, Kosek E, Lavand’homme P, Nicholas M, Perrot S, Scholz J, Schug S, Smith BH, Svensson P, Vlaeyen JW, Wang SJ. A classification of chronic pain for ICD-11. PAIN. 2015;156:1003–7. doi: 10.1097/j.pain.0000000000000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jensen TS, Baron R, Haanpaa M, Kalso E, Loeser JD, Rice AS, Treede RD. A new definition of neuropathic pain. PAIN. 2011;152:2204–5. doi: 10.1016/j.pain.2011.06.017. [DOI] [PubMed] [Google Scholar]
- 21.Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, Gilron I, Haanpaa M, Hansson P, Jensen TS, Kamerman PR, Lund K, Moore A, Raja SN, Rice AS, Rowbotham M, Sena E, Siddall P, Smith BH, Wallace M. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14:162–73. doi: 10.1016/S1474-4422(14)70251-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Häuser W, Bartram-Wunn E, Bartram C, Reinecke H, Tolle T. Systematic review: placebo response in drug trials of fibromyalgia syndrome and painful peripheral diabetic neuropathy-magnitude and patient-related predictors. PAIN. 2011;152:1709–17. doi: 10.1016/j.pain.2011.01.050. [DOI] [PubMed] [Google Scholar]
- 23.Dworkin RH, Turk DC, Peirce-Sandner S, Burke LB, Farrar JT, Gilron I, Jensen MP, Katz NP, Raja SN, Rappaport BA, Rowbotham MC, Backonja MM, Baron R, Bellamy N, Bhagwagar Z, Costello A, Cowan P, Fang WC, Hertz S, Jay GW, Junor R, Kerns RD, Kerwin R, Kopecky EA, Lissin D, Malamut R, Markman JD, McDermott MP, Munera C, Porter L, Rauschkolb C, Rice AS, Sampaio C, Skljarevski V, Sommerville K, Stacey BR, Steigerwald I, Tobias J, Trentacosti AM, Wasan AD, Wells GA, Williams J, Witter J, Ziegler D. Considerations for improving assay sensitivity in chronic pain clinical trials: IMMPACT recommendations. PAIN. 2012;153:1148–58. doi: 10.1016/j.pain.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 24.Enck P, Bingel U, Schedlowski M, Rief W. The placebo response in medicine: minimize, maximize or personalize? Nat Rev Drug Discov. 2013;12:191–204. doi: 10.1038/nrd3923. [DOI] [PubMed] [Google Scholar]
- 25.Rief W, Bingel U, Schedlowski M, Enck P. Mechanisms involved in placebo and nocebo responses and implications for drug trials. Clin Pharmacol Ther. 2011;90:722–6. doi: 10.1038/clpt.2011.204. [DOI] [PubMed] [Google Scholar]
- 26.Vase L, Amanzio M, Price DD. Nocebo vs placebo: the challenges of trial design in analgesia research. Clin Pharmacol Ther. 2015;97:143–50. doi: 10.1002/cpt.31. [DOI] [PubMed] [Google Scholar]
- 27.Kirsch I. The placebo effect revisited: lessons learned to date. Complement Ther Med. 2013;21:102–4. doi: 10.1016/j.ctim.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 28.Benedetti F. Placebo effects: understanding the mechanisms in health and disease. Second. Oxford University Press; Oxford, United Kingdom: 2014. [Google Scholar]
- 29.Vase L, Riley JL, III, Price DD. A comparison of placebo effects in clinical analgesic trials versus studies of placebo analgesia. PAIN. 2002;99:443–52. doi: 10.1016/S0304-3959(02)00205-1. [DOI] [PubMed] [Google Scholar]
- 30.Moerman DE, Jonas WB. Deconstructing the placebo effect and finding the meaning response. Ann Intern Med. 2002;136:471–6. doi: 10.7326/0003-4819-136-6-200203190-00011. [DOI] [PubMed] [Google Scholar]
- 31.Amanzio M, Corazzini LL, Vase L, Benedetti F. A systematic review of adverse events in placebo groups of anti-migraine clinical trials. PAIN. 2009;146:261–9. doi: 10.1016/j.pain.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 32.Mitsikostas DD, Mantonakis LI, Chalarakis NG. Nocebo is the enemy, not placebo. A meta-analysis of reported side effects after placebo treatment in headaches. Cephalalgia. 2011;31:550–61. doi: 10.1177/0333102410391485. [DOI] [PubMed] [Google Scholar]
- 33.Papadopoulos D, Mitsikostas DD. A meta-analytic approach to estimating nocebo effects in neuropathic pain trials. J Neurol. 2012;259:436–47. doi: 10.1007/s00415-011-6197-4. [DOI] [PubMed] [Google Scholar]
- 34.Petersen GL, Finnerup NB, Colloca L, Amanzio M, Price DD, Jensen TS, Vase L. The magnitude of nocebo effects in pain: a meta-analysis. PAIN. 2014;155:1426–34. doi: 10.1016/j.pain.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hrobjartsson A, Gotzsche PC. Is the placebo powerless? An analysis of clinical trials comparing placebo with no treatment. N Engl J Med. 2001;344:1594–602. doi: 10.1056/NEJM200105243442106. [DOI] [PubMed] [Google Scholar]
- 36.Vase L, Petersen GL, Riley JL, III, Price DD. Factors contributing to large analgesic effects in placebo mechanism studies conducted between 2002 and 2007. PAIN. 2009;145:36–44. doi: 10.1016/j.pain.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 37.Petersen GL, Finnerup NB, Grosen K, Pilegaard HK, Tracey I, Benedetti F, Price DD, Jensen TS, Vase L. Expectations and positive emotional feelings accompany reductions in ongoing and evoked neuropathic pain following placebo interventions. PAIN. 2014;155:2687–98. doi: 10.1016/j.pain.2014.09.036. [DOI] [PubMed] [Google Scholar]
- 38.Petersen GL, Finnerup NB, Norskov KN, Grosen K, Pilegaard HK, Benedetti F, Price DD, Jensen TS, Vase L. Placebo manipulations reduce hyperalgesia in neuropathic pain. PAIN. 2012;153:1292–300. doi: 10.1016/j.pain.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 39.Baron R, Hans G, Dickenson AH. Peripheral input and its importance for central sensitization. Ann Neurol. 2013;74:630–6. doi: 10.1002/ana.24017. [DOI] [PubMed] [Google Scholar]
- 40.Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009;10:895–926. doi: 10.1016/j.jpain.2009.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li J, Simone DA, Larson AA. Windup leads to characteristics of central sensitization. PAIN. 1999;79:75–82. doi: 10.1016/S0304-3959(98)00154-7. [DOI] [PubMed] [Google Scholar]
- 42.Staud R, Vierck CJ, Cannon RL, Mauderli AP, Price DD. Abnormal sensitization and temporal summation of second pain (wind-up) in patients with fibromyalgia syndrome. PAIN. 2001;91:165–75. doi: 10.1016/s0304-3959(00)00432-2. [DOI] [PubMed] [Google Scholar]
- 43.Staud R, Weyl EE, Riley JL, III, Fillingim RB. Slow temporal summation of pain for assessment of central pain sensitivity and clinical pain of fibromyalgia patients. PLoS One. 2014;9:e89086. doi: 10.1371/journal.pone.0089086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Klinger R, Schmitz J, Benson S, Elsenbruch S, Kamping S, Flor H. Schmerzreduktion durch Variation von Kontextreizen: möglichkeiten zur Selbstwirksamkeit in der Schmerztherapie? Der Schmerz. 2013;27:47–9. [Google Scholar]
- 45.De Pascalis V, Chiaradia C, Carotenuto E. The contribution of suggestibility and expectation to placebo analgesia phenomenon in an experimental setting. PAIN. 2002;96:393–402. doi: 10.1016/S0304-3959(01)00485-7. [DOI] [PubMed] [Google Scholar]
- 46.Montgomery GH, Kirsch I. Classical conditioning and the placebo effect. PAIN. 1997;72:107–13. doi: 10.1016/s0304-3959(97)00016-x. [DOI] [PubMed] [Google Scholar]
- 47.Price DD, Milling LS, Kirsch I, Duff A, Montgomery GH, Nicholls SS. An analysis of factors that contribute to the magnitude of placebo analgesia in an experimental paradigm. PAIN. 1999;83:147–56. doi: 10.1016/s0304-3959(99)00081-0. [DOI] [PubMed] [Google Scholar]
- 48.Zubieta JK, Bueller JA, Jackson LR, Scott DJ, Xu Y, Koeppe RA, Nichols TE, Stohler CS. Placebo effects mediated by endogenous opioid activity on mu-opioid receptors. J Neurosci. 2005;25:7754–62. doi: 10.1523/JNEUROSCI.0439-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zubieta JK, Yau WY, Scott DJ, Stohler CS. Belief or need? Accounting for individual variations in the neurochemistry of the placebo effect. Brain Behav Immun. 2006;20:15–26. doi: 10.1016/j.bbi.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 50.Price DD, Barrell JJ. Inner experience and neuroscience: merging both perspectives. Cambridge: MIT Press; 2012. [Google Scholar]
- 51.Colloca L, Miller FG. The nocebo effect and its relevance for clinical practice. Psychosom Med. 2011;73:598–603. doi: 10.1097/PSY.0b013e3182294a50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schmid J, Theysohn N, Gass F, Benson S, Gramsch C, Forsting M, Gizewski ER, Elsenbruch S. Neural mechanisms mediating positive and negative treatment expectations in visceral pain: a functional magnetic resonance imaging study on placebo and nocebo effects in healthy volunteers. PAIN. 2013;154:2372–80. doi: 10.1016/j.pain.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 53.Amanzio M, Benedetti F, Porro CA, Palermo S, Cauda F. Activation likelihood estimation meta-analysis of brain correlates of placebo analgesia in human experimental pain. Hum Brain Mapp. 2013;34:738–52. doi: 10.1002/hbm.21471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Büchel C, Geuter S, Sprenger C, Eippert F. Placebo analgesia: a predictive coding perspective. Neuron. 2014;81:1223–39. doi: 10.1016/j.neuron.2014.02.042. [DOI] [PubMed] [Google Scholar]
- 55.Craggs JG, Price DD, Perlstein WM, Verne GN, Robinson ME. The dynamic mechanisms of placebo induced analgesia: evidence of sustained and transient regional involvement. PAIN. 2008;139:660–9. doi: 10.1016/j.pain.2008.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Craggs JG, Price DD, Robinson ME. Enhancing the placebo response: functional magnetic resonance imaging evidence of memory and semantic processing in placebo analgesia. J Pain. 2014;15:435–46. doi: 10.1016/j.jpain.2013.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Eippert F, Finsterbusch J, Bingel U, Buchel C. Direct evidence for spinal cord involvement in placebo analgesia. Science. 2009;326:404. doi: 10.1126/science.1180142. [DOI] [PubMed] [Google Scholar]
- 58.Dib-Hajj SD, Waxman SG. Translational pain research: lessons from genetics and genomics. Sci Transl Med. 2014;6:249sr244. doi: 10.1126/scitranslmed.3007017. [DOI] [PubMed] [Google Scholar]
- 59.de la Fuente-Fernandez R, Lidstone S, Stoessl AJ. Placebo effect and dopamine release. J Neural Transm Suppl. 2006:415–18. doi: 10.1007/978-3-211-45295-0_62. [DOI] [PubMed] [Google Scholar]
- 60.Lidstone SC, Schulzer M, Dinelle K, Mak E, Sossi V, Ruth TJ, de la Fuente-Fernandez R, Phillips AG, Stoessl AJ. Effects of expectation on placebo-induced dopamine release in Parkinson disease. Arch Gen Psychiatry. 2010;67:857–65. doi: 10.1001/archgenpsychiatry.2010.88. [DOI] [PubMed] [Google Scholar]
- 61.Zubieta JK, Stohler CS. Neurobiological mechanisms of placebo responses. Ann N Y Acad Sci. 2009;1156:198–210. doi: 10.1111/j.1749-6632.2009.04424.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hall KT, Loscalzo J, Kaptchuk TJ. Genetics and the placebo effect: the placebome. Trends Mol Med. 2015;21:285–94. doi: 10.1016/j.molmed.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Diatchenko L, Nackley AG, Tchivileva IE, Shabalina SA, Maixner W. Genetic architecture of human pain perception. Trends Genet. 2007;23:605–13. doi: 10.1016/j.tig.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 64.Kambur O, Mannisto PT. Catechol-O-methyltransferase and pain. Int Rev Neurobiol. 2010;95:227–79. doi: 10.1016/B978-0-12-381326-8.00010-7. [DOI] [PubMed] [Google Scholar]
- 65.Martinez-Jauand M, Sitges C, Rodriguez V, Picornell A, Ramon M, Buskila D, Montoya P. Pain sensitivity in fibromyalgia is associated with catechol-O-methyltransferase (COMT) gene. Eur J Pain. 2013;17:16–27. doi: 10.1002/j.1532-2149.2012.00153.x. [DOI] [PubMed] [Google Scholar]
- 66.Chen Q, He G, Qin W, Chen QY, Zhao XZ, Duan SW, Liu XM, Feng GY, Xu YF, St Clair D, Li M, Wang JH, Xing YL, Shi JG, He L. Family-based association study of synapsin II and schizophrenia. Am J Hum Genet. 2004;75:873–7. doi: 10.1086/425588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hall KT, Lembo AJ, Kirsch I, Ziogas DC, Douaiher J, Jensen KB, Conboy LA, Kelley JM, Kokkotou E, Kaptchuk TJ. Catechol-O-methyltransferase val158met polymorphism predicts placebo effect in irritable bowel syndrome. PLoS One. 2012;7:e48135. doi: 10.1371/journal.pone.0048135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yu R, Gollub RL, Vangel M, Kaptchuk T, Smoller JW, Kong J. Placebo analgesia and reward processing: integrating genetics, personality, and intrinsic brain activity. Hum Brain Mapp. 2014;35:4583–93. doi: 10.1002/hbm.22496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pecina M, Love T, Stohler CS, Goldman D, Zubieta JK. Effects of the Mu opioid receptor polymorphism (OPRM1 A118G) on pain regulation, placebo effects and associated personality trait measures. Neuropsychopharmacology. 2015;40:957–65. doi: 10.1038/npp.2014.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Peciña M, Martinez-Jauand M, Hodgkinson C, Stohler CS, Goldman D, Zubieta JK. FAAH selectively influences placebo effects. Mol Psychiatry. 2014;19:385–91. doi: 10.1038/mp.2013.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wrobel N, Wiech K, Forkmann K, Ritter C, Bingel U. Haloperidol blocks dorsal striatum activity but not analgesia in a placebo paradigm. Cortex. 2014;57:60–73. doi: 10.1016/j.cortex.2014.02.023. [DOI] [PubMed] [Google Scholar]
- 72.Amanzio M, Benedetti F. Neuropharmacological dissection of placebo analgesia: expectation-activated opioid systems versus conditioning-activated specific subsystems. J Neurosci. 1999;19:484–94. doi: 10.1523/JNEUROSCI.19-01-00484.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Benedetti F, Amanzio M, Rosato R, Blanchard C. Nonopioid placebo analgesia is mediated by CB1 cannabinoid receptors. Nat Med. 2011;17:1228–30. doi: 10.1038/nm.2435. [DOI] [PubMed] [Google Scholar]
- 74.Benedetti F, Thoen W, Blanchard C, Vighetti S, Arduino C. Pain as a reward: changing the meaning of pain from negative to positive co-activates opioid and cannabinoid systems. PAIN. 2013;154:361–7. doi: 10.1016/j.pain.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 75.Kessner S, Sprenger C, Wrobel N, Wiech K, Bingel U. Effect of oxytocin on placebo analgesia: a randomized study. JAMA. 2013;310:1733–5. doi: 10.1001/jama.2013.277446. [DOI] [PubMed] [Google Scholar]
- 76.Medoff ZM, Colloca L. Placebo analgesia: understanding the mechanisms. PAIN Manag. 2015;5:89–96. doi: 10.2217/pmt.15.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Colloca L, Pine DS, Ernst M, Miller FG, Grillon C. Vasopressin boosts placebo analgesic effects in women: a randomized trial. Biol Psychiatry. 2015 doi: 10.1016/j.biopsych.2015.07.019. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bingel U, Wanigasekera V, Wiech K, Ni Mhuircheartaigh R, Lee MC, Ploner M, Tracey I. The effect of treatment expectation on drug efficacy: imaging the analgesic benefit of the opioid remifentanil. Sci Transl Med. 2011;3:70ra14. doi: 10.1126/scitranslmed.3001244. [DOI] [PubMed] [Google Scholar]
- 79.Benedetti F, Amanzio M, Casadio C, Oliaro A, Maggi G. Blockade of nocebo hyperalgesia by the cholecystokinin antagonist proglumide. PAIN. 1997;71:135–40. doi: 10.1016/s0304-3959(97)03346-0. [DOI] [PubMed] [Google Scholar]
- 80.Wendt L, Albring A, Benson S, Engler H, Engler A, Hinney A, Rief W, Witzke O, Schedlowski M. Catechol-O-methyltransferase Val158Met polymorphism is associated with somatosensory amplification and nocebo responses. PLoS One. 2014;9:e107665. doi: 10.1371/journal.pone.0107665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hall KT, Tolkin BR, Chinn GM, Kirsch I, Kelley JM, Lembo AJ, Kaptchuk TJ, Kokkotou E, Davis RB, Conboy LA. Conscientiousness is modified by genetic variation in catechol-O-methyltransferase to reduce symptom complaints in IBS patients. Brain Behav. 2015;5:39–44. doi: 10.1002/brb3.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Finnerup NB, Sindrup SH, Jensen TS. The evidence for pharmacological treatment of neuropathic pain. PAIN. 2010;150:573–81. doi: 10.1016/j.pain.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 83.Katz J, Finnerup NB, Dworkin RH. Clinical trial outcome in neuropathic pain: relationship to study characteristics. Neurology. 2008;70:263–72. doi: 10.1212/01.WNL.0000275528.01263.6c. [DOI] [PubMed] [Google Scholar]
- 84.Simpson DM, Rice AS, Emir B, Landen J, Semel D, Chew ML, Sporn J. A randomized, double-blind, placebo-controlled trial and open-label extension study to evaluate the efficacy and safety of pregabalin in the treatment of neuropathic pain associated with human immunodeficiency virus neuropathy. PAIN. 2014;155:1943–54. doi: 10.1016/j.pain.2014.05.027. [DOI] [PubMed] [Google Scholar]
- 85.Lund K, Vase L, Petersen GL, Jensen TS, Finnerup NB. Randomised controlled trials may underestimate drug effects: balanced placebo trial design. PLoS One. 2014;9:e84104. doi: 10.1371/journal.pone.0084104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Diener HC, Dowson AJ, Ferrari M, Nappi G, Tfelt-Hansen P. Unbalanced randomization influences placebo response: scientific versus ethical issues around the use of placebo in migraine trials. Cephalalgia. 1999;19:699–700. doi: 10.1046/j.1468-2982.1999.019008699.x. [DOI] [PubMed] [Google Scholar]
- 87.Fields HL, Price DD. Toward a neurobiology of placebo analgesia. In: Harrington A, editor. The placebo effect. Boston: Harvard University Press; 1997. pp. 93–116. [Google Scholar]
- 88.Kaptchuk TJ, Kelley JM, Conboy LA, Davis RB, Kerr CE, Jacobson EE, Kirsch I, Schyner RN, Nam BH, Nguyen LT, Park M, Rivers AL, McManus C, Kokkotou E, Drossman DA, Goldman P, Lembo AJ. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ. 2008;336:999–1003. doi: 10.1136/bmj.39524.439618.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Katz N. Methodological issues in clinical trials of opioids for chronic pain. Neurology. 2005;65(suppl 4):S32–49. doi: 10.1212/wnl.65.12_suppl_4.s32. [DOI] [PubMed] [Google Scholar]
- 90.Price DD, Vase L. The contributions of desire, expectation and reduced negative emotions to placebo anti-hyperalgesia in irritable bowel syndrome. In: Colloca L, Flaten M, Meissner K, editors. Placebo and pain from bench to bedside. Amsterdam: Academic Press Inc; 2013. pp. 215–16. [Google Scholar]
- 91.Vase L, Vollert J, Finnerup NB, Miao X, Atkinson G, Marshall S, Nemeth R, Lange B, Liss C, Price DD, Maier C, Jensen TS, Segerdahl M. Predictors of the placebo analgesia response in randomized controlled trials of chronic pain: a meta-analysis of the individual data from nine industrially sponsored trials. PAIN. 2015;156:1795–802. doi: 10.1097/j.pain.0000000000000217. [DOI] [PubMed] [Google Scholar]


