Abstract
Prior research suggests that immigrant enclaves provide respiratory health benefits for US Hispanic residents. We test if immigrant enclaves provide differential respiratory health benefits for Hispanic children in El Paso (Texas) based on individual-level factors. Results reveal that higher neighborhood immigrant density is associated with reduced odds of wheezing, but that the protective immigrant enclave effect is modified by poverty, general health status, body mass index (BMI), and caretaker nativity. Higher immigrant density is significantly more protective for poor children and those with foreign-born caretakers; conversely, it is significantly less protective for children in worse health and those with higher BMI. These findings foster a novel understanding of how immigrant enclaves may be differentially protective for Hispanic children based on individual-level factors.
Keywords: children; asthma; multilevel models; Hispanic health paradox; neighborhood effects; El Paso, Texas; health risk and protective factors; ethnic density; immigrant; enclave
INTRODUCTION AND BACKGROUND
The “Hispanic health paradox” (HHP) denotes an apparent contradiction in which Hispanic immigrant populations in the US experience more economic deprivation but better health outcomes than their native-born counterparts and other racial/ethnic subgroups, including the white-Anglo majority (Markides & Coreil 1986). Hypothesized reasons for the HHP include reverse migration, whereby ill Hispanics return to their countries of origin; the Hispanic lifestyle, which emphasizes the presence of exceptionally strong socio-cultural ties that are protective for health; and the healthy migrant effect, which suggests that those migrating are healthier than average, due to the demands of migration (Thomson et al. 2013). Asthma, the leading chronic disease during childhood in the industrialized world (Shankardass et al. 2007), is a condition for which a HHP has been noted. Studies have shown that US-born Hispanic children have higher rates of asthma than Hispanic children born outside the US (Eldeirawi et al. 2005; Holguin et al. 2005), which is notable since immigrants not only tend to be economically deprived, but also experience healthcare access barriers, legal residency challenges and English-language limitations (Holguin et al. 2005; Javier et al. 2007).
Research over the past decade indicates that the HHP may be shaped in part by the protective effects of living in co-ethnic neighborhoods (Browning & Cagney 2003; Cagney et al. 2005; 2007; Wen et al. 2003; Landy et al. 2012; Peak & Weeks 2002). A systematic review of the literature revealed mounting evidence of protective physical health effects associated with increasing Hispanic ethnic density in the US (Bécares et al. 2012). Of direct relevance here is a studying showing that high Hispanic immigrant concentration at the neighborhood level decreased odds of respiratory health problems among Hispanics in Chicago (Cagney et al. 2005, 2007). Researchers found a graded effect for the relationship between neighborhood percent foreign-born (immigrant density) and asthma prevalence among Chicago adults, in that foreign-born Latinos had low prevalence rates for asthma (5%) when they lived in immigrant neighborhoods (1.5 SD above mean for percent foreign born) and high prevalence rates of asthma (22%) when they lived in non-immigrant neighborhoods (1.5 SD below mean) (Cagney et al. 2007).
This suggests that the effect of immigrant enclave residence on respiratory health among Hispanics is modified by nativity. The protective mechanism associated with residing in immigrant enclaves has been explained based on the collective benefits that come from enhanced resource sharing, psychosocial support, and access to information regarding available health care services among co-ethnic immigrants who congregate in such settings (Browning & Cagney 2003; Cagney et al. 2005; 2007; Wen et al. 2003).
Such findings for US Hispanic populations, along with those from a broader literature highlighting the mental (and to a lesser extent, physical) health benefits of increased ethnic density for multiple lower status racial/ethnic minority groups in the US and the UK (Pickett & Wilkinson 2008; Bécares 2012), support the conventional wisdom that Hispanic immigrant enclave residence has generally protective health effects. However, no prior research has examined if enclave living may present respiratory health risks (in addition to previously documented benefits) for specific Hispanic subgroups based on other axes of individual difference.
In this study we examine the roles of individual-level variables associated with Hispanic children’s sex (male/female), socioeconomic status, medical history, exposure to in-home environmental triggers of wheezing, caretakers’ nativity (i.e., foreign vs. US born), and length of residence in the Hispanic immigrant gateway of El Paso (Texas) – in addition to the percent of foreign-born residents in the neighborhood (immigrant density) – to provide a more comprehensive and nuanced characterization of the effects of immigrant enclave residence on children’s respiratory health than has been accomplished by prior studies. This allows us to expand knowledge beyond the current one-dimensional understanding (i.e., ethnic enclaves may be protective for Hispanics) toward a multidimensional understanding of individual-level protective and risk factors associated with neighborhood immigrant density. Specifically, we employ multilevel logistic regression modeling with cross-level interactions. This methodological approach directs attention toward the contexts in which people reside and how social settings may impact different types of people in different ways (Wright & Subramanian 2007). A multilevel framework is needed to understand and successfully reduce asthma disparities (Wright & Subramanian 2007; Canino et al. 2009). Multilevel models permit examination of how immigrant density at the neighborhood level relates to children’s health; multilevel models with cross-level interactions also enable us to determine if effects of neighborhood immigrant density vary for different types of children at the individual level.
The primary research questions and hypotheses are: (1) Does neighborhood foreign-born (i.e., immigrant) density significantly impact Hispanic children’s wheezing independent of individual-level factors? Based on prior research, we hypothesize that Hispanic children in neighborhoods with higher immigrant density will have lower odds of wheezing. (2) Do the effects of individual-level independent variables on Hispanic children’s wheezing vary based on neighborhood immigrant density? In other words, does immigrant density affect the respiratory health of different types of children in divergent ways? Two specific sub-questions are addressed. (2a) Do the effects of neighborhood immigrant density vary between Hispanic children of foreign-born caretakers and those whose caretakers were born in the US? Prior research (Cagney et al. 2007) supports the hypothesis that greater neighborhood immigrant density will be associated with lower odds of wheezing for children of immigrant caretakers. (2b) Do the effects of neighborhood immigrant density vary between Hispanic children based on sex (male/female), socioeconomic status, medical history, exposure to in-home environmental triggers of wheezing, or length of residence in El Paso? There is not a strong deductive basis for postulating hypotheses regarding question 2b, as it is a novel element of this study.
METHODS
Study Area
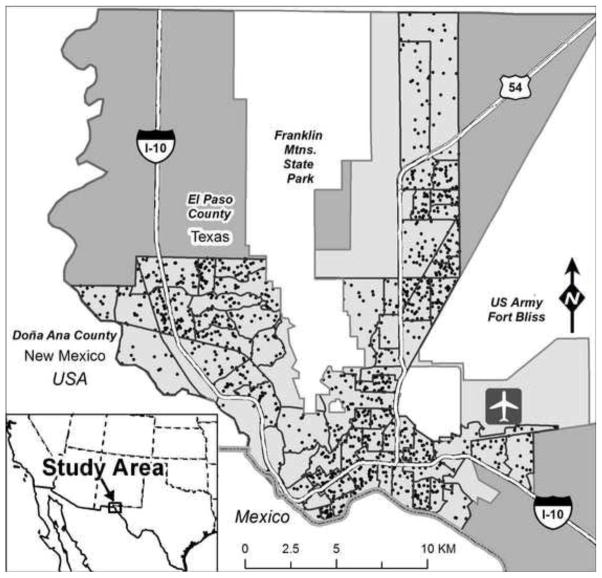
The study area is El Paso, Texas, which had an estimated population of 640,066 in 2011 (see Figure 1). In 2011, 80.7% of El Paso residents were Hispanic (compared to 16.1% of US residents and 37.2% of Texas residents). Smaller percentages of the city’s population were non-Hispanic white (14.7%) and non-Hispanic black (2.8%). According to the most recent US Bureau of the Census (2010 Census (2011) figures, 23.3% of El Paso residents lived in poverty (compared to the US figure of 14.3%). Among El Paso residents, 25.5% were foreign-born (US=12.8%) and 29.1% were less than 18 years of age (US=24.0%). Additionally, El Paso has a children’s lifetime asthma prevalence rate of 15% (based on the survey administered as part of this study). This is relatively high compared to the Texas state children’s lifetime prevalence rate of 12% (American Lung Association 2012). The El Paso children’s lifetime prevalence rate of 15% is also notably high given that the city’s child population is predominantly Mexican-origin; this subgroup has a substantially lower Texas state prevalence rate of 12% (Lara et al. 2006).
Figure 1.
Approximate home locations of Hispanic children (black points) in census tracts (black bordered polygons) analyzed within the EPISD (light grey)
Study Design and Subjects
Individual-level data for El Paso children were collected through a population-based, cross-sectional, observational mail survey that was approved by our university’s Institutional Review Board. The closed-ended questionnaire was sent to all primary caretakers (parents and guardians) of fourth/fifth grade students in the El Paso Independent School District (EPISD). The survey was conducted using the tailored design method (TDM) to obtain the highest achievable response rates (Dillman et al. 2009). All survey materials were provided to households in English and Spanish. Mailings were sent in three waves during May 2012. The first mailing consisted of the survey packet, which included a consent letter and the survey (in both English and Spanish), a $2 incentive and a postage-paid return envelope. A week later, we mailed a bilingual reminder postcard. One week after that, we re-sent the survey packet to all non-respondents (again with $2 and a postage-paid return envelope).
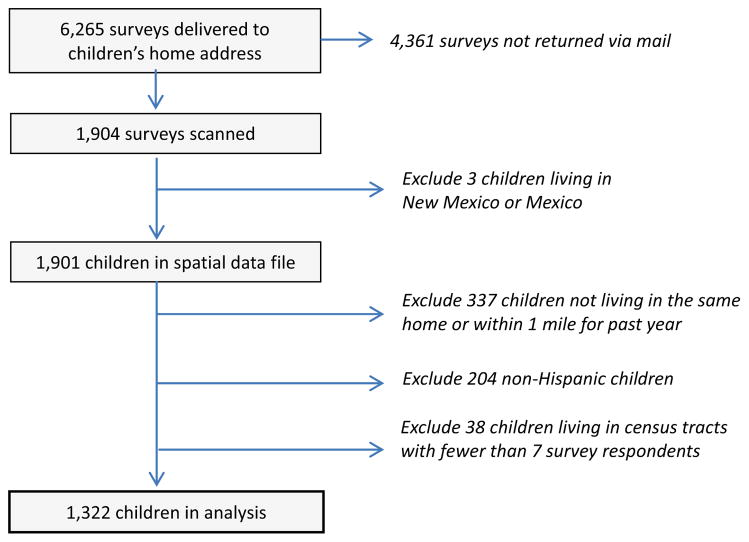
Ultimately, 6,295 primary caretakers were provided surveys at their home address and 1,904 were returned completed for a 30.2% response rate. Research indicates that similar and substantially lower survey response rates can yield representative samples (Curtin et al. 2000; Holbrook et al. 2008; Keeter et al. 2006; Visser et al. 1996). Respondents were primarily mothers (82%), fathers (10%) and grandparents (4%). More detailed descriptive statistics are presented below, but it is notable that the mean income of households was $20,000–$29,000. The vast majority of children (90%) were born in the US, and 16% were not continuously covered by health insurance over the past 12 months. This approximates the high rate of uninsured children in Texas, which leads the nation at 19% (the US average is 9%) (US-Mexico Border Health Commission 2010). Descriptive statistics indicate that our sample of fourth and fifth graders is generally representative of the EPISD student population across all grades, kindergarten through twelve (EPISD 2013). The percent male and percent Hispanic are nearly identical between the sample and the EPISD (49.9% vs. 51.4% and 82.2% vs. 82.6% respectively); the sample has a lower percentage of economically disadvantaged children than the EPISD as a whole (60.4% vs. 71.1%).
Based on home address data from the survey, residential locations for the 1,901 individual children living in El Paso were geocoded. Because we examine neighborhood effects on health conditions occurring over the past 12 months, it was valid to include cases only if children had lived at or near their current residence for 12 months or more. As an inclusion criterion, the survey question: “How long has this child lived within 1 mile (1.6 km) of your current residence?” was employed; the 337 cases responding “For less than 12 months” were excluded. We then excluded 204 non-Hispanic children from the analysis. Given the racial/ethnic diversity in asthma (e.g., blacks have higher rates than Hispanics), our interest in Hispanic health and immigrant density, and the low numbers of other races in the sample (e.g., only 112 children were black and 47 were Native American), we controlled for the effect of race/ethnicity by removing children of non-Hispanic racial/ethnic groups from the analyzed dataset.
The concept of a neighborhood is operationally defined as coinciding with 2010 census tract boundaries. This study includes each of 63 census tracts having at least seven Hispanic children, which we implemented as a cut-off for multilevel modeling. After excluding 38 children located in census tracts containing less than seven cases, there were 1,322 Hispanic children meeting all inclusion criteria. Figure 1 displays census tracts and approximate locations of children included in the analysis, while Figure 2 summarizes the process that yielded the survey data analyzed here.
Figure 2.
The EPISD Survey Sample
Multiple imputation (MI) was applied to the individual-level dataset to address missing values and non-response bias, and the multiply imputed data were analyzed using HLM software. MI is currently a best practice for addressing missing data in statistical analysis. MI involves creating multiple sets of values for missing observations using a regression-based approach (Penn 2007). It is used to avoid the bias that can occur when missing values are not missing completely at random (MCAR) (Penn 2007) and is appropriate for self-reported survey data (Enders 2010). In SPSS, 10 imputed datasets were specified to increase power and 200 between-imputation iterations were used to ensure that the resulting imputations were independent of each other. Using more than 3–5 datasets is the current “rule of thumb” in MI as it maximizes power and improves the validity of multi-parameter significance tests (Enders 2010). Analyzing a single imputed dataset treats the filled-in values as real data, which may underestimate sampling error. MI techniques appropriately adjust the standard errors for missing data (Enders 2010). HLM software allows for a maximum of 10 datasets in its MI option, and it accommodates the MI procedure by performing separate analyses on each dataset and then pooling results across analyses. The percent missing for the variables (described below) ranged from a low of 0.6% (general health status) to a high of 29.4% (body mass index).
Dependent Variable
The primary outcome variable is children’s “current wheeze”, which has been used in several previous studies (Asher et al. 2001; Björkstén et al. 2011; Brunekreef et al. 2012; Ellwood et al. 2001). Taken from the International Study of Asthma and Allergies in Childhood, the current wheeze item is a generally valid measure of asthma symptoms as responses to the question are in close agreement with asthma diagnosis by a respiratory physician (Jenkins et al 1996). The current wheeze variable is described in Table 1.
Table 1.
Analysis Variables: Survey Question, Coding, and Justification
| Variable | Survey Question | Coding | Justification |
|---|---|---|---|
| Individual-level | |||
| Current Wheeze | Has your child had wheezing or whistling in the chest in the last 12 months? From the International Study of Asthma and Allergies in Childhood (ISAAC) |
1=Yes 0=No |
Wheezing is a common symptom of asthma. It is easily recognized by parents and is more specific to asthma than cough (Warren 1999). Current wheeze was selected instead of diagnosed asthma due to this study’s emphasis on immigration, a characteristic that shapes access to medical care and thus an asthma diagnosis. |
| Sex (Male) | What is the child’s sex? | 1=Male 0=Female |
Boys have higher rates of asthma and other respiratory health problems than girls (CDC 2013). |
| Socio-economic Status1 | How many people are living or staying at this address? Which of the following best describes your yearly total household income for 2011 before taxes? 1=Less than $1,999 – 15=$150,000 or more |
1=Poor, according to the US Department of Health and Human Services (2011) definitions of poverty status 0=Non-poor |
Asthma rates are higher for children of lower socioeconomic status (Mitchell et al. 1989; Mielck et al. 1996). |
| Which of the following best describes your yearly total household income for 2011 before taxes? 1=Less than $1,999 – 15=$150,000 or more | 1=Affluent ($80,000 or more) 0=Not Affluent |
||
| General Health Status | How would you describe the overall health of the child? From the ISAAC |
1=Very poor – 6=Excellent | Health status is used as a medical history variable to account for the child’s underlying state of health (Aligne et al. 2000). |
| BMI (body mass index) | How tall is the child as of now? How much does the child weigh as of now? |
Reported height divided by the square of the reported weight | BMI is used as a medical history variable; being overweight is specifically associated with higher rates of asthma in Hispanic children (Morales et al. 2002). |
| Current smoking | At any time during the past 12 months, has anybody smoked inside your child’s home? | 1=Yes 0=No |
Smoking inside homes is an important cause of respiratory illness (Burr et al. 1999; Radic et al. 2011). |
| Mold | Has your child’s home had moldy or musty odors during the past 12 months? | 1=Yes 0=No |
Moldy/damp housing environments are associated with wheezing and asthma (Strachan 1988; Strachan & Sanders 1989; Williamson et al. 1997). |
| Length of Residence in El Paso (EP) | How long has this child lived in El Paso County? | 1=‘For less than 12 months’- 5=‘Since the child’s birth’ | Children’s asthma and allergy prevalence increased with longer residential duration in El Paso (Svendsen et al. 2009). |
| Primary Caretaker (PC) Born in the US | Primary caretakers were asked: “Where were you born?” | 1=US-born 0=Foreign- born |
Hispanic children born to US-born mothers have higher rates of asthma than the children of foreign-born mothers (Subramanian et al. 2009). |
| Neighborhood-level | |||
| % Foreign Born (Immigrant Density) | Percent of the census tract population not born in the US | Continuous variable | Foreign-born density in Chicago neighborhoods was protective for asthma and other respiratory diseases for foreign-born individuals (Cagney et al. 2007). |
Socioeconomic status is measured using a categorical variable (i.e., affluent, middle class, and poor). Middle class is the reference group in the analyses, and includes all children defined as being both non-poor and not affluent.
Individual-level Independent Variables
Individual-level covariates – including child’s sex, socioeconomic status (poverty and affluence compared to middle class), child’s general health status, child’s body mass index (BMI), smoking in the home, moldy odors in the home, child’s length of residence in El Paso, and primary caretaker’s nativity (US- or foreign-born) – are included as explanatory variables in this study because they have been associated with respiratory health outcomes in previous studies (see Table 1).
Neighborhood-level Independent Variable
Raw data to construct the variable for percent of foreign-born at the census tract-level (i.e., neighborhood immigrant density) were downloaded from the US Bureau of the Census website (US Bureau of the Census 2011) and transformed for analysis purposes (Table 1). We selected data for the years 2007–2011 (American Community Survey, 5-year estimates) since they were the closest available match to our 2012 survey data.
Descriptive Statistics
Table 2 presents descriptive statistics for all individual- and neighborhood-level variables prior to multiple imputation. Approximately 15% of caretakers reported that their children wheezed in the last 12 months. About 49% of the children in this study are male. While 16% of households are affluent, 44% of households are in poverty. Also, 8% and 13% of respondents reported smoking and moldy odors, respectively, in their homes in last 12 months. The mean value for the percent of the census tract population that is foreign born (neighborhood immigrant density) is 27%. Ages of children in the sample ranged from 9 to 13 years; 89.1% of children in this study were 9 to 11 years of age and 77.2% were 10–11 years of age. These descriptive statistics indicated that age-adjustment was not needed in this analysis.
Table 2.
Descriptive Statistics of Analysis Variables
| N | Mean | SD | Min | Max | % Missing | |
|---|---|---|---|---|---|---|
| Individual
|
||||||
| Current Wheeze | 1250 | 0.15 | 0.35 | 0.00 | 1.00 | 2.42 |
| Sex (Male) | 1241 | 0.49 | 0.50 | 0.00 | 1.00 | 3.15 |
| Poverty | 1117 | 0.44 | 0.50 | 0.00 | 1.00 | 12.46 |
| Affluence | 1155 | 0.16 | 0.36 | 0.00 | 1.00 | 9.46 |
| Health Status | 1273 | 4.981 | 0.93 | 2.00 | 6.00 | 0.59 |
| BMI | 900 | 20.012 | 5.50 | 6.67 | 69.20 | 29.40 |
| Smoking | 1227 | 0.08 | 0.27 | 0.00 | 1.00 | 4.25 |
| Mold | 1231 | 0.13 | 0.33 | 0.00 | 1.00 | 4.03 |
| Length Res. EP3 | 1136 | 4.244 | 1.24 | 1.00 | 5.00 | 11.44 |
| PC5 Born US | 1256 | 0.44 | 0.50 | 0.00 | 1.00 | 1.98 |
|
| ||||||
| Neighborhood
|
||||||
| % Foreign Born | 63 | 26.22 | 10.69 | 3.46 | 51.17 | 0 |
The mean Health Status (4.98) for children is above “good” (4) and just below “very good” (5).
The mean BMI (20.01) for children is based on weight in kilograms/height in meters squared.
Abbreviation for El Paso
The mean Length of Residence in El Paso (4.24) for children is between “since after the child’s birth, but before the child was 2 years old” (4) and “since the child’s birth” (5).
Abbreviation for Primary Caretaker
Analytic Strategy
Because this study is designed to assess the influence of neighborhood context on an individual-level binary dependent variable, we employed hierarchical logistic regression modeling (HLRM). HLRM enables multivariate analyses of multilevel data structures with binary outcomes. It is preferable to traditional logistic regression modeling for data analysis with different levels, because ignoring the hierarchical structure of data causes aggregation bias and leads to incorrect inferences (Raudenbush & Bryk 2002).
Specifically, the level-1 equation analyzes the following variables: child’s sex, poverty, affluence, child’s health status, child’s BMI, smoking behaviors, moldy odors, child’s residential duration in El Paso, and primary caretaker’s nativity. Percent foreign born is included in the level-2 equation. First, determinants of current wheeze are modeled with only individual-level (level-1) variables (Model 1). Then, the neighborhood-level percent foreign-born variable is included in Model 2.
In order to comprehensively examine neighborhood effects on children’s respiratory health and address research question 2, it was necessary to analyze cross-level interactions in addition to main effects. Model 3 is a cross-level interaction model that includes interactions between the individual-level variables and percent foreign-born at the neighborhood level in addition to all main effects variables. Since HLM software does not perform multicollinearity diagnostic tests, SPSS was used to examine possible multicollinearity among the analysis variables included in each model. According to variance inflation factor, tolerance, and condition index criteria (Belsley et al. 1980), inferences from the models do not appear to have been affected by multicollinearity problems. Additionally, we performed two sensitivity analyses. One was performed to evaluate the sensitivity of the reported findings to the choice of “current wheeze” as the dependent variable as compared to caretaker-reported “doctor-diagnosed asthma.” The second was performed to evaluate the sensitivity of the reported findings to the choice of covariates for inclusion in the statistical models to address concerns about bias due to over-adjustment for variables on the causal pathway between neighborhood foreign-born density and current wheeze (see Shrier & Platt 2008). Specifically, we developed a causal diagram of relationships between all variables; then we ran a reduced Model 2 that omitted the four covariates (BMI, poverty, health status, and primary caretaker’s nativity) that plausibly mediated the effect of neighborhood foreign-born density on children’s current wheeze.
RESULTS
Table 3 displays results for Models 1 and 2, which reveal determinants of children’s wheezing status accounting for individual-level variables and foreign-born density at the neighborhood level. Model 1 reports the effects of the individual-level variables on children’s odds of current wheezing. Household poverty and child’s general health status significantly predict wheezing. Child’s residential duration in El Paso and primary caretaker’s US-nativity are significantly and positively associated with current wheeze; i.e., the longer a child had lived in El Paso or if their caretaker was US-born, the greater the likelihood that they had recently experienced wheezing. Moldy odor indoors also approaches significance in Model 1 (p<0.10).
Table 3.
Individual and Neighborhood Characteristics Associated with Children’s Current Wheeze
| Variables | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| Coef. | OR | 95% CI | Coef. | OR | 95% CI | |
| Intercept | −0.010 | 0.989 | (0.222,4.407) | 0.486 | 1.626 | (0.327,8.086) |
| Individual | ||||||
| Sex (Male) | 0.214 | 1.239 | (0.920,1.671) | 0.201 | 1.223 | (0.909,1.647) |
| Poverty | −0.466** | 0.627 | (0.437,0.899) | −0.386*** | 0.679 | (0.464,0.994) |
| Affluence | 0.257 | 1.293 | (0.851,1.968) | 0.211 | 1.235 | (0.816,1.873) |
| Health Status | −0.737*** | 0.478 | (0.394,0.580) | −0.756*** | 0.469 | (0.386,0.572) |
| BMI | 0.007 | 1.007 | (0.982,1.033) | 0.008 | 1.008 | (0.983,1.034) |
| Smoking | −0.220 | 0.802 | (0.415,1.553) | −0.200 | 0.818 | (0.423,1.583) |
| Mold | 0.402* | 1.495 | (0.925,2.415) | 0.424* | 1.528 | (0.942,2.480) |
| Length Res. EP1 | 0.287*** | 1.332 | (1.115,1.593) | 0.290*** | 1.336 | (1.118,1.598) |
| PC2 Born US | 0.780*** | 2.181 | (1.629,2.922) | 0.746*** | 2.110 | (1.577,2.823) |
| Neighborhood | ||||||
| % Foreign Born | … | … | … | −0.016** | 0.983 | (0.969,0.998) |
p<0.01,
p<0.05,
p<0.10
Abbreviation for El Paso
Abbreviation for Primary Caretaker
Model 2 includes percent foreign-born at the neighborhood level (i.e., immigrant density). Percent foreign-born significantly and negatively predicts children’s wheezing (OR= 0.983); i.e., the greater the immigrant density of the neighborhood, the lower the odds of wheezing among children (adjusting for the nativity of the primary caretaker, along with all other individual-level variables). All individual-level variables with significance in Model 1 (i.e., poverty, health status, duration of residence in El Paso, primary caretaker born in US) show the same direction and significance in Model 2.
Table 4 reports the results of Model 3, which includes all level-1 variables, neighborhood-level percent foreign-born and cross-level interactions between percent foreign-born at the neighborhood level and each of the individual-level variables. The cross-level interaction results reveal that the associations of individual-level poverty, children’s general health status, BMI, and primary caretaker’s nativity with the odds of children’s current wheezing vary based on neighborhood percent foreign born (immigrant density). First, children living in poverty (in comparison to those of middle class) exhibit significantly reduced odds of wheezing as immigrant density increases. Second, children with better (as opposed to worse) health and lower (versus higher) BMI exhibit reduced odds of wheezing as immigrant density increases. Third, children of foreign-born primary caretakers (compared to children of US-born caretakers) exhibit significantly reduced odds of wheezing as immigrant density increases (p=0.065). In terms of main effects, poverty, health status and BMI at the individual-level and percent of foreign-born people at the neighborhood-level are significant or approach significance.
Table 4.
Cross-level Interactions with Percent Foreign Born (Model 3)
| Variables | Coef. | OR | 95% CI |
|---|---|---|---|
| Intercept | 1.537 | 4.654 | (0.390,55.574) |
| Individual | |||
| Sex (Male) | 0.373 | 1.452 | (0.854,2.469) |
| Poverty | −0.873*** | 0.417 | (0.252,0.691) |
| Affluence | 0.050 | 1.051 | (0.476,2.322) |
| Health Status | −0.967*** | 0.380 | (0.260,0.557) |
| BMI | 0.076*** | 1.079 | (1.032,1.130) |
| Smoking | −0.011 | 0.988 | (0.340,2.879) |
| Mold | 0.126 | 1.134 | (0.491,2.618) |
| Length Res. EP1 | 0.118 | 1.125 | (0.943,1.344) |
| PC2 Born US | 0.086 | 1.090 | (0.704,1.689) |
| Neighborhood | |||
| % Foreign Born | −0.067* | 0.934 | (0.863,1.013) |
| Cross-level Interactions | |||
| Sex* Foreign Born | −0.004 | 0.995 | (0.976,1.014) |
| Poverty* Foreign Born | 0.020** | 1.020 | (1.003,1.039) |
| Affluence* Foreign Born | 0.002 | 1.002 | (0.975,1.032) |
| Health Status* Foreign Born | 0.017** | 1.017 | (1.005,1.031) |
| BMI* Foreign Born | −0.002*** | 0.997 | (0.996,0.999) |
| Smoking* Foreign Born | −0.004 | 0.995 | (0.964,1.027) |
| Mold* Foreign Born | 0.010 | 1.010 | (0.983,1.038) |
| Length Res. EP* Foreign Born | 0.001 | 1.001 | (0.995,1.007) |
| PC Born US* Foreign Born | 0.013* | 1.013 | (0.999,1.029) |
p<0.01,
p<0.05,
p<0.10
Abbreviation for El Paso
Abbreviation for Primary Caretaker
Results of the sensitivity analyses (tables not shown) reveal the following. First, the effects are generally the same for doctor-diagnosed asthma as they are for current wheeze with the exception of the fact that there are fewer significant cross-level interaction terms for doctor-diagnosed asthma. In Model 2, the statistically significant individual-level findings are the same, except male becomes significant (p<0.01). Neighborhood foreign-born density significantly predicts asthma diagnosis at the p<0.05 level and maintains the same directionality as with current wheeze. In terms of cross-level interactions for doctor-diagnosed asthma, there was one significant term in Model 3. The relationship between health status and asthma significantly varied based on neighborhood immigrant density, as it did with current wheeze. Second, the significant negative effect of neighborhood foreign-born density on current wheeze in the reduced Model 2 (p=0.034, OR= 0.986) – which omitted BMI, poverty, health status, and primary caretaker’s nativity – is the same as that reported in the full Model 2. This suggests that the results for neighborhood foreign-born density are not biased by the inclusion of those covariates.
DISCUSSION
The extant literature generally supports the conventional wisdom that immigrant enclave have protective health effects for Hispanic residents in the US (Landy et al. 2012; Cagney et al. 2007; see Bjornstrom 2011 for an example of an exception). Expanding upon current knowledge, this is the first study to examine whether or not immigrant enclave living presents differential respiratory health benefits (or risks, in addition to previously documented benefits) for specific Hispanic subgroups based on other axes of individual difference. In concordance with the extant literature, findings reveal that higher immigrant density is generally protective for Hispanic children in El Paso, in that it is associated with reduced odds of wheezing. In terms of novel findings, cross-level interaction results indicate that the protective effect of immigrant density on Hispanic children’s wheezing is modified by poverty status, general health status, BMI, and caretaker nativity. Specifically, higher immigrant density is significantly more protective for children in poverty than for children who are middle class and for children of immigrant caretakers than for those with US-born caretakers; conversely, higher immigrant density is significantly less protective for children in worse (as opposed to better) general health and for children with higher (as opposed to lower) measures of BMI. We discuss these findings in turn.
Consistent with our hypothesis for research question 1, we found that neighborhood immigrant density was significantly and negatively associated with Hispanic children’s wheezing. Model 2 shows that Hispanic children in neighborhoods with higher immigrant density have lower odds of wheezing, which highlights a protective effect of co-ethnic residence in Hispanic immigrant enclaves. Previous research has reported similar findings (Cagney et al. 2007), which points toward a possible neighborhood explanation for the Hispanic health paradox (HHP). Note that the significant protective individual-level effects of having a foreign-born caretaker (found in Model 1) persist even when accounting for neighborhood immigrant density (Model 2). This indicates that immigrant status has both compositional (individual) and contextual (neighborhood) effects that are protective of Hispanic children’s respiratory health. Another plausible explanation for the protective effects of immigrant status, contextually-relevant to the study area, is that foreign-born (predominantly Mexican-origin) Hispanics living in El Paso’s immigrant enclaves are more likely to cross the international border to Ciudad Juárez in order to access relatively low-cost medical treatments (Rivera et al. 2009). However, that is not a valid primary explanation since less than 5% of Hispanic children whose parents responded to the survey had their usual source of care in Mexico.
The cross-level interaction findings (from Model 3) address research question 2 as well as Wright and Subramanian’s (2007) call to investigate how neighborhood characteristics impact different types of people in divergent ways. First, the finding that higher levels of immigrant density are associated with significantly lower odds of wheezing for Hispanic children in poverty as compared to those are middle class is counterintuitive. This relates to a surprising main effect found in all models, in which household poverty was significantly associated with decreased odds of children’s wheezing. To our knowledge, no prior studies have found poverty to be significantly protective of respiratory health at the individual level. These findings may be explained by the enhanced access to mutual support enjoyed among poor Hispanic people within El Paso’s generally economically-deprived immigrant enclaves. Shankardass et al. (2007) speculated that, in the context of low SES, Hispanic communities may have collective advantages against asthma, possibly due to their enhanced social capital, compared with communities primarily of other racial/ethnic make-up. This suggests that the typically deleterious effects of poverty on health outcomes may be attenuated by strong social and cultural ties that tend to be constituted within certain racial/ethnic minority communities. As Wen et al. (2003: 856) state, in such cases “the prevalence of social resources mediates the impact of neighborhood affluence, indicating that neighborhood economic context might work through social resources to influence health status”.
We assert that it is unlikely that similar results for individual-level poverty would be found in other contexts, since impoverished yet stable, close-knit communities characterized by strong mutual support are not common in most US cities. Instead, poverty is typically associated with inner city problems, including social isolation and violence, which has been linked to stress and high asthma rates (Wright & Subramanian 2007). While El Paso is among the poorest of US cities (with generally relatively high Hispanic and immigrant densities), it paradoxically has among the lowest violent crime rates in the nation. Within El Paso, a recent study found that increasing Hispanic and immigrant neighborhood densities were not associated with higher homicide rates, which runs counter to expectations (Emerick et al. 2013). Additionally, relatively poor Hispanic immigrant enclaves in El Paso exhibit high levels of home ownership and residential stability compared to socio-demographically similar areas in other US cities. Beyond our speculation regarding the counterintuitive associations between household poverty, immigrant density and children’s wheezing found here, more multilevel modeling analyses that include measures of collective efficacy and/or social capital (e.g., Cagney et al. 2007) and that test such relationships across a range of social contexts are needed in order to clarify understanding.
Second, the finding that higher levels of immigrant density are associated with lower odds of wheezing for children of immigrant caretakers as compared to children of US-born caretakers is novel, although it generally aligns with findings of Cagney et al. (2007). It suggests greater access to mutual support is enjoyed by immigrants in particular from living within immigrant enclaves. In other words, greater collective efficacy, socio-cultural cohesion and exchanges of resources and information related to respiratory health within Hispanic immigrant enclaves may translate into enhanced protective effects for children of immigrant (in comparison to US-born) primary caretakers.
Third, the finding that higher neighborhood immigrant density is associated with reduced odds of wheezing for children in better (as opposed to worse) health and with lower (as opposed to higher) BMI measures suggests that there are physiological constraints to the protective effects of residing in co-ethnic immigrant enclaves for Hispanic children. That is, Hispanic children whose medical histories indicate worse health may experience significantly reduced respiratory health benefits from residing in immigrant neighborhoods compared to children in better health. This suggests that optimism about the apparent resilience to wheezing exhibited by impoverished, Hispanic children dwelling in immigrant enclaves should be tempered by the finding that the respiratory health benefits of enclave living are significantly less likely to be experienced by unhealthy (rather than healthy) children.
In conclusion, the multilevel analysis approach implemented here enabled clarification of differential health benefits to specific groups of Hispanic children in association with immigrant enclave residence. In future studies, analysts should employ longitudinal study designs in order to disentangle complex causal pathways, which could not be fully clarified based on the cross-sectional study design employed here. More longitudinal and multilevel research examining how neighborhood characteristics impact different types of people in divergent ways is needed to foster a multidimensional understanding of individual-level protective and risk factors.
Hispanic children in immigrant enclaves generally enjoy respiratory health benefits
However, enclaves are differentially protective based on individual-level factors
Enclaves are more protective for poor children and those with foreign-born caretakers
Enclaves are less protective for children in worse health and those with higher BMI
Acknowledgments
We acknowledge Bibi Mancera and Zuleika Ramirez at the Hispanic Health Disparities Center and the staff at the UTEP Campus Post Office for their assistance in carrying out the survey. The research participants are also gratefully recognized. The work of student research assistants Anthony Jimenez, Marie Gaines, Stephanie Clark-Reyna, Alexander Balcazar, and Paola Chavez-Payan is appreciated. We also acknowledge Dr. Rosalind Wright for her thoughtful comments on an earlier version of this manuscript. This project was supported by Award Number P20 MD002287-05S1 from the National Institute on Minority Health and Health Disparities (NIMHD) and the Environmental Protection Agency (EPA) and Award Number CMMI-1129984 from the National Science Foundation (NSF).
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMHD, EPA, or NSF.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Young-An Kim, Email: youngank@uci.edu, Department of Sociology & Anthropology, University of Texas at El Paso, 500 West University Ave, El Paso, Texas 79968, USA.
Timothy W. Collins, Email: twcollins@utep.edu, Department of Sociology & Anthropology, University of Texas at El Paso, 500 West University Ave, El Paso, Texas 79968, USA Tel. +19157476526; fax +19157475505
Sara E. Grineski, Email: segrineski@utep.edu, Department of Sociology & Anthropology, University of Texas at El Paso, 500 West University Ave, El Paso, Texas 79968, USA
References
- Aligne CA, Auinger P, Byrd RS, Weitzman M. Risk factors for pediatric asthma: Contributions of poverty, race, and urban residence. American Journal of Respiratory and Critical Care Medicine. 2000;162:873–877. doi: 10.1164/ajrccm.162.3.9908085. [DOI] [PubMed] [Google Scholar]
- American Lung Association. Trends in Asthma Morbidity and Mortality. 2012 Available from http://www.lung.org/finding-cures/our-research/trend-reports/asthma-trend-report.pdf.
- Asher MI, Barry D, Clayton T, Crane J, Souza WD, Ellwood P, Ford RPK, Mitchell EA, Moyes C, Pattemore P, Pearce N, Stewart AW. The burden of symptoms of asthma, allergic rhino conjunctivitis and atopic eczema in children and adolescents in six New Zealand centers: ISAAC Phase One. New Zealand Medical Journal. 2001;114:114–120. [PubMed] [Google Scholar]
- Bécares L, Shaw R, Nazroo J, Stafford M, Albor C, Atkin K, Kiernan K, Wilkinson R, Pickett K. Ethnic density effects on physical morbidity, mortality, and health behaviors: a systematic review of the literature. American Journal of Public Health. 2012;102 (12):e33–e66. doi: 10.2105/AJPH.2012.300832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsley D, Kuh E, Welsch R. Regression diagnostics: Identifying influential data and sources of collinearity. Hoboken, NJ: Wiley; 1980. [Google Scholar]
- Björkstén B, Aït-Khaled N, Innes Asher M, Clayton TO, Robertson C the ISAAC Phase Three Study Group. Global analysis of breast feeding and risk of symptoms of asthma, rhino conjunctivitis and eczema in 6–7 year old children: ISAAC Phase Three. Allergologia et Immunopatholgia. 2011;39 (6):318–325. doi: 10.1016/j.aller.2011.02.005. [DOI] [PubMed] [Google Scholar]
- Bjornstrom E. To live and die in LA County: Neighborhood economic and social context and premature age-specific mortality rates among Latinos. Health & Place. 2011;17 (1):230–237. doi: 10.1016/j.healthplace.2010.10.009. [DOI] [PubMed] [Google Scholar]
- Browning CR, Cagney KA. Moving beyond poverty: Neighborhood structure, social processes, and health. Journal of Health and Social Behavior. 2003;44:552–571. [PubMed] [Google Scholar]
- Brunekreef B, Mutius EV, Wong GK, Odhiambo JA, Clayton TO the ISAAC Phase Three Study Group. Early life exposure to farm animals and symptoms of asthma, rhino conjunctivitis and eczema: an ISAAC Phase Three Study. International Journal of Epidemiology. 2012;41:753–761. doi: 10.1093/ije/dyr216. [DOI] [PubMed] [Google Scholar]
- Burr ML, Anderson HR, Austin JB, Harkins LS, Kaur B, Strachan DP, Warner JO. Respiratory symptoms and home environment in children: a national survey. Thorax. 1999;54(1):27–32. doi: 10.1136/thx.54.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cagney KA, Browning CR, Wallace DM. Explaining the Latino Asthma Advantage: The Role of Neighborhood Social Context. Population Association of America Annual Meeting; Philadelphia, PA. 2005. Available from https://ssa.uchicago.edu/sites/default/files/uploads/10212004.pdf. [Google Scholar]
- Cagney KA, Browning Christopher R, Wallace DM. The Latino Paradox in Neighborhood Context: The Case of Asthma and Other Respiratory Conditions. American Journal of Public Health. 2007;97(5):919–925. doi: 10.2105/AJPH.2005.071472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canino G, McQuaid EL, Rand CS. Addressing Asthma Health Disparities: A Multilevel Challenge. Journal of Allergy and Clinical Immunololgy. 2009;123 (6):1209–1219. doi: 10.1016/j.jaci.2009.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Dieseases Control and Prevention (CDC) Asthma’s Impact on the Nation Data from the CDC National Asthma Control Program. 2013 Available from http://www.cdc.gov/asthma/impacts_nation/AsthmaFactSheet.pdf.
- Curtin R, Presser S, Singer E. The Effects of Response Rate Changes on the Index of Consumer Sentiment. Public Opinion Quarterly. 2000;64 (4):413–428. doi: 10.1086/318638. [DOI] [PubMed] [Google Scholar]
- Dillman DA, Smyth JD, Christian LM. Internet, Mail, and Mixed-mode Surveys: The Tailored Design Method. 3. Hoboken, New Jersey: John Wiley & Sons; 2009. [Google Scholar]
- Ellwood P, Asher MI, Bjorksten B, Burr M, Pearce N, Robertson CF the ISAAC Phase One Study Group. Diet and asthma, allergic rhino conjunctivitis and atopic eczema symptom prevalence: an ecological analysis of the International Study of Asthma and Allergies in Childhood (ISAAC) data. European Respiratory Journal. 2001;17:436–443. doi: 10.1183/09031936.01.17304360. [DOI] [PubMed] [Google Scholar]
- Eldeirawi K, McConnell R, Freels S, Persky VW. Associations of place of birth with asthma and wheezing in Mexican American children. American Academy of Allergy, Asthma and Immunology. 2005;116 (1):42–48. doi: 10.1016/j.jaci.2005.03.041. [DOI] [PubMed] [Google Scholar]
- Emerick NA, Curry TR, Collins TW, Fernando Rodriguez S. Homicide and Social Disorganization on the Border: Implications for Latino and Immigrant Populations. Social Science Quarterly. 2013 doi: 10.1111/ssqu.12051. [DOI] [Google Scholar]
- Enders CK. Applied Missing Data Analysis. New York: Guilford Press; 2010. [Google Scholar]
- EPISD. Enrollment Statistics, 2011–2012. 2013 [Cited 29 June 2013]; Available from: http://www.episd.org/district_info/enrollment_stats.php.
- Holbrook A, Krosnick J, Pfent A. The Causes and Consequences of Response Rates in Surveys by the News Media and Government Contractor Survey Research Firms. In: Lepkowski JM, Tucker NC, Brick JM, De Leeuw ED, Japec L, Lavrakas PJ, Link MW, Sangster RL, editors. Advances in telephone survey methodology. New York: Wiley; 2008. pp. 499–528. [Google Scholar]
- Holguin F, David M, Mannino JA, Mott J, Ford ES, Teague WG, Redd SC, Romieu I. Country of birth as a risk factor for asthma among Mexican Americans. American Journal of Respiratory and Critical Care Medicine. 2005;171:103–108. doi: 10.1164/rccm.200402-143OC. [DOI] [PubMed] [Google Scholar]
- Javier JR, Wise PH, Mendoza FS. The Relationship of Immigrant Status With Access, Utilization, and Health Status for Children with Asthma. Ambulatory Pediatrics. 2007;7:421–430. doi: 10.1016/j.ambp.2007.06.004. [DOI] [PubMed] [Google Scholar]
- Jenkins MA, Clarke JR, Carlin JB, Robertson CF, Hopper JL, Dalton MF, Giles GG. Validation of questionnaire and bronchial hyperresponsiveness against respiratory physician assessment in the diagnosis of asthma. International journal of epidemiology. 1996;25 (3):609–616. doi: 10.1093/ije/25.3.609. [DOI] [PubMed] [Google Scholar]
- Keeter S, Kennedy C, Dimock M, Best J, Craighill P. Gauging the Impact of Growing Nonresponse on Estimates from a National RDD Telephone Survey. Public Opinion Quarterly. 2006;70 (5):759–779. [Google Scholar]
- Landy DC, Mintzer MJ, Silva AK, Dearwater SR, Schulman CI. Hispanic Ethnicity and Fatal Fall Risk: Do Age, Gender, and Community Modify the Relationship? Journal of Surgical Research. 2012;175 (1):113–117. doi: 10.1016/j.jss.2011.02.035. [DOI] [PubMed] [Google Scholar]
- Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics. 2006;117 (1):43–53. doi: 10.1542/peds.2004-1714. [DOI] [PubMed] [Google Scholar]
- Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. Journal of Health Care Poor Underserved. 2002;13:477–503. doi: 10.1177/104920802237532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides KS, Coreil J. The health of Hispanics in the southwestern United States: An epidemiologic paradox. Public Health Reports. 1986;101:253–265. [PMC free article] [PubMed] [Google Scholar]
- Mielck A, Reitmeir P, Wjst M. Severity of Childhood Asthma by Socioeconomic Status. International Epidemiological Association. 1996;25 (2):388–393. doi: 10.1093/ije/25.2.388. [DOI] [PubMed] [Google Scholar]
- Mitchell EA, Stewart AW, Pattemore PK, Asher MI, Harrison AC, Rea HH. Socioeconomic Status in Childhood Asthma. International Epidemiological Association. 1989;18 (4):888–890. doi: 10.1093/ije/18.4.888. [DOI] [PubMed] [Google Scholar]
- Peak C, Weeks JR. Does community context influence reproductive outcomes of Mexican origin women in San Diego, California? Journal of Immigrant Health. 2002;4 (3):125–136. doi: 10.1023/A:1015646800549. [DOI] [PubMed] [Google Scholar]
- Penn DA. Estimating missing values from the general social survey: an application of multiple imputation. Social Science Quarterly. 2007;88 (2):573–584. [Google Scholar]
- Pickett K, Wilkinson R. People like us: Ethnic density effects on health. Ethnicity & Health. 2008;13 (4):321–334. doi: 10.1080/13557850701882928. [DOI] [PubMed] [Google Scholar]
- Radic SD, Gvozdenovic BS, Pesic IM, Zivkovic ZM, Skodric-Trifunovic V. Exposure to tobacco smoke among asthmatic children: parents’ smoking habits and level of education. The International Journal of Tuberculosis and Lung Disease. 2011;15 (2):276–280. [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Thousand Oaks, NJ: Sage; 2002. [Google Scholar]
- Rivera JO, Ortiz M, Cardenas V. Cross-Border Purchase of Medications and Health Care in a Sample of Residents of El Paso, Texas, and Ciudad Juarez, Mexico. Journal of the National Medical Association. 2009;101 (2):167–173. doi: 10.1016/s0027-9684(15)30831-2. [DOI] [PubMed] [Google Scholar]
- Shankardass K, McConnell RS, Milam J, Berhane K, Tatalovich Z, Wilson JP. The association between contextual socioeconomic factors and prevalent asthma in a cohort of Southern California school children. Social Science and Medicine. 2007;65 (8):1792–1806. doi: 10.1016/j.socscimed.2007.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrier I, Platt RW. Reducing bias through directed acyclic graphs. BMC Medical Research Methodology. 2008;8:70. doi: 10.1186/1471-2288-8-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strachan DP. Damp housing and childhood asthma: validation of reporting of symptoms. British Medical Journal. 1988;297:1223–1226. doi: 10.1136/bmj.297.6658.1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strachan DP, Sanders CH. Damp housing and childhood asthma; respiratory effects of indoor air temperature and relative humidity. Journal of Epidemiology and Community Health. 1989;43:7–14. doi: 10.1136/jech.43.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian SV, Jun HJ, Kawachi I, Wright RJ. Contribution of race/ethnicity and country of origin to variations in lifetime reported asthma: Evidence for a nativity advantage. American Journal of Public Health. 2009;99 (4):690–697. doi: 10.2105/AJPH.2007.128843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svendsen ER, Gonzales M, Ross M, Neas LM. Variability in childhood allergy and asthma across ethnicity, language, and residency duration in El Paso, Texas: A cross-sectional study. Environmental Health. 2009;8 (55):1–15. doi: 10.1186/1476-069X-8-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson EF, Nuru-Jeter A, Richardson D, Raza F, Minkler M. The Hispanic Paradox and older adults’ disabilities: is there a healthy migrant effect? International Journal of Environmental Research and Public Health. 2013;10 (5):1786–1814. doi: 10.3390/ijerph10051786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US-Mexico Border Health Commission. Health Disparities and the US-México Border: Challenges and Opportunities. The United States–México Border Health Commission; El Paso, TX: 2010. [Google Scholar]
- US Bureau of the Census. 2010 US Decennial Census. 2010 [Cited 29 June 2013]; Available from: http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml.
- US Bureau of the Census. American Community Survey, 2007–2011 5-year Estimates. 2011 [Cited 29 June 2013]; Available from: http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml.
- Visser PS, Krosnick JA, Marquette J, Curtin M. Mail Surveys for Election Forecasting? An Evaluation of the Columbus Dispatch Poll. Public Opinion Quarterly. 1996;60 (2):181–227. [Google Scholar]
- Warren N. Potential data sources for asthma surveillance at a county and state level in California. Berkley, CA: Regional Asthma Management and Prevention Initiative; 1999. [Google Scholar]
- Wen M, Browning CR, Cagney KA. Poverty, affluence, and income inequality: Neighborhood economic structure and its implications for health. Social Science & Medicine. 2003;57:843–860. doi: 10.1016/s0277-9536(02)00457-4. [DOI] [PubMed] [Google Scholar]
- Williamson IJ, Martin CJ, McGill G, Monie RDH, Fennerty AG. Damp housing and asthma: a case-control study. Thorax. 1997;52:229–234. doi: 10.1136/thx.52.3.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright RJ, Subramanian SV. Advancing a multilevel framework for epidemiologic research on asthma disparities. Chest. 2007;132 (5):757S–769S. doi: 10.1378/chest.07-1904. [DOI] [PubMed] [Google Scholar]